Program Book - Keck School of Medicine of USC - University of ...
Program Book - Keck School of Medicine of USC - University of ...
Program Book - Keck School of Medicine of USC - University of ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
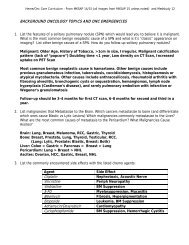
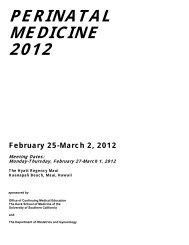
Nonmaturation <strong>of</strong> arm arteriovenous fistulas forhemodialysis access: A systematic review <strong>of</strong> riskfactors and results <strong>of</strong> early treatmentEduard H. J. Voormolen, BSc,a,b Abdelkarime Khodadade Jahrome, MD,c Lambertus W. Bartels, PhD,bFrans L. Moll, MD, PhD,c Willem P. Mali, MD, PhD,a and Peter J. Blankestijn, MD, PhD,dUtrecht, The NetherlandsIntroduction: Arteriovenous fistula (AVF) nonmaturation increases reliance <strong>of</strong> hemodialysis patients on grafts andcatheters, exposing them to associated high complication risks. This systematic review assessed the success rates andcomplications <strong>of</strong> therapeutic interventions in arm hemodialysis AVFs experiencing nonmaturation. It also compared theefficacy <strong>of</strong> preoperative clinical factors (eg, age, gender, race), and preoperatively and postoperatively acquiredhemodynamicparameters (eg, arterial diameter or blood flow through the AVF) at stratifying risk <strong>of</strong> nonmaturation.Methods: Two independent researchers used a systematic strategy to search literature databases and extract data fromarticles judged relevant and valid. The evidence base for this review comprised 33 articles, 12 about treatment, and 21concerning risk stratification. A meta-analysis was performed to calculate summary measures for nonmaturationtreatment success and risk stratification efficacy (eg, excess risk and relative risk) <strong>of</strong> preoperative clinical, preoperativehemodynamic, and postoperative hemodynamic risk factors.Results: The success rate <strong>of</strong> early endovascular or surgical treatment, defined as the possibility <strong>of</strong> achieving adequatehemodialysis, averaged 86%, with 1-year primary patencies <strong>of</strong> 51%, 1-year secondary patencies <strong>of</strong> 76%, and complicationrates <strong>of</strong> 9.3%, with 5.5% minor complications. Overall, patients with preoperative clinical risk factors had excessnonmaturation risks <strong>of</strong> 21% (95% confidence interval [CI], 11%-30%) and a relative risk <strong>of</strong> 1.7 (95% CI, 1.3-2.1). Patientswith preoperative hemodynamic risk factors had average estimated excess risks <strong>of</strong> 24% (95% CI, 15%-33%) and a relativerisk <strong>of</strong> 1.7 (95% CI, 1.4-2.0). Patients with hemodynamic risk factors present shortly after operation had excessnonmaturation risks <strong>of</strong> 50% (95% CI, 42%-58%) and a relative risk <strong>of</strong> 4.3 (95% CI, 3.4-5.5).Conclusions: Patients can be treated effectively for AVF nonmaturation early on, and it is possible to identify thosepatients at risk <strong>of</strong> nonmaturation most effectively with an early postoperative assessment <strong>of</strong> hemodynamic risk factors.Additional research is needed that concentrates on adopting the strategy <strong>of</strong> early treatment <strong>of</strong> patients with postoperativerisk factors. ( J Vasc Surg 2009;49:1325-36.)Meta-analysis• 1794 articles 33 articles with 745 patients fit criteria• Summary measures for risk stratification efficacy• Methodological quality <strong>of</strong> studies evaluated• Excess risk and relative risk for non-maturation calculated– Excess risk: The difference between the absolutenonmaturation risk <strong>of</strong> patients considered at risk (ie, patientswith risk factors) and considered not at risk (ie,patientswithout risk factors). A measure <strong>of</strong> 0% means no risk isconferred by the risk factor.– Relative risk: The nonmaturation risk <strong>of</strong> a patient at riskdivided by the nonmaturation risk <strong>of</strong> a patient not at risk. Ameasure <strong>of</strong> 1.0 means no risk is conferred.Voormolen E. J Vasc Surg 2009Meta-analysis•Methodological quality for most studies was poorRisk FactorsExcess Non-maturationRiskRelative Non-maturationRiskPre-operative Clinical Risk Factors 21% (95% CI, 11%-30%) 1.7 (95% CI, 1.3-2.1)Pre-operative Hemodynamic Factors 24% (95% CI, 15%-33%) 1.7 (95% CI, 1.4-2.0)Post-operative Hemodynamic Factors 50% (95% CI, 42%-58%) 4.3 (95% CI, 3.4-5.5)Voormolen E. J Vasc Surg 200987