AETNA PPO PLAN - My Benefits Portfolio - Trinity Health
AETNA PPO PLAN - My Benefits Portfolio - Trinity Health
AETNA PPO PLAN - My Benefits Portfolio - Trinity Health
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
PARTICIPATION<br />
WHEN PARTICIPATION BEGINS<br />
You may elect coverage under the Plan within 30 days of the date you are first eligible for coverage (your<br />
“Initial Enrollment Period”) or during Annual Open Enrollment. If you are a newly hired benefits-eligible<br />
Associate and you elect coverage for yourself during your Initial Enrollment Period (i.e., within 30 days of<br />
your date of hire), your coverage will begin on the first day of the month after 30 days of employment with<br />
your Employer, measured from your date of hire. If you are a newly hired benefits-eligible Associate and<br />
you elect coverage for your eligible Dependents during your Initial Enrollment Period, your eligible<br />
Dependents’ coverage will begin on the same day your coverage begins.<br />
If you become a benefits-eligible Associate, as defined in your Employer’s policy that defines Associate<br />
classifications, after your initial date of hire by your Employer, your coverage will begin on the first day of the<br />
pay period following the date you become a benefits-eligible Associate (or the first day of the pay period<br />
following the date you complete 30 days of employment with your Employer, if later) if you enroll yourself in<br />
the Plan during your Initial Enrollment Period (i.e., within 30 days of the date you become a benefits-eligible<br />
Associate). If you become a benefits-eligible Associate after your initial date of hire by your Employer and<br />
you elect coverage for your eligible Dependents during your Initial Enrollment Period, your eligible<br />
Dependents’ coverage will begin on the same day your coverage begins.<br />
You must enroll yourself in the Plan in order to enroll your Dependents in the Plan.<br />
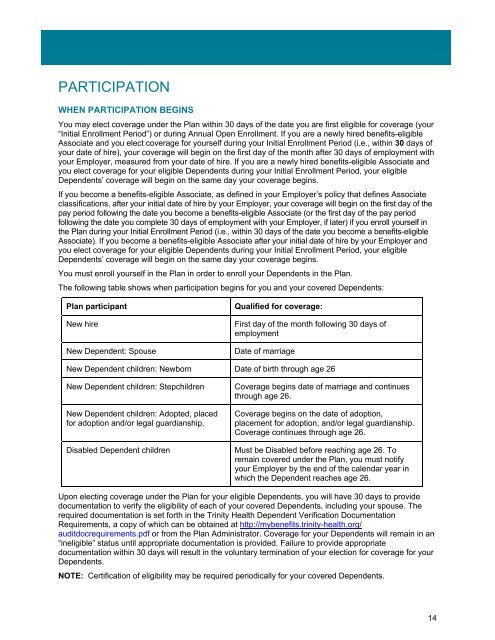
The following table shows when participation begins for you and your covered Dependents:<br />
Plan participant Qualified for coverage:<br />
New hire First day of the month following 30 days of<br />
employment<br />
New Dependent: Spouse Date of marriage<br />
New Dependent children: Newborn Date of birth through age 26<br />
New Dependent children: Stepchildren Coverage begins date of marriage and continues<br />
through age 26.<br />
New Dependent children: Adopted, placed<br />
for adoption and/or legal guardianship,<br />
Coverage begins on the date of adoption,<br />
placement for adoption, and/or legal guardianship.<br />
Coverage continues through age 26.<br />
Disabled Dependent children Must be Disabled before reaching age 26. To<br />
remain covered under the Plan, you must notify<br />
your Employer by the end of the calendar year in<br />
which the Dependent reaches age 26.<br />
Upon electing coverage under the Plan for your eligible Dependents, you will have 30 days to provide<br />
documentation to verify the eligibility of each of your covered Dependents, including your spouse. The<br />
required documentation is set forth in the <strong>Trinity</strong> <strong>Health</strong> Dependent Verification Documentation<br />
Requirements, a copy of which can be obtained at http://mybenefits.trinity-health.org/<br />
auditdocrequirements.pdf or from the Plan Administrator. Coverage for your Dependents will remain in an<br />
“ineligible” status until appropriate documentation is provided. Failure to provide appropriate<br />
documentation within 30 days will result in the voluntary termination of your election for coverage for your<br />
Dependents.<br />
NOTE: Certification of eligibility may be required periodically for your covered Dependents.<br />
14