Anthem Blue Cross Blue Shield PPO Plan - Teamworks at Home ...
Anthem Blue Cross Blue Shield PPO Plan - Teamworks at Home ...
Anthem Blue Cross Blue Shield PPO Plan - Teamworks at Home ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
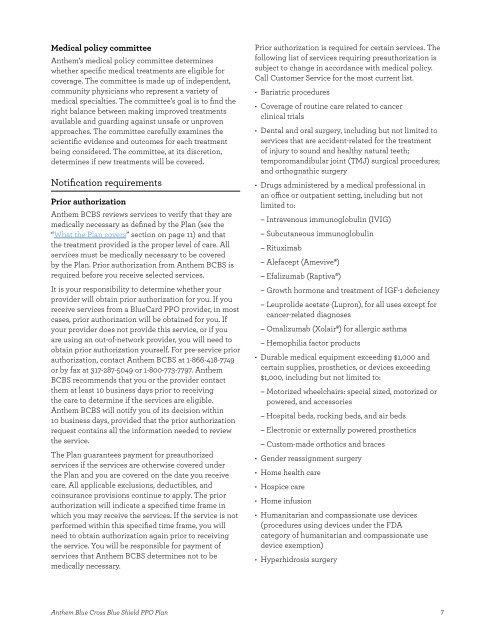
Medical policy committee<br />
<strong>Anthem</strong>’s medical policy committee determines<br />
whether specifc medical tre<strong>at</strong>ments are eligible for<br />
coverage� The committee is made up of independent,<br />
community physicians who represent a variety of<br />
medical specialties� The committee’s goal is to fnd the<br />
right balance between making improved tre<strong>at</strong>ments<br />
available and guarding against unsafe or unproven<br />
approaches� The committee carefully examines the<br />
scientifc evidence and outcomes for each tre<strong>at</strong>ment<br />
being considered� The committee, <strong>at</strong> its discretion,<br />
determines if new tre<strong>at</strong>ments will be covered�<br />
Notifc<strong>at</strong>ion requirements<br />
Prior authoriz<strong>at</strong>ion<br />
<strong>Anthem</strong> BCBS reviews services to verify th<strong>at</strong> they are<br />
medically necessary as defned by the <strong>Plan</strong> (see the<br />
“Wh<strong>at</strong> the <strong>Plan</strong> covers” section on page 11) and th<strong>at</strong><br />
the tre<strong>at</strong>ment provided is the proper level of care� All<br />
services must be medically necessary to be covered<br />
by the <strong>Plan</strong>� Prior authoriz<strong>at</strong>ion from <strong>Anthem</strong> BCBS is<br />
required before you receive selected services�<br />
It is your responsibility to determine whether your<br />
provider will obtain prior authoriz<strong>at</strong>ion for you� If you<br />
receive services from a <strong>Blue</strong>Card <strong>PPO</strong> provider, in most<br />
cases, prior authoriz<strong>at</strong>ion will be obtained for you� If<br />
your provider does not provide this service, or if you<br />
are using an out-of-network provider, you will need to<br />
obtain prior authoriz<strong>at</strong>ion yourself� For pre-service prior<br />
authoriz<strong>at</strong>ion, contact <strong>Anthem</strong> BCBS <strong>at</strong> 1-866-418-7749<br />
or by fax <strong>at</strong> 317-287-5049 or 1-800-773-7797� <strong>Anthem</strong><br />
BCBS recommends th<strong>at</strong> you or the provider contact<br />
them <strong>at</strong> least 10 business days prior to receiving<br />
the care to determine if the services are eligible�<br />
<strong>Anthem</strong> BCBS will notify you of its decision within<br />
10 business days, provided th<strong>at</strong> the prior authoriz<strong>at</strong>ion<br />
request contains all the inform<strong>at</strong>ion needed to review<br />
the service�<br />
The <strong>Plan</strong> guarantees payment for preauthorized<br />
services if the services are otherwise covered under<br />
the <strong>Plan</strong> and you are covered on the d<strong>at</strong>e you receive<br />
care� All applicable exclusions, deductibles, and<br />
coinsurance provisions continue to apply� The prior<br />
authoriz<strong>at</strong>ion will indic<strong>at</strong>e a specifed time frame in<br />
which you may receive the services� If the service is not<br />
performed within this specifed time frame, you will<br />
need to obtain authoriz<strong>at</strong>ion again prior to receiving<br />
the service� You will be responsible for payment of<br />
services th<strong>at</strong> <strong>Anthem</strong> BCBS determines not to be<br />
medically necessary�<br />
Prior authoriz<strong>at</strong>ion is required for certain services� The<br />
following list of services requiring preauthoriz<strong>at</strong>ion is<br />
subject to change in accordance with medical policy�<br />
Call Customer Service for the most current list�<br />
• Bari<strong>at</strong>ric procedures<br />
• Coverage of routine care rel<strong>at</strong>ed to cancer<br />
clinical trials<br />
• Dental and oral surgery, including but not limited to<br />
services th<strong>at</strong> are accident-rel<strong>at</strong>ed for the tre<strong>at</strong>ment<br />
of injury to sound and healthy n<strong>at</strong>ural teeth;<br />
temporomandibular joint (TMJ) surgical procedures;<br />
and orthogn<strong>at</strong>hic surgery<br />
• Drugs administered by a medical professional in<br />
an ofce or outp<strong>at</strong>ient setting, including but not<br />
limited to:<br />
– Intravenous immunoglobulin (IVIG)<br />
– Subcutaneous immunoglobulin<br />
– Rituximab<br />
– Alefacept (Amevive®)<br />
– Efalizumab (Raptiva®)<br />
– Growth hormone and tre<strong>at</strong>ment of IGF-1 defciency<br />
– Leuprolide acet<strong>at</strong>e (Lupron), for all uses except for<br />
cancer-rel<strong>at</strong>ed diagnoses<br />
– Omalizumab (Xolair®) for allergic asthma<br />
– Hemophilia factor products<br />
• Durable medical equipment exceeding $1,000 and<br />
certain supplies, prosthetics, or devices exceeding<br />
$1,000, including but not limited to:<br />
– Motorized wheelchairs: special sized, motorized or<br />
powered, and accessories<br />
– Hospital beds, rocking beds, and air beds<br />
– Electronic or externally powered prosthetics<br />
– Custom-made orthotics and braces<br />
• Gender reassignment surgery<br />
• <strong>Home</strong> health care<br />
• Hospice care<br />
• <strong>Home</strong> infusion<br />
• Humanitarian and compassion<strong>at</strong>e use devices<br />
(procedures using devices under the FDA<br />
c<strong>at</strong>egory of humanitarian and compassion<strong>at</strong>e use<br />
device exemption)<br />
• Hyperhidrosis surgery<br />
<strong>Anthem</strong> <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>PPO</strong> <strong>Plan</strong> 7