INTENSIVE CARE
8dI2AMDUa
8dI2AMDUa
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
After dexamethasone was given for one day, an ECHO on<br />
showed: improved mild to moderate right sided chamber<br />
dilation, and normal right ventricular systolic function, ongoing.<br />
The child had significant pulmonary improvement with<br />
dexamethasone. The dexamthasone was weaned by 0.1 mg/kg/<br />
per day from 0.4 to 0.1 mg/kg/ per day over three days. At six<br />
days of age HFOV settings were: (MAP: 15 cmH2O, Amplitude:<br />
34, Hz: 9, Flow: 20 Lpm, Inspiratory time 33% and FiO2 0.34).<br />
The iNO was weaned from 20 ppm to 18 ppm while PaO2<br />
remained greater than 90 mmHg. The goal was to keep PaO2 60<br />
to 100 mmHg, as the child was very labile.<br />
iNO had been weaned to 4 ppm remained at 4 ppm despite an<br />
increase in oxygen requirement. pCO2 on serial cbg’s showed<br />
a compensated respiratory acidosis at 57 to 55 mmHg post<br />
extubation.<br />
Repeat echocardiogram was done after the iNO was initially<br />
weaned. This showed improvement in pulmonary arterial<br />
pressures. Pulmonary artery pressure improved and right sided<br />
chamber dilatation decreased.<br />
At seven days of age, the infant transitioned back to conventional<br />
ventilation (SIMV mode, respiratory rate of 45 breaths per<br />
minute, PIP: 25 cmH2O, PEEP: 7 cmH2O, I time: 0.38 seconds,<br />
10 cmH2O of pressure support and FiO2 0.35). Nebulizers via the<br />
aerogen was restarted every six hours. Pulmicort SVN as added<br />
in BID 0.5 mg. Nitric Oxide was then weaned by 5ppm every six<br />
hours until reaching a dose of 5 ppm.<br />
At eight days of age, the infant met the NICU’s extubation<br />
guideline: FiO2 ≤35%, rate ≤ 25 bpm, PIP ≤ 18 cmH2O; pH ≥ 7.20,<br />
PCO2 ≤ 55 mmHg; No paralytic or excessive sedation; Caffeine if<br />
GA ≤30 wks; Post extubation support for 72 hrs.<br />
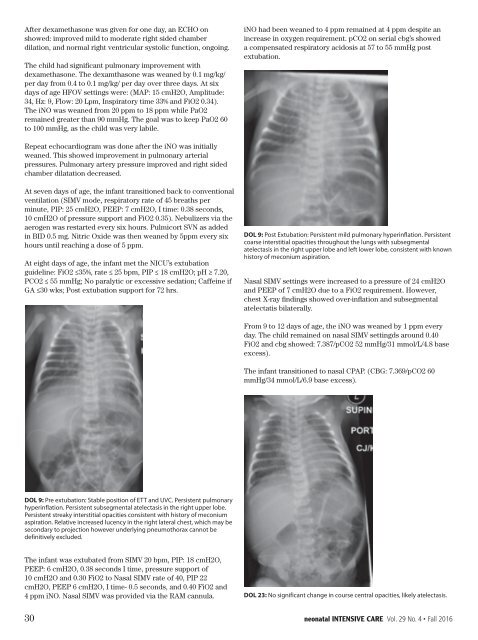
DOL 9: Post Extubation: Persistent mild pulmonary hyperinflation. Persistent<br />
coarse interstitial opacities throughout the lungs with subsegmental<br />
atelectasis in the right upper lobe and left lower lobe, consistent with known<br />
history of meconium aspiration.<br />
Nasal SIMV settings were increased to a pressure of 24 cmH2O<br />
and PEEP of 7 cmH2O due to a FiO2 requirement. However,<br />
chest X-ray findings showed over-inflation and subsegmental<br />
atelectatis bilaterally.<br />
From 9 to 12 days of age, the iNO was weaned by 1 ppm every<br />
day. The child remained on nasal SIMV settingds around 0.40<br />
FiO2 and cbg showed: 7.387/pCO2 52 mmHg/31 mmol/L/4.8 base<br />
excess).<br />
The infant transitioned to nasal CPAP. (CBG: 7.369/pCO2 60<br />
mmHg/34 mmol/L/6.9 base excess).<br />
DOL 9: Pre extubation: Stable position of ETT and UVC. Persistent pulmonary<br />
hyperinflation. Persistent subsegmental atelectasis in the right upper lobe.<br />
Persistent streaky interstitial opacities consistent with history of meconium<br />
aspiration. Relative increased lucency in the right lateral chest, which may be<br />
secondary to projection however underlying pneumothorax cannot be<br />
definitively excluded.<br />
The infant was extubated from SIMV 20 bpm, PIP: 18 cmH2O,<br />
PEEP: 6 cmH2O, 0.38 seconds I time, pressure support of<br />
10 cmH2O and 0.30 FiO2 to Nasal SIMV rate of 40, PIP 22<br />
cmH2O, PEEP 6 cmH2O, I time- 0.5 seconds, and 0.40 FiO2 and<br />
4 ppm iNO. Nasal SIMV was provided via the RAM cannula.<br />
DOL 23: No significant change in course central opacities, likely atelectasis.<br />
30 neonatal <strong>INTENSIVE</strong> <strong>CARE</strong> Vol. 29 No. 4 • Fall 2016