INTENSIVE CARE
8dI2AMDUa
8dI2AMDUa
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
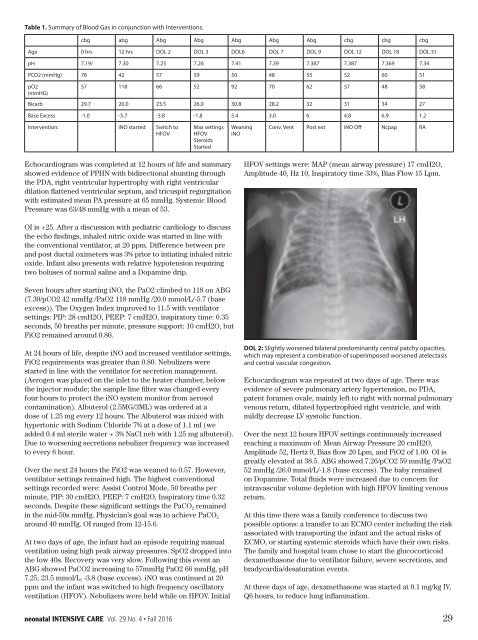
Table 1. Summary of Blood Gas in conjunction with Interventions.<br />
cbg abg Abg Abg Abg Abg Abg cbg cbg cbg<br />
Age 0 hrs 12 hrs DOL 2 DOL 3 DOL6 DOL 7 DOL 9 DOL 12 DOL 18 DOL 31<br />
pH 7.19/ 7.30 7.25 7.26 7.41 7.39 7.387 7.387 7.369 7.34<br />
PCO2 (mmHg) 78 42 57 59 50 48 55 52 60 51<br />
pO2<br />
(mmHG)<br />
57 118 66 52 92 70 62 57 48 58<br />
Bicarb 29.7 20.0 23.5 26.0 30.8 28.2 32 31 34 27<br />
Base Excess -1.0 -5.7 -3.8 -1.8 5.4 3.0 6 4.8 6.9 1.2<br />
Intervention: iNO started Switch to<br />
HFOV<br />
Max settings<br />
HFOV<br />
Steroids<br />
Started<br />
Weaning<br />
iNO<br />
Conv. Vent Post ext iNO Off Ncpap RA<br />
Echocardiogram was completed at 12 hours of life and summary<br />
showed evidence of PPHN with bidirectional shunting through<br />
the PDA, right ventricular hypertrophy with right ventricular<br />
dilation flattened ventricular septum, and tricuspid regurgitation<br />
with estimated mean PA pressure at 65 mmHg. Systemic Blood<br />
Pressure was 63/48 mmHg with a mean of 53.<br />
HFOV settings were: MAP (mean airway pressure) 17 cmH2O,<br />
Amplitude 40, Hz 10, Inspiratory time 33%, Bias Flow 15 Lpm.<br />
OI is +25. After a discussion with pediatric cardiology to discuss<br />
the echo findings, inhaled nitric oxide was started in line with<br />
the conventional ventilator, at 20 ppm. Difference between pre<br />
and post ductal oximeters was 3% prior to intiating inhaled nitric<br />
oxide. Infant also presents with relative hypotension requiring<br />
two boluses of normal saline and a Dopamine drip.<br />
Seven hours after starting iNO, the PaO2 climbed to 118 on ABG<br />
(7.30/pCO2 42 mmHg /PaO2 118 mmHg /20.0 mmol/L/-5.7 (base<br />
excess)). The Oxygen Index improved to 11.5 with ventilator<br />
settings: PIP: 28 cmH2O, PEEP: 7 cmH2O, inspiratory time: 0.35<br />
seconds, 50 breaths per minute, pressure support: 10 cmH2O, but<br />
FiO2 remained around 0.80.<br />
At 24 hours of life, despite iNO and increased ventilator settings,<br />
FiO2 requirements was greater than 0.80. Nebulizers were<br />
started in line with the ventilator for secretion management.<br />
(Aerogen was placed on the inlet to the heater chamber, below<br />
the injector module; the sample line filter was changed every<br />
four hours to protect the iNO system monitor from aerosol<br />
contamination). Albuterol (2.5MG/3ML) was ordered at a<br />
dose of 1.25 mg every 12 hours. The Albuterol was mixed with<br />
hypertonic with Sodium Chloride 7% at a dose of 1.1 ml (we<br />
added 0.4 ml sterile water + 3% NaCl neb with 1.25 mg albuterol).<br />
Due to worsening secretions nebulizer frequency was increased<br />
to every 6 hour.<br />
Over the next 24 hours the FiO2 was weaned to 0.57. However,<br />
ventilator settings remained high. The highest conventional<br />
settings recorded were: Assist Control Mode, 50 breaths per<br />
minute, PIP: 30 cmH2O, PEEP: 7 cmH2O, Inspiratory time 0.32<br />
seconds. Despite these significant settings the PaCO 2 remained<br />
in the mid-50s mmHg. Physician’s goal was to achieve PaCO 2<br />
around 40 mmHg. OI ranged from 12-15.6.<br />
At two days of age, the infant had an episode requiring manual<br />
ventilation using high peak airway pressures. SpO2 dropped into<br />
the low 40s. Recovery was very slow. Following this event an<br />
ABG showed PaCO2 increasing to 57mmHg PaO2 66 mmHg, pH<br />
7.25, 23.5 mmol/L, -3.8 (base excess). iNO was continued at 20<br />
ppm and the infant was switched to high frequency oscillatory<br />
ventilation (HFOV). Nebulizers were held while on HFOV. Initial<br />
DOL 2: Slightly worsened bilateral predominantly central patchy opacities,<br />
which may represent a combination of superimposed worsened atelectasis<br />
and central vascular congestion.<br />
Echocardiogram was repeated at two days of age. There was<br />
evidence of severe pulmonary artery hypertension, no PDA,<br />
patent foramen ovale, mainly left to right with normal pulmonary<br />
venous return, dilated hypertrophied right ventricle, and with<br />
mildly decrease LV systolic function.<br />
Over the next 12 hours HFOV settings continuously increased<br />
reaching a maximum of: Mean Airway Pressure 20 cmH2O,<br />
Amplitude 52, Hertz 9, Bias flow 20 Lpm, and FiO2 of 1.00. OI is<br />
greatly elevated at 38.5. ABG showed 7.26/pCO2 59 mmHg /PaO2<br />
52 mmHg /26.0 mmol/L/-1.8 (base excess). The baby remained<br />
on Dopamine. Total fluids were increased due to concern for<br />
intravascular volume depletion with high HFOV limiting venous<br />
return.<br />
At this time there was a family conference to discuss two<br />
possible options: a transfer to an ECMO center including the risk<br />
associated with transporting the infant and the actual risks of<br />
ECMO, or starting systemic steroids which have their own risks.<br />
The family and hospital team chose to start the glucocorticoid<br />
dexamethasone due to ventilator failure, severe secretions, and<br />
bradycardia/desaturation events.<br />
At three days of age, dexamethasone was started at 0.1 mg/kg IV,<br />
Q6 hours, to reduce lung inflammation.<br />
neonatal <strong>INTENSIVE</strong> <strong>CARE</strong> Vol. 29 No. 4 • Fall 2016 29