EDI - BdiZ
EDI - BdiZ
EDI - BdiZ
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
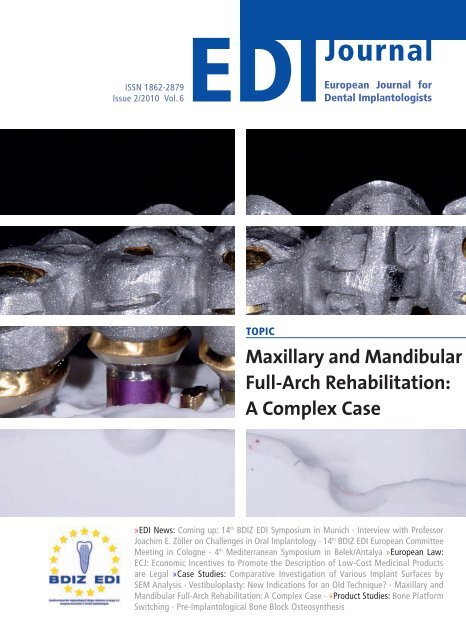
ISSN 1862-2879<br />
Issue 2/2010 Vol. 6<br />
<strong>EDI</strong> Journal<br />
European Journal for<br />
Dental Implantologists<br />
TOPIC<br />
Maxillary and Mandibular<br />
Full-Arch Rehabilitation:<br />
A Complex Case<br />
»<strong>EDI</strong> News: Coming up: 14 th BDIZ <strong>EDI</strong> Symposium in Munich · Interview with Professor<br />
Joachim E. Zöller on Challenges in Oral Implantology · 14 th BDIZ <strong>EDI</strong> European Committee<br />
Meeting in Cologne · 4 th Mediterranean Symposium in Belek/Antalya »European Law:<br />
ECJ: Economic Incentives to Promote the Description of Low-Cost Medicinal Products<br />
are Legal »Case Studies: Comparative Investigation of Various Implant Surfaces by<br />
SEM Analysis · Vestibuloplasty: New Indications for an Old Technique? · Maxillary and<br />
Mandibular Full-Arch Rehabilitation: A Complex Case · »Product Studies: Bone Platform<br />
Switching · Pre-Implantological Bone Block Osteosynthesis
ONE BOA CONSTRICTOR, TWO SCORPIONS<br />
TWELVE PIRANHAS<br />
AND A RELIABLE IMPLANT<br />
Life can be dangerous. Camlog is safe.<br />
More information: www.camlog.com<br />
a perfect fit ©
If you don’t already know<br />
Bavaria and Munich –<br />
come and get to know<br />
it now! I would like to<br />
invite you to the “me -<br />
tro polis with a heart” on<br />
the banks of the river<br />
Isar on 15 and 16 October 2010. As you can imagine, it was not<br />
primarily the interesting museums and the unique Bavarian<br />
spirit that prompted me to issue this invitation. Rather, it<br />
was that on these two days, BDIZ <strong>EDI</strong> is going to address the<br />
challenges awaiting oral implantologists and their teams now<br />
and over the next few years.<br />
This issue of the <strong>EDI</strong> Journal contains the complete schedule<br />
of events for this notable symposium – and I can promise you<br />
that you will not be lacking in anything: Reliable information<br />
by eminent healthcare experts explaining to you in which<br />
direction the fee schedule discussion is developing and what<br />
the legal and political framework for your dental office will be<br />
in the future. And there will be top-notch continuing dental<br />
education – as usual you can trust Prof Joachim E. Zöller to<br />
select a highly qualified and balanced team of expert speakers.<br />
Talking about challenges in oral implantology means moving<br />
the focus away from the successes and breathtaking pictures<br />
and taking a more scrutinizing look instead. This time we are<br />
also going to show the problems and the failures, offering tips<br />
and tricks for the pre-insertion stages to prevent complications<br />
before they can manifest themselves, and helpful advice for<br />
dealing with problems that nevertheless occur.<br />
By popular request, BDIZ <strong>EDI</strong> will again be holding this event<br />
in the exclusive atmosphere of the five-star Sofitel Munich Bayer -<br />
post. More than 400 attendees had enjoyed themselves there<br />
last year, and we hope to equal, if not exceed, this mark in 2010.<br />
So we will be holding our symposium in the middle of the<br />
city again, offering you a special treat right at the beginning: A<br />
“getting-ready-for-success” training for the entire dental team<br />
with former first-league handball player Jörg Löhr, today a<br />
much sought-after motivational coach who has inspired the<br />
managers and staff of many major companies in Germany.<br />
I myself was at one of his coaching sessions at one point, and<br />
I can assure you: After only two hours, you and your team will<br />
be highly motivated and set on taking active steps, or at least<br />
looking at things from a new angle.<br />
It’s the Right Mix<br />
that Counts!<br />
Determination and a thirst for action are two of the attri -<br />
butes that characterize members of the free professions anyway.<br />
Unfortunately, our tedious daily struggle with laws, rules<br />
and regulations – not to mention the eternal fights with reimbursement<br />
agents – will often cause us to lose our drive. Time,<br />
then, to revive it!<br />
With just the right dose of motivation, you will be ready<br />
to meet the challenges of the fee schedule discussions at<br />
the Health Politics Forum. Our team of experts and decision-makers<br />
will update you on current issues in healthcare<br />
politics.<br />
Here, too, a healthy mix of theory and practice is the road to<br />
success. And with this, I am actually giving away a secret, the<br />
secret of the BDIZ <strong>EDI</strong> philosophy: A healthy mix of theory and<br />
practice is what the BDIZ founding father, the late Prof Egon<br />
Brinkmann kept demanding almost ad nauseam. We are continuing<br />
along the path he outlined for us: The mix of theory<br />
and practice is reflected in the daily work of BDIZ <strong>EDI</strong>. Proof<br />
of this are the annual Guideline of the European Consensus<br />
Conference held under the auspices of BDIZ <strong>EDI</strong>, as well as<br />
the BDIZ <strong>EDI</strong> symposia – which becomes particularly obvious<br />
when you look at the second part of the event, the scientific<br />
programme. So what, exactly, are the challenges we are facing<br />
in daily clinical practice? How do I avoid complications, including<br />
major ones such as nerve damage? How do I tackle surgical<br />
and prosthetic problems – more specifically: What do I<br />
do if the nerve already appears to be damaged? How do I<br />
proceed during a sinus lift? And what about subsequent coverage?<br />
What is the key to success in bone augmentation?<br />
What pre-existing conditions must I take into account, and<br />
what medications are actually helpful? What are the benefits<br />
of drilling stents and 3D planning and surgery? How do<br />
I design, process and insert ceramic restorations to avoid<br />
fractures and chipping?<br />
In our daily practice it is important to forestall complications,<br />
to master problems and to avoid failures. And this can in fact<br />
be done successfully. Come to Munich and see for yourself!<br />
Attend the congress, bring your team – and make sure you set<br />
aside a few hours to enjoy the city and its splendours!<br />
Sincerely,<br />
Christian Berger, Kempten/Germany<br />
President of BDIZ <strong>EDI</strong><br />
<strong>EDI</strong><br />
Editorial<br />
3
4 <strong>EDI</strong><br />
Table of Content<br />
<strong>EDI</strong> News<br />
Mastering Challenges in Everyday Practice<br />
14 th BDIZ <strong>EDI</strong> Symposium in Munich,<br />
15/16 October 2010 8<br />
The Time of Breathtaking Pictures is over<br />
Interview with Prof Joachim E. Zöller on<br />
challenges in oral implantology 22<br />
European Curriculum under Development<br />
14 th BDIZ <strong>EDI</strong> European Committee meeting<br />
in Cologne 26<br />
4 th Mediterranean Symposium: See Turkey and<br />
Learn Something<br />
Successful BDIZ <strong>EDI</strong> continuing-education week<br />
in Belek/Antalya 28<br />
Top-level Implantological Training<br />
12 th BDIZ <strong>EDI</strong> Curriculum Implantology to start<br />
in November 2010 34<br />
Successful Exam Candidate in Cologne<br />
EDA Expert in Implantology 37<br />
Upcoming EDA Expert in Implantology<br />
Certification Exam<br />
Munich, 17 October 2010 37<br />
International Expert Symposium for Regenerative<br />
Methods in Medicine and Dentistry<br />
Visiting Fuerteventura for the 20 th time 38<br />
BDIZ <strong>EDI</strong> in Barcelona<br />
14 th Dentsply Friadent World Symposium 39<br />
International Congress for Maxillofacial Surgery<br />
Belgrade, 27 to 29 October 2010 40<br />
18 th International SEI Convention in Spain<br />
Seville, 25 to 27 November 2010 40<br />
Europe Ticker 42<br />
European Law<br />
ECJ: Economic Incentives to Promote the<br />
Description of Low-Cost Medicinal Products<br />
are Legal 46<br />
Page 78: Pre-implantological bone block osteosynthesis.<br />
Case Studies<br />
Surprises in the Land of Microns<br />
Comparative investigation of various implant<br />
surfaces by SEM analysis 50<br />
New Indications for an Old Technique?<br />
Neugebauer on vestibuloplasty 55<br />
Maxillary and Mandibular Full-Arch Rehabilitation:<br />
A Complex Case<br />
Well-organized teamwork: Periodontology,<br />
implantology, prosthodontics 58<br />
Marketing and Other Types of “Mad Cow Disease”<br />
Neugebauer et al on augmentation materials 70<br />
Product Studies<br />
Bone Platform Switching<br />
3D finite element analysis comparing standard<br />
and reverse conical neck implants 72<br />
Functional Innovations<br />
Pre-implantological bone block osteosynthesis 76<br />
Business & Events<br />
Success is...<br />
14 th Dentsply Friadent World Symposium 80<br />
The Conversation of Geneva<br />
ITI World Symposium 2010 84<br />
For the Patient’s Benefit<br />
Osteology Symposium Baden-Baden 2010 86<br />
6 th Mozo-Grau Update Congress on Implantology 90<br />
International Osteology Symposium, Cannes,<br />
April 14 to 16, 2011 91<br />
Straumann Launches Digital Solutions Platform 92<br />
Materialise Dental NV Collaborates with<br />
Cefla Dental Group and QR srl 93<br />
Twenty Years of Omnia 94<br />
Dr Berthold Reusch Takes over 95<br />
News and Views<br />
Editorial: It’s the Right Mix that Counts! 3<br />
Imprint 6<br />
Product Reports 96<br />
Product News 100<br />
Calendar of Events 106<br />
Publishers Corner 106
Encode_Impression_System ad_<strong>EDI</strong> 07/06/10 11:07 Page 1<br />
Say Goodbye To Impression Copings<br />
Introducing The Encode ® Impression System<br />
Ask Your Surgeon To Place Encode Healing<br />
Abutments Exclusively Through BIOMET 3i<br />
To Learn More About All Of The Superior Solutions BIOMET 3i Has To<br />
Offer, Contact Your Local Sales Representative Today.<br />
Europe, Middle East, Africa Headquarters: +34-93-470-55-00<br />
or visit us online at www.biomet3i.com<br />
Encode is a registered trademark of BIOMET 3i LLC. BIOMET is a registered trademark and BIOMET 3i<br />
and design are trademarks of BIOMET, Inc. ©2010 BIOMET 3i LLC. All rights reserved.
6<br />
<strong>EDI</strong><br />
Imprint<br />
<strong>EDI</strong><br />
European Journal for Dental Implantologists<br />
a BDIZ <strong>EDI</strong> publication<br />
published by teamwork media GmbH, Fuchstal<br />
Association: The European Journal for Dental Implantologists (<strong>EDI</strong>)<br />
is published in cooperation with BDIZ <strong>EDI</strong><br />
Publisher Board<br />
Members:<br />
Christian Berger<br />
Prof Dr Dr Joachim E. Zöller<br />
Dr Detlef Hildebrand, Dr Thomas Ratajczak<br />
Editor in Chief: Ralf Suckert, r.suckert@teamwork-media.de<br />
Editors: Anita Wuttke, Phone +49 89 72069-888, wuttke@bdizedi.org<br />
Simone Stark, Phone +49 8243 9692-34, s.stark@teamwork-media.de<br />
Scientific Board: Prof Dr Alberico Benedicenti, Genoa Dr Marco Degidi, Bologna<br />
Dr Eric van Dooren, Antwerp Prof Dr Rolf Ewers, Vienna<br />
Prof Dr Antonio Felino, Porto PD Dr Jens Fischer, Bern<br />
Dr Roland Glauser, Zurich Prof Dr Dr Ingrid Grunert, Innsbruck<br />
Dr Detlef Hildebrand, Berlin Dr Axel Kirsch, Filderstadt<br />
Prof Dr Ulrich Lotzmann, Marburg Prof Dr Edward Lynch, Belfast<br />
Dr Konrad Meyenberg, Zurich Prof Dr Georg Nentwig, Frankfurt<br />
Dr Jörg Neugebauer, Cologne Prof Hakan Özyuvaci, Istanbul<br />
Prof Dr Georgios Romanos, Rochester MDT Luc and Patrick Rutten, Tessenderlo<br />
Dr Henry and Maurice Salama, Atlanta Dr Ashok Sethi, London<br />
Ralf Suckert, Fuchstal Prof Dr Dr Joachim Zöller, Cologne<br />
All case reports and scientific documentations are peer reviewed by the international editorial board<br />
of “teamwork – Journal of Multidisciplinary Collaboration in Restorative Dentistry“<br />
Project Management<br />
& Advertising:<br />
Marianne Steinbeck, MS Media Service, Badstraße 5, D-83714 Miesbach,<br />
Phone +49 8025 5785, Fax +49 8025 5583, ms@msmedia.de, www.msmedia.de<br />
Publishers: teamwork media Verlags GmbH, Hauptstr. 1, D-86925 Fuchstal<br />
Phone +49 8243 9692-11, Fax +49 8243 9692-22<br />
service@teamwork-media.de, www.teamwork-media.de<br />
Layout: Sigrid Eisenlauer; teamwork media GmbH<br />
Printing: J. Gotteswinter GmbH; Munich<br />
Publication Dates: March, June, September, December<br />
Subscription Rates: Annual subscription: Germany € 40.- including shipping and VAT. All other countries € 58.- including shipping. Subscription<br />
payments must be made in advance. Ordering: in written form only to the publisher. Cancellation deadlines:<br />
in written form only, 8 weeks prior to end of subscription year. Subscription is governed by German law. Past issues<br />
are available. Complaints regarding nonreceipt of issues will be accepted up to 3 months after date of publication.<br />
Current advertising rate list No. 1, from 1/01/05<br />
ISSN 1862-2879<br />
Payments: to teamwork media GmbH;<br />
Raiffeisenbank Fuchstal BRC 733 698 54 Account No.100 416746<br />
Copyright and<br />
Publishing Rights:<br />
All rights reserved. The magazine and all articles and illustrations therein are protected by copyright. Any utilization<br />
without the prior consent of editor and publisher is inadmissible and liable to prosecution. No part of this publication<br />
may be produced or transmitted in any form or by any means, electronic or mechanical including by photocopy, recording,<br />
or information storage and retrieval system without permission in writing from the publisher. With acceptance of<br />
manuscripts the publisher has the right to publish, translate, permit reproduction, electronically store in databases, produce<br />
reprints, photocopies and microcopies. No responsibility shall be taken for unsolicited books and manuscripts. Articles<br />
bearing symbols other than of the editorial department or which are distinguished by the name of the authors represent<br />
the opinion of the afore-mentioned, and do not have to comply with the views of BDIZ <strong>EDI</strong> or teamwork media<br />
GmbH. Responsibility for such articles shall be borne by the author. All information, results etc. contained in this publication<br />
are produced by the authors with best intentions and are carefully checked by the authors and the publisher. All<br />
cases of liability arising from inaccurate or faulty information are excluded. Responsibility for advertisements and other<br />
specially labeled items shall not be borne by the editorial department.<br />
Copyright: teamwork media GmbH . Legal Venue: Munich
100223_WH_AD_ELCOMED_A4_AEN_120JAHRE:Layout 1 26.02.10 10:48 Seite 1<br />
80 Ncm<br />
Powerful for surgery<br />
120 Years W&H.<br />
Help us support SOS Children’s Villages!<br />
The new Elcomed from W&H: logical and easy to use. Uncompromising<br />
in performance: with a torque of up to 80 Ncm on the rotating instrument,<br />
the surgical drive unit guarantees smooth usage, which can be completely<br />
documented at no further cost thanks to an integrated USB interface.<br />
These are just three of the many advantages of the new W&H Elcomed.<br />
People have Priority: W&H supports the humanitarian organization SOS Children’s Villages.<br />
Get involved! Further information at wh.com<br />
Captivation and precision
8<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
An old adage says that the early bird catches the<br />
worm. With so many different options, choosing the<br />
right activity from the pre-congress programme may<br />
be a challenge in its own right. If you attend the<br />
CBCT course on radiation protection in dentistry,<br />
you will be among the first up and around on Friday.<br />
The course hopes to duplicate last year’s success,<br />
with more than 100 dentists attending. Part 1 will<br />
run from 7:30 am to 12:30 pm on Friday and from<br />
6:00 pm to 7:00 pm on Saturday. Part 2 and the<br />
final examination will take place on 5 March 2011,<br />
at the 6 th BDIZ <strong>EDI</strong> Expert Symposium in Cologne.<br />
If you do not require the CBCT course, you may<br />
choose between three different industry workshops:<br />
bredent medical, Sirona Dental and Camlog are all<br />
ready to meet the challenges of oral implantology in<br />
their own way.<br />
Training for success<br />
14 th BDIZ <strong>EDI</strong> Symposium in<br />
Munich, 15/16 October 2010<br />
Mastering<br />
Challenges<br />
in Everyday<br />
Practice<br />
Munich, the Bavarian metropolis that styles itself “cosmopolitan city with a heart”, will soon catch the attention of clinical<br />
dental implantologists for the second year in a row. The 14 th BDIZ <strong>EDI</strong> Symposium, to be held at the Sofitel Munich Bayerpost<br />
on 15 and 16 October 2010, will address topics of interest to the entire dental team. As in 2009, BDIZ <strong>EDI</strong> is expecting more<br />
than 400 attendees. The motto of the symposium will be “Mastering Challenges”.<br />
Course in radiation protection<br />
Starting at 10 o’clock on Friday, BDIZ <strong>EDI</strong> will offer<br />
an absolute novelty for the dental office – that is,<br />
the entire dental team: Former professional handball<br />
player and star motivational coach Jörg Löhr from<br />
Augsburg will present dentists and assistants a number<br />
of important facets of successful office management.<br />
Löhr is one of the most popular coaches in Germany,<br />
inspiring Top 100 companies such as carmaker<br />
BMW, Germany’s mighty automobile association<br />
ADAC and Bundesliga football team Eintracht Frankfurt.<br />
After the lunch break, dental assistants will<br />
branch off to their own programme.<br />
For dentists, a top-notch panel of speakers hosted<br />
by BDIZ <strong>EDI</strong> President Christian Berger will try to<br />
answer the question “Quo vadis, GOZ?” at the Health-<br />
On Friday, 15 October and Saturday, 16 October, BDIZ will be offering another CBCT course (Part 1) in radiation<br />
protection in dentistry covering advanced technical aspects of digital cone-beam computed tomography, also<br />
called digital volume tomography or DVT. This special course has been approved by the Chambers of Dentists<br />
of the state of North Rhine-Westphalia and Bavaria and is a prerequisite for gaining approval operating a CBCT<br />
unit. Approval requires, in addition to the theoretical expertise acquired within the framework of the Munich<br />
course (Part 1) and by attending the presentations at the Munich symposium, a three-month practical training<br />
period after the course. This practical training will be offered at the University of Cologne in small groups by<br />
individual appointment. Part 2 of the course and the final examination will take place on 5 March 2011 at the<br />
6 th BDIZ <strong>EDI</strong> Expert Symposium in Cologne. More information: www.bdizedi.org
The Sofitel<br />
Munich Bayerpost<br />
will be the<br />
venue of the<br />
14 th BDIZ <strong>EDI</strong><br />
Symposium.<br />
care Politics Forum, including renowned experts on<br />
the German healthcare scene. (GOZ is the German<br />
standard fee schedule for dentists, applicable to private<br />
patients, including patients with private health<br />
insurance.) Prof Johann Eekhoff will present an analysis<br />
of the status quo in healthcare, while Dr Thomas<br />
Drabinski of the Institute for Micro-Data Analysis<br />
(IfMDA) in Kiel will explain what the so-called small<br />
flat-rate health insurance premium (“kleine Gesundheitsprämie”)<br />
will mean for dentists. Peter Knüpper,<br />
attorney and Managing Director of the Bavarian<br />
Chamber of Dentists, will explore whether dental<br />
care can continue to be funded by statutory health<br />
insurance. Wolfgang Reif of the Bavarian State Committee<br />
for private health insurance will be addressing<br />
the issue of future remuneration models for dental<br />
services from the point of view of private health<br />
insurers. Michael Schwarz, President of the Bavarian<br />
Chamber of Dentists, will show how HOZ (which is<br />
the German Dental Association’s fee schedule) can<br />
be implemented in the dental office. This part of the<br />
Hot Sax Club<br />
symposium will conclude with Dr Thomas Ratajczak<br />
answering the quo vadis question. This year’s welcoming<br />
address will be given by Dr Wolfgang Heu -<br />
bisch, BDIZ <strong>EDI</strong> member and Bavarian State Minister<br />
of Science, Research and Art.<br />
The “Prime Minister” is coming!<br />
Friday night’s highlight is likely to be the performance<br />
by political satirist Wolfgang Krebs parodying<br />
former Bavarian prime minister Edmund Stoiber at<br />
the BDIZ <strong>EDI</strong> gala night. “Edmund Stoiber” is bent on<br />
explaining the world to oral implantologists. At the<br />
request of many members and attendees, the fivecourse<br />
gala dinner and musical entertainment will<br />
once again be held at the Lenbach – not in the<br />
restaurant’s dining room this time, but in the tapestry<br />
room. Also like last year, the four saxophone players<br />
of the Hot Sax Club will play to their heart’s<br />
desire, and again you may look forward to beholding<br />
them in their constantly changing, breathtakingly<br />
glamorous wardrobe. BDIZ <strong>EDI</strong> President Christian<br />
Berger will be awarding the 2010 BDIZ <strong>EDI</strong> Medal of<br />
Honour to a highly deserving implantologist, who is<br />
also a speaker at the scientific sessions. (But that is<br />
all we are ready to give away at this time!)<br />
B as in Brodbeck to Z as in Zöller<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
After a glamourous evening and night, it will be “back<br />
to business” on Saturday. What do the challenges in<br />
oral implantology consist of today? This will be the<br />
focus of the scientific programme at the 14 th BDIZ <strong>EDI</strong><br />
Symposium. If you want to read up on the topic<br />
ahead of time, you should not miss the interview<br />
Annual General Meeting<br />
The Hot Sax Club is an all-female jazz quartet whose members will be<br />
performing familiar jazz tunes on their saxophones – acoustic saxophones,<br />
no amplifiers. These could be catchy tunes from the 1920s like<br />
Charleston or Entertainer, or melodies from the Glenn Miller era such as<br />
In the Mood or Summertime – or more contemporary arrangements<br />
such as The Pink Panther or Don't worry, be happy.<br />
This year’s Annual General Meeting of BDIZ <strong>EDI</strong><br />
will take place at the Sofitel Munich Bayerpost<br />
hotel on Saturday, 16 October 2009 between<br />
12:15 pm and 2:00 pm. Conspicuous signs will<br />
guide participants to the appropriate room.<br />
9
Institute<br />
The Eduardo Anitua Institute (Vitoria, Spain)<br />
is one of the outstanding international<br />
training centres in the fields of implantology<br />
and oral rehabilitation. Supported by most<br />
modern medical and audiovisual technologies<br />
you experience advanced training on highest<br />
level, scientific and practice oriented.<br />
The centre includes an auditorium for 74<br />
persons, several seminar rooms and an<br />
additional training room for practical<br />
exercises.<br />
Advanced Training<br />
The desired live-surgery courses of Dr. Eduardo<br />
Anitua are offered several times per year. The<br />
capabilities of the attendants get improved in the<br />
most important areas of implantology by livesurgeries,<br />
practice oriented lectures and handson<br />
exercises.<br />
For further information<br />
please contact:<br />
BTI Biotechnology Institute<br />
San Antonio 15 - 5º<br />
01005 Vitoria (ALAVA) • SPAIN<br />
BTI<br />
Training Center<br />
www.eduardoanitua.com<br />
Tel.: (34) 945 149 202<br />
Fax: (34) 945 154 909<br />
export@bti-implant.es
Extrashort implants<br />
5-year retrospective study with<br />
BTI short implants (99.2 % success<br />
rate):<br />
Anitua E, Orive G, Aguirre JJ, Andía I. 5 year clinical<br />
evaluation of short dental implants placed in posterior<br />
areas: a retrospective study. J Periodontology 2008;<br />
79: 42-48.<br />
0.5 mm.<br />
Biotechnology Institute<br />
San Antonio 15 - 5º<br />
01005 Vitoria (ALAVA)<br />
SPAIN<br />
Tel.: (34) 945 149 202<br />
Fax: (34) 945 154 909<br />
export@bti-implant.es<br />
LEADING INNOVATION<br />
1.5 mm.<br />
4 mm.<br />
5.5 mm.<br />
0.5 mm.<br />
L: 5.5 mm. L: 6.5 mm. L: 7.5 mm. L: 8.5 mm.<br />
1.5 mm.<br />
5 mm.<br />
Ø mm.: 2.5 3 3.3 3.5 3.75 3.3 3.5 3.75 4 4.25 4 4.5 5 5.5 4.5 5 5.5 6<br />
6.5 mm.<br />
These implants have 1,5 mm from the platform to the first thread. If we place them in a supracrestal way<br />
we would need only a 4 mm of bone in order to fix the implant.<br />
Only with a 5.5 mm of bone we would be able to place an implant of 6.5 mm length, in a supracrestal way.<br />
World's largest range of implant diameter and lengths<br />
Predictability and biosafety of BTI Dental Implants.<br />
Anitua E, Orive G, Aguirre JJ, Andía I. Clinical outcome of immediately loaded BTI dental implants: a 5-year retrospective study.<br />
J Peridontology 2008;79:1168-1176.<br />
Retrospective study with 5787 BTI Dentals Implants in 1060 patients (99.2 % of success).<br />
Anitua E, Orive G, Aguirre JJ, Andía I. 5-year clinical experience with BTI Dental Implants: risk factors for implant failure.<br />
J Clin Periodontol 2008;35:724-732.<br />
BTI of North America<br />
1730 Walton Road<br />
Suite 110<br />
Blue Bell, PA 19422-1802 US<br />
Tel: (1) 215 646-4067<br />
Fax: (1) 215 646-4066<br />
info@bti-implant.us<br />
BTI Deutschland GmbH.<br />
Mannheimer Str. 17<br />
75179 Pforzheim<br />
GERMANY<br />
Tel: (49) 7231 428060<br />
Fax: (49) 7231 4280615<br />
info@bti-implant.de<br />
BTI Implant Italia Srl.<br />
Piazzale Piola n.1<br />
20131 Milano<br />
ITALY<br />
Tel.: (39) 02 70605067<br />
Fax: (39) 02 70639876<br />
bti.italia@bti-implant.it<br />
BTI de México<br />
Lope de Vega 117, 701-702<br />
11570 Col. Chapultepec Morales<br />
México DF • MEXICO<br />
Tel.: (52) 55 52502964<br />
Fax: (52) 55 55319327<br />
bti.mexico@bti-implant.com<br />
BTI Portugal<br />
R. Pedro Homem de Melo<br />
55 S/6.03<br />
4150-000 Porto • PORTUGAL<br />
Tel: (351) 22 618 97 91<br />
Fax: (351) 22 610 59 21<br />
bti.portugal@sapo.pt<br />
www.bti-implant.com / www.prgf.org
12<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
with Prof Joachim E. Zöller, Scientific Director of the<br />
programme and BDIZ <strong>EDI</strong> Vice President, in the <strong>EDI</strong><br />
News section of this issue. The “Challenges” topic<br />
complements the range of issues that had been discussed<br />
earlier this year at the Expert Symposium in<br />
Cologne. But even if you did not attend Cologne, the<br />
programme of the 14 th BDIZ <strong>EDI</strong> Symposium will offer<br />
valuable advice for your clinical practice and assist<br />
you in dealing with complications.<br />
The panel of speakers includes experienced<br />
implantologists who are not afraid to discuss complications<br />
and failures. The initial presentation by<br />
Dr Jörg Neugebauer (Cologne) will try to answer the<br />
question whether medications can influence implantological<br />
success. Next, Dr Achim Nickenig (Cologne)<br />
will address the technique of template-guided<br />
implant insertion; Prof Rolf Ewers (Vienna) will elaborate<br />
on principles of guided surgery. Dr Stefan Reinhardt<br />
(Münster) will present the various bone augmentation<br />
options, and Prof Peter Tetsch (Münster)<br />
will evaluate the sinus lift. Dr Frank Kistler (Landsberg)<br />
will demonstrate the immediate placement<br />
of implants without augmentation. Prof Germán<br />
Gómez-Román (Tübingen) will inquire into what<br />
parameters determine success in the aesthetic zone.<br />
Dr Arndt Happe (Münster) will focus on the difficult<br />
issue of soft-tissue management. Before looking<br />
more closely at the materials, Prof Antonio Felino<br />
(Porto) is planning to emphasize the importance of<br />
bone-preserving surgical techniques for subsequent<br />
implantation procedures. Prof Peter Pospiech (Bad<br />
Homburg) will tackle the issue of ceramic chippings,<br />
!<br />
Please register via fax<br />
+49 228 9359-246<br />
or by mail<br />
BDIZ <strong>EDI</strong> Geschäftsstelle Bonn<br />
An der Esche 2<br />
D-53111 Bonn<br />
trying to investigate whether chipping is a problem<br />
in prosthodontics or a problem in material technology.<br />
Dr Urs Brodbeck (Zürich) is also going to look at allceramic<br />
restorations and tries to answer the question<br />
whether everything really is simple without metal.<br />
“Managing complications in oral implantology<br />
requires a thorough understanding of the biological<br />
situation and many years of clinical experience”,<br />
wrote Prof Joachim E. Zöller in his preface to the<br />
programme of the 14 th BDIZ <strong>EDI</strong> Symposium. These<br />
experienced practitioners and representatives of the<br />
academic world will share their knowledge with the<br />
attendees of the Munich event.<br />
AWU<br />
Registration<br />
Symposium und CBCT course<br />
Members/assistant members of BDIZ <strong>EDI</strong>: €700 (after 1 August: €790)<br />
Non-members: €1,300 (after 1 August: €1,390)<br />
Symposium only<br />
Members of BDIZ <strong>EDI</strong>: €320 (after 1 August: €390) Non-members: €390 (after 1 August: €460)<br />
Assistants/students: €260 (after 1 August: €310)<br />
Programme for dental assistants<br />
€120 (after 1 August: €160)<br />
(The conference fee is not subject to VAT.)<br />
Gala Night: ______ tickets @ €95 p.p. (incl. VAT) = € __________<br />
I will be attending the General Meeting.<br />
Family name and given name<br />
Street address<br />
Postal code and city<br />
Contact/Phone/E-Mail<br />
Date and signature<br />
Hotel reservations<br />
BDIZ <strong>EDI</strong> has secured a contingent of Superior<br />
rooms at the Sofitel Munich Bayerpost hotel for<br />
the participants of the symposium. Participants<br />
are requested to make their own reservations,<br />
mentioning “BDIZ <strong>EDI</strong>” at the time of booking:<br />
Sofitel Munich Bayerpost<br />
Bayerstraße 12, 80335 München, Germany<br />
Phone: +49 89 59948-3000<br />
Fax: +49 89 59948-1000<br />
h5413@sofitel.com<br />
Superior room per night, including breakfast<br />
€ 165.00
YOU’RE THE ONE<br />
I’M AFTER<br />
Innovative German high performance implant system seeks discerning user for<br />
successful permanent relationship. My ideal partner values an exceptionally<br />
strong prosthesis interface, excellent osseointegration, top German quality<br />
at an affordable price, and a wide range of prosthetic components for all<br />
conventional indications. If you too are seeking to forge links on a foundation<br />
of titanium prosthetic components, BEGO cobalt-chrome alloy Wirobond ® MI<br />
and BeCe zirconium for example, drop me a line. I look forward to getting to<br />
know you.<br />
Curious? Meet me at bego-implantology.com<br />
Should you wish, I can also visit you.
14<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Friday, 15 October, 10:00 am<br />
Getting Ready for Success with Jörg Löhr<br />
Jörg Löhr Erfolgstraining, founded in 1995, is considered the leading provider of seminars on success, motivation and personality<br />
in the German-speaking area. This company, owned by “Europe’s most sought-after success and personality coach”, claims as<br />
its mission to support people in all wakes of life in developing their full potential.<br />
Löhr’s coaching clients include top athletes and<br />
national sports teams as well as well-known business<br />
corporations such as Allianz, Arcor, BASF, BMW,<br />
IBM, Daimler, Deutsche Telekom, L’Oréal, Oracle, SAP<br />
and numerous major German financial institutions.<br />
In recent years, Jörg Löhr has received several<br />
awards for his ability to combine the transfer of solid<br />
knowledge with his talent to inspire. In 2006, he was<br />
accepted into the Speakers’ Hall of Fame in recognition<br />
of his lifetime achievements. As an athlete, he<br />
had played on the national handball team 94 times,<br />
Friday, 15 October, 9:00 pm<br />
winning the European and German cups and multiple<br />
German championships.<br />
He was a business consultant, owns several companies<br />
and is a bestselling author. Today he is considered<br />
one of the foremost speakers in Europe.<br />
Jörg Löhr has made the methodology he developed,<br />
and his own motivation and inspiration, the<br />
focus of his own professional life. His seminars invariably<br />
incorporate the most recent research, the results<br />
of which he disseminates not only as a speaker but<br />
also as a lecturer at the University of Augsburg.<br />
“Edmund Stoiber”: Explaining the World<br />
to Oral Implantologists<br />
The much-parodied former prime minister of Bavaria, Edmund Stoiber, as impersonated by political satirist Wolfgang Krebs,<br />
will be talking to the people, as impersonated by the attendees of the BDIZ <strong>EDI</strong> Symposium. Krebs, born in 1966, performed<br />
on stage for the first time when he was only five years old. During his school years, he was active in student and local theatre<br />
groups. Since 1988 Krebs has been performing, on and off, as a speaker in various radio plays.<br />
Having attended comprehensive acting workshops in<br />
Berlin and in London, where he obtained his actor’s<br />
licence, Wolfgang Krebs has been present on Bavarian<br />
TV, impersonating the Bavarian prime minister<br />
ostensibly commenting aspects of a popular satirical<br />
show – and not only him, but also other well-known<br />
figures in regional politics, including the current<br />
holder of the Bavarian prime minister office, Horst<br />
Seehofer.<br />
Wolfgang Krebs’ satirical stage performances have<br />
also been highly acclaimed, as have his impersonations<br />
of a mail carrier-cum-voice imitator claiming<br />
to present greetings from Chancellor Angela Merkel<br />
and other well-known people in German public life.<br />
He gained the attention of a broader public when<br />
he went so far as to impersonate Edmund Stoiber in<br />
mock interviews to the German national press in the<br />
context of the 2005 coalition talks.<br />
He is also the author of a children’s book entitled<br />
Star journeys: seven dream journeys for children and<br />
the patron of a project called Secret Matter Porcupine,<br />
a violence prevention programme for children<br />
and adolescents founded in 1998 by fellow actor<br />
Olaf Krätke.<br />
Jörg Löhr<br />
Wolfgang Krebs
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
The programme on 15 and 16 October 2010<br />
Introduction<br />
Christian Berger<br />
Prof Joachim E.<br />
Zöller<br />
Meeting challenges – this motto for our 14 th BDIZ <strong>EDI</strong><br />
Symposium in Munich is important for the dental<br />
office – in terms of professionalism and in terms of<br />
politics. The overall healthcare politics framework<br />
will result in selective reimbursement agreements in<br />
statutory and private health insurance alike. How<br />
does our profession react to this and other challenges<br />
associated with the various fee schedules?<br />
Add to that the challenges we are facing in our professional<br />
work. Reports about implantological successes<br />
are one, shiny, side of the coin. What does the<br />
other side look like? The 14 th BDIZ <strong>EDI</strong> Symposium in<br />
Munich will help you find out. I am looking forward<br />
to seeing you there!<br />
Christian Berger, President BDIZ <strong>EDI</strong><br />
Managing complications in oral implantology<br />
requires a thorough understanding of the biological<br />
situation and many years of clinical experience. Experienced<br />
practitioners and representatives of the academic<br />
world want to share their knowledge with you.<br />
The 4 th European Consensus Conference of BDIZ <strong>EDI</strong><br />
has made one important step in the right direction<br />
by developing its clinical guidelines on complications.<br />
In Munich we will add new dimensions to this<br />
topic: we will be reviewing medications, immediate<br />
placement procedures, soft-tissue management, bone<br />
augmentation, sinus lifts and high-quality ceramic<br />
restorations. Don’t miss Munich!<br />
Prof Joachim E. Zöller, Scientific Director<br />
BDIZ <strong>EDI</strong> would like to extend its sincere thanks to the<br />
following sponsors:<br />
Gold sponsor: Silver sponsors:<br />
15
16<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Friday, 15 October 2010<br />
Pre-congress Programme<br />
7:30 am – 12:30 pm CBCT course CBCT course in radiation protection in dentistry (Part 1)<br />
pursuant to Sect. 18a para. 1 of the German x-ray ordinance<br />
Prof Joachim E. Zöller/Dr Jörg Neugebauer<br />
8:00 am – 10:00 am Workshop 1 Preoperative planning and treatment of implantological and<br />
bredent medical prosthodontic complete rehabilitation cases<br />
Dr Michael Weiss, Ulm, Germany<br />
8:00 am – 10:00 am Workshop 2 New avenues in fixed implant superstructures<br />
Camlog Dr Martin Gollner, Bayreuth, Germany<br />
8:00 am – 10:00 am Workshop 3 Cerec meets Galileos – simultaneous prosthetic and<br />
Sirona Dental surgical implant planning<br />
Dr Lutz Ritter<br />
Friday, 15 October 2010<br />
Getting Ready for Success in the Dental Office<br />
for dentists and dental assistants<br />
10:00 am – 10:05 am Welcome and introduction<br />
Christian Berger, President BDIZ <strong>EDI</strong><br />
10:05 am – 12:15 pm Success and motivation for the dental office<br />
Jörg Löhr, motivational trainer, Augsburg, Germany<br />
12:15 pm – 1:00 pm Buffet lunch · Dental exhibition visit<br />
Friday, 15 October 2010<br />
Programme for Dental Assistants<br />
“Getting ready for success in the dental office” is also a part of the programme for dental assistants.<br />
1:00 pm – 2:00 pm Accounting problems – Dealing with health insurance funds<br />
Dr Thomas Ratajczak, Sindelfingen, Germany<br />
2:00 pm – 3:00 pm Advise, convince, inspire: Toward successful patient information<br />
Dr Dirk Duddeck, Cologne, Germany<br />
3:00 pm – 3:30 pm Break · Dental exhibition visit<br />
3:30 pm – 4:30 pm Reprocessing surgical instruments<br />
Marina Nörr-Müller, Munich, Germany<br />
4:30 pm – 5:30 pm GOZ: Capitalizing on chances – avoiding errors<br />
Dr Stefan Liepe, Hannover, Germany
18<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Friday, 15 October 2010<br />
Quo Vadis, GOZ? Health Politics Forum<br />
1:00 pm – 1:05 pm Welcome and introduction<br />
Christian Berger, President BDIZ <strong>EDI</strong><br />
1:05 pm – 1:15 pm Welcoming address by the Bavarian State Minister of Science, Research and Art<br />
Dr Wolfgang Heubisch, Munich, Germany<br />
1:15 pm – 2:00 pm Whither healthcare policy?<br />
Prof Johann Eekhoff, Institute of Economic Policy, University of Cologne, Germany<br />
2:00 pm – 2:30 pm Financial viability of the German health insurance system<br />
Dr Thomas Drabinski, Institute for Micro-Data Analysis (IfMDA), Kiel, Germany<br />
2:30 pm – 3:00 pm Sufficient, appropriate, economical: Will dental care continue to be funded<br />
by statutory health insurance?<br />
Peter Knüpper, solicitor, Managing Director of the Bavarian Chamber of Dentists<br />
3:00 pm – 3:15 pm Discussion<br />
3:15 pm – 3.45 pm Break · Dental exhibition visit<br />
3:45 pm – 4:15 pm Future funding for dental services: Selective agreements?<br />
Wolfgang Reif, Member of the Board of the Bavarian State Committee<br />
for private health insurance, Munich, Germany<br />
4:15 pm – 4:45 pm Implementing the HOZ schedule of fees in the dental practice<br />
Michael Schwarz, President, Bavarian Chamber of Dentists, Bernau, Germany<br />
4:45 pm – 5:15 pm Quo vadis, GOZ?<br />
Dr Thomas Ratajczak, specialist attorney for social law, specialist attorney for medical law,<br />
BDIZ <strong>EDI</strong> legal adviser, Sindelfingen, Germany<br />
5:45 pm – 6:00 pm Final discussion<br />
Host: Christian Berger<br />
Friday, 15 October 2010<br />
Gala Night<br />
8:00 pm Gala Night at the Lenbach<br />
(Tapestry Room)<br />
Dining, music and political satire<br />
The gala night will take place at the Lenbach.
Nobel Biocare
20<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Saturday, 16 October 2010<br />
Meeting Challenges in Oral Implantology –<br />
Scientific Day<br />
Note: Simultaneous interpretation of the scientific presentations will be available.<br />
8:30 am – 8:45 am Welcome and introduction<br />
Christian Berger, President BDIZ <strong>EDI</strong><br />
Prof Joachim E. Zöller, Scientific Director<br />
8:45 am – 9:15 am Can medications influence implantological success?<br />
Dr Jörg Neugebauer, Cologne, Germany<br />
9:15 am – 9:45 am Template-guided implant insertion: What resources are required?<br />
Dr Achim Nickenig, Cologne, Germany<br />
9:45 am – 10:15 am Guided surgery: Prosthetic results by simple means<br />
Prof Rolf Ewers, Vienna, Austria<br />
10:15 am – 10:30 am Discussion<br />
10:30 am – 11:00 am Break · Dental exhibition visit<br />
11:00 am – 11:30 am Building bone – but how?<br />
Dr Stefan Reinhardt, Münster, Germany<br />
11:30 am – 12:00 noon Sinus floor elevation: More complications than benefits?<br />
Prof Peter Tetsch, Münster, Germany<br />
12:15 pm – 2:00 pm Break · Dental exhibition visit<br />
BDIZ <strong>EDI</strong> General Meeting<br />
2:00 pm – 2:30 pm Immediate placement of implants without augmentation: Successes and problems<br />
Dr Frank Kistler, Landsberg, Germany<br />
2:30 pm – 3:00 pm What parameters determine success in the aesthetic zone?<br />
Prof Germán Gómez-Román, Tübingen, Germany<br />
3:00 pm – 3:30 pm Surgical or prosthetic soft-tissue management?<br />
Dr Arndt Happe, Münster, Germany<br />
3:30 pm – 3:45 pm Discussion<br />
3:45 pm – 4:15 pm Break · Dental exhibition visit<br />
4:15 pm – 4:45 pm The importance of bone-preserving surgical techniques for subsequent implantation procedures<br />
Prof Antonio Felino, Porto, Portugal<br />
4:45 pm – 5:15 pm Ceramic chipping – A problem in prosthodontics or a problem in material technology?<br />
Prof Peter Pospiech, Homburg, Germany<br />
4:15 pm – 5:45 pm All-ceramics – Everything simply without metal<br />
Dr Urs Brodbeck, Zürich, Switzerland<br />
5:45 pm – 6:00 pm Final discussion<br />
Host: Prof Joachim E. Zöller, Cologne, Germany<br />
6:00 pm – 7:00 pm CBCT course, Part 1 (continued)<br />
Prof Joachim E. Zöller/Dr Jörg Neugebauer
Keystone
22<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Interview with Prof Joachim E. Zöller on challenges in oral implantology<br />
The Time of Breathtaking<br />
Pictures is over<br />
So far, oral implantology has mostly featured exciting cases, beautiful results and happy patients. But the times are changing –<br />
they have to be. More and more patients opt for high-quality implant treatment – and the more patients are treated, the<br />
more cases we see that do not end with the patient flashing that perfect smile. But who likes to talk about failures or about<br />
intra operative or postoperative complications? BDIZ <strong>EDI</strong> will do so on 16 October 2010, at its 14 th Annual Symposium in Munich.<br />
“Meeting challenges” is the motto – facing failures and complications. And the focus will naturally be on what can be done<br />
to avoid those failures and complications. <strong>EDI</strong> Journal spoke with the scientific director of the symposium and BDIZ <strong>EDI</strong> Vice<br />
President, Prof Joachim E. Zöller, Chairman of the Interdisciplinary Department for Oral Surgery and Implantology and of the<br />
Department of Oral and Maxillofacial Plastic Surgery of the University of Cologne.<br />
Professor Zöller, can you give us an overview of current<br />
challenges in oral implantology?<br />
We are witnessing a time of changes in oral<br />
implantology. 3D diagnostics and, increasingly, CAD/<br />
CAM technologies are gaining ground and will gradually<br />
become standard, at least when it comes to<br />
major locations. Progress is rapid, and universities are<br />
increasingly tasked to provide the appropriate scientific<br />
background and training. At the same time, we<br />
are seeing a restructuring of the implant market,<br />
where some smaller firms offering top-quality products<br />
will continue to gain market share, which will<br />
result in changes in price levels.<br />
The BDIZ <strong>EDI</strong> Expert Symposium in Cologne in February<br />
was the first to address the issue of failures and<br />
complications. The Annual Symposium in Munich in<br />
October will move in the same direction. You have<br />
been responsible for the scientific programmes at<br />
both these events. Why should someone who has<br />
attended Cologne also attend Munich?<br />
Avoiding failures and managing failures is an<br />
important skill for any oral implantologist. We have<br />
reached the point where many experienced speakers<br />
are beginning to talk about their complications. Just<br />
a few years ago, this was still a difficult thing to do.<br />
Everybody just wanted to show off their breathtaking<br />
pictures, which all of us have seen to saturation in<br />
implantological journals. But looking at these pictures<br />
no longer does anything for the experienced<br />
implantologist. Only honest presentations that talk<br />
about successes and problem cases alike will really<br />
teach us something. This is what we were trying to<br />
work on at the Expert Symposium in Cologne this<br />
year, and we will continue in this direction at the<br />
Annual Symposium in Munich in October.<br />
Treatment providers must investigate whether their<br />
patients are in fact eligible for the planned implant<br />
therapy – ahead of time. How much influence can<br />
systemic diseases have on the success or failure of<br />
implant treatment?<br />
This aspect has been insufficiently considered in<br />
recent years. Our patients are getting older, and this<br />
means they will be increasingly likely to suffer from<br />
systemic diseases. This is our most important patient
world innovation<br />
Cleaning – so easy<br />
Now possible:<br />
machine preparation of the fully equipped surgical tray<br />
tiologic © � en<br />
Turnstraße 31 · 75228 Ispringen · Germany · Phone + 49 72 31 / 803-0 · Fax + 49 72 31 / 803-295<br />
www.dentaurum-implants.de · E-Mail: info@dentaurum-implants.de
24<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
group! Systemic diseases have serious repercussions for<br />
the prognosis of implant treatments. I keep wondering<br />
about results where implant success rates of more than<br />
95 percent are claimed for edentulous patients. I would<br />
like to ask the authors of those reports: Were all those<br />
edentulous patients 18 years old? Or did you exclude all<br />
older patients with concomitant diseases? Of course<br />
this effect is particularly pronounced in patients for<br />
whom bone augmentation has been planned. Yet in<br />
these patients, the best augmentation procedure is the<br />
one that is not implemented.<br />
What influence does the choice of materials have –<br />
the “right” implant or the “right” bone replacement<br />
material?<br />
An analysis of the patient population and a major<br />
study we conducted have shown that, as long as the<br />
appropriate protocols are observed, the materials<br />
used have no significant influence on success rates.<br />
Unfortunately, many oral implantologists have<br />
become almost addicted to discussing materials here<br />
and properties there. But patient selection, the physiology<br />
of wound healing and, most of all, operator<br />
skills are much more important.<br />
Nerve injuries must be included among the serious treatment<br />
errors. Is there any reliable method to avoid them?<br />
Many experts have shown us that, while nerve<br />
injury may be due to inferior surgical techniques, its<br />
main cause will generally be inappropriate treatment<br />
planning. Cases abound where the operator deviates<br />
from the treatment plan intraoperatively because of<br />
unpleasant surprises during implant insertion, such<br />
as an insufficient supply of transversal bone. To avoid<br />
augmentation, implants are frequently inserted too<br />
deeply in these cases.<br />
Your department performs sophisticated and demanding<br />
procedures such as bone augmentation. At the<br />
Expert Symposium, one of the speakers – Prof Khoury –<br />
said that there is no augmentation without complication.<br />
What will be your focus at the 14 th BDIZ <strong>EDI</strong> Annual<br />
Symposium when it comes to bone augmentation?<br />
Complications may occur during any type of augmentation<br />
surgery. How frequent they are depends<br />
both on the procedure and on the operator. The<br />
greater the amount of allogenous material, the higher<br />
the infection rate. It is therefore important to do<br />
with as little alloplastic material as possible. At this<br />
point, the transplantation of autogenous vital bone<br />
is still the most valuable procedure from a biological<br />
point of view, with the lowest infection rates.<br />
What is the relative importance of immediate implant<br />
insertion procedures today? The European Consensus<br />
Conference 2006 had developed pertinent guidelines.<br />
Have we had new insights regarding materials and<br />
procedures since?<br />
The “fad” of immediate insertion surgery has subsided<br />
somewhat as more complications are seen –<br />
as many operators have been disappointed to learn.<br />
With the exception of the mandibular intraforaminal<br />
region, the relevant criteria have not been firmly<br />
established. I believe that immediate insertion is<br />
rarely indicated for the average patient at this time.<br />
I am sure these patients prefer safe, low-risk implant<br />
procedures and will opt for the lengthier but more<br />
successful treatment once properly informed.<br />
Implantation and augmentation procedures often<br />
compromise the soft tissues. What possibilities do we<br />
have today to avoid complications in this area?<br />
Next to augmentation and implantation, the<br />
important third element of success is soft-tissue surgery.<br />
The operator must determine whether a special<br />
soft-tissue technique is required as early as during<br />
reentry. If peri-implantitis manifests itself later,<br />
vestibuloplasties will often fail to deliver the desired<br />
result, and the peri-implantitis and the associated<br />
bone loss will proceed. When exposing implants following<br />
bone augmentation, special soft-tissue management<br />
techniques are required. Apically repositioned<br />
flaps play an important role. The flap, when<br />
created correctly, will not only create a zone of periimplant<br />
attached gingiva 2 to 3 mm in height, but<br />
it will allow the operator to shape the vestibulum<br />
again.<br />
Well, that really arouses our curiosity as to the scientific<br />
day in Munich. Professor Zöller, thank you very<br />
much for this interview.<br />
AWU
XiVE ®<br />
:<br />
Implantology Unlimited<br />
Superior surgical and prosthetic versatility<br />
Outstanding primary stability<br />
even in soft bone<br />
Successful in even the narrowest gaps<br />
with XiVE ®<br />
3.0<br />
Immediate implant restoration<br />
due to the integrated TempBase concept<br />
Greatest possible prosthetic variety<br />
valued worldwide<br />
Discover your implantological freedom with XiVE ®<br />
.<br />
http://xive.dentsply-friadent.com<br />
Implantology Unlimited<br />
AZ_XiVE_3mm_A4_en.indd 1 15.06.2010 14:40:01 Uhr
26<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
14 th BDIZ <strong>EDI</strong> European Committee meeting in Cologne<br />
European Curriculum<br />
under Development<br />
European issues play an important role in the day-to-day work of BDIZ <strong>EDI</strong>. That the partner associations are<br />
keenly interested in this work is underscored by their regular attendance at the BDIZ <strong>EDI</strong> European Committee<br />
meetings. The topic in Cologne last February was the common European curriculum.<br />
Participants this year included Prof Hakan Özyuvaci<br />
(Istanbul) for Turkey, Dr Philip Bennett (Lyme Regis) for<br />
our British partner association ADI, Prof Andrzej Wojtowicz<br />
(Warsaw) and Dr Christoph Sliwowski for our<br />
Polish partner association OSIS <strong>EDI</strong>, Prof Vitomir Kons -<br />
tantinovic (Belgrade), Dr Zoran Marjanovic (Novi Sad)<br />
and Dr Dusan Vasiljevic for our Serbia-Montenegro<br />
partner association, Prof Bernhard Broos (Villach), who<br />
represented Austrian implantologists, and Dr Peter A.<br />
Ehrl (Berlin), who organizes the Greek-German Curriculum<br />
for BDIZ <strong>EDI</strong>. On the part of BDIZ <strong>EDI</strong> itself, participants<br />
included Christian Berger, Dr Detlef Hildebrand,<br />
Dr Jörg Neugebauer and Dr Dirk Duddeck, Anita Wuttke,<br />
Dr Thomas Ratajczak as secretary and Dr Stefan Liepe.<br />
Ralf and Angelika Suckert were present in the capacity<br />
of publishers for BDIZ <strong>EDI</strong> konkret and <strong>EDI</strong> Journal.<br />
Qualification and comparability<br />
The most important point on the agenda was the<br />
European curriculum that the partner associations<br />
want to join forces to initiate. The meeting discussed<br />
suggestions by Dr Ehrl and Dr Neugebauer (who is the<br />
organizer of the BDIZ <strong>EDI</strong> Curriculum Implantology).<br />
Dr Neugebauer pointed out that even within Germany<br />
there is a number of different curricula with considerable<br />
variation with respect to the quality of the syllabus.<br />
The BDIZ <strong>EDI</strong> curriculum is considered to be particularly<br />
highly developed. BDIZ <strong>EDI</strong> President Christian<br />
Berger thanked both speakers and pointed out the<br />
importance of reaching comparable standards for the<br />
curriculum throughout all the different countries. Each<br />
of the partner organizations is now tasked to evaluate,<br />
on a national level, what additional modules could be<br />
helpful to ensure comparable entry skills and qualifications<br />
throughout Europe. The committee members<br />
then discussed the current status of curriculum development,<br />
which differs considerably across different<br />
countries. The committee agreed that qualified pre-<br />
senters and a comparable syllabus both within participating<br />
countries and on a European level are a<br />
prerequisite for creating a European curriculum.<br />
Individual countries<br />
Dr Phil Bennett outlined the new e-learning program<br />
that the British ADI had initiated, teaching implantological<br />
basics to prospective implant dentists. Prof<br />
Andrzej Wojtowicz announced an international twoday<br />
symposium of Polish oral and maxillofacial surgeons<br />
in May and a broad-based multi-country Eastern<br />
European symposium in 2011. Prof Vitomir Konstantinovic<br />
reported on developments in oral implantology in<br />
Serbia. The Serbian association of oral and maxillofacial<br />
surgeons will be holding a major symposium in Belgrade<br />
in the autumn of 2010. Konstantinovic asked for<br />
BDIZ <strong>EDI</strong> support in the shape of the delegation of<br />
qualified speakers. He also suggested organizing major<br />
multicenter studies using uniform study protocols<br />
throughout Europe.<br />
Toward the end of the meeting, Ralf Suckert gave<br />
an overview of e-learning and e-journals at teamwork<br />
media – not least with iPads in mind, which are<br />
expected to become very popular in the near future.<br />
AWU<br />
The outlines of the European curriculum are beginning to take shape. Representatives<br />
of seven countries engaged in highly constructive discussions.
28<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Successful BDIZ <strong>EDI</strong> continuing-education week in Belek/Antalya<br />
4 th Mediterranean Symposium:<br />
See Turkey and Learn Something<br />
The BDIZ <strong>EDI</strong> Mediterranean Symposium has become a small but highly appreciated event for implant dentists in Europe offering<br />
top-notch training under the auspices of the association – and that far beyond Germany’s borders. Following Montenegro (2007),<br />
Crete (2008) and Vouliagméni (2009), this year’s one-week BDIZ <strong>EDI</strong> continuing-education event was held in May under the<br />
motto of “Avoiding Treatment Errors – Managing Complications” on the “Turkish Riviera” at Belek.<br />
Twelve speakers and fourteen presentations on a<br />
single day left little time to enjoy the sun, the<br />
beach and the sea, the international golf courses<br />
or the comfort of a luxury hotel built in the style of<br />
a Moorish castle. Nevertheless, neither the Turkish<br />
nor the German attendees felt they were missing<br />
anything – the one-day symposium and workshops,<br />
interpreted simultaneously, simply had too<br />
A job well done: BDIZ <strong>EDI</strong> Presidents Prof Joachim E. Zöller<br />
and Christian Berger with Prof Hakan Özyuvaci (centre).<br />
The Kempinski Hotel The Dome was built in the style of a<br />
Moorish castle.<br />
much to offer. The two scientific directors of the<br />
continuing-education week, Prof Joachim E. Zöller<br />
(Cologne) and Prof Hakan Özyuvaci (Istanbul), had<br />
fine-tuned the programme together, arriving at a<br />
delicate composition of topics focusing on complications<br />
in oral implantology, including restorative<br />
issues and sidelines such as mathematics or<br />
anaesthesia.<br />
Before the symposium: Taking a look at the venue,<br />
the Karatay ballroom.
STRAUMANN ® EMDOGAIN<br />
IS TRUE PERIODONTAL REGENERATION<br />
IMPORTANT FOR YOU?<br />
before after<br />
More than 100 clinical publications in peer-reviewed journals demonstrate Straumann ® Emdogain<br />
to be safe and effective in stimulating the formation of new periodontal soft and hard tissue.<br />
These clinical studies involve more than 3000 defects in over 2500 patients.<br />
Excellent clinical results 1,2,3<br />
Clinical long-term benefit 4,5<br />
Improved patient satisfaction 6,7<br />
1 Tonetti et al. J Clin Periodontol 2002;29:317–325<br />
2 Froum et al. J Periodontol 2001;72:25–34<br />
3 McGuire et al. J Periodontol 2003;74:1110 & 1126<br />
4 Heden et al. J Periodontol 2006;77:295–301<br />
5 Sculean et al. Int JPRD 2007;27:221–229<br />
6 Jepsen et al. J Periodontol 2004;75:1150–1160<br />
7 Sanz et al. J Periodontol 2004;726–733
30<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Prof Joachim E. Zöller Prof Hakan Özyuvaci Özcan Yildirim Hilal Kuday<br />
Dr Kerem Dedeoglu Dr Serdar Yalcin Chris tian Berger Dr Atakan Elter<br />
Looking beyond the dental fence<br />
Prof Özyuvaci opened the proceedings by presenting<br />
a classification of complications as preoperative,<br />
intraoperative and postoperative. Some of his illustrations<br />
showed dislocated implants within the maxillary<br />
sinus. Prof Zöller also pointed out the interrelationship<br />
between an aging patient population and<br />
the rising incidence of concomitant systemic diseases.<br />
In addition to local diagnostic findings, he<br />
said, systemic afflictions must always be taken into<br />
account by the treatment concept. His presentation<br />
focused on the importance of the patient’s medical<br />
history, general clinical findings and psychosocial<br />
background in addition to the anatomical situation.<br />
Everybody expects to come home from continuing<br />
education with new ideas to be implemented in clinical<br />
practice. The symposium paid special attention to<br />
dental technology. Dental technician Özcan Yildirim<br />
(Istanbul) explained how present-day dental laboratories<br />
work and demonstrated the differences be -<br />
tween conventional and CAD/CAM restorations in the<br />
production phase. He concluded that the precision<br />
of milled restorations is greater than that of cast<br />
restorations when it comes to wide-span bridges.<br />
Dental technician Hilal Kuday (Istanbul) emphasized<br />
the importance of patient discussions and of paying<br />
attention to the patient’s overall facial features<br />
when introducing high-quality aesthetic anterior<br />
restorations.<br />
Dr Kerem Dedeoglu (Istanbul) spoke about the<br />
importance of getting an accurate patient history,<br />
presenting some case reports to demonstrate the<br />
potential dramatic consequences of incomprehensible<br />
clinical descriptions. Prof Serdar Yalcin (Istanbul)<br />
pointed to possible complications, including implant<br />
loss after immediate insertion, citing a significantly<br />
higher rate of complications following immediate<br />
implant insertion in inflamed regions. Christian Ber -<br />
ger (Kempten) made the connection to endodontics,<br />
referring to a number of clinical cases to demonstrate<br />
that, given the current state of the art and the<br />
currently available treatment options, an endodontically<br />
treated tooth may well be the better implant.<br />
Aesthetics and mathematics<br />
What does aesthetic dentistry have to do with mathematics?<br />
Quite a lot, Dr Atakan Elter (Istanbul) thinks.<br />
Nature, human beings in general and the human
The new kit for success.<br />
Geistlich Combi-Kit Collagen – the best kit<br />
for successful and predictable results in ridge<br />
preservation and minor augmentations.<br />
Geistlich<br />
Bio-Oss ® Collagen and<br />
Geistlich Bio-Gide ®<br />
From May 2010<br />
combined in Geistlich<br />
Combi-Kit Collagen<br />
www.geistlich-pharma.com LEADING REGENERATION
32<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Prof Vitomir Konstantinovic Dr Holger Janssen Dr Jörg Karst<br />
Dr Detlef Hildebrand<br />
mouth in particular are governed by the golden ratio<br />
linking the principles of symmetry and asymmetry.<br />
The golden ratio, which has often been called the<br />
divine proportion, is a mathematical constant that<br />
can be derived from, and be used in, dental aesthetics.<br />
For example, this constant phi (oI = 1,6180339887...)<br />
can manifest itself in the relationship between the<br />
length and the width of the tooth. Although the<br />
golden ratio is an oft-cited topic in dental aesthetics,<br />
the attendees in Belek were once again fascinated by<br />
this irrational mathematical ratio that is considered<br />
particularly harmonious and beautiful – whether in<br />
architecture or in present-day dentistry.<br />
Nerve injury and bone augmentation<br />
From aesthetics, the focus returned to the depth of<br />
the maxillary sinus – which is the realm of Prof Joa -<br />
chim E. Zöller. In his second presentation he illustrated<br />
the importance of a correct diagnosis before any<br />
implantological procedure in order to prevent nerve<br />
injury and enumerated the therapeutic guidelines to<br />
be applied. A typical nerve injury he cited was the<br />
damage sometimes caused by a casual injection.<br />
Experience has shown that the inferior alveolar nerve<br />
hardly ever ruptures – not even in the event of a<br />
mandibular fracture. On the other hand, the nerve is<br />
highly susceptible to damage by pointed or sharp<br />
instruments, being more sensitive to pressure than to<br />
tension. His advice was to “keep the tweezers away”.<br />
Zöller also discussed augmentation and the associated<br />
risks. He made clear that the use of autologous<br />
bone material was the most valuable procedure from<br />
a biological point of view. Bone replacement material<br />
should be reserved for sinus lift procedures or collateral<br />
augmentation of defects.<br />
Meeting before the background of the Mediterranean scenery: Speakers, organizers and some participants meeting on the roof terrace of the<br />
Kempinski Hotel The Dome in Belek to exchange impressions and ideas after a demanding symposium. Some of the people in this picture:<br />
Christian Berger (front left), Prof Joachim E. Zöller (centre), Anita Wuttke (BDIZ <strong>EDI</strong>, European matters) and Prof Hakan Öyzuvaci; Dr Holger<br />
Janssen (far right), Prof Vitomir Konstantinovic; Dr Jörg Karst and Dr Detlef Hildebrand (behind them, right).
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Prof Vitomir Konstantinovic (Belgrade) took the<br />
audience “back to the surface” by presenting safe<br />
treatment concepts in oral implantology, especially<br />
the two-stage procedure. Dr Holger Janssen (Berlin)<br />
explained in his presentation on the prevention of<br />
prosthetic errors that the static concept of occlusion<br />
is increasingly giving way to a dynamic and functional<br />
concept where the teeth are being treated as sensitive<br />
receptors for the brain.<br />
General anaesthesia – yes or no?<br />
The risks and benefits of general anaesthesia in the<br />
context of dental surgery were the topic of anaesthesist<br />
Dr Jörg Karst (Berlin). He explained that general<br />
anaesthesia may be indicated for high-risk patients<br />
and protracted procedures, as today’s anaesthetic<br />
methods are becoming increasingly safer. Dr Detlef<br />
Hildebrand (Berlin) presented guided surgery procedures,<br />
the Robodent system and stent-guided instrument<br />
navigation, showing that precise planning and<br />
accurate implementation helps avoid complications.<br />
Conclusion<br />
In his closing message, Prof Zöller concluded that the<br />
continuing-education week, which after the symposium<br />
itself continued with industry workshops and<br />
interactive training on complications, had reached a<br />
very high level internationally: “We have seen excellent<br />
presentations by Turkish and German speakers<br />
that were characterized by a high level of scientific<br />
expertise, beautifully complementing each other in<br />
the issues they addressed and the conclusions they<br />
arrived at.” BDIZ <strong>EDI</strong> President Christian Berger also<br />
took positive stock of the event, thanking the Turkish<br />
partner of BDIZ <strong>EDI</strong>, Prof Hakan Özyuvaci, and his<br />
team for organizing it. Similar to the continuingeducation<br />
week in Greece the previous year, this<br />
year’s event on the Turkish Mediterranean coast was<br />
characterized by a vivid exchange of ideas between<br />
the speakers and the Turkish and German audience,<br />
supporting the mission of BDIZ <strong>EDI</strong> of promoting<br />
high standards of quality in oral implantology and<br />
working for establishing uniform implantological<br />
standards throughout Europe.<br />
AWU<br />
Thanking our sponsors<br />
BDIZ <strong>EDI</strong> thanks its sponsors for their support of<br />
its continuing-education event: Sirona Dental,<br />
Geistlich Biomaterials, Dentsply Friadent, Camlog<br />
and Straumann.<br />
33<br />
A-DE10001<br />
Aesculap ® Dental<br />
Bone Fixation<br />
Easy Handling – Excellent Results<br />
Bone Fixation Forceps:<br />
❚ Delicate and adaptable working tips<br />
❚ Universal application ➠ upper and lower jaw<br />
Screws:<br />
❚ Highest stability<br />
❚ Smallest possible screw head<br />
❚ Biocompatible<br />
❚ Easy removal of residues<br />
Aesculap AG | Am Aesculap-Platz | D-78532 Tuttlingen | Germany<br />
Phone +49 7461 95-2496 | Fax +49 7461 78980<br />
eMail dental@aesculap.de | www.aesculap-dental.com
34<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
12 th BDIZ <strong>EDI</strong> Curriculum Implantology to start in November 2010<br />
Top-level Implantological Training<br />
“Practical exercises on human specimens and a relaxed and congenial atmosphere helped make this Curriculum a success.<br />
The hands-on workshops were excellently prepared, and the content of the course was immensely better than that offered by<br />
other providers.” These and similar observations were heard from attendees of the 11 th Curriculum Implantology, who had success-<br />
fully mastered their first step on the way to Certified Expert in Oral Implantology status. Participants appreciated the agenda<br />
itself, but also the selection of speakers and the fact that a significant part of the Curriculum consisted of practical exercises.<br />
The organizers received special praise for fostering an atmosphere of open exchange of discussions, both within the group of<br />
participants and with the speakers and presenters. No questions remained unanswered, and each speaker shared his or her<br />
own personal views on a variety of topics covering the entire field of oral implantology.<br />
The BDIZ <strong>EDI</strong> Curriculum Implantology appeals not<br />
only to young dentists and to newcomers to oral<br />
implantology, but the modular design of the Curriculum<br />
makes it particularly interesting to dentists who<br />
perform implant surgery only occasionally but want<br />
to make sure their treatment rests on solid ground.<br />
The Curriculum allows its successful graduates to<br />
master even difficult indications and to address<br />
potential complications successfully.<br />
Important criteria<br />
The BDIZ <strong>EDI</strong> Curriculum Implantology can look back<br />
on a long history. Since the Curriculum series was<br />
inaugurated in 2004, more than 270 attendees have<br />
participated in the Curricula held in Cologne and on<br />
Fuerteventura. But it is not the numbers alone that<br />
indicate the success of these Curricula. In addition<br />
to the Curriculum’s overall approach, which is scientifically<br />
sound and at the same time eminently practical<br />
in outlook, it is the modular design that attracts<br />
many new members to this form of continuing edu-<br />
”Practical exercises on human specimens and a relaxed<br />
and congenial atmosphere helped make this Curriculum<br />
a success.” (Dr W. Greeven)<br />
”The hands-on workshops were excellently prepared,<br />
and the content of the course was immensely better<br />
than that offered by other providers.” (M. Mariusz)<br />
“I particularly appreciated the many live operations<br />
and the fact that many different speakers partici -<br />
pated.” (Dr W. Rizza)<br />
12 th Curriculum Implantology agenda<br />
25/26 Nov 2010 1. Basics of oral implantology<br />
21/22 Jan 2011 2. Treatment planning and diagnosis<br />
21/22 Feb 2011 3. Surgical techniques<br />
17/18 Mar 2011 4. Prosthetics<br />
07/08 Apr 2011 5. Augmentation 1 – Regional bone augmentation<br />
12/13 May 2011 6. Soft-tissue management<br />
26/27 May 2011 7. Augmentation 2 – Remote autologous bone grafts<br />
14/15 July 2011 8. Recall and complications<br />
cation. Continuing-education modules successfully<br />
completed with other organizations than BDIZ <strong>EDI</strong><br />
may be transferred to the Curriculum for credit –<br />
saving time and money.<br />
Practical training is an important aspect<br />
Six years since its inception, the continuing-education<br />
series entitled “Curriculum Implantology” finds<br />
its proven overall concept unchanged. Quality beats<br />
No questions<br />
remain<br />
unanswered.
36<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
The BDIZ <strong>EDI</strong> Curricula are characterized by a considerable share of practical instruction.<br />
quantity – open training sessions for a limited number<br />
of participants in the Curriculum units and a<br />
sizable percentage of practical instruction take<br />
precedence over “accommodating the masses”.<br />
Attendees particularly appreciate the surgical exercises<br />
on human specimens that make for realistic<br />
hands-on workshops. These practical units are an<br />
integral part of the Curriculum. Human specimens<br />
provided by the Anatomical Institute of the University<br />
of Cologne are prepared for participants at different<br />
stages and tissue levels. This promotes threedimensional<br />
orientation, facilitating close study of<br />
the various structures worthy of preservation. Participants<br />
gain a greater understanding of the complications<br />
that may accompany sinus lift procedures, helping<br />
them avoid uncontrollable situations.<br />
“The practical workshops train skills that support<br />
sophisticated treatment approaches and facilitate<br />
meaningful treatment in complex cases or in the<br />
event of complications”, says Prof Joachim E. Zöller,<br />
who, besides serving as Vice President of BDIZ <strong>EDI</strong>, is<br />
the director of the Department of Oral, Maxillary and<br />
Plastic Facial Surgery and the Interdisciplinary Clinic<br />
for Oral Surgery and Implantology of the University<br />
of Cologne and has been the scientific director of the<br />
Curriculum Implantology of BDIZ <strong>EDI</strong> since its inauguration<br />
in 2004. The team of instructors around<br />
Zöller is supported by speakers who are dentists in<br />
private practice, as the treatment concept practiced<br />
at the University Hospital in Cologne cannot cover<br />
the entire bandwidth of indications, patients and<br />
dental offices. The Curricula strive to present the<br />
entire range of possible implantological treatment<br />
approaches, allowing the participants to decide<br />
freely what treatment concept they deem best for<br />
their own situation. The individual Curriculum building<br />
blocks offered, for example, at the Expert Congress<br />
on Fuerteventura, have magnetically attracted<br />
participants. The reason is that sophisticated training<br />
units in small groups with plenty of available time<br />
are highly attractive. As Christian Berger explains the<br />
concept: “A generous share of hands-on practical<br />
exercises has been included, making it easy for beginners<br />
to take the first steps and offering more experienced<br />
dentists a way to enlarge their practical armamentarium.”<br />
“What I particularly liked about the BDIZ <strong>EDI</strong> Curriculum<br />
was of course the live surgery units but also the<br />
congenial atmosphere and the high level of competence<br />
exhibited by the speakers.” (I. Lell)<br />
“Experienced colleagues reported on their own mistakes<br />
and taught us how to avoid them.” (Dr K. Tolk)<br />
“I felt very positive about the chronological structure<br />
and the practical exercises. I can only recommend other<br />
dentists to take this course.” (O. Becker)<br />
The 12 th BDIZ <strong>EDI</strong> Curriculum Implantology will take<br />
off on Thursday, 25 November 2010. A few vacancies<br />
are still available. Details on the Curriculum can be<br />
found online at www.bdizedi.org (select English and<br />
click “Education“). For information by phone call please<br />
call the BDIZ <strong>EDI</strong> office at +49 228 9359-244.<br />
DUD<br />
Contact Address<br />
Dr Dirk U. Duddeck<br />
Interdisciplinary Policlinic for Oral Surgery<br />
and Implantology<br />
Department of Oral and Maxillofacial Plastic Surgery<br />
University of Cologne<br />
Director: Professor Joachim E. Zöller<br />
Kerpener Straße 32 · 50931 Köln · GERMANY<br />
Phone: +49 221 478-4744 · Fax: -6721<br />
dirk.duddeck@uk-koeln.de
EDA Expert in Implantology<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
37<br />
Successful Exam<br />
Can didate in Cologne<br />
Following the<br />
presentation<br />
and discussion of the case reports<br />
submitted, the three-member<br />
jury was impres sed with the candidate’s<br />
qualifications.<br />
If you, too, are interested in sitting<br />
the certification exam for<br />
EDA Expert in Implantology, you<br />
On the occasion of the 5 th Expert Symposium, Dr<br />
Michael Vogeler of Merzhausen, Germany, success -<br />
fully passed the EDA Expert in Implantology certifi -<br />
cation exam.<br />
Munich, 17 October 2010<br />
will find all the information you<br />
need at the www.bdizedi.org<br />
website (currently in German<br />
only, click “Fortbildung”). The<br />
members of the Cologne examination<br />
board were Per Fossdal,<br />
Christian Berger and Prof Joachim<br />
E. Zöller. AWU<br />
Upcoming EDA Ex pert<br />
in Implantology<br />
Certification Exam<br />
The next certification exam will be held at the 14 th BDIZ <strong>EDI</strong> Symposium<br />
in Munich at the Sofitel Munich Bayerpost on 17 October 2010.<br />
Admission requirements for the<br />
certification exam include:<br />
• 250 EDA-recognized advanced<br />
education/training hours in<br />
various sub-disciplines of<br />
implantology<br />
• Submission of ten documented,<br />
independently performed<br />
im plan tological treatment<br />
cases<br />
• At least five years of professional<br />
activity primarily in the<br />
field of implantology<br />
Specific experience and primary<br />
activity in the field of implantology<br />
must be documented by at<br />
least 400 implants inserted and<br />
150 implants restored within the<br />
past five years. If you would like<br />
to register for the certification<br />
exam, you can receive the requisite<br />
information and registration<br />
documents from the BDIZ <strong>EDI</strong><br />
office in Bonn:<br />
office-bonn@bdizedi.org.<br />
AWU<br />
Q-Implant ®<br />
For all indications,<br />
also for atrophied upper and lower jaw<br />
Atraumatic one-phase concept<br />
Immediate temporisation and<br />
immediate loading possibilities<br />
Easy to follow treatment sequence<br />
Clearly arranged titanium instruments<br />
Microroughness of the implant surface through Surfoss II<br />
Reduced treatment time for both patient and dentist<br />
Minimal cost layout and extreme low storage requirements<br />
Problem-free hygiene accessibility for the patient<br />
Q-MultiTractor<br />
Modular titanium distractor<br />
Innovative pin-base-plate<br />
High stability<br />
Minimally invasive surgery<br />
For upper and lower jaw<br />
Q-Mesh<br />
3-D formed titanium mesh<br />
Convenient handling<br />
Less surgery time<br />
Individual modulation<br />
Applicable to atrophied<br />
maxilla<br />
Q-Implant MARATHON<br />
One-week-intensive-courses in implantology<br />
®<br />
in the Caribbean islands<br />
and Indochina<br />
Four years experience with more than<br />
20.000 inserted implants<br />
This 40-hours course gives the opportunity to intensify theoretical<br />
know-how and to collect practical experience in implantology. Under<br />
supervision of highly skilled surgeons and in cooperation with<br />
generally accepted university clinics.<br />
Training teams will consist of 2-3 participants; each one may insert<br />
30 – 50 implants per week.<br />
Timetable and details available at email:<br />
q-implant-marathon@trinon.com
38<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Visiting Fuerteventura for the 20 th time<br />
International Expert Symposium<br />
for Regenerative Methods in<br />
Medicine and Dentistry<br />
The 20 th International Expert Symposium for Regen-<br />
erative Methods in Medicine and Dentistry will be<br />
held at the Robinson Club Esquinzo Playa on Fuerte -<br />
ventura from 26 October to 4 November 2010.<br />
The realignment at last year’s symposium, with a<br />
clear focus on dental issues and related general medical<br />
treatment options, has been greeted with great<br />
enthusiasm on the part of the attendees. An interesting<br />
and diverse schedule consisting of presentations,<br />
seminars and workshops with practical exercises<br />
allowed speakers and trainers to effectively present –<br />
and attendees to effectively digest – a broad range of<br />
relevant topics.<br />
Innovations and biomaterials<br />
The focus for 2010 will be on “Biomaterials: Innovation<br />
is not limited to the surgical field”. This focus<br />
takes into account the exciting developments of<br />
recent years, with various innovations in dental surgery<br />
and prosthodontics opening up new treatment<br />
options for patients. The use of exogenous materials<br />
frequently allows the reconstruction of lost hard and<br />
soft tissue, creating a wide range of treatment<br />
adjuncts for different indications. Speakers will present<br />
their favorite biomaterials for specific indications<br />
and share their experiences, which in some cases<br />
have been accumulated over decades.<br />
An intensive exchange of thoughts and ideas is<br />
facilitated by the very special networking atmosphere<br />
outside the sessions themselves. The symposium<br />
does not limit itself to presenting innovative<br />
thought. Rather, its main strength is its personal<br />
atmosphere that is highly conducive to interdisciplinary<br />
discussion.<br />
NEU<br />
Speakers on Fuerteventura<br />
MDT Stefan Adler, Landsberg/Lech<br />
Christian Berger, Kempten<br />
Dr Fred Bergmann, Viernheim<br />
Dr Claudio Cacaci, Munich<br />
Prof Rolf Ewers, Vienna<br />
Dr Erni Fuchs, Thalwil<br />
Dr Ulrich Fürst, Attnang<br />
Dr Arndt Happe, Münster<br />
Dr Viktor E. Karapetian, Cologne<br />
Dr Frank Kistler, Landsberg/Lech<br />
Dr Frank Kormann, Oppenheim<br />
Dr Klaus Lotzkat, Hannover<br />
Dr Thea Lingohr, Cologne<br />
Dr Jörg Neugebauer, Cologne<br />
Dr Christoph Niesel, Karlsruhe<br />
Dr Stefan Reinhard, Münster<br />
Dr Daniel Rothamel, Cologne<br />
Gerhard Stachulla, Augsburg<br />
Dr Gerhard Werling, Bellheim<br />
Prof Joachim E. Zöller, Cologne
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
14 th Dentsply Friadent World Symposium<br />
BDIZ <strong>EDI</strong> in<br />
Barcelona<br />
The 14 th Dentsply Friadent World Symposium 2010 took place in<br />
Dr Werner Groll, CEO and Vice President<br />
of Dentsply Friadent, had<br />
promised that the symposium<br />
was going to present knowledge<br />
and skills revolving around the<br />
dental office. Getting dental<br />
offices ready for the future – even<br />
in economically difficult times –<br />
was the objective of the Barcelona<br />
event. One hundred renowned<br />
speakers and a program and discussion<br />
forums spanning a wide<br />
range of topics implemented the<br />
guidelines issued by the symposium’s<br />
scientific directors, Prof<br />
Heiner Weber (Tübingen), Dr Henry<br />
Salama (Atlanta) and Prof Lim<br />
39<br />
Barcelona with 2,500 participants from all over the world attending.<br />
BDIZ <strong>EDI</strong> had its own booth – and the two days were an all-around<br />
success: Great networking, many international contacts and plenty<br />
of new subscriptions for the <strong>EDI</strong> Journal. All the sample issues were<br />
completely gone as early as halfway through the second day.<br />
Kwong Cheung (Hongkong). The<br />
hands-on workshops on augmentation<br />
techniques and soft-tissue<br />
management were completely<br />
sold out.<br />
The 14 th Dentsply Friadent<br />
World Symposium was a huge<br />
public forum for dentists from a<br />
host of different countries. The<br />
BDIZ <strong>EDI</strong> booth got inquiries from<br />
the Middle East and from Asia as<br />
well as from all parts of Europe<br />
and the Americas – which goes to<br />
show that an international multiday<br />
meeting is a highly attractive<br />
event.<br />
AWU<br />
BDIZ <strong>EDI</strong> and DGOI representatives in Barcelona – BDIZ <strong>EDI</strong> President Christian<br />
Berger and DGOI President Dr Georg Bayer (right) with DGOI Secretary General<br />
Karl-Heinz Glaser (left).<br />
Û MECTRON<br />
PIEZOSURGERY®<br />
THE THIRD<br />
GENERATION OF<br />
THE ORIGINAL<br />
Û NEW PIEZOSURGERY® 3 –<br />
FASTER, EASIER, MORE PRECISE!<br />
mectron s.p.a., via Loreto 15/A, 16042 Carasco (Ge)<br />
ITALIA, tel +39 0185 35361, fax +39 0185 351374<br />
www.mectron.com, mectron@mectron.com
40<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Belgrade, 27 to 29 October 2010<br />
International Congress for<br />
Maxillofacial Surgery<br />
The International College for Oral Maxillo-Facial Surgery (ICMFS) will be holding its 25 th international annual<br />
congress in Belgrade. This major event will be held jointly with the Serbian Association of Maxillofacial<br />
Surgeons, addressing a broad range of topics presented by international speakers.<br />
Attendees will have the opportunity to learn more<br />
about current and future developments in maxillo -<br />
facial surgery and its various fields such as traumatology,<br />
oncology, reconstructive and plastic surgery,<br />
distraction osteogenesis, craniofacial deformations,<br />
implant surgery etc. In his online welcoming address,<br />
Congress President Nebojsa Jovic explains that the<br />
event is directed at international participants, which<br />
is reflected by the list of keynote speakers that also<br />
includes German speakers.<br />
Seville, 25 to 27 November 2010<br />
BDIZ <strong>EDI</strong> offers this major event in Belgrade its<br />
moral and practical support in the form of a panel<br />
of speakers. Contact between BDIZ <strong>EDI</strong> and ICMFS<br />
has been established via Prof Vitomir Konstantinovic,<br />
who is one of the organizers of the congress. Kons -<br />
tantinovic is Professor for oral and maxillofacial surgery<br />
at the University of Belgrade and has been a<br />
presenter at several recent BDIZ <strong>EDI</strong> symposia. For<br />
more information, please consult the ICMFS website<br />
at www.icmfs2010.org. AWU<br />
18 th International<br />
SEI Convention in Spain<br />
The Spanish Congress of Oral Implantologists (Sociedad Española de Implantes, SEI) will be holding its<br />
25 th National and 18 th International Annual Convention in Seville, Spain, from 25 to 27 November 2010.<br />
From the very beginning, SEI conventions have ad -<br />
dressed interdisciplinary issues. For three days, inter -<br />
national experts will be presenting clinical cases and<br />
scientific and technical innovations. The convention<br />
will be held at the Melia Lebreros hotel in Seville and<br />
will be hosted by Dr Araceli Morales Sánchez, President<br />
of SEI, which is a partner association of BDIZ <strong>EDI</strong><br />
and an affiliate of the ICOI. Additional support will<br />
be provided by the Seville Chamber of Dentists and<br />
local and regional government bodies.<br />
Seville is not only a distinguished convention<br />
venue – it is also famous for its rich history. Its enormous<br />
cathedral, one of the biggest in the world, was<br />
built on the site of Muslim Seville’s main mosque<br />
between 1401 and 1507. One highlight of the cathedral’s<br />
lavish interior is Christopher Columbus’ supposed<br />
tomb inside the south entrance. On the banks<br />
of the River Guadalquivir stands the Torre de Oro,<br />
which is today one of Seville’s major landmarks. It<br />
was originally built by the Moors as a way to block<br />
access to the harbour by attaching a chain to it and<br />
to the opposite river bank.<br />
SEI expects a sizable turnout, expecting that this<br />
top-class event will be an unforgettable experience<br />
for all participants.<br />
AWU<br />
Prof Vitomir<br />
Konstantinovic<br />
Dr Araceli<br />
Morales Sánchez
������������������������������������<br />
�����������������������������<br />
������������������<br />
������������������������������<br />
�������������������<br />
��������������������������������������<br />
����������������������������������������������������������������������������������������
42<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
New British government: Cut this and<br />
cut that – but not health expenses<br />
The new British government must cut expenses.<br />
Shortly after taking office, the British Conservative-<br />
Liberal Democrat coalition government announced<br />
its first concrete austerity measure to rehabilitate<br />
the national budget. The cuts will affect “wasteful”<br />
public spending on e.g. administration, travel,<br />
consultants or IT programs, as Chancellor George<br />
Osborne explained before a meeting of Conserva-<br />
tive Party members. The in-year spending cuts will<br />
amount to £6.25 billion. Osborne promised that<br />
there would be no cuts in education, defence and<br />
health. However, local governments will have to<br />
reduce their expenses by more than £1 billion. Partner<br />
companies of the affected departments will<br />
be contacted soon to implement the cuts as quickly<br />
as possible.<br />
Source: Welt Online, Germany<br />
Italy, Greece, Spain and Portugal:<br />
Rome to cut health expenses<br />
Italians will have to brace themselves for budget<br />
cuts: To reduce the mounting public debt, the government<br />
in Rome is taking drastic austerity measures,<br />
saving 24 billion euros by 2012. The health sector will<br />
be affected as well. In addition, payouts to the local<br />
and regional governments will be reduced.<br />
Europe Ticker<br />
Another victim of the budget cuts will be the<br />
publicly financed Institute for Studies and Economic<br />
Analyses (ISAE), which has conducted surveys on<br />
the business climate and on consumer confidence.<br />
Its tasks will be taken over by the Italian Ministry of<br />
Economy. At 115 percent of GDP, Italy caries the highest<br />
debt burden among the 16 euro-zone countries,<br />
although its budget deficit of 5.3 percent is still relatively<br />
low compared to that of other countries.<br />
With its austerity program, Italy now follows other<br />
countries in the euro zone. Its move had been preced-<br />
ed by Greece, which had enacted a drastic austerity<br />
program in the amount of 30 billion euros against<br />
fierce domestic resistance. Spain has presented an<br />
austerity plan that provides for spending cuts of<br />
50 billion euros over the next three years. France has<br />
raised the statutory retirement age, while Portugal<br />
has increased taxes. Germany will decide on budget<br />
cuts in June.<br />
Source: ZDF – German Television<br />
Photo: panthermedia/Jörg Rüger
Let’s get to work.<br />
True working results with the true all-in-one<br />
Orthopantomograph ®<br />
Tools for professionals.<br />
Orthopantomograph ®<br />
OC200 D VT<br />
The only original Orthopantomograph ®<br />
with new Core<br />
Lateral Ceph imaging program. Same proven superb<br />
image quality as before with up to 68% less radiation.<br />
All the important imaging tools you need in one unit –<br />
including Volumetric Tomography.<br />
Learn more at www.instrumentariumdental.com<br />
www.instrumentariumdental.com<br />
ID_<strong>EDI</strong>_Journal_March_issue_2010_A4.indd 1 24.2.2010 12:59:54
44<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Austria: Healthcare – Afraid of cuts<br />
Austrians are highly satisfied with their healthcare<br />
system, but afraid that it might deteriorate over<br />
the next few years. This is the core message of the<br />
current Health Barometer Austria presented by<br />
Minister of Health Alois Stöger (Social Democrats) in<br />
early May. For the second time, 1000 Austrians were<br />
asked their opinions on healthcare. Customer satisfaction<br />
with healthcare continues to be high; at<br />
62 percent, it is approximately on a par with the EU<br />
average, according to Peter Filzmaier, the author of<br />
the study. On the other hand, an equal proportion<br />
(60 percent) of those surveyed fear a deterioration<br />
of the system due to budget cuts.<br />
In this situation, Stöger is not planning any major<br />
cuts in the healthcare sector. He said that healthcare<br />
fund reform was already in progress and that<br />
drug cost inflation had been brought down from<br />
six to eight percent to two percent today. Instead,<br />
Stöger favours economic stimulus programs in the<br />
healthcare sector; he said such programs “focus on<br />
adding value and create crisis-proof jobs”. The survey<br />
also revealed a high level of public expectations<br />
in connection with the introduction of joint medical<br />
practices planned for later this year. A majority of<br />
those surveyed expect these to become a viable<br />
alternative to hospital outpatient departments,<br />
with shorter waiting times, longer opening hours<br />
and a better choice of treatment providers as a<br />
result.<br />
Source: nachrichten.at, Austria<br />
European Commission survey:<br />
Europeans afraid of treatment errors<br />
Europeans are afraid of adverse events while receiving<br />
healthcare. Their overall opinion of their healthcare<br />
systems, however, is positive.<br />
One-third of all German respondents felt they<br />
could be harmed by healthcare (both by hospital<br />
and non-hospital care). Looking at the EU as a<br />
whole, the corresponding figure is almost 50 percent.<br />
The perceived possible causes include hospital-related<br />
infections or incorrect, missed or delayed<br />
diagnoses.<br />
These were the results of a survey conducted for<br />
the European Commission in autumn 2009. The<br />
survey population included 26,663 people from all<br />
27 EU member states, who were asked questions<br />
related to patient safety and healthcare quality in<br />
Europe. The results of the study were published in<br />
mid-April. Trust in the healthcare system was lowest<br />
in Greece, where 83 percent of those polled expect<br />
treatment-related injury.<br />
More than one-fifth of all EU citizens cite negative<br />
experiences with medical care. The German<br />
figures are actually above average, with 30 percent<br />
citing negative experiences, although only onethird<br />
of those affected had reported the incidents<br />
in question.<br />
Most of those surveyed do not know which institutions<br />
or organizations are responsible for patient<br />
safety. One-third believes that the responsibility lies<br />
with the ministries of health, while 27 percent think<br />
that healthcare providers (e.g. hospitals, physicians)<br />
are responsible. Most of those who reported having<br />
suffered treatment-related injury in their home<br />
country or another EU member state expect that an<br />
investigation into the case or financial compensation<br />
would be the forms of redress. Three-quarters of the<br />
Germans surveyed indicated that they were planning<br />
to seek help from a lawyer for this purpose.<br />
Yet with all that scepticism, an average 70 percent<br />
of those surveyed consider the quality of healthcare<br />
in Europe to be good. Top figures were achieved by<br />
Belgium, with 97 percent, and Austria, with 95 percent.<br />
At 86 percent, the German result is in the upper<br />
third of the table. At the bottom of the list are Romania<br />
and Greece, with only 25 percent.<br />
In addition, one third of those surveyed believe<br />
that healthcare in their own country is better than<br />
in other EU member states. Here, too, Belgium and<br />
Austria topped the list with 65 and 64 percent,<br />
respectively. In Germany the corresponding figure is<br />
54 percent.<br />
The reason why the European Commission conducted<br />
this survey is its effort to improve the quality<br />
of medical care across the EU and to eliminate<br />
inequalities. These efforts include the planned directives<br />
on patient information rights and on prescription<br />
drugs as well as a recommendation by the EU<br />
ministers of health for improving patient safety.<br />
Source: Ärzte-Zeitung, Germany
© MIS Corporation. All rights Reserved.<br />
TM<br />
Innovative Bonding<br />
Graft Material.<br />
BondBone TM is a unique resorbable, osteoconductive,<br />
synthetic bi-phasic calcium sulphate bone-grafting<br />
material. Using BondBone TM does not<br />
require one to stop using any other<br />
bone graft one may be familiar<br />
with. Bonding a grafting material<br />
with BondBone TM will allow<br />
superior handling, enhancing<br />
bond regeneration and<br />
predictable resorption. The<br />
material is known for<br />
eliminating migration of<br />
granules from the grafting site<br />
and has a great advantage in<br />
cost-effectiveness, due to the<br />
larger volume that can be<br />
maintained. BondBone TM can<br />
also be used as a bone graft for<br />
small defects and can act as a<br />
bioresorbable barrier.<br />
INNOVATION<br />
MIS offer a wide range of innovative kits and<br />
®<br />
accessories that provide creative and simple<br />
solutions for the varied challenges encountered<br />
in implant dentistry. To learn more about MIS,<br />
visit our website: mis-implants.com. Make it Simple
46 <strong>EDI</strong><br />
European Law<br />
ECJ: Economic Incentives<br />
to Promote the<br />
Description of Low-Cost<br />
Medicinal Products are Legal<br />
In its decision dated 22 April 2010 (C-62/09), the European<br />
Court of Justice in Luxemburg (ECJ) has ruled<br />
that a scheme by national public health authorities<br />
offering financial incentives to medical practices to<br />
prescribe low-cost medicinal products is compatible<br />
with European law.<br />
The background of the case: In England and Wales,<br />
the National Health Service (NHS) is responsible for<br />
providing a comprehensive health service, including<br />
the procurement of medical drugs. If healthcare professionals<br />
issue prescriptions to be funded by the<br />
NHS, they must comply with its rules. To reduce the<br />
costs of medicinal products, the NHS has introduced<br />
financial incentive schemes to induce physicians to<br />
prescribe for their patients specific named medicinal<br />
products, thereby establishing a positive list of lowcost<br />
medicinal products (statins, in the case at hand).<br />
Physicians were to give preference to medicinal products<br />
in the same therapeutic class, but not necessarily<br />
containing the same active substances. The rules did<br />
not exclude the possibility that another medicinal<br />
product in the same therapeutic class might be better<br />
suited to the treatment of a particular patient, so that<br />
switching the prescribed medication to another based<br />
on a different active substance in some cases might<br />
have adverse consequences for the patient. The NHS<br />
established therapeutic equivalence of medicinal<br />
products in the same therapeutic class in accordance<br />
with, inter alia, the guidelines of the National Institute<br />
for Health and Clinical Excellence.<br />
Financial incentives<br />
Under the scheme, financial inducements are calculated<br />
according to how certain targets are met. One<br />
target is to increase the proportion of prescriptions<br />
for a specific named medicinal product from the positive<br />
list. Another target is to increase the number of<br />
patients whose established medicinal product has<br />
been changed in favour of a specific named medicinal<br />
product from the list.<br />
The Association of the British Pharmaceutical<br />
Industry (ABPI), representing 70 pharmaceutical companies<br />
operating in the United Kingdom, objected to<br />
these financial incentives, voicing its concerns to the<br />
British Ministry of Health and requiring an investigation,<br />
especially in the light of Directive 2001/83/EC on<br />
a community code relating to medicinal products for<br />
human use. The Directive states, inter alia, that persons<br />
qualified to prescribe medicinal products must<br />
be able to carry out these functions objectively without<br />
being influenced by direct or indirect financial<br />
inducements. Where medicinal products are being<br />
promoted, no premiums or other advantages in<br />
money or in kind may be given, offered or promised<br />
to persons qualified to prescribe or supply them,<br />
unless they are inexpensive and relevant to the practice<br />
of medicine or pharmacy, as Article 94 (1) of<br />
Directive 2001/83/EC states.<br />
Safeguarding of public health<br />
an essential aim<br />
The British Ministry of Health considered the NHS<br />
incentive schemes to be legal, as in its opinion the<br />
prohibition of incentives in Directive 2001/83/EC did<br />
not apply to national public health authorities but<br />
only to commercial organizations, whereupon the<br />
ABPI brought an action before the High Court of<br />
Justice (England and Wales). This court referred the<br />
case to the ECJ for an interpretive ruling of Directive<br />
2001/83/EC, asking whether a public body forming<br />
part of a national public health service is precluded<br />
by Article 94 (1) from offering financial incentives to<br />
medical practices for prescribing a specific named<br />
medicine.<br />
During the ECJ proceedings, the European Commission<br />
submitted, in support of the ABPI, that the<br />
provision also applied to national authorities, precluding<br />
the NHS from offering financial inducements<br />
for the prescription of specific named medicinal prod -<br />
ucts. The United Kingdom held an opposing view,
Tixos is a porous surface<br />
characterized by<br />
interconnected cavities,<br />
with predetermined<br />
geometry, that enhance<br />
fast bone formation*.<br />
* References available upon request.<br />
L E A D E<br />
R<br />
I T A L I A<br />
The Laser Microfused Titanium Surface<br />
by LEADER IMPLANTS<br />
Perfect adherence<br />
between<br />
the implant neck<br />
and<br />
soft tissues<br />
MUCOSAL CONNECTIVE FIBERS ADHERE AND PENETRATE DEEP INSIDE<br />
THE SURFACE OF TIXOS IMPLANT (BLUE)<br />
LEADER ITALIA s.r.l.<br />
Via Aquileja, 49 - 20092 Cinisello Balsamo (MI) ITALY<br />
ph. +39 02 618651 - fax +39 02 61290676 - www.leaderitalia.it - export@leaderitalia.it
48 <strong>EDI</strong><br />
European Law<br />
supported in this by the Czech, Estonian, Spanish,<br />
French and Netherlands governments. No other<br />
Member State submitted an opinion.<br />
According to the ECJ, the essential aim of Directive<br />
2001/83/EC is to safeguard public health. This aim is<br />
not endangered by a national public health authority<br />
offering financial incentives for prescribing certain<br />
medicinal products, as this very authority is the<br />
one in charge of safeguarding public health, including<br />
but not limited to evaluating the therapeutic<br />
value of the medicinal products they authorize to be<br />
marketed and the control of the public expenditure<br />
for healthcare. Since the authority is pursuing noncommercial<br />
aims, the NHS’ financial incentive<br />
scheme cannot be regarded as falling within the<br />
definition of commercial promotion of medicinal<br />
products. As the ECJ phrased it: “In those circumstances,<br />
it is permissible for those authorities, in the<br />
exercise of the responsibilities which they assume,<br />
to determine, on the basis of evaluations of the therapeutic<br />
qualities of medicinal products by reference<br />
to their cost for the public budget, whether, in order<br />
to treat certain conditions, certain medicinal products<br />
containing a given active substance are, from<br />
the point of view of public finances, preferable to<br />
other medicinal products containing a different<br />
active substance, but falling within the same therapeutic<br />
class.” Or in other words, the end justifies the<br />
means.<br />
ECJ: Objectivity of physicians<br />
not compromised<br />
The public health authorities should, however, not be<br />
allowed to act entirely freely but should be subject to<br />
some measure of control by the pharmaceutical<br />
industry. The ECJ pointed to Council Directive<br />
89/105/EEC of 21 December 1988 relating to the<br />
transparency of measures regulating the prices of<br />
medicinal products for human use and their inclusion<br />
in the scope of national health insurance systems.<br />
The ECJ considers the resulting legitimate<br />
interests and rights of the pharmaceutical industry<br />
to be adequately protected if the financial incentive<br />
scheme implemented by the public authorities is<br />
based on objective criteria and if the pharmaceutical<br />
industry can verify this objectivity. The ECJ had<br />
already taken the same stance in other cases (e.g. in<br />
its decision of 2 April 2009, A. Menarini et al., C-<br />
352/07). To allow this objectivity to be verified, not<br />
only must the relevant scheme be made public, but<br />
the evaluations establishing the therapeutic equivalence<br />
of the active substances must also be made<br />
available to healthcare professionals and profession-<br />
als in the pharmaceutical industry. But this examination<br />
of incentive schemes is likely to be possible only<br />
for pharmaceutical companies (that do not benefit<br />
from them). Individual physicians will most likely not<br />
be in a position to do so, because they lack the necessary<br />
time and, possibly, the requisite pharmacological<br />
expertise.<br />
Nor does the ECJ seem to believe that financial<br />
incentives can compromise the objectivity of physicians,<br />
which is also required by Directive 2001/83/EC.<br />
Prescribing physicians are prevented by their code of<br />
professional conduct to prescribe a given medicinal<br />
product if it is not fitting for the treatment of<br />
the patient, despite the existence of public financial<br />
inducements for its prescription. In addition, all physicians<br />
in England practice under the supervision of<br />
the public health authorities, which are authorized to<br />
provide them with recommendations relating to the<br />
prescription of medicinal products, either directly or<br />
indirectly by appointing professional organizations<br />
to that effect. This, too, is not considered to infringe<br />
on the physician’s objectivity.<br />
In this last argument, the ECJ seems to consider a<br />
financial incentive to be the same as a recommendation<br />
by a public health authority. However, the<br />
ECJ neglects that Recital 50 in the Preamble to<br />
Directive 2001/83/EC explicitly and exclusively<br />
addresses the prohibition of financial incentives.<br />
Recommendations by a public health authority are<br />
not covered by the Directive at all, because they are<br />
certainly less binding on physicians and less likely<br />
to influence them than financial incentives. European<br />
legislators were apparently aware of this<br />
when they passed the Directive; not so the ECJ.<br />
Its expectations of the professional ethics of physicians’<br />
actions seem to be quite high: The ECJ<br />
assumes that physicians will critically evaluate the<br />
determinations of therapeutic equivalence made by<br />
the National Institute for Health and Clinical Excellence,<br />
being influenced by financial incentives only<br />
where this does not cause the patient any harm.<br />
Especially in a chronically underfunded system as<br />
the NHS, it will be very difficult for physicians to<br />
resist the temptations of financial incentives in a<br />
given situation.<br />
Solicitor Dr Berit Jaeger<br />
Ratajczak & Partners<br />
Berlin · Cologne · Essen · Freiburg ·<br />
Meissen · Munich · Sindelfingen<br />
Posener Straße 1, 71065 Sindelfingen<br />
Germany<br />
www.RPmed.de
+ Close to nature<br />
+ No peri-implantitis<br />
+ Tooth coloured<br />
zit-vario z<br />
Ask for<br />
start-up<br />
offer<br />
now !<br />
Tel. [+49] 9842-9369-0<br />
ziterion gmbh : Bahnhofstraße 3 : D-97215 Uffenheim : Tel. [+49] 9842-9369-0 : Fax [+49] 9842-9369-10 : info@ziterion.com : www.ziterion.com
50 <strong>EDI</strong><br />
Case Studies<br />
Comparative investigation of various implant surfaces by SEM analysis<br />
Surprises in the Land of Microns<br />
Dr Dirk U. Duddeck, PD Dr Jörg Neugebauer, Dr Martin Scheer, Dr Franziska Möller,<br />
Dr H. Mauricio Herrera and Professor Joachim E. Zöller, Cologne/Germany<br />
Implant surface treatment to enlarge the bioactive surface is a clinically proven method and has been accepted by all manu-<br />
facturers as the basis for successful osseointegration of their implants [1-4]. The present study, which had its origins in the work<br />
of the Qualification and Registration Committee, demonstrates that contamination with organic compounds often cannot be<br />
completely avoided when dental implants are manufactured on an industrial scale. All implants inspected exhibited residue<br />
from the production process or from the handling of the implant blanks prior to sterile packaging of the implant, depending on<br />
the production process used.<br />
Correlation between surface morphology<br />
and osseointegration<br />
Since the mid-1970s, implant surfaces have been<br />
modified by microstructuring and surface enlargement.<br />
Numerous studies have shown that retentive,<br />
i.e. rough and porous, titanium surfaces improve<br />
adhesion and promote the production of a matrix<br />
by the osteoblasts [5, 6]. The high initial success rates<br />
of the first Brånemark fixtures were mainly due to<br />
the fact that these only minimally roughened,<br />
machined implants were inserted mainly into compact<br />
mandibular bone rather than into augmented<br />
bone or into maxillary bone with its significantly<br />
lower bone density. Additive procedures such as titanium<br />
plasma spray coating (TPS) or implant coating<br />
with calcium phosphate ceramics were tried in<br />
Fig. 1 Sandblasted and acid-etched surface topography,<br />
x 10,000 (Templant, Medentis).<br />
recent years but have not won general acceptance.<br />
Today, surfaces are generally modified by subtractive<br />
procedures such as sandblasting and/or surface<br />
etching or by anodizing [7, 8].<br />
The implant surface must support the process of<br />
osseointegration, especially when using highly<br />
sophisticated surgical augmenting techniques such<br />
as those required in the highly atrophic maxilla. In<br />
recent years, therefore, several working groups and<br />
implant manufacturers have presented a multitude<br />
of techniques for micromorphological structuring<br />
of implant surfaces in order to improve success rates<br />
[9-13]. Osteoblasts proliferation and differentiation at<br />
the implant surface will to a large extent depend on<br />
the microstructure of that surface [14]. To support the<br />
apposition of osteoblast filopodia, the implant surface<br />
should exhibit a porous structure with micropores<br />
approximately 0.5 to 1 μm in diameter.<br />
Additional micropores 3 to 5 μm in diameter allow<br />
osteoblasts to cling tightly to these depressions.<br />
Implant surfaces with a microstructure characterized<br />
by a very rough surface and the uniform and homo -<br />
genous porous structure (Fig. 1) yield the best results<br />
in terms of osteoblast proliferation and differentiation<br />
[15, 16].<br />
Background<br />
Scanner electron microscope (SEM) studies conducted<br />
in recent years have shown that different surface<br />
treatments for titanium performed during the industrial<br />
implant production process not only influence<br />
the surface characteristics of the implants but also<br />
may leave traces on the implants themselves. The
Manufacturer Country Type Surface treatment<br />
3i Implant Innovations United States Osseotite Certain Prevail Double-etched<br />
Altatec Germany/Switzerland Camlog Sandblasted/etched<br />
Anthogyr France Ossfit Sandblasted/etched<br />
Astra Sweden OsseoSpeed Sandblasted/fluoride-modified<br />
Bego Germany Semados Sandblasted (until 2008)<br />
Bicon United States Bicon Uncoated Implant Sandblasted/etched<br />
Bredent Germany blueSKY Sandblasted/etched<br />
BTI Spain Interna Etched<br />
Curasan Germany Revois Sandblasted/etched<br />
Dentsply Friadent Germany XIVE S Plus Sandblasted/etched<br />
Heraeus Germany IQ:Nect Anodized<br />
International Defcon Group Spain Defcon TSA Double-etched<br />
Konus Dental Implant Systems Germany Plus+ Implantat Etched<br />
Medentis Germany Templant Sandblasted/etched<br />
Neoss United Kingdom Neoss Implant Kit Bimodal Surface Double-sandblasted<br />
Nobel Biocare Sweden Branemark MK III TiU Anodized<br />
Nobel Biocare Sweden Branemark MK III RP Machined<br />
Osstem Korea Georgeous Sandblasted/etched<br />
Straumann Switzerland SLActive Sandblasted/etched<br />
Straumann Switzerland Standard Plus Sandblasted/etched<br />
Sweden Martina Italy Global ZirTi Sandblasted/etched<br />
Thommen Switzerland SPI-Element Sandblasted/etched<br />
Zimmer United States AdVent Sandblasted<br />
Tab. 1 List of implants examined (sorted by manufacturer).<br />
objective of the present study has been to detect and<br />
identify process-related residue and handling-specific<br />
contamination on various implant systems. In doing<br />
so, generalized residue distributed across the entire<br />
implant surface was to be distinguished from random<br />
local contamination; in either case, the findings<br />
were to be subjected to measurements and qualitative<br />
and quantitative elemental analysis.<br />
Materials and methods<br />
A total of 23 different implant systems by 21 implant<br />
manufacturers from nine countries were examined<br />
under the scanning electron microscope (Tab. 1). The<br />
<strong>EDI</strong> 51<br />
Case Studies<br />
production processes for the implant systems examined<br />
differed with regard to fundamental aspects. In<br />
addition to the sandblasted/acid-etched implants<br />
popular today, acid-etched, sandblasted, anodized<br />
and machined implants were included in the study.<br />
The study protocol called for three distinct study<br />
phases:<br />
• The SEM material contrast image allowed conclusions<br />
to be drawn on (1) the chemical nature of<br />
the target material and (2) the distribution of different<br />
materials across the depicted surface. Elements<br />
with an atomic number lower than that of<br />
titanium (and, hence, less electron backscattering)<br />
appear darker in the material contrast image.
52 <strong>EDI</strong><br />
Case Studies<br />
Figs. 2a to c Organic contamination seen in the material contrast image (Curasan Revois, x 20, x 100, x 250).<br />
Fig. 2d Qualitative and quantitative elemental<br />
analysis of the organic contamination.<br />
• The qualitative and quantitative analysis of the<br />
implant surfaces, the so-called energy-dispersive<br />
x-ray spectroscopy (EDS), uses the x-rays emitted<br />
by a sample to determine its elemental composition.<br />
An areal analysis and one or more spot<br />
analyses were performed for each implant.<br />
• In the third and final phase of the study protocol,<br />
those implants exhibiting interesting findings on<br />
the material contrast image that were not only<br />
local (handling-related) but distributed across<br />
most of the implant surface (process-related)<br />
were topographically surveyed to identify the<br />
average area affected as a percentage of the<br />
total area.<br />
Results<br />
None of the implants examined was without local<br />
and/or generalized findings. The bandwidth of these<br />
findings ranged from irregularities in surface topo -<br />
graphy such as inexactly tapped threads (Nobel Bio-<br />
care, Osstem), deposited titanium particles (Nobel<br />
Biocare) and organic contamination such as carbon<br />
particles on the surfaces of 18 of the implants examined,<br />
all the way to regular generalized inorganic<br />
residue traceable to the production process of nine of<br />
the 23 implants. The EDS spot analyses of isolated<br />
local contamination demonstrated the large number<br />
of implicated chemical elements (Tab. 2).<br />
Organic contamination<br />
Spot measurements on the black areas clearly discernible<br />
on the material contrast images (backscattered<br />
electron/BSE images) showed carbon concentrations<br />
of between 9 at. % and 84 at. %. The local<br />
spots with high carbon concentrations differed in<br />
size (30-100 μm), shape and penetration depth and<br />
included flat and superficial (Figs. 2a to d) as well as<br />
impressively extensive contamination areas (Fig. 3). In<br />
addition, carbon-containing structures were found<br />
that obviously had penetrated the titanium surface<br />
Element C F Na Mg Al Si P S Cl K Ca<br />
Min. at. % 9.2 4.3 2.3 0.2 1.12 1.4 1.9 0.7 0.7 1.3 0.4<br />
Max. at. % 84.2 4.3 23.4 4.1 91.2 3.4 7.0 4.4 15.1 13.4 5.8<br />
Number of implants 18 1 3 1 12 2 2 4 3 2 6<br />
Tab. 2 Elements found in the EDS analysis.<br />
Fig. 3 Heraeus IQ:Nect, x 332. Fig. 4 Straumann SLActive, x 606.
Fig. 5 Bicon Uncoated, x 145. Fig. 6 Altatec Camlog, x 21. Fig. 7a Straumann Standard, x 500.<br />
Fig. 7b EDS analysis, Straumann Standard. Fig. 8a Bego Semados, x 1000. Fig. 8b EDS analysis, Bego Semados.<br />
more deeply (Fig. 4). Among the carbon spots found<br />
repeatedly and regularly, contamination of the outer<br />
threads was particularly prominent. The presence<br />
of organic compounds could be demonstrated both<br />
parallel to the thread (Bicon, Thommen, Defcon)<br />
(Fig. 5) and perpendicular to the thread (Altatec,<br />
Dentsply Friadent) (Fig. 6).<br />
Inorganic residue<br />
For inorganic residue, a distinction must be made<br />
between localized spots and generalized coverage of<br />
the entire implant surface with process-related<br />
residue such as Al 2 O 3 . For example, some sandblasted<br />
and acid-etched implants exhibited pronounced<br />
entrapments of Al 2 O 3 in the spot analysis (Figs. 7a<br />
and b). One implant that had merely been sandblasted<br />
with aluminium oxide (Figs. 8a and b) exhibited a<br />
remarkably high percentage of 14.4% aluminium in<br />
generalized Al 2 O 3 residue.<br />
Generalized contamination with<br />
lightweight elements<br />
Nine implants regularly exhibited dark spots in the<br />
material contrast image (BSE). These dark spots indicated<br />
lighter elements that were quantified by<br />
measurements at five points on the implant surfaces,<br />
in terms of the relative percentage of the<br />
implant surface made up of them. The resulting percentage<br />
values were 0.2% to 23.8%. The descriptive<br />
statistics using one-way ANOVA indicated a group of<br />
six manufacturers for which the generalized contamination<br />
amounted to 0.3% and 2.4%, with a low<br />
level of scattering (Heraeus, 3i Implant Innovations,<br />
Zimmer, Osstem, Sweden Martina and Medentis). By<br />
contrast with the implants just named, the implants<br />
made by Bicon, Altatec and Bego exhibited light elements<br />
on a significantly higher percentage of the<br />
surface (p < 0.01) (Fig. 9). Within this group, the Bicon<br />
and Altatec implants differed significantly from<br />
Bego implants, which exhibited light elements on a<br />
significantly larger percentage of the surface. The<br />
production process for this implant has since been<br />
modified.<br />
Discussion<br />
<strong>EDI</strong> 53<br />
Case Studies<br />
Implant loss and especially loss of the periapical<br />
implant/bone contact is invariably due to multiple<br />
etiological factors [17-20]. For example, apical periimplant<br />
lesions have been associated with an insufficient<br />
local blood supply, vascular ischaemia, overheating<br />
during the preparation of the implant bed or,<br />
possibly, contamination of the implant surface [21].<br />
There are few reports on the clinical relevance of<br />
different types of contamination in connection with<br />
apical peri-implant lesions. In a retrospective study<br />
on 3,578 patients, cases of implant loss were documented<br />
and evaluated over a period of ten years<br />
(1996 to 2006) [22]. Implant loss occurred in 126<br />
patients (3.5%). In 80% of the cases, implant loss
54 <strong>EDI</strong><br />
Case Studies<br />
occurred before the implants were loaded. Once<br />
iatrogenic factors such as surgical technique, peri -<br />
operative contamination or occlusal trauma (17.5%),<br />
insufficient bone quality (3%) and peri-implantitis<br />
(1%) were excluded, 75% of the cases were left with<br />
no obvious clinical reason for implant loss. Hence,<br />
when examining the possible causes of implantological<br />
failure, one possible cause – over and above<br />
improper indications, surgical technique or patientspecific<br />
clinical aspects – may be surface contamination.<br />
Insufficient or missing osseointegration – especially<br />
when observed radiologically in the apical<br />
region of the implant – may be the result of an<br />
undesirable histological reaction to extraneous<br />
materials that prevent the formation of the biologically<br />
inert titanium oxide layer.<br />
Since the early 1990s, endosseous titanium<br />
implants have been examined for residue [23] that<br />
may be related to the manufacturing process or to<br />
product-specific handling subsequent to the production<br />
process [24]. Piattelli, Degidi and co-workers performed<br />
an animal study that led them to the conclusion<br />
that residual aluminium oxide particles on<br />
implants have no impact on the osseointegration of<br />
dental implants made of titanium [25].<br />
Shibli, in a qualitative and quantitative elemental<br />
analysis performed in 2005 that was comparable to<br />
the present study, examined 21 non-osseointegrated<br />
titanium implants in 16 patients [26]. Of these,<br />
14 implants have been removed prior to loading, six<br />
after loading and one due to encroachment on the<br />
mandibular canal. Two implants in sterile packages<br />
served as control group. Material contrast images<br />
were taken and EDS elemental analyses performed<br />
on all implants. Unlike the implants of the control<br />
group, all explanted implants exhibited different<br />
types of organic residue that manifested themselves<br />
as differently sized dark spots on the implant surfaces.<br />
The elements found on these implants included<br />
carbon, oxygen, sodium, aluminium, calcium and<br />
silicon. However, the author was unable to prove a<br />
correlation between the contamination and the<br />
implant loss, even though the elemental composition<br />
of the residue on the lost implants differed from<br />
that on the control implants.<br />
Conclusion<br />
The principal distinction must be made between (1)<br />
the medium used in sandblasting (such as Al 2 O 3 ) and<br />
possible residue from the etching process (such as<br />
acid deposits below impacted aluminium oxide particles)<br />
and (2) complex salts whose presence can be<br />
inferred from the presence of phosphorus, sulphur,<br />
chlorine and calcium. The latter may form in varying<br />
Fig. 9 Multiple comparison of the surface percentages of light elements.<br />
Additional studies<br />
In a comprehensive follow-up study, numerous implants by other<br />
manufacturers are currently being examined using the same study<br />
protocol. The objective of that ongoing research is to obtain an<br />
overview of the surface characteristics of as many implants on the<br />
market as feasible. For the first time, this research will also include<br />
zirconia implants, mini-implants and intermediate structures in the<br />
SEM analyses.<br />
compositions depending on the etching solutions<br />
and cleansing bath used.<br />
In addition, carbon residue may be indicative of<br />
traces of handling particles whose provenance may<br />
be rubber gloves or the industrial production process<br />
itself. Residue originating from the conditioning of<br />
the implant surface, whose presence can be<br />
demonstrated in the majority of the implants examined<br />
by a qualitative and quantitative elemental<br />
analysis would appear almost unavoidable, but just<br />
like the organic contamination derived from the handling<br />
process, these do not appear to have any clinical<br />
relevance at the concentrations found.<br />
A list of references will be supplied by the editorial office on request.<br />
Contact Address<br />
Dr Dirk U. Duddeck<br />
Interdisciplinary Policlinic for Oral Surgery<br />
and Implantology<br />
Department of Oral and Maxillofacial Plastic Surgery<br />
University of Cologne<br />
Director: Professor Joachim E. Zöller<br />
Kerpener Straße 32 · 50931 Köln<br />
GERMANY<br />
Phone: +49 221 478-4744 · Fax: -6721<br />
dirk.duddeck@uk-koeln.de
Neugebauer on vestibuloplasty<br />
New Indications<br />
for an Old Technique?<br />
PD Dr Jörg Neugebauer, Dr Franziska Möller, Dr Georg Bayer and Prof Joachim E. Zöller,<br />
Cologne/Germany<br />
In the heyday of preprosthetic surgery, vestibuloplasty was considered one of the procedures to improve the function of<br />
This treatment option is prone to recurrence since<br />
fixation in the edentulous jaw is contingent on, and<br />
can only be achieved by, the prosthetic restoration.<br />
<strong>EDI</strong> 55<br />
Case Studies<br />
prosthetic restorations [1,2]. Elevating the alveolar crest in relative terms would create an opportunity to significantly improve<br />
the function of complete dentures at least on a temporary basis [3-5]. Due to the high recurrence rate involved, a number of<br />
modifications to basic vestibuloplasty were presented and, once again, were shown to bring about different outcomes [6].<br />
Submucosal vestibuloplasty as described by Edlan Mecha is particularly noteworthy, as this technique can establish a relatively<br />
well-shaped vestibulum through a local approach.<br />
Missing<br />
mucobuccal fold<br />
after Le Fort I<br />
osteotomy<br />
(with scarring).<br />
Extensive free<br />
split-skin graft<br />
(covering sites 16<br />
through 26).<br />
Healed graft<br />
following<br />
vestibuloplasty.<br />
An alternative recommendation in this situation is to<br />
widen the attached mucosa through a free mucosal<br />
graft harvested from the palate or to attach a splitskin<br />
graft from the thigh or buttock [7-9]. These procedures<br />
are known to yield more predictable outcomes.<br />
However, they also create problems in the<br />
oral cavity – free mucosal grafts by being associated<br />
with scar formation and split-skin grafts by inclusion<br />
of skin structures [10]. Split-skin grafts in particular<br />
involve the secondary effect of creating a moist<br />
chamber associated with the development of C. albicans<br />
underneath fixed dentures. The use of this procedure<br />
should therefore remain confined to very specific<br />
indications.<br />
Why was the mucosal tissue lost?<br />
Nevertheless, vestibuloplasty still remains a simple<br />
way of widening the attached mucosa on implant<br />
surfaces, notably when the procedure can be used<br />
to correct prosthetic restorations that have been<br />
inserted already. However, it is essential to consider<br />
the reason why the attached mucosa was lost in the<br />
first place. If a flattened mucobuccal fold has formed<br />
after surgery (e.g. because the soft tissue had to be<br />
mobilized for plastic coverage) adequate relocation<br />
will be relatively simple. Loss of attached mucosa<br />
may also occur if a bone substitute is placed for<br />
vestibular augmentation. This situation will normally<br />
render vestibuloplasty somewhat more difficult to<br />
perform down the road, as the tissue structures are<br />
altered by the foreign material.
56 <strong>EDI</strong><br />
Case Studies<br />
Mobile mucosa following<br />
restoration of implants.<br />
Suturing the mucosa inside the newly<br />
established mucobuccal fold.<br />
Fixation of the gauze strip with a periodontal<br />
dressing.<br />
Clinical procedure<br />
Mucosal incision for<br />
vestibuloplasty.<br />
Vestibuloplasty needs to start out by providing infiltration<br />
anaesthesia, such that the individual tissue<br />
layers are expanded as the local anaesthetic spreads<br />
through them. This will greatly facilitate the subsequent<br />
task of conducting a strictly mucosal prepara-<br />
Exposure of the deepened mucobuccal fold.<br />
Note the open wound area.<br />
Epithelialized wound area following suture<br />
removal ten days after surgery.<br />
Preparation of the mucosal flap. Excision of the submucosal<br />
connective tissue.<br />
Placing a iodoform gauze strip on the exposed<br />
wound area.<br />
Follow-up examination eight months after<br />
surgery.<br />
tion. Mucosal flap preparation will be completed on<br />
reaching the implant margin if there is no relation<br />
between the flap and the connective tissue and no<br />
tensile interaction between the tissue types.<br />
An epiperiosteal preparation can be performed to<br />
thin down the connective tissue structure. This will<br />
dislodge the soft tissue, which previously caused the
<strong>EDI</strong><br />
Case Studies<br />
“pump effect” in the peri-implant area, from the<br />
periosteum. Finally, the mucosal flap is transposed<br />
to the newly created mucobuccal fold. The mobilized<br />
mucosa is secured to the periosteum using vertical<br />
mattress sutures. The resultant exposed wound area<br />
is usually covered with an in lay for disinfection (e.g.<br />
iodoform gauze strips) and is then immobilized with<br />
a periodontal dressing. This will ensure that the sulcus<br />
(or the mucobuccal fold) can become widened by<br />
secondary granulation.<br />
Since a relatively deep position must be expected<br />
depending on the width of the mucosal flap,<br />
resorbable sutures should be used for fixation (as a<br />
precaution if primary suture removal inside the sulcus<br />
is not possible after ten days) to avoid inflammatory<br />
reactions in the newly established sulcus.<br />
Patients may need antibiotic coverage in the post -<br />
operative course, depending on the individual risk of<br />
morbidity. This requirement varies both with the<br />
size of the vestibuloplasty and with general health<br />
considerations. Generally speaking, healthy patients<br />
in ASA physical status class 1 or 2 will not require<br />
antibiotic coverage. As the free granulation area may<br />
be relatively painful, information to this effect should<br />
be offered to the patients. They may experience pain<br />
notably when eating acidic food.<br />
Discussion<br />
Keratinized mucosa cannot be attained by vestibuloplasty<br />
alone. Through a submucosally prepared<br />
vestibuloplasty, it becomes possible to reduce the<br />
mobile mucosa which may frequently lead to periimplantitis<br />
via pump movements [11]. Reducing the<br />
mucosal thickness to less than 4 mm will minimize<br />
the risk of anaerobe accumulation. Both free mucosal<br />
and split-skin grafts involve the use of a secondary<br />
donor site [12], which normally will always involve<br />
an extended phase of regeneration compared to the<br />
primary surgical area.<br />
In particular, a vestibuloplasty conducted as a secondary<br />
procedure to optimize the peri-implant soft<br />
tissue is an important tool to ensure long-term outcomes<br />
in healthy patients, as they can either prevent or<br />
limit the progression of an existing peri-implantitis.<br />
A list of references will be supplied by the editorial office on request.<br />
Contact Address<br />
PD Dr Jörg Neugebauer<br />
Interdisciplinary Clinic for Oral Surgery and Dental<br />
Implantology, Department of Dentistry and Oral and<br />
Maxillofacial Surgery of the University of Cologne<br />
Kerpener Straße 32 . 50931 Köln · GERMANY<br />
joerg.neugebauer@uk-koeln.de<br />
57<br />
High Definition<br />
Every single feature<br />
defines a Masterpiece<br />
•11º Morse taper connection<br />
• Platform switching<br />
• Microthreads<br />
• 45º implant shoulder<br />
• RBM Surface treatment<br />
• Anatomic design<br />
• Loading resistance<br />
• Immediate loading<br />
• Surface treated up to the implant collar<br />
• Prosthetic solutions for each case<br />
Are you interested<br />
in becoming our<br />
distributor? Contact us.<br />
The key for a perfect result<br />
CHILE CHINA COLOMBIA POLAND<br />
PORTUGAL SPAIN TAIWAN VENEZUELA<br />
HEADQUARTERS<br />
C/ Santiago López González, 7<br />
47197 Valladolid . Spain<br />
Tel. +34 983 211 312<br />
Fax +34 983 304 021<br />
info@mozo-grau.com<br />
www.mozo-grau.com
58 <strong>EDI</strong><br />
Case Studies<br />
Well-organized teamwork: Periodontology, implantology, prosthodontics<br />
Maxillary and Mandibular<br />
Full-Arch Rehabilitation:<br />
A Complex Case<br />
Dr Jochen Frank, MSc, Aindling/Germany, Gerhard Stachulla, MDT, and Sandra Nodlbichler,<br />
Bergen/Germany<br />
Meticulous planning and intensive collaboration between the dentist and dental technician are an important prerequisite<br />
for implantological success. This article presents a clinical case to demonstrate a systematic periodontological, implantological<br />
and prosthodontic treatment approach for a full-arch rehabilitation.<br />
The 47-year-old male patient presented with several<br />
mobile teeth. His tooth mobility caused him pain and<br />
limited him during meals. The patient also suffered<br />
from extremely bad breath. He was aware that some<br />
of his teeth might not be salvageable. However, he<br />
considered a removable denture with palatal coverage<br />
unacceptable; he urgently requested stable and<br />
functional teeth.<br />
Patient history<br />
The patient’s general health was good. Pocket depths of<br />
up to 12 mm were measured in the maxilla. A purulent<br />
discharge occurred during probing. The teeth generally<br />
exhibited Class III mobility. In the mandible, pocket<br />
depths at teeth 36 to 33, 43 and 45 were between<br />
4 and 9 mm, with the teeth exhibiting Class I mobility.<br />
The patient suffered from an aggressive periodontitis.<br />
Treatment planning<br />
• In the mandible, extraction of teeth 37, 32 to 42 and<br />
44 and a long-term provisional restoration spanning<br />
teeth 33 to 45 via 43.<br />
• In the maxilla, extraction of all teeth and provisionalization<br />
with a complete denture.<br />
• Closed periodontal therapy of the remaining<br />
mandibular teeth plus administration of antibio -<br />
tics (combination according to van Winkelhoff et<br />
al., 1989) with regular follow-up sessions with a<br />
dental hygienist.<br />
• Insertion of five Camlog implants at sites 32, 42, 44,<br />
46 and 47.<br />
• Maxillary CT diagnostics using the Med3D system<br />
and insertion of eight Camlog implants at sites 16,<br />
15, 14, 12, 22, 24, 25, 26; provisionalization with four<br />
provisional implants (IPI, Nobel Biocare) and a fixed<br />
temporary bridge.<br />
• Fixed maxillary and mandibular rehabilitation<br />
comprising crowns and bridges.<br />
Treatment<br />
Provisionalization<br />
Impressions were taken of the baseline situation, and<br />
casts were poured and mounted in an adjustable<br />
articulator (Fig. 1). The dental laboratory was tasked<br />
with the wax-up, with particular attention to preserving<br />
the vertical dimensions, and to analyzing<br />
tooth lengths as well as overbite and overjet. This<br />
anticipatory wax-up served as the foundation for all<br />
subsequent prosthetic and, consequently, implantological<br />
steps (backward planning). Teeth 33, 43 and<br />
45 were prepared, and impressions were taken. Teeth<br />
37 and 32 to 42 were extracted and provisionalized<br />
using a temporary resin bridge (Tempron, GC Europe).<br />
Two weeks later, deep scaling and root planing were<br />
performed on the residual mandibular teeth. The day<br />
before, the patient had started taking the Winkelhoff<br />
antibiotic cocktail (500 mg amoxicillin and 400 mg<br />
metronidazole three times a day for eight days) [1].<br />
At the same appointment, the laboratory-produced<br />
metal-reinforced provisional bridge from tooth 33 to 45<br />
via 43 was inserted (Fig. 2), the maxillary teeth were extracted<br />
and an immediate provisional denture provided.
Fig. 1<br />
Baseline casts.<br />
Fig. 2<br />
Framework of<br />
the provisional<br />
metal-reinforced<br />
mandibular<br />
bridge.<br />
Fig. 3<br />
OPG with<br />
markers for<br />
mandibular<br />
diagnostics.<br />
Fig. 4<br />
Mandibular<br />
situation<br />
before implant<br />
placement.<br />
Fig. 5<br />
During mandi -<br />
bular implant<br />
placement, with<br />
some of the<br />
healing caps<br />
already in place.<br />
Fig. 6<br />
Control radio -<br />
graph following<br />
mandibular im -<br />
plant insertion.<br />
Fig. 7<br />
Barium<br />
sulphate splint<br />
for creating the<br />
CT stent.<br />
1 2<br />
3 4<br />
5 6<br />
7<br />
The overall aesthetic type of the patient was to be preserved,<br />
although improvements in terms of closing<br />
gaps were explicitly approved. Because the patient was<br />
suffering from an untreated aggressive periodontitis, it<br />
was decided not to place any implants immediately, as<br />
the bacterial load would have posed a considerably increased<br />
risk to the stability of the implants. Four to<br />
eight weeks following extraction is considered the ideal<br />
window for implantation. At this time, the soft tissue<br />
will have healed sufficiently while the amount of bone<br />
loss at the alveolar ridge will still be tolerable [2].<br />
<strong>EDI</strong> 59<br />
Case Studies<br />
The surgical procedure<br />
After six weeks, five Camlog implants were inserted<br />
in the mandible at sites 32, 42, 44, 46 and 47 (Figs. 3<br />
and 4). Only a general stent for orientation was<br />
employed to position the implants, because the<br />
bone supply was satisfactory and the favourable<br />
location of the residual teeth provided additional<br />
guidance for implant alignment. No bone augmentation<br />
was required, so the implants immediately<br />
received their healing caps and were allowed to heal<br />
openly (Figs. 5 and 6).<br />
The maxillary bone had been compromised by the<br />
pre-existing periodontitis, which made CT diagnostics<br />
a sensible idea. The provisional restoration was used as<br />
the basis for aesthetic reconstruction, facilitating the<br />
fabrication of a prosthodontic drilling stent and defining<br />
tooth positions, tooth axes and, most importantly,<br />
the implant emergence profile. The temporary maxillary<br />
restoration was relined once the extraction wound<br />
had healed and duplicated for the fabrication of the CT<br />
stent that served to guide the Med3D system (Fig. 7).
60 <strong>EDI</strong><br />
Case Studies<br />
8<br />
10 11<br />
Figs. 8 to 11 Implant planning using the Med3D system.<br />
To prevent dislocation of the stent during the CT<br />
scan, the patient visited the dental office prior to the<br />
scan, where he received local anaesthesia and the<br />
stent was secured to his palate with two microscrews<br />
(Martin, 1,5 x 13 mm). After the scan, the<br />
patient returned to the office for removal of the<br />
stent. Extra holes have been provided in the stent<br />
to allow a second round of local anaesthesia to be<br />
administered.<br />
The CT diagnosis was performed at the planning<br />
centre using the Med3D system. Virtual implants<br />
were placed by the oral implantologist, and the result<br />
was stored on the system. The data required for adjusting<br />
the positioner were printed on a data form<br />
(Figs. 8 to 11). The data obtained were transferred to<br />
the drilling stent using a hexapod (Figs. 12a and b).<br />
This hexapod was freshly adjusted for each implant<br />
9<br />
site and sleeve (Fig. 13). The treatment provider received<br />
a surgical plan containing information about<br />
implant positions, diameters and lengths. This plan<br />
facilitated a predictable surgical procedure with no<br />
major surprises, affording the patient and dentist additional<br />
safety and reducing risk.<br />
By comparison, drilling sleeves in conventional<br />
stents will result in serious deviations from the ideal<br />
position (angular deviation > 5°, positional deviation<br />
> 1 mm) in two thirds of all cases [4].<br />
Eight months following the extraction of the maxillary<br />
teeth, the eight implants were inserted with the<br />
assistance of the drilling stent. To prevent interfering<br />
soft tissue from being displaced or injured during the<br />
consecutive drilling steps, the incision was made from<br />
palatally of the drilling stents. Wound healing was
Figs. 12a and b<br />
Fabricating the<br />
drilling stent in<br />
the laboratory.<br />
Fig. 13<br />
The data<br />
obtained were<br />
transferred using<br />
the hexapod.<br />
12a<br />
12b<br />
Fig. 14 Two weeks after implant insertion. Wound healing<br />
with epitheliolysis.<br />
therefore associated with an epitheliolysis at the<br />
palatal wound margins (Fig. 14), although this did not<br />
present a problem. Epitheliolysis is actually a rather<br />
frequent occurrence if the incision in the mandible<br />
has to deviate from the crestal course that would be<br />
ideal from the point of view of wound healing. The<br />
drilling stent with its double tubes (tube in tube) was<br />
again attached to the palate using traction screws<br />
(Fig. 15). Since the Camlog range does not include any<br />
extra-long implant drills, Straumann ITI drills were<br />
used for preparing the implant bed up to a diameter<br />
13<br />
Fig. 15 The drilling stent was attached to the palate.<br />
<strong>EDI</strong> 61<br />
Case Studies<br />
of 3.5 mm. For the diameters of 3.8 mm and up, the<br />
preparation was performed with Camlog drills without<br />
the drilling stent. The drilling holes for the four<br />
provisional implants were simply apertures without<br />
sleeves and were designed so small that they accommodated<br />
only the pre-drill. The CT diagnosis had<br />
shown that a full-length provisional implant could not<br />
be used, so that the provisional implant had already<br />
been trimmed accordingly prior to the procedure and<br />
was available as a sterile implant of the right length at<br />
the time of the operation.
62 <strong>EDI</strong><br />
Case Studies<br />
16<br />
18 19<br />
Direct bilateral sinus floor elevation procedures<br />
were performed (Figs. 16 and 17). To save the patient<br />
the ordeal of bone harvesting, xenogenous material<br />
(Bio-Oss, Geistlich) was used for this augmentation<br />
almost exclusively; only a very small amount of autologous<br />
bone was collected during drilling and added to<br />
the augmentation material. Even sinus floor augmentation<br />
procedures conducted exclusively with Bio-Oss<br />
have shown the same or even better healing rates or<br />
survival rates than procedures using autologous bone<br />
[5,6,8]. The lateral fenestration was closed with a<br />
xenogenous collagen membrane (Bio-Gide, Geistlich).<br />
Using the membrane promoted the formation of vital<br />
bone and increased the chances for implant survival<br />
[7]. All implants – definitive and provisional – could be<br />
inserted as planned with the Med3D system (Figs. 18<br />
and 19).<br />
Closed healing was provided for the definitive implants.<br />
The temporary denture was reworked into<br />
a bridge at the laboratory and was fitted directly on<br />
the temporary implants postoperatively. This required<br />
tilting the implant heads at the locations provided to<br />
17<br />
achieve parallelism. To prevent the temporary implants<br />
from being accidentally removed or loosened,<br />
they had to be secured below the tilting hinge with<br />
a pair of pliers before tilting. The sleeves to be incorporated<br />
were placed over the implants; undercuts<br />
were blocked out using boxing wax, and the resin<br />
bridge that had been the temporary denture was polymerized<br />
while in occlusion. Once the bridge had been<br />
cleaned and excess material removed, the bridge was<br />
inserted using a temporary cement (Temp Bond, Kerr)<br />
and the occlusion checked and adjusted where needed<br />
(Fig. 20).<br />
Several factors guided the decision in favour of temporary<br />
implants. One of them was that the patient<br />
was unwilling to wear a complete denture during the<br />
six-month healing period. Another reason was that<br />
mechanical loading of the alveolar ridge promotes<br />
crestal bone loss. Mechanical stress increases osteoclast<br />
activity, especially during the initial healing<br />
phase following extraction [3]. A possible alternative<br />
solution would have been a provisional immediate<br />
restoration for the four definitive anterior implants.<br />
Fig. 16<br />
Lateral axis<br />
window for<br />
the sinus<br />
augmentation<br />
procedure.<br />
Fig. 17<br />
Left maxilla<br />
following<br />
implant insertion<br />
and sinus lift.<br />
Fig. 18<br />
Right maxilla<br />
following implant<br />
insertion and<br />
sinus lift.<br />
Fig. 19<br />
Control radiograph<br />
following maxillary<br />
implant insertion.
Fig. 20<br />
Cemented<br />
long-term<br />
provisional<br />
on provisional<br />
implants.<br />
Fig. 21<br />
Preparing for the<br />
maxillary ...<br />
Fig. 22<br />
... and mandibular<br />
impression.<br />
Fig. 23<br />
Maxillary<br />
implant<br />
impression.<br />
Fig. 24<br />
Mandibular<br />
implant<br />
impression.<br />
21<br />
23 24<br />
However, we rejected this possibility because it would<br />
have meant an additional risk for the definitive implants<br />
and would, moreover, have been associated<br />
with considerable additional cost. But the provisional<br />
restoration has its disadvantages with regard to softtissue<br />
support, aesthetics and phonetics. The distance<br />
between the bridge and the alveolar ridge was 2 to<br />
4 mm. There was a potential hazard of a collapsing<br />
upper lip and undesirable wrinkles. If the upper lip is<br />
short, it may expose the void during smiling or even<br />
get caught in the gap. Because air may escape between<br />
the bridge and the alveolar ridge, inflating the<br />
vestibular area, some patients may experience a phonetic<br />
challenge. Patients may find attempts to prevent<br />
this very strenuous, and changes in pronunciation may<br />
result. In the case presented here, the phonetic challenge<br />
did exist, but it was accepted by the patient for<br />
the duration of the provisional phase.<br />
22<br />
<strong>EDI</strong> 63<br />
Case Studies<br />
Final restoration<br />
The maxillary implants were uncovered after seven<br />
months. The patient surprisingly opted for a removable<br />
bridge as definitive maxillary restoration, no<br />
longer being deterred by the idea of having to<br />
remove the bridge each day for oral hygiene. On the<br />
contrary, the patient realized the advantages of<br />
being able to clean the restoration while in plain<br />
view. The patient chose a removable telescopic<br />
bridge whose primary components were custom allceramic<br />
abutments. Four weeks after re-entry, opentray<br />
maxillary and mandibular Permadyne impressions<br />
were taken (Figs. 21 to 24). A bite rim attached<br />
with a screw to the implant outside 22 assisted in<br />
determining the approximate centric position. The<br />
vertical dimension found during the time the provisional<br />
restoration was in place was verified with a<br />
gauge.
64 <strong>EDI</strong><br />
Case Studies<br />
Fig. 25 Copy-milled primary crowns as produced by the<br />
Cercon milling unit.<br />
Fig. 27 ... and the secondary copings produced by electroplating.<br />
Fig. 29 Maxillary tertiary framework ...<br />
The maxillary telescopes:<br />
The dental technician waxed up the primary telescopes<br />
on the Camlog Insert abutments. The wax-up<br />
was copy-milled using the Cercon milling unit (Fig. 25)<br />
and adhesively connected to the prepared titanium<br />
abutments in the laboratory. The surface of the telescopes<br />
was finished by wet grinding with a turbine<br />
(Fig. 26). The secondary copings were electroplated<br />
onto the finished primary crowns using the Degu-<br />
Fig. 26 The all-ceramic primary crowns were milled individually ...<br />
Fig. 28 Electroplated copings on the zirconia primary crowns.<br />
Fig. 30 ... complete with jig and bite rim.<br />
Dent Solaris electroplating unit (Figs. 27 and 28). The<br />
tertiary structure was cast in a non-precious metal<br />
(Figs. 29 and 30).<br />
The mandibular restoration:<br />
The combination of natural and implanted mandibular<br />
abutments required a multiply segmented bridge<br />
design. The framework was cast in the classical manner<br />
using a high-gold bonding alloy (Figs. 31a and b).
Fig. 31a The mandibular frameworks.<br />
<strong>EDI</strong> 65<br />
Case Studies<br />
Fig. 31b The finished maxillary and mandibular frameworks exhibit a<br />
good fit.<br />
Fig. 32 The maxillary provisional/travel denture. Fig. 33 Second mandibular provisional.<br />
Fig. 34a Maxillary ceramic abutment try-in. Fig. 34b Control radiograph.<br />
New provisionals were provided for both the maxilla<br />
and the mandible (Figs. 32 and 33).<br />
In-office try-in:<br />
The ceramic abutments in the maxilla were tried<br />
in, some of them in anaesthesia (Fig. 34a and b). Titanium<br />
abutments were used in the mandible. The<br />
definitive abutment margins were checked and any<br />
corrections required were documented. A provisional<br />
implant between sites 14 and 15 had to be removed,<br />
because there was too little space. The provisional<br />
bridge was relined in this region and supported by<br />
the healing caps. This was followed by the important<br />
aesthetic wax-up, into which the patient’s expectations<br />
were duly incorporated. The vertical dimension<br />
was once again verified based on the speaking<br />
space.
66 <strong>EDI</strong><br />
Case Studies<br />
Fig. 35 Once the abutments have been seated, the secondary components<br />
were tried in ...<br />
Fig. 37 Tertiary framework with anterior jig.<br />
Fig. 38 Maxillary ... Fig. 39 ... and mandibular overimpression.<br />
The prosthetic appointment:<br />
In a single session, the provisional implants were re -<br />
moved, the abutments were definitively inserted, the<br />
electroplated telescopic crowns were tried in (Fig. 35)<br />
and adhesively connected to the tertiary frame -<br />
work in the mouth using AGCem (Wieland). In the<br />
mandible, the abutments were inserted prior to bite<br />
registration, and the frameworks were connected<br />
using fine A-silicone impression material. The centric<br />
relation was recorded in detail based on the tertiary<br />
framework (Fig. 36). The vertical dimension was<br />
Fig. 36 ... and the centric relation determined.<br />
determined by an anterior jig (Fig. 37). Next, an overimpression<br />
of the frameworks was taken using Permadyne<br />
(Figs. 38 and 39).<br />
At the end of this extended treatment session, the<br />
patient received a maxillary resin bridge without<br />
any metal reinforcements to serve as a travel denture<br />
(Fig. 40), which also served as a provisional restoration<br />
until the definitive restoration was inserted. This also<br />
meant that the patient would never be without a<br />
restoration even in the event that the definitive
Fig. 40 Maxillary travel denture and second provisional mandibular<br />
bridge.<br />
Fig. 42 Ceramic veneer for the mandibular anterior ... Fig. 43 ... and posterior regions.<br />
44 45<br />
Figs. 44 and 45 Wax try-in and remounting.<br />
restoration required repairs, a precaution that is generally<br />
highly appreciated. For reasons of stability, the<br />
palate could not be left completely uncovered in this<br />
case. A new provisional restoration with a shortened<br />
span was inserted in the mandible (Fig. 41).<br />
Fabrication of the definitive restorations:<br />
At the laboratory, new master casts were poured<br />
and remounted in the articulator in the newly determined<br />
centric relation. The definitive restoration<br />
could now be fabricated based on the results of the<br />
<strong>EDI</strong> 67<br />
Case Studies<br />
Fig. 41 Everything has been prepared for the try-in of the maxillary<br />
wax-up and the mandibular framework after the first firing.<br />
aesthetic wax-up and the desires and phonetic<br />
requirements of the patient. In the mandible, the<br />
restoration was veneered using the Duceram Kiss<br />
veneering ceramic by DeguDent (Figs. 42 and 43). The<br />
maxillary framework was veneered with a light-polymerizing<br />
material, Sinfony by Espe. The missing gingival<br />
segments were added using Sinfony Gingiva.<br />
The next step was the important try-in of the maxillary<br />
wax-up and the mandibular framework after the<br />
first firing, followed by remounting (Figs. 44 and 45).
68 <strong>EDI</strong><br />
Case Studies<br />
46 47<br />
48a<br />
Figs. 48a and b All-ceramic primary crowns in the maxilla.<br />
The final steps were the definitive cementing of the<br />
mandibular restoration (Figs. 46 and 47), adaptation of<br />
the travel denture to the new occlusal situation and<br />
remounting of the definitive maxillary restoration,<br />
which had been designed as a removable bridge that<br />
lets the palate completely free (Figs. 48a to 50). The<br />
entire treatment took 15 months to complete.<br />
A list of references will be supplied by the editorial office on request.<br />
48b<br />
Fig. 46<br />
Titanium abutments<br />
in the<br />
mandible prior to<br />
segmentation.<br />
Fig. 47<br />
Cemented<br />
mandibular<br />
crowns and<br />
bridges.<br />
49a 49b Figs. 49a and b<br />
The definitive<br />
restoration<br />
in situ.<br />
Fig. 50<br />
Final radiograph.<br />
Contact Addresses<br />
Dr Jochen Frank,<br />
Master of Science for Oral Implantology (DGI)<br />
Arnhofenerstr. 4 1/2 · 86447 Aindling · GERMANY<br />
Frank.Pflumm@t-online.de<br />
Dentallabor Stachulla<br />
Gerhard Stachulla, MDT<br />
Derchinger Str. 11 · 86444 Bergen · GERMANY<br />
gerhard@stachulla.de
Carestream Health<br />
© Carestream Health, Inc., 2010. The Kodak trademark and<br />
trade dress are used under license from Kodak.<br />
KODAK 9000 3D Extraoral Imaging System<br />
Innovation, in reach.<br />
Now available with stitching program<br />
Extended field of view at the same affordable price as before!<br />
Automatically combines<br />
localized volumes<br />
3D exams from<br />
multiple quadrants<br />
visit www.kodakdental.com<br />
or call 00800 4567 7654
70 <strong>EDI</strong><br />
Case Studies<br />
Neugebauer et al on augmentation materials<br />
Marketing and Other Types of<br />
“Mad Cow Disease”<br />
PD Dr Jörg Neugebauer, PD Dr Dr Daniel Rothamel and Prof Joachim E. Zöller, Cologne/Germany<br />
For patients to be treated with implants and implant-supported restorations, a number of different medical devices are<br />
required such that adequate treatment can be performed in line with current scientific evidence. Many products and suppliers<br />
have become established in recent years. As a result, highly specific surgical techniques and materials are available today to<br />
deal with a variety of different indications.<br />
Notably in the highly competitive market of bone<br />
substitutes, various marketing concepts are employed<br />
in an attempt to acquire new customers or users.<br />
This implies that the pertinent documentation – usually<br />
supplied by the industry – needs to be critically<br />
ap praised. Summaries that seemingly bring together<br />
various sources from the literature may be linked to<br />
other statements and recommendations that were<br />
never made or, for that matter, never intended by the<br />
original authors. Over the past few weeks, numerous<br />
implant dentists have been faced with a message<br />
(first launched through anonymous mailing) that<br />
bone substitutes derived from bovine material must<br />
be expected to carry risks. Procedures of this type,<br />
they were told, should henceforth become safer and<br />
simpler through the introduction of a new bone substitute<br />
or a novel application. Once users had been<br />
sensitized to this campaign by repeated mailings, the<br />
product was introduced. It was marketed as similar<br />
in structure to conventional bovine materials while<br />
being manufactured by purely synthetic means.<br />
Power of innovation<br />
by product development<br />
The past few years have seen powerful innovations<br />
in dentistry. This has clearly been due to the potential<br />
of product development offered by industry. Only a<br />
limited number of implant systems, implant surfaces<br />
and bone substitutes would today be available in<br />
the absence of this industry base. However, the relatively<br />
generous design of introducing medical de -<br />
vices at the suppliers’ own responsibility within the<br />
European Community should not be interpreted such<br />
that marketing-driven efforts can be allowed to cast<br />
doubt on any established products that have been<br />
around for numerous years. Any users of medical<br />
devices, and healthcare providers conducting followup<br />
treatments, are required by law to report any<br />
unexpected events or side-effects to their national<br />
supervisory authority (e.g. the German Institute for<br />
Drugs and Medical Devices). However, calling products<br />
into question in an effort to be provocative will<br />
give rise to uncertainty in the market, notably when<br />
patients come across such information that was originally<br />
intended for physicians. Many of them will lack<br />
the scientific background to take these campaigns<br />
for what they are, objectively speaking. Similar to<br />
many other devices used in dentistry, products are<br />
available not only from the market leader but also<br />
from other manufacturers offering bone substitutes<br />
with similar technologies.<br />
Based on the current body of literature, it can be<br />
stated that the clinical functionality of bovine bone<br />
substitutes has been demonstrated in an evidencebased<br />
fashion by animal experiments, clinical surveillance<br />
studies and prospective studies for indications<br />
related to both periodontology and implant dentistry<br />
[1-4]. Data for this purpose have been collected and<br />
published both in university settings and by experienced<br />
implant dentists.<br />
A theoretical risk that prion infection might occur<br />
during grafting with bovine bone substitutes is open<br />
to discussion [5-7]. However, different studies on this<br />
issue have already been presented [8,9]. Decisions<br />
based on cultural, ethnic or religious concerns are an<br />
entirely different matter and should be left at the discretion<br />
of individual users. In this way, the various<br />
products can be presented to patients on the basis of<br />
scientific validation, thus helping them to avoid any
Fig. 1a Bio-Oss – overview (40 x)<br />
Fig. 1b Bio-Oss – detailed view (200 x)<br />
Fig. 2a Cerabone – overview (40 x)<br />
risks involved. In the English-speaking countries, allogeneic<br />
materials are preferably used along with bo -<br />
vine materials [10,11]. These allogeneic products have<br />
also become more popular in continental Europe, so<br />
far without any major discussions related to infection<br />
[12].<br />
Figures 1a to 3b illustrate biopsies of bovine xenogeneic<br />
bone substitutes, obtained six months after<br />
two-stage sinus floor elevation within the context of<br />
oral implant treatments. Three materials are shown:<br />
Bio-Oss (Geistlich Biomaterials, Wolhusen, Switzerland),<br />
Cerabone (botiss dental GmbH, Berlin, Germany)<br />
and Bego OSS (Bego Implants, Bremen, Germany).<br />
All materials display a reliable degree of<br />
osteoconductive effectiveness. Throughout the augmented<br />
zone, individual granules are invaginated by<br />
newly formed hard tissue and are cross-linked to<br />
each other via hard-tissue bridges. The different<br />
staining pattern of the granules results from the different<br />
preparation technique to which the bovine<br />
bone was subjected.<br />
EU Commission Directive 2003/32/EC details the<br />
legal specifications for the use of medical devices of<br />
animal origin [13]. Regarding the safety of Bio-Oss, a<br />
statement by the German Society for Dentistry and<br />
Oral and Maxillofacial Surgery (DGZMK) is available<br />
[14]. The safety of Cerabone and Bego OSS has been<br />
Fig. 2b Cerabone – detailed view (200 x)<br />
<strong>EDI</strong> 71<br />
Case Studies<br />
Fig. 3a Bego OSS – overview (40 x)<br />
Fig. 3b Bego OSS – detailed view (200 x)<br />
officially certified by the health authority of the German<br />
state of Hesse [13,15].<br />
It seems odd that a new product for which limited<br />
scientific information is available should provide<br />
more safety than xenogeneic materials that have<br />
been well established for use in augmentative procedures<br />
over several decades. It is precisely in regenerative<br />
procedures that long-term treatment outcomes<br />
will only be evident after several years. The claims<br />
made by this manufacturer are even more surprising<br />
when considering that very few scientific studies<br />
have been published about other bone substitutes<br />
offered by that company despite relatively long follow-up<br />
periods. Apparently, the manufacturer in<br />
question is marketing a new concept on the basis of<br />
fear-mongering without offering validation of their<br />
claims by pertinent scientific data.<br />
A list of references will be supplied by the editorial office on request.<br />
Contact Address<br />
PD Dr Jörg Neugebauer<br />
Interdisciplinary Clinic for Oral Surgery and Dental<br />
Implantology, Department of Dentistry and Oral and<br />
Maxillofacial Surgery of the University of Cologne<br />
Kerpener Straße 32 . 50931 Köln · GERMANY<br />
joerg.neugebauer@uk-koeln.de
72 <strong>EDI</strong><br />
Product Studies<br />
3D finite element analysis comparing standard and reverse conical neck implants<br />
Bone Platform Switching<br />
Matteo Danza, MD 1 , Ilaria Zollino, MD 2 , Luigi Paracchini, Engineer 3 , Iole Vozza, DDS 4 ,<br />
Guidi Riccardo, DDS 2 , and Francesco Carinci, MD 2<br />
Biomechanical optimization is an important objective in the design of dental implants [1]. Finite element analysis (FEA) has become<br />
an increasingly useful tool for predicting the biomechanical stress on an implant and the surrounding bone [2]. The components in<br />
a dental implant-bone system are geometrically complex [2]. The use of FEA in implant biomechanics offers many advantages over<br />
other methods when it comes to simulating the complexity of clinical situations [3]. FEA facilitates predictions of stress distribution<br />
in the contact area between implant walls and cortical bone and between the apical aspect of the implants and trabecular bone [2].<br />
Although the success rates of some implant systems have been high, implant failures do occur [4, 5].<br />
To achieve stable osseointegration, high stress concentrations<br />
in bone should be avoided because they<br />
can induce severe resorption of the surrounding<br />
bone, leading to gradual mobility and potentially to a<br />
complete loss of the implant [6]. A key factor for the<br />
implant success is the manner in which loads are<br />
transferred to the surrounding bone [7]. It has long<br />
been recognized that both the implant and the bone<br />
should be loaded within a certain range for physiologic<br />
homeostasis. Overload can cause bone resorption<br />
or fatigue failure of the implant, whereas underloading<br />
may lead to disuse atrophy and subsequent<br />
bone loss [8, 9].<br />
Factors that influence load transfer at the boneimplant<br />
interface include the type of loading, the<br />
bone-implant interface, implant geometry, the type<br />
of restoration and the quality and quantity of the<br />
surrounding bone [2]. Implant length, diameter and<br />
shape, representing the implant geometry, can be<br />
modified easily in the implant design, while the quality<br />
and quantity of the cortical and cancellous bone<br />
need to be assessed clinically and should influence<br />
implant selection [2].<br />
Analyzing the load transfer at the bone-implant<br />
interface is an essential step in the overall load analysis<br />
[10], and FEA has been widely used for the quantitative<br />
evaluation of loads on implants and surrounding<br />
bone.<br />
In the present study, 3D FEA was used to examine<br />
the biomechanical behaviour of two types of<br />
implants differing only in emergence profile that<br />
were subjected to static loading in contact with D1<br />
and D4 bone tissue.<br />
Materials and methods<br />
The biomechanical behaviour of two different<br />
implants (SPI and SFB, Alpha Bio Implant, Petach<br />
Tikva, Israel) subjected to static loading in contact<br />
with D1 and D4 bone tissue was evaluated in the<br />
present study. The implants were 4.2 mm in diameter<br />
and 13 mm in length, and the abutments were<br />
straight. The implants were identical except for their<br />
emergence profile: SPI has a straight profile, whereas<br />
SFB has a tapered profile (Figs. 1a and b).<br />
The volumes of the single implants and their differences<br />
were calculated. The total volume of a SFB<br />
implant is 219.94 mm 3 , while the volume of a SPI<br />
implant is 225.51 mm 3 . The difference is 5.57 mm 3 .<br />
Therefore, placing the SFB implant will save 5.57 mm 3<br />
of crestal bone around the implant neck, with potential<br />
beneficial effects on the bone-implant interface<br />
and on the papilla.<br />
FEA was used to determine the strain distribution<br />
within peri-implant bone as a function of the different<br />
profiles of the implant neck. Implant system,<br />
bone type and the axial and transversal loads applied<br />
to the different configurations had to be examined to<br />
evaluate the biomechanical behaviour. The directions<br />
of the axial and transversal loads when applied to<br />
the top of the implant were evaluated. A double system<br />
was analyzed: (a) FY strength along the Y axis at<br />
200 N; (b) FZ strength applied along the Z axis at 140 N<br />
(Fig. 2).<br />
The mathematical models produced by FEA are<br />
curves, surfaces and solids. Once drawn the systems<br />
that were object of the study by CAD (Computer<br />
1 Dental School, University<br />
of Chieti, Italy<br />
2 Maxillofacial<br />
Surgery, University<br />
of Ferrara, Italy<br />
3 Private practice,<br />
Milano, Italy<br />
4 Dental School,<br />
University of Rome<br />
“La Sapienza”, Italy
Fig. 1a Straight neck of a SPI implant.<br />
Fig. 2 FY and FZ strengths applied along Y and Z directions at<br />
200 N and 140 N, respectively.<br />
Aided Design), the FEA discretized solids composing<br />
the system in many infinitesimal little elementary<br />
solids defined finite elements. This resulted in a mesh<br />
in which the single finite elements were connected<br />
by nodes (Fig. 3). Once the solids, the mesh and the<br />
projected loads (direction and intensity) were<br />
defined, a definition of the chemical and physical<br />
properties of materials was required. When performing<br />
a biomechanical analysis of the materials under<br />
low-intensity stress, it must be remembered that the<br />
materials were considered to be homogeneous, linear<br />
and isotropic. The FEA simulation assumed a linear<br />
relationship between loads and deformations.<br />
The portion of bone containing the implant was<br />
delimited by joints on two sides, removing all degrees<br />
of freedom within the system.<br />
The pivot inside the bone tissue was delimited by<br />
contact elements such as the connecting screw and<br />
the abutment. The CAD 3-D mathematical models used<br />
for FEA were implemented using a surface modeller<br />
Fig. 1b Tapered neck of a SFB implant.<br />
(Rhinoceros 4.0 – McNeel Europe, Barcelona, Spain)<br />
and a solid modeller (Solid Works 2007 SP 2.2, Solid-<br />
Works Corporation Headquarters, Concord, Massachusetts,<br />
USA, both belonging to Windows XP Pro -<br />
fessional SP1, Microsoft Corporation, Milano, Italy).<br />
The discretization in finite elements and the FEA<br />
were realized by NEiFusion 1.12 (Noran Engineering,<br />
Inc., Westminster, California, USA).<br />
Results<br />
<strong>EDI</strong> 73<br />
Product Studies<br />
Fig. 3 Mesh formation where the single finite elements were<br />
connected by nodes.<br />
The results obtained with the FEA simulation showed<br />
that the stress distribution of a tapered profile of an<br />
implant neck at the abutment insertion area differed<br />
from that of an implant with a straight neck at the<br />
level of the bone. Stress in a bone matrix is commonly<br />
determined according to von Mises’ theory. This<br />
theory was used here in order to determine the distribution<br />
of stresses at the bone-implant system interface<br />
in two different bone classes (D1 and D4).
74 <strong>EDI</strong><br />
Product Studies<br />
For the tapered-neck (SFB) implants, the load distribution<br />
was more uniform; the strain tended to be<br />
uniformly distributed inside the bone. By contrast<br />
the load acting on a straight neck (SPI) implant tended<br />
to confine the strain next to the external surface<br />
of the implant, and it was not distributed inside the<br />
bone (Figs. 4a to 5).<br />
Table 1 reports the values of the loads applied to SPI<br />
and SFB implants.<br />
Discussion<br />
Primary implant stability and bone density are considered<br />
essential for achieving predictable osseo -<br />
integration and the long-term clinical survival of<br />
implants [11].<br />
The long-term clinical performance of a dental<br />
implant is dependent on the preservation of good<br />
bone quality around the implant and a sound interface<br />
between the bone and the biomaterial. Both are<br />
governed by the stress and strain distribution within<br />
the bone [2].<br />
An effective way to ensure excellent clinical performance<br />
is to use a biomechanically optimized<br />
implant that provides a health stress-strain level as<br />
required for normal bone resorption and deposition<br />
4a 4b<br />
4c 4d<br />
Fig. 5 Different strain distributions in the peri-implant bone<br />
around implants. In the SFB implant, the strain tends to<br />
spread uniformly inside the bone. In SPI implants, the load<br />
tends to confine the strain next to the external surface of<br />
the implant, and it is not distributed within the bone.<br />
at the implant site [12]. Implant features causing<br />
excessively high or low stresses may contribute to<br />
pathologic bone resorption or bone atrophy [8, 9].<br />
Most efforts have been directed at optimizing the<br />
geometry of the implants to maintain beneficial<br />
stress levels at the bone-implant interface [13].<br />
Implant geometry includes length, diameter and<br />
shape. The optimum length and diameter necessary<br />
Figs. 4a and b<br />
Stress distribution<br />
(von Mises) of<br />
SPI implants in<br />
D1 and D4 bone,<br />
respectively.<br />
Figs. 4c and d<br />
Stress distribution<br />
(von Mises) of<br />
SFB implants in<br />
D1 and D4 bone,<br />
respectively.
Tab. 1<br />
Values of the<br />
loads applied<br />
to SPI and SFB<br />
implants.<br />
Bone class Type of implant _ (MPa) _ (micro-strain)<br />
D1 Tapered neck 97 5.4e-003<br />
D4 Tapered neck 82 5.25e-003<br />
D1 Straight neck 75 3.9e-003<br />
D4 Straight neck 65 8.1e-003<br />
for long-term success depend on the condition of<br />
the bone – if the bone is normal, length and diameter<br />
will not be significant factors for implant success,<br />
but if the bone condition is poor, large diameters<br />
are recommended, and short implants should be<br />
avoided [5, 14].<br />
Previous studies had mainly focused on the<br />
mechanics of implant and abutment connections<br />
and their impact on abutment mobility as well as on<br />
the effect of implant shapes on stress distribution<br />
within the bone.<br />
The effect of the abutment type on stress distribution<br />
within the bone under vertical and inclined<br />
loads was investigated by Chun et al. [6] using FEA.<br />
They found that the type of abutment used significantly<br />
influences the stress distribution within the<br />
bone because of different load-transfer mechanisms<br />
and the differences in size of the contact areas<br />
between the abutment and implant.<br />
With regard to implant shape, theoretical analysis<br />
implies that clinically, whenever possible, an optimized<br />
– not necessarily larger – dental implant shape<br />
should be used based on the specific morphological<br />
limitations of the mandible [2].<br />
Siegele and Soltesz [15] compared cylindrical, conical,<br />
stepped, screw and hollow cylindrical implant<br />
shapes exposed to physiologic stresses and examined<br />
the stress concentrations at the site of implant<br />
emergence from the bone using FEA. They demonstrated<br />
that different implant shapes led to significant<br />
variations in stress distribution within the bone<br />
because implant surfaces with very small radii of<br />
curvature (conical) or geometric discontinuities<br />
(stepped) induced significantly higher stresses than<br />
smoother shapes (cylindrical, screw-shaped).<br />
Danza and Carinci [16] elaborated on the concept<br />
of bone platform switching (BPS) obtained by using<br />
dental fixtures with a reverse conical neck. BPS is an<br />
internal bone ring in the coronal part of the implant<br />
yielding more residual crestal bone around the<br />
implant neck, with several advantages: reduced<br />
mechanical stress in the crestal area of the alveolar<br />
bone, repositioning of gingival papillae on the bone<br />
<strong>EDI</strong> 75<br />
Product Studies<br />
ring and a proper vascularization to the hard tissue<br />
even in cases of reduced inter-implant space.<br />
Load transmissions and resultant stress distributions<br />
at the bone-implant interface have been the subject of<br />
several FEA studies. Some authors [17, 18] have drawn<br />
attention to the fact that repeated loading and unloading<br />
cycles result in alternating contact and separation<br />
of components of the implant. Clinical findings of<br />
screw-loosening and failure probably result from these<br />
separation events and from elevated strains within the<br />
screw. The other mechanism of screw loosening is related<br />
to the fact that no surface is completely smooth.<br />
Because of the microroughness of components, when<br />
the screw interface is subjected to external loads,<br />
micromovement occurs between the surfaces.<br />
Design changes to avoid or reduce the incidence of<br />
clinical problems and abutment screw failures by<br />
improving the stress distribution of implant components<br />
have been suggested in this FEA study.<br />
Different strain distributions in the peri-implant<br />
bone around implants with a tapered neck seem to<br />
result in more bone activity with less crestal bone<br />
resorption. Zero or near-zero strain, as observed in<br />
implants with a straight neck (SPI), does not engage<br />
the bone matrix adequately, which may lead to a<br />
crestal bone resorption [19]. The strain values have<br />
shown that in the straight-neck implant (SPI) a higher<br />
propensity to deformation (higher micro-strain<br />
values) in the apical portion was present, leading to<br />
greater implant instability (see Tab. 1). Higher instability<br />
of a straight implant causes more micromovement<br />
at the interface, with a higher risk of fibrous<br />
connective tissue formation at the interface [20].<br />
A list of references can be found on www.teamwork-media.de<br />
Contact Address<br />
Professor Francesco Carinci, MD<br />
Chair of Maxillofacial Surgery<br />
Arcispedale S. Anna<br />
Corso Giovecca 203 . 44100 Ferrara · ITALY<br />
Phone/Fax: +39 0532 455582<br />
crc@unife.it . www.carinci.org
76 <strong>EDI</strong><br />
Product Studies<br />
Pre-implantological bone block osteosynthesis:<br />
Functional Innovations<br />
Dr Dr Andres Stricker, Constance/Germany<br />
Enossal implantation has been established as a predictably reliable option for the treatment of edentulous patients. Aimed at<br />
approximating complete remission, the implant should meet not only functional requirements, but also aesthetic expectations.<br />
The demand that the implant should be perfectly positioned in all three dimensions marks the end of approaches that simply<br />
use the available residual bone – and the beginning of prosthetically perfect implant positioning. Perfect implant positioning<br />
very often requires bone augmentation, since bone deficits need to be addressed either before or during implant insertion.<br />
For alveolar crests with advanced atrophy (less than<br />
3 mm in width), simultaneous procedures can be<br />
contraindicated because they significantly increase<br />
implant failure rates. Here it would be preferable<br />
to pursue a two-stage approach where, ideally, an<br />
autologous bone graft from an appropriate donor<br />
site is transferred to the deficient alveolar crest<br />
region before embarking on implant surgery. After a<br />
healing period of at least three months, the osseous<br />
implant bed will be optimally integrated in three<br />
dimensions, ready for perfect implant positioning. In<br />
pre-implantological augmentation procedures there<br />
is a clear tendency towards intraoral bone grafts harvested<br />
from the retromolar region (or possibly from<br />
the mental bone or the zygomaticoalveolar crest),<br />
but away from extraoral grafts harvested from the<br />
iliac crest. The congeneric origin and consequent<br />
similar bone structure (due to the neuroectodermal<br />
formation of the viscerocranium and the mandible)<br />
make intraoral bone grafts the preferred solution,<br />
especially with regard to their significantly better<br />
absorption properties compared to extraoral iliac crest<br />
grafts, where the bone originates from enchondral<br />
ossification.<br />
The criteria for successful healing and integration<br />
of bone grafts are secure and predictable fixation and<br />
tension-free suture closure. But soft-tissue management<br />
(incision control, lobe design) deserves at least<br />
as much attention as contouring and securing the<br />
bone block. Both these factors are interdependent, as<br />
excessive stress on the suture leads to dehiscence of<br />
the soft parts, eventually resulting in the total or partial<br />
loss of the graft. The results of secondary implant<br />
insertion in partially integrated grafts tend to be aesthetically<br />
less satisfactory. Therefore, solid fixation<br />
and secure suturing are an absolutely prerequisite<br />
for successful bone grafting. At the same time, the<br />
insertion of the graft itself and its connection to<br />
the atrophied residual bone should be as easy as<br />
possible. The principles of functionally stable osteo -<br />
synthesis, which also apply to bone grafting, have<br />
been known for many years, even since before the<br />
introduction of enossal implants. These principles<br />
demand secure anchorage within the residual bone,<br />
while avoiding excessive compression of the graft<br />
at the transplant bed, which would entail the risk<br />
of fracture and, consequently, partial absorption or<br />
complete loss of the graft.<br />
Fig. 1 Intraoral appearance indicating severe atrophy. Fig. 2 Intraoperative presentation of the atrophied alveolar crest.
78 <strong>EDI</strong><br />
Product Studies<br />
Fig. 3 Fixation of the retromolar bone graft. Fig. 4 Presentation prior to suture closure.<br />
Fig. 5 Intraoral appearance after two months. Fig. 6 Presentation of the well-healed bone graft after three<br />
months.<br />
Fig. 7 Secondary implant insertion three months after block<br />
augmentation.<br />
In most cases, a small countersinking groove is<br />
reamed into the bone graft in the region of the sliding<br />
hole using a round burr to minimize the stress on<br />
the bone block graft at the level of the screw heads.<br />
This used to be the only method available to prevent<br />
the round screw from exerting excessive pressure<br />
during insertion of the graft. Alternative procedures<br />
without countersinking groove required the screw<br />
head to be left protruding and secured above the<br />
graft. For the surgeon, this situation presented the<br />
following dilemma: If screw heads were not countersunk,<br />
the soft-tissue treatment would be complicated<br />
by the protruding screw heads exerting additional<br />
Fig. 8 Implant reentry three months after insertion and six<br />
months after augmentation.<br />
pressure on the soft-tissue lobes. Taking neither<br />
measure would have resulted in a failed bone graft,<br />
because the screw head pressing on the graft would<br />
cause stress cracking within the graft, resulting in<br />
secondary absorption or failure, while the protruding<br />
screw head accompanied by heavier suturing would<br />
lead to suture dehiscence and, eventually, complete<br />
loss of the graft. The most straightforward way to<br />
resolve this was to cut a slight groove in the grafts<br />
with a round burr, minimizing the pressure on the<br />
graft and improving mucosal adaptation.<br />
With the osteosynthesis screws developed and<br />
supplied by Aesculap as part of their Ergoplant bone
2034-0906 © Directa AB<br />
79 79<br />
Fig. 9 iCAT volume tomography of the osseointegrated implant.<br />
fixation sets, there is now a titanium screw that has<br />
a very flat head but will still not shear off thanks to<br />
the strong material it is made of. The flat screw head<br />
minimizes the pressure on the bone graft without<br />
requiring the precaution of countersinking with a<br />
round burr. It also greatly simplifies soft-tissue management,<br />
as there will be less tension on the sutures<br />
caused by increased volume expansion. The micro -<br />
thread of the screw allows quick fixation, with only a<br />
few turns, even in very thin residual bone (Figs. 1 to 10).<br />
Dentists all over the world are<br />
using LUXATOR ® instruments<br />
as the preferred method of<br />
performing extractions.<br />
Implantology starts at<br />
the time of extraction!<br />
Easier for the dentist and dramatically less<br />
traumatic for patients and their dentition.<br />
<strong>EDI</strong> 79<br />
Product Studies<br />
The innovative head design of the new bone fixation<br />
screw together with its new microthread and its<br />
very robust titanium alloy facilitate predictable and<br />
successful osteosynthesis for securing bone grafts in<br />
place. For the implantologist performing augmentations,<br />
this means high-quality results through successful<br />
and stable osteosynthesis by a simpler and<br />
quicker procedure.<br />
Contact Address<br />
Dr Dr Andres Stricker<br />
Wessenbergstr. 6<br />
78462 Konstanz<br />
GERMANY<br />
Phone: +49 7531 917110<br />
Fig. 10<br />
Innovative<br />
design of the<br />
screw head.
80 <strong>EDI</strong><br />
Business & Events<br />
14 th Dentsply Friadent<br />
World Symposium<br />
in Barcelona<br />
Success is...<br />
It was another congress of superlatives. 2,500 atten-<br />
dees from more than 60 countries met in Barcelona<br />
on 19 and 20 March 2010. A pulsating city, more<br />
than 100 outstanding presentations and hands-on<br />
workshops – only a few of the impressions the participants took home with them after two days of scientific<br />
and technical deliberations. The scientific leaders were Prof Lim K. Cheung (Hong Kong), Dr Henry Salama<br />
(Atlanta, USA) and Prof Heiner Weber (Tübingen, Germany).<br />
“What we offer is not just implants. What we offer is<br />
dental solutions, from apex to cusp.” These were the<br />
words Dentsply Friadent Managing Director Dr Wer -<br />
ner Groll used to illustrate the symposium’s motto,<br />
“Focus on a Successful Practice”. But what is success?<br />
Safe and clinically successful treatments are as much<br />
a part of success as our knowledge about ongoing<br />
developments in oral implantology. Various fora and<br />
sessions offered first-hand information. In the<br />
“Proven Applications and New Approaches” forum,<br />
experienced practitioners presented practical treatment<br />
approaches and innovative procedures. In the<br />
“Today’s Progress for Tomorrow’s Practice” forum,<br />
speakers representing the research side gave their<br />
audience an impression of ongoing studies and scientifically<br />
founded developments. Interdisciplinary<br />
cooperation played a focal role at the congress. For<br />
example, interfaces with endodontics, periodontology<br />
or dental technology serve to link these disciplines<br />
into a broad and holistic implantological concept.<br />
So the “apex to cusp” motto that Dr Groll cited<br />
in his opening address was thoroughly confirmed as<br />
the congress went on.<br />
Timing, aesthetics, treatment protocols<br />
and risk management<br />
Keynote lectures highlighted four important factors<br />
of implantological success – timing, aesthetics, treatment<br />
protocols and risk management – on the basis<br />
of practical examples as well as against a scientific<br />
background. In his opening presentation, Prof Dennis<br />
Tarnow (USA) emphasized the points that are impor-<br />
tant for long-term success: In potential immediateplacement<br />
cases, extra attention should be paid to<br />
the status of the soft tissues and the buccal wall of<br />
the bone, which must be sufficiently well preserved.<br />
Dr Peter Gehrke (Germany) made a case for general<br />
and objective aesthetic parameters. More than<br />
80 percent of all patients consider aesthetics an<br />
important factor of success. Dr Marco Degidi and<br />
Prof Adriano Piattelli (Italy) presented their “chamber”<br />
constant. Under certain circumstances, as the<br />
chamber video impressively demonstrated, a threedimensional<br />
biological structure arises between<br />
the implant shoulder and the abutment. Dr Sanjay<br />
Sethi (United Kingdom) called for paying more<br />
attention to the biological consequences of treatment<br />
planning and to its financial consequences.<br />
Prof Wilfried Wagner (Germany) listed a number of<br />
anatomical, biological, aesthetic, surgical, prosthetic<br />
and mechanical risk factors along with suitable<br />
preventive measures.<br />
The afternoon’s Expert Talk before a tremendously<br />
interested public saw Dr Dietmar Weng, Dipl-Ing Holger<br />
Zipprich, Dr Marco Degidi, Dr Tord M. Lundgren,<br />
Prof Karl Andreas Schlegel and Prof Dennis Tarnow discuss<br />
the Tissue Care concept and the importance of<br />
primary stability. Given the different backgrounds of<br />
the panellists, it soon became obvious that important<br />
tendencies with regard to immediate loading<br />
and aesthetic long-term success should be given a<br />
closer and more differentiated look, requiring scientific<br />
evidence and enlarging our existing knowledge<br />
base. The Ankylos and Xive implant system support<br />
With more than<br />
2,500 attendees,<br />
the Dentsply<br />
Friadent World<br />
Symposium has<br />
become one of<br />
the world’s most<br />
important congresses<br />
in oral<br />
implantology.
&<br />
B E S T S O L U T I O N<br />
FOR IMPLANTOLOGY<br />
Powerful Surgical Unit with Illumination and Advanced<br />
Handpiece Calibration<br />
• Wide speed range of 200-40,000 min-1<br />
• Powerful torque: 5-50 Ncm<br />
• High power 210W<br />
• Lightweight compact body reduces hand fatigue and improves balance<br />
• Low noise, low vibration with minimal heat generation<br />
• Excellent durability<br />
• High torque accuracy<br />
A Powerful Ultrasonic Surgical System with Illumination<br />
• Power: superior cutting capability shortens treatment time<br />
• Visibility: optic handpiece assures safe, easy surgical procedures<br />
• Minimally invasive: eliminates heat generation during bone dissection<br />
• Safe: avoids damage to soft tissue even during accidental contact<br />
• Precision: cavitation effect of irrigation solution keeps surgical<br />
site blood free<br />
NSK Europe GmbH<br />
Elly-Beinhorn-Str. 8, 65760 Eschborn, Germany<br />
TEL : +49 (0) 61 96/77 606-0 FAX : +49 (0) 61 96/77 606-29<br />
w w w . n s k . c o m<br />
POWERFUL PARTNERS
82 <strong>EDI</strong><br />
Business & Events<br />
Prof Dennis Tarnow explaining the factors that are<br />
important for long-term success.<br />
two essential findings on long-term success by<br />
ensuring tissue preservation and predictable primary<br />
stability. The short introductory presentations by<br />
Weng, Zipprich and Degidi gave rise to an interesting<br />
discussion on the measurability and definition of two<br />
relevant core aspects of clinical long-term success.<br />
Biomaterials and implant design –<br />
what will the future bring?<br />
What new treatment options can we expect to see in<br />
the future, from a scientific point of view? Prof Karl<br />
Andreas Schlegel (Germany) believes that a biologically<br />
controlled bone augmentation process will<br />
become more important in the light of an aging<br />
patient population. Dr Christopher McCulloch (Canada)<br />
spoke on diabetes mellitus as an example of where<br />
optimized implant surfaces will permit implant<br />
treatment of patients for which it had previously<br />
been contraindicated. Dr Tord M. Lundgren (USA)<br />
showed how Ankylos implants can help avoid vertical<br />
bone loss in selected cases. And Dr Paul Weigl<br />
(Germany) demonstrated how short (8 mm) Ankylos<br />
implants could make bone augmentation in the<br />
posterior area dispensable.<br />
In times when problems become ever more complex<br />
and in which more and more materials and<br />
methods are extant, specialization alone can be<br />
counterproductive, as Dr Henry Salama (USA) and<br />
Dr Bernhard Saneke (Germany) underscored in their<br />
final presentation. Successful implant therapy requires<br />
interdisciplinary cooperation and networks consisting<br />
of experts from different fields. Cooperation is<br />
the only way to leverage the immense potential of<br />
modern technologies.<br />
Teamwork approach, personal meetings<br />
and hands-on workshops<br />
“Oral implantology needs dental technology” was<br />
the title of a separate forum – a title that would have<br />
been equally descriptive of both days of the symposium.<br />
It is rare that dental technologists play such an<br />
important role at an implantological congress. As<br />
usual, MDT Gerhard Stachulla confidentially moderated<br />
the presentations, of which the joint presentation<br />
by Carsten Fischer and Peter Gehrke may have<br />
been the most memorable. In the hands-on workshops,<br />
offered this year for the first time and<br />
completely sold out, participants were able to<br />
use anatomical preparations to learn more about<br />
augmentation techniques (Dr Thomas Hanser) and<br />
soft-tissue management (Dr Wolfram Hahn and<br />
Dr Stephan Klotz) and get some training in guided<br />
surgery using ExpertEase on real casts (Dr Fred<br />
Bergmann).<br />
The positive response on the part of the attendees<br />
convincingly attested to the quality of the speakers<br />
and the successful congress organization. Particularly<br />
agreeable were the prevailing neutral point of view<br />
and the independent nature of the information presented.<br />
The Dentsply Friadent World Symposium is<br />
an important implantological congress that has preserved<br />
its informal fabric despite its considerable<br />
size. Even before they left, many participants indicated<br />
that they would be attending the next World Symposium,<br />
which will be held in Hamburg on 16 and<br />
17 March 2012.<br />
Annett Kieschnick<br />
The scientific directors (left to right): Dr Henry Salama (Atlanta, USA), Prof Heiner<br />
Weber (Tübingen, Germany), Dr Werner Groll (Managing Director, Dentsply Friadent)<br />
and Prof Lim K. Cheung (University of Hong Kong).
Together as one<br />
SCANORA® 3D low dose digital<br />
cone beam unit featuring real<br />
panoramic imaging.<br />
Effective. Ergonomic. Versatile.<br />
Digital imaging made easy<br />
Effective<br />
Thanks to the focus on quality, ergonomy,<br />
workflow and low dose (ALARA*), with<br />
SCAnORA® 3D SOREDEX can offer you the<br />
most efficient and time saving tool to meet<br />
your daily diagnostic imaging tasks.<br />
Ergonomic<br />
Using a motorized chair not only improves<br />
patient comfort but ensures a stable and easy<br />
patient positioning while the ClearTouch<br />
control panel simplifies the operation.<br />
Versatile<br />
Multi-Volume (60 x 60 mm, 100 x 75 mm,<br />
145 x 75 mm and 145 x 130 mm) and real<br />
Panoramic Imaging. With this “Two in One”<br />
concept SCAnORA® sets a new benchmark<br />
to meet the daily diagnostic requirements of<br />
your professional environment.<br />
*ALARA principle - As Low As Reasonably<br />
Achievable dose<br />
www.soredex.com<br />
Manufactured by: SOREDEX<br />
P.O.Box 148 FI-04301 TUUSULA, FInLAnD<br />
info@soredex.com Tel. +358 10 270 2000<br />
SDX_<strong>EDI</strong>_210x297mm_March_2010.indd 1 23.2.2010 11:54:09
84 <strong>EDI</strong><br />
Business & Events<br />
ITI World Symposium 2010<br />
The Conversation of Geneva<br />
That the Swiss canton of Geneva is only small, made the ITI World Symposium seem only the bigger – the biggest and most<br />
successful in the history of the International Team for Implantology to date. Even though the first half of 2010 was speckled<br />
with congresses and conventions, dentists all over the world seem to be far from having enough of continuing education.<br />
And so, visitors from 82 countries ended up travelling to the ITI World Symposium in Geneva in April. What they saw was a<br />
congress of superlatives: almost 4,000 attendees, 113 speakers, an interesting and diverse schedule and, of course, the<br />
30 th anniversary of the ITI.<br />
The presentations were highly practical and were<br />
delivered in a professional manner. Dr Thomas von<br />
Arx (Berne, Switzerland) demonstrated his affinity<br />
both to implantology and to architecture. In his wellstructured<br />
presentation, he discussed the topic of<br />
localized bone defects, especially in buccal alveolar<br />
walls in the anterior region. The correct three-dimensional<br />
placement of an implant requires a certain<br />
amount of bone volume; however, this bone volume<br />
will not always be available due to changes the alveolar<br />
ridge has undergone following extractions,<br />
infection, trauma or malformation. To keep the number<br />
of surgical interventions as well as overall treatment<br />
time and cost at a minimum, implant placement<br />
should coincide, wherever possible, with the<br />
GBR (guided bone regeneration) measures taken.<br />
However, Dr von Arx strongly emphasized that certain<br />
criteria must be fulfilled for a single-set procedure<br />
to be successful. If primary implant stability<br />
cannot be achieved or if the implant cannot be positioned<br />
correctly, bone augmentation must precede<br />
implant placement with a sufficient margin. Other<br />
important criteria for treatment planning include<br />
the healing potential of the implant site and the<br />
patient’s general health.<br />
“As simple as possible. But not simpler<br />
than that.” (Albert Einstein)<br />
Dr Franck Renouard (Paris, France) had a question for<br />
the audience: “What is short, and what is not?” The<br />
implantologist in private practice reported on his<br />
clinical experience, highlighting treatment with<br />
short implants in particular, which he regretted were<br />
often still discussed mostly in terms of the disadvantages.<br />
He cited a number of arguments in favour of<br />
short implants, stressing that these implants may<br />
have a routinely good biomechanical prognosis.<br />
Recent publications have shown that in greatly atrophied<br />
bony implant beds, short implants can be more<br />
favorable than long implants in augmented bone. In<br />
addition, short implants provided added therapeutic<br />
ITI President<br />
Prof Daniel<br />
Buser (Berne,<br />
Switzerland) was<br />
impressed with<br />
the well-filled<br />
auditorium.
Dr Thomas von Arx<br />
Dr Stephen Chen Prof Matteo Chiapasco<br />
flexibility. So the question really is: “Why so much<br />
treatment complexity?” Dr Renouard proposed to<br />
redefine the concept of relative length as applied to<br />
crowns and implants. His explanation sounds plausible:<br />
Studies using the finite-element methods (FEM)<br />
have shown that loads always concentrate on the<br />
first three intraosseous millimetres of an implant.<br />
Hence, longer implants will not necessarily tolerate<br />
higher loads than shorter implants.<br />
“Knowledge is good. But skills are better.”<br />
(Emanuel Geibel)<br />
In a highly informative presentation, Dr Stephen Chen<br />
(Melbourne, Australia) presented the evidence for<br />
flapless procedures in the anterior region, taking a<br />
critical view of the growing enthusiasm for this therapeutic<br />
method. He shed some light on a number of<br />
recent clinical studies and performed a systematic<br />
analysis of the literature. The advantages of minimally<br />
invasive procedures with their benefits for the<br />
patient and the low level of intraoperative bleeding<br />
remain undisputed. But how about the claim that<br />
procedures will be shorter? Or, to cite Dr Chen’s words<br />
of warning: “If you do not fold back a flap, you will be<br />
groping in the dark.” To find the exact position for the<br />
implant in a flapless procedure, the bone must first be<br />
probed meticulously and the anatomical structures<br />
analyzed extensively. Dr Chen asked himself aloud<br />
whether the surgery really takes less time that way.<br />
He concluded that the flapless insertion of an implant<br />
requires a lot of experience, presence of cortical bone,<br />
a wide ridge and a fake gingival biotype. Flapless<br />
insertion is attractive, even seductive, for well-known<br />
and understandable reasons – but the technique has<br />
its limits, which the surgeon must be aware of.<br />
Prof Matteo Chiapasco (Milan, Italy) elaborated on<br />
the reconstruction of deficient bone volume in the<br />
posterior maxilla. His presentation gave an overview<br />
of the current literature and offered reliable information<br />
and sensible treatment standards for treating<br />
the atrophied posterior jaw. One of the issues Prof<br />
Chiapasco addressed was the surface texture of<br />
implants, which was also the focus of the entire sym-<br />
posium. Ever since ITI has presented its first evidence-based<br />
recommendations for insertion times at<br />
the 3 rd ITI Consensus Conference in 2003, implantologists<br />
actually have a decision tree they can follow.<br />
This year’s World Symposium only confirmed that<br />
the opinion leaders in oral implantology continue to<br />
agree on this issue.<br />
This was just a small peek at a comprehensive<br />
World Symposium programme, intended to demonstrate<br />
that the ITI is eminently practical while building<br />
on solid scientific foundations. The congress was<br />
highly convincing and once again demonstrated how<br />
important organizations such as the ITI are for dentistry.<br />
Medical research requires independence, open<br />
space and occasions for discussion.<br />
Networking meets implantology<br />
Congratulations! The International Team for Implantology<br />
is celebrating its 30 th birthday this year. The<br />
two most important initiators of this organization,<br />
founded in 1980, were Prof André Schroeder (Berne,<br />
Switzerland) and Dr Fritz Straumann (Waldenburg,<br />
Switzerland). Its goal was, and is, to bring together<br />
specialists and research experts in order to promote<br />
the field of oral implantology. Today, this organization<br />
can boast more than 8,000 members – and science,<br />
idealism and the well-being of the patient continue<br />
to be at the focus.<br />
André Schroeder Research Award<br />
<strong>EDI</strong> 85<br />
Business & Events<br />
At a ceremony on the occasion of the World Symposium<br />
of the International Team for Implantology (ITI),<br />
Beat Spalinger, President and CEO of Straumann,<br />
presented the André Schroeder Research award to<br />
Dr Maria Retzepi for her study entitled “The Effect of<br />
Experimental Diabetes on Guided Bone Regeneration”,<br />
in which she examined the effects of controlled<br />
and uncontrolled diabetes on intracellular processes<br />
and on cellular genetic profiles during the healing<br />
process subsequent to guided bone regeneration.<br />
With the World Symposium in Geneva, the Inter -<br />
national Team for Implantology has made itself an<br />
impressive birthday present, confirming the ITI<br />
hypothesis that the need for evidence-based research<br />
and implantological training and continuing education<br />
is far from being fully satisfied. A great number of<br />
satisfied attendees, top-notch presentations and interesting<br />
discussions made this meeting and all-round<br />
success – although a certain volcano on Iceland made<br />
getting home a difficult task for not so few.<br />
Annett Kieschnick
86 <strong>EDI</strong><br />
Business & Events<br />
Osteology Symposium Baden-Baden 2010<br />
For the Patient’s Benefit<br />
The 3 rd National Symposium of the Osteology Foundation took place on 19 and 20 March 2010. More than 500 interested<br />
dentists had assembled in Baden-Baden to learn more about which new concepts for the regeneration of hard and soft tissues<br />
are of importance for clinical practice. We are looking at a minimally invasive future with less stress for the patient during<br />
surgical interventions. To some extent, this development is already happening.<br />
On Friday, 15 workshops forged a link between theory<br />
and practice. On Saturday, the theme was further<br />
expanded on in a series of scientific and clinical<br />
presentations by internationally renowned speakers.<br />
The most important innovation presented at the<br />
3 rd Osteology Symposium is probably a collagen<br />
matrix “straight from the blister pack”, currently<br />
approved for covering recession areas. Depending<br />
on the clinical baseline situation, the harvesting procedure<br />
otherwise required for this indication may<br />
become dispensable.<br />
Current trends in soft-tissue replacement<br />
Prof Mariano Sanz (Madrid, Spain) held a presentation<br />
on options for soft-tissue regeneration and the<br />
preservation of keratinized gingiva. He contrasted the<br />
classic mucosal transplant with its alloplastic alternatives<br />
including a human skin matrix from cadaver<br />
donors and a soft-tissue replacement material based<br />
on a 3D collagen matrix of porcine origin. According<br />
to recent study results, the 3D collagen matrix is a<br />
promising alternative to – or even superior to – the<br />
classic mucosal transplant and the coronally repositioned<br />
flap (Allen technique) in terms of inflammation,<br />
recession and keratinized-mucosa gain. Advantage<br />
cited was the significantly lower patient morbidity<br />
that was owed to the absence of a separate<br />
procedure for harvesting the connective-tissue transplant.<br />
Prof Sanz believes that alloplastic soft-tissue<br />
replacement will become a standard in oral reconstructive<br />
surgery.<br />
Prof Christoph Hämmerle (Zürich, Switzerland)<br />
summarized the topic of socket management following<br />
tooth extractions. He pointed out that not even<br />
immediate placement of implants and fresh extraction<br />
sockets can prevent bone loss. Introducing<br />
bovine biomaterials into the socket, by contrast, preserves<br />
soft tissue for subsequent plastic coverage. In<br />
addition, there are more and more indications that<br />
the contour of the alveolar ridge may be preserved<br />
if a suitable technique is used. An ongoing study<br />
performed by Prof Hämmerle’s Zürich workgroup<br />
compares the clinical hard- and soft-tissue volumes<br />
following socket or ridge preservation procedures.<br />
Dr Markus Schlee (Forchheim, Germany) also<br />
addressed the topic of future trends in soft-tissue<br />
replacement, especially for recession coverage. Longterm<br />
stability, he reported, is contingent on adequate<br />
tissue thickness. Dr Schlee also mentioned that gingi-<br />
Prof Jürgen Becker and... ... Prof Christoph Hämmerle<br />
presided over the scientific<br />
part of the symposium.<br />
Most of the work -<br />
shops included<br />
hands-on exer -<br />
cises on animal<br />
preparations,<br />
forging a good<br />
link between<br />
theory and<br />
practice.
Implant Direct
88 <strong>EDI</strong><br />
Business & Events<br />
val thickness is dependent on the apical base and<br />
on the inclination of the tooth, where a predictable<br />
result presupposes complete coverage of the transplant<br />
or matrix introduced.<br />
Prof Karl-Ludwig Ackermann (Filderstadt, Germany)<br />
presented various clinical cases to demonstrate available<br />
options in soft-tissue surgery in the aesthetic<br />
zone, the relevant surgical techniques and their<br />
chances and limits as a function of the prevailing<br />
indication. Any surgical intervention constitutes an<br />
intentional local trauma. Trauma-related postoperative<br />
changes should therefore be invisible and not<br />
limiting to the patient as well as ethically acceptable<br />
in the light of the resulting benefits.<br />
Novel concepts in bone regeneration<br />
The second section of the day entitled “Novel concepts<br />
in bone regeneration” was opened by Prof Rai -<br />
ner Schmelzeisen (Freiburg, Germany) with a forwardlooking<br />
discussion of the clinical state of the art in<br />
bone marrow aspiration. In the light of the emerging<br />
potential of stem cells retrieved from bone marrow<br />
aspirate to be used in bone augmentation procedures,<br />
his verdict was critical when it came to autologous<br />
bone – until now considered the gold standard.<br />
By obtaining stem cells from a conventional blood<br />
sample, patient comfort could be improved compared<br />
to the harvesting of autologous bone from a<br />
separate donor site.<br />
Dr Daniel Thoma (Zürich, Switzerland) reported on<br />
the use of growth factors in localized bone regeneration,<br />
citing a combination of rhBMP-2 or rhPDGF<br />
(osteoinductive growth factors) with mechanically<br />
stable osteoconductive grafts such as DBBM or allografts<br />
as the most promising method. However, there<br />
are as yet no clinical studies evaluating a combination<br />
of rhBMP-2 and appropriate carrier materials –<br />
especially when used to block transplants – in more<br />
complex defect situations.<br />
Successful peri-implantitis therapy<br />
Prof Andrea Mombelli (Geneva, Switzerland) gave an<br />
overview of diagnostic procedures for the prevention<br />
of periodontitis and peri-implantitis, with special<br />
attention to an evaluation of the diagnostic benefits<br />
of the procedures presented.<br />
An overview of therapeutic concepts and regenerative<br />
periodontal therapy was given by Prof Anton<br />
Sculean (Berne, Switzerland) who demanded human<br />
histological evidence for the use of materials, especially<br />
with regard to periodontal regeneration; this<br />
evidence was still lacking for alloplastic materials<br />
such as bioactive glass.<br />
The 3 rd National Osteology Symposium was a success for everyone attending.<br />
Based on in-depth science and exciting clinical data, top-notch presenters explained<br />
concepts and treatment approaches.<br />
The scientific program concluded with the presentation<br />
by Dr Frank Schwarz (Düsseldorf, Germany) on<br />
current approaches to peri-implantitis therapy as<br />
employed at the dental clinic of the University of<br />
Düsseldorf. The results showed that non-surgical<br />
treatment approaches in periodontitis (laser or<br />
curette) in combination with antibiotic therapy must<br />
be considered ineffective in terms of long-term treatment<br />
success due to a lack of new bone formation<br />
and reossification. A classification of cases as low,<br />
medium or high risk helps guide the choice of surgical<br />
intervention performed, taking both systemic and<br />
local factors into account. Implants are cleaned using<br />
plastic curettes, cotton pellets and saline solution.<br />
Subsequent treatment options, according to Schwarz,<br />
include implantoplasty (for the supracrestal aspects<br />
of the defect, present in approximately 80 percent<br />
of all cases), augmentation (for the intraosseous<br />
aspects of the defect), and additionally the use of the<br />
laser (for supraosseous aspects of the defect greater<br />
than 1 mm with buccal dehiscences or a circumferential<br />
intraosseous bone defect).<br />
The 3 rd National Symposium of the Osteology Foundation<br />
showed the participants how to implement<br />
the most recent scientific findings in clinical practice.<br />
The more than 500 attendees at the congress itself<br />
and the more than 300 participants of the workshops,<br />
all of which were sold out, appreciated the<br />
lively and relevant discussions and the very suitable<br />
overall format.<br />
Dr Barbara Paleska
90 <strong>EDI</strong><br />
Business & Events<br />
1500 professionals at the Sixth Mozo-Grau Update Congress on Implantology<br />
Update on Implantology<br />
The 2010 Sixth Update Congress on Implantology<br />
attracted over 1500 attendees from more than<br />
ten countries to IFEMA Southern Auditorium in<br />
Madrid, Spain, on 19 and 20 February.<br />
Close to 50 expert presenters guided the attendees<br />
through the main and research programmes.<br />
Acknowledging that the best way to learn is to practise,<br />
limited-attendance courses were organised on<br />
implantology for newcomers as well as on sinus lifts<br />
and bone grafts.<br />
One focus of the main programme was on specialcare<br />
patients, a highlight being the presentation by<br />
Dr Rafael Martín-Granizo, President of the Spanish<br />
Oral and Maxillofacial Surgery Society (SECOM), on<br />
implant treatment for patients under bisphosphonate<br />
medication – a highly topical issue.<br />
Dr Miguel Peñarrocha, Director of the Department<br />
of Oral Surgery of Valencia University, focused on<br />
implant treatment for special-care patients with systemic<br />
diseases.<br />
Prof Carlos Navarro Vila, Director of the Department<br />
of Oral and Maxillofacial Surgery at Complutense University<br />
(Madrid), presented a study on oral rehabilitation<br />
with a success rate of 92.9 percent osseointegrated<br />
implants in oncologic patients treated at the<br />
Department of Maxillofacial Surgery of the Gregorio<br />
Marañón General University Hospital, where he heads<br />
the Department of Maxillofacial Surgery.<br />
Another segment of the main programme<br />
addressed immediate loading. Dr Juan Antonio<br />
Hueto, Titular Doctor at the Oral and Maxillofacial<br />
Surgery Service at the Vall D´Hebró Hospital,<br />
Barcelona, gave practical advice related to this field.<br />
He also supervised a practical workshop on sinus<br />
lifts.<br />
The congress’s Scientific Committee commented<br />
on the unprecedented attendance: “Mozo-Grau continues<br />
to be one of the fastest-growing implant companies<br />
in Spain. The presentations and attendance<br />
are indicative of our interest in research, and we<br />
would like to thank everyone for attending.”<br />
The research programme – where universities, hospitals<br />
and doctors could present the results of their<br />
ongoing research with Mozo-Grau products – was a<br />
remarkable success.<br />
More than 1500<br />
professionals<br />
attended the<br />
Sixth Mozo-Grau<br />
Update Congress<br />
on Implantology<br />
in Madrid.<br />
Course organized<br />
for the surgical<br />
assistant team.
<strong>EDI</strong> 91<br />
Business & Events<br />
International Osteology Symposium,<br />
Cannes, April 14 to 16, 2011<br />
Focussing on<br />
Regenerative<br />
Dentistry<br />
The Osteology Symposium is the only international<br />
congress series that focuses on the key subject of<br />
regeneration. After successful conferences in Lucerne<br />
and Monaco the next International Osteology Sympo-<br />
sium will take place in Cannes on April 14 t0 16, 2011.<br />
In line with the congress title, Clinical Excellence, Risk<br />
Factors and Complications in Regenerative Dentistry,<br />
experienced researchers and well-known practitioners<br />
will discuss the latest clinical innovations,<br />
research results and current treatment concepts.<br />
The Pre-Symposium on Thursday will be entirely<br />
practice-oriented. In different workshops the participants<br />
will be able to broaden their theoretical and<br />
practical knowledge in different fields of regenerative<br />
dentistry (soft tissue management, concepts of<br />
bone regeneration, advanced suturing techniques,<br />
etc.).<br />
The International Osteology Symposium in Cannes<br />
will again link high-quality science with the de -<br />
mands of dental practice on one of Europe’s most<br />
beautiful coastlines.<br />
More Information and Registration<br />
Osteology Foundation<br />
www.osteology-cannes.org
92 <strong>EDI</strong><br />
Business & Events<br />
Straumann launches digital solutions platform<br />
Connecting Dental<br />
Professionals across Disciplines<br />
At the Chicago Dental Society Midwinter Meeting, one of America’s largest dental exhibitions, Straumann<br />
presented an array of integrated computer-based technologies that have been designed to increase confidence,<br />
safety, precision and reliability in implant and restorative dentistry.<br />
Under the new umbrella brand of ‘Straumann Digital<br />
Solutions’, the company now offers state-of-theart<br />
computer-guided surgery, intra-oral scanning,<br />
and CAD/CAM prosthetics to specialists, general<br />
dentists and dental laboratories in various markets<br />
around the world. With these innovations in intraoral<br />
scanning, CAD/CAM and computer guided surgery,<br />
a complete Straumann tooth – from implant to<br />
final crown – is now available from a single provider.<br />
Straumann’s integrated state-of-the-art digital solutions<br />
now support implant placement, restoration<br />
and esthetic performance.<br />
Gilbert Achermann, President and CEO, commented:<br />
“Digitalization will impact all aspects of dentistry<br />
as digital workflows supersede labor-intensive<br />
manual processes, enhancing interfaces, shortening<br />
treatment, reducing potential for error and<br />
improving quality assurance. These benefits are<br />
expected to translate into lower treatment costs,<br />
added convenience and improved comfort for<br />
patients. Straumann is committed to bringing the<br />
new technologies to customers as part of an integrated<br />
array of flexible, reliable solutions that are<br />
designed to optimize workflows and enhance<br />
patient care.”<br />
A major drawback facing dental professionals<br />
wishing to invest in digital applications is that<br />
equipment, such as scanners, surgical guides etc.,<br />
has to be sourced from a variety of manufacturers<br />
without standardization, or is part of a closed system<br />
offered exclusively by a single provider. Customers<br />
therefore face being ‘locked in’ or having flexibility<br />
without full assurance of connectivity, quality and<br />
comprehensive support services. Straumann Digital<br />
Solutions offer the flexibility of state-of-the-art systems<br />
together with seamless connectivity to one of<br />
the world’s leading implant, restoration and regenerative<br />
systems, in addition to guaranteed Straumann<br />
quality, service and network support.<br />
Computer-guided surgery<br />
The combined use of 3D imaging digital design software<br />
to plan and execute precise implant placement<br />
is an emerging trend. Using a computed tomographic<br />
image of the patient’s jaw, the dental surgeon plans<br />
the position, angulation and depth of the implant on<br />
a computer using sophisticated planning software.<br />
The data are then used to produce a plastic surgical<br />
template that fits onto the patient’s teeth or gum.<br />
The template incorporates sleeves that guide drills,<br />
taps and profilers, designed for optimal implant<br />
placement. Computer-guided surgery is designed to<br />
offer the dentist a clear view of the bone condition,<br />
the position of nerve and vascular structures, and the<br />
final implant location. It simplifies the planning and<br />
execution of complex procedures, which can reduce<br />
the risk of surgical and prosthetic complications.<br />
Straumann entered this exciting field in 2009<br />
through the acquisition of the dental business of IVS<br />
Solutions AG, a German company specializing in software<br />
applications for computer-guided surgery,<br />
including surgical template design and fabrication.<br />
Straumann is rolling out the technology internationally,<br />
announcing that it will be available in North<br />
America in the course of this year.<br />
In addition to the benefits of user-friendliness and<br />
predictability, Straumann’s guided surgery system<br />
offers ‘open-system’ flexibility as the templates can<br />
be produced quickly and efficiently in local laboratories<br />
rather than exclusively by a central supplier. Furthermore,<br />
Straumann’s comprehensive instrument<br />
kit can be used with any Cone Beam CT scanner and<br />
can be used with other implant libraries.<br />
Powerful intra-oral scanning<br />
Straumann also announced that its CAD/CAM service<br />
is now connected to Cadent’s iTero intra-oral scanning
system. Intra-oral scanning enables the dentist to create<br />
a 3D image of the patient’s teeth using a digital<br />
scanner inside the mouth. Replacing the slower conventional<br />
process of impression-taking in the dental<br />
practice and model casting in the laboratory, digital<br />
intra-oral scanning is designed to deliver considerable<br />
time and cost savings – as well as high precision – for<br />
both the lab and the dental practice.<br />
In addition to the data sharing-agreement that connects<br />
the two companies’ systems, Straumann has<br />
exclusive distribution rights for Cadent’s iTero scanning<br />
system in Europe and offers European dentists leading<br />
intra-oral scanning technology as part of its integrated<br />
range of solutions. The iTero scanner is designed to be<br />
easy to use and convenient because it eliminates prescan<br />
coating of teeth.<br />
Advanced CAD/CAM technology<br />
Modern dental prosthetic inlays, onlays, crowns, and<br />
bridges are best designed by computer (CAD) and<br />
milled on computerized machines (CAM). This procedure<br />
is considerably more efficient than traditional<br />
processes and can be highly profitable for dental<br />
laboratories. Central milling of CAM prosthetics on<br />
industrial machines offers a high level of precision<br />
and reliability. Straumann provides a comprehensive<br />
CAD/CAM prod uct portfolio including scanners, soft-<br />
Materialise Dental focuses on 3D Digital Dentistry,<br />
offering a range of solutions for computer guided<br />
dentistry. Its SimPlant software is compatible with all<br />
implant brands and CT and cone-beam 3D scanners,<br />
thus providing clinicians the opportunity to stay with<br />
their own implant brands and scanning equipment.<br />
The newly established cooperation between Materialise<br />
Dental and Cefla Dental Group and QR srl<br />
is non-exclusive and offers customers of the two latter<br />
companies the possibility to have SimPlant Pro<br />
pre-installed on the cone-beam workstations upon<br />
<strong>EDI</strong> 93<br />
Business & Events<br />
ware and a full range of prosthetics in modern biocompatible,<br />
durable and esthetic materials, including<br />
polymer, metals and ceramics. Through its partnership<br />
with Ivoclar Vivadent, Straumann also offers<br />
high-performance glass ceramics for high-end<br />
esthetic restorations that are designed to be indistinguishable<br />
from natural teeth.<br />
The new advanced CAD/CAM system includes a<br />
new scanner, which will be capable of scanning solid<br />
master, section-cut and antagonist models. One<br />
small practical feature is an integrated web-camera<br />
to facilitate a new level online service support.<br />
Because design software is a key component in<br />
CAD/CAM, Straumann regularly releases upgrades to<br />
its installed scanner base. The latest ‘5.0 IO’ upgrade<br />
includes a number of new features that improve<br />
workflows and functionality.<br />
Apart from the new scanning capabilities, software<br />
and materials, Straumann will launch a number of<br />
additional CAD/CAM features this year, including<br />
veneers, inlays and onlays.<br />
More Information<br />
Institut Straumann AG<br />
Peter Merian-Weg 12<br />
CH-4052 Basel · SWITZERLAND<br />
www.straumann.com<br />
Materialise Dental NV collaborates with Cefla Dental Group and QR srl<br />
Cooperation Established<br />
Materialise Dental has established a cooperation with Cefla Dental Group and QR srl to pre-install SimPlant<br />
Pro on their cone-beam 3D scanning equipment.<br />
purchase of a NewTom (NewTom 9000, 3G, VGi) or<br />
MyRay (SkyView) cone-beam 3D scanner.<br />
More Information<br />
Materialise Dental NV – Headquarters<br />
Technologielaan 15<br />
3001 Leuven<br />
BELGIUM<br />
Phone: +32 16 396620<br />
simplant@materialise.be<br />
www.materialisedental.com
94 <strong>EDI</strong><br />
Business & Events<br />
Manufacturer of disposable medical devices celebrates anniversary<br />
Twenty Years of Omnia<br />
Omnia, the name of the resulting company – now<br />
considered the market leader in Italy and throughout<br />
Europe, represented in more than 40 countries – is<br />
Latin for “everything” and reflects the company’s mission:<br />
Everything is possible. The company has taken a<br />
close look at the way surgical and implant dentists<br />
work in order to identify the specific requirements of<br />
sterile devices in dentistry.<br />
“Back in the old days, treatment providers often<br />
rejected extensive sterile precautions, feeling that<br />
there is nothing much to be kept sterile in the mouth<br />
anyway”, reports Alexander Keim, Sales Manager at<br />
Omnia. It is true that the oral environment is fairly<br />
tolerant of challenges, but today’s dental treatment<br />
methods have reached a critical limit that not even<br />
the proverbially good self-healing capacity of the<br />
mouth can cope with.<br />
A hospital’s operation theater is a completely different<br />
setting from a dental surgery. While in an operation<br />
theater, several assistants perform the necessary<br />
preparatory steps in a controlled anteroom to<br />
help prevent infection, both the treatment provider<br />
and his or her assistant in the dental surgery generally<br />
operate in an uncontrolled environment. “Some<br />
of the precautions you can take are very simple. For<br />
example, you can fold a wrapper such that an assistant<br />
– who like everyone else has only two hands –<br />
can open it without touching the sterile device<br />
inside.”<br />
At Omnia, consistent specialization has resulted<br />
in an enormous accumulation of competence. The<br />
cleanroom technology employed at the separate<br />
production sites for non-wovens in Fidenza near<br />
Parma and plastic products near Mantua matches<br />
microchip production environments. A large number<br />
of custom surgical sets is available, which makes for<br />
a high degree of complexity in production. These custom<br />
surgical sets are a unique characteristic of the<br />
Many dental treatment providers attempt to prepare for their increasingly demanding surgical<br />
procedures by selecting their surgical materials from among those in common use in hospitals –<br />
which works, in a way, but certainly not too well. Then, twenty years ago, Lauro Cereoli in Italy<br />
had an idea: He decided to apply medical standards to the dental environment and to take<br />
a close look at the specifics of the dental surgery in terms of which product features can be<br />
dispensed with and which features are very special and highly important.<br />
Omnia range of products. They complement the<br />
many standard dental sets developed by cooperation<br />
with dental experts and opinion leaders – names like<br />
Massimo Simion, Tiziano Testori, Ferdinando D’Avenia<br />
and Mauro Labanca speak for themselves. Sets may<br />
be customized for individual surgeries, treatment<br />
providers or even procedures and will usually be<br />
delivered in sterile condition within a record 30 days.<br />
“This reduces the number of parts that end up being<br />
discarded unused and simplifies the procurement<br />
logistics. Each treatment provider can receive a surgical<br />
set that is tailored to his or her treatment environment<br />
and methods. The higher price paid for custom<br />
solutions is more than made up for by better<br />
economy and time savings”, says Alexander Keim.<br />
“The introduction of consistent quality management<br />
regime in dental offices throughout Germany will<br />
make the cost situation much more transparent;<br />
dentists are in for quite a few surprises in the field of<br />
infection control and instrument reprocessing”,<br />
Francesca Isi, Distribution Management at Omnia,<br />
adds. “Those who attend our seminars usually quickly<br />
realize the ergonomic and economical benefits<br />
of custom surgical sets.” Omnia in bonum – all the<br />
best – for the next twenty years!<br />
STE<br />
Alexander Keim,<br />
Sales Manager,<br />
and Francesca Isi,<br />
Distribution<br />
Management<br />
at Omnia
New General Manager for Germany,<br />
Austria and Switzerland<br />
<strong>EDI</strong> 95<br />
Business & Events<br />
Dr Berthold Reusch<br />
Takes over<br />
Materialise Dental has appointed Dr Berthold Reusch as General<br />
Manager for Germany, Austria and Switzerland. He brings over 17 years<br />
of global marketing, sales, clinical and business management<br />
experience in the field of dental materials and digital dentistry.<br />
Most recently, Reusch worked for<br />
the dental division of 3M Espe<br />
where he was Director of Operations<br />
for the digital imaging<br />
device business which he successfully<br />
developed outside the U.S.<br />
From 2007 to 2009 he was a<br />
member of the executive management<br />
team of Brontes Technologies,<br />
a 3M company based in<br />
Boston, MA, building the digital<br />
impressioning business in the U.S.<br />
As General Manager at Materialise<br />
Dental GmbH, Reusch and<br />
his team will further develop the<br />
SimPlant and SurgiGuide business<br />
within the German, Austrian<br />
and German-speaking Swiss<br />
markets.<br />
Reusch received his diploma<br />
and PhD (Dr rer nat) in Physics<br />
from the University of Tubingen,<br />
Germany, and then went on to<br />
receive his MBA, with an emphasis<br />
on marketing and international<br />
business management, from the<br />
Business School at the Catholic<br />
University of Eichstätt.<br />
When asked about his new<br />
position, Dr Berthold Reusch said,<br />
“I’m very enthusiastic to join<br />
Materialise Dental, an innovative<br />
and technologically driven organ-<br />
Dr Berthold Reusch<br />
ization. I’m looking forward to<br />
undertaking the challenging task<br />
of heading my division and –<br />
together with my team – offering<br />
our customers the most innovative<br />
and advanced products to<br />
meet their computer-guided im -<br />
plant dentistry needs.”<br />
More Information<br />
Materialise Dental NV –<br />
Headquarters<br />
Technologielaan 15<br />
3001 Leuven<br />
BELGIUM<br />
Phone: +32 16 396620<br />
simplant@materialise.be<br />
www.materialisedental.com<br />
SINUS<br />
RETRACTORS<br />
ACC. TO PROF. (NYU) DR. MED. DENT.<br />
MANFRED LANG<br />
Clinical Associate Professor<br />
Department of Implant Dentistry, New York University<br />
· retraction of the mucoperiosteal flap during<br />
lateral sinus window preparation<br />
· mucoseal flap is secured by the “shark-teeth”<br />
· designed asymmetrically, right and left version<br />
· also suitable for retraction in the<br />
anterior region<br />
· anatomical handle ensures only moderate<br />
retraction force<br />
· patent pending<br />
Bodenseeallee 14-16<br />
78333 Stockach Germany<br />
Tel. +49 7771-64999-0<br />
Fax +49 7771-64999-50<br />
www.kohler-medizintechnik.de
96 <strong>EDI</strong><br />
Product Reports<br />
Planmeca launches a 3D face photo system and a new 3D imaging field size<br />
New Members for the<br />
3D Imaging Product Family<br />
To fulfil the most diverse diagnostic needs of today’s dental professionals, Planmeca’s recognised 3D imaging concept has<br />
grown with two new products. Planmeca ProMax 3D ProFace is a CBVT imaging unit with integrated 3D face scan system,<br />
a true 3D application of the future. Planmeca ProMax 3D Mid introduces an extended selection of 3D volume sizes combined<br />
with traditional 2D panoramic and cephalometric imaging.<br />
Both products are based on the acknowledged Planmeca<br />
ProMax platform making future upgrades<br />
extremely simple. Planmeca ProMax 3D ProFace, the<br />
CBVT unit integrated face scan, produces a realistic<br />
3D face photo in addition to traditional digital maxillofacial<br />
radiography. Planmeca is the first to introduce<br />
this type of concept. The lasers scan the facial<br />
geometry and the digital cameras capture the<br />
colour texture of the face. One scan generates both<br />
a 3D photo and a CBVT volume, or if required solely a<br />
3D photo, in which case no radiation is emitted.<br />
3D photo visualises soft tissue in relation to dentin,<br />
providing an effective follow-up tool for maxillofacial<br />
operations. As Planmeca ProMax 3D ProFace acquires<br />
both a CBVT image and 3D photo in a single scan, the<br />
patient position, facial expression, and muscle position<br />
remain unchanged, resulting in perfectly compatible<br />
images. Operation preplanning, where the<br />
medical professional may study the face anatomy in<br />
detail, facilitates a careful operation and enhances<br />
the aesthetic results.<br />
Another novelty introduced is Planmeca ProMax<br />
3D Mid offering an extended selection of volume<br />
choices to optimise imaging areas according to specific<br />
diagnostic tasks, all while complying Planmeca’s<br />
strong commitment to the ALARA (as low as reasonably<br />
achievable) principle to minimise radiation. With<br />
Planmeca ProMax 3D Mid, an optimal volume size is<br />
available for every application, e.g. for endodontics<br />
requiring high resolution, for implantology requiring<br />
images with a smaller field of view, and for orthodontics<br />
requiring large image sizes – without compromising<br />
the best practices of dentistry. It is also capable<br />
of acquiring traditional panoramic and cephalometric<br />
images.<br />
The existing products in Planmeca’s 3D concept<br />
are Planmeca ProMax 3D s, ideal for applications<br />
where a smaller field of view is sufficient, Planmeca<br />
ProMax 3D, for general 3D applications with a field<br />
size covering the mandible and maxilla, and Planmeca<br />
ProMax 3D Max offering field sizes from a single<br />
tooth to the whole maxillofacial area.<br />
More Information<br />
Planmeca Oy<br />
Asentajankatu 6<br />
00880 Helsinki . FINLAND<br />
Phone: +358 20 7795-500<br />
www.planmeca.com<br />
The product information produced here editorially is based on information<br />
provided by the manufacturer and has not been checked by the editor<br />
for its accuracy.
Get it!<br />
Fax +49 8243 9692-22<br />
teamwork media GmbH<br />
Hauptstr. 1,<br />
86925 FUCHSTAL<br />
GERMANY<br />
Phone +49 8243 9692-0<br />
Fax +49 8243 9692-22<br />
service@teamwork-media.de<br />
www.teamwork-media.de<br />
<strong>EDI</strong><br />
Yes, I sign up for a 1-year subscription to <strong>EDI</strong> Journal (4 issues) for only € 40,– (incl. shipping and VAT in<br />
Germany). For readers outside Germany the annual subscription is € 58,– . The subscription period will automatically<br />
renew for a successive one (1) year unless cancelled by the subscriber 8 weeks before the end of the<br />
related subscription term.<br />
Name<br />
Street<br />
Country / Post Code / Town<br />
Phone / Fax<br />
Date / 1. Signature<br />
I am aware of having the right to cancel this subscription order up until two weeks upon receipt of the order<br />
confirmation. In order to cancel it is sufficient to send a written note to: teamwork media GmbH, Hauptstr. 1,<br />
86925 Fuchstal, Germany. I confirm being aware of it with my 2. signature.<br />
Date / 2. Signature<br />
<strong>EDI</strong> Journal is the first and only European professional<br />
journal of its kind, written for all clinicians with distinct<br />
interest in dental implantology. This publication aims<br />
at uniting European dentistry in a common effort, to<br />
establish appropriate standards and to help open up<br />
new markets.<br />
The specific dental section of this periodical offers a<br />
wealth of original work, case reports, scientific research<br />
and other articles presented by authors from countries<br />
all over Europe, all helping to make this top-quality<br />
platform a truly international voice in the dental<br />
profession. Product innovations are covered in depth.<br />
And for the first time ever, dental implantologists are<br />
offered exhaustive information on important ancillary<br />
themes such as European standards, quality guidelines,<br />
legal issues, questions of remuneration and professional<br />
specialization.<br />
Information on upcoming events of importance to dental<br />
implantology and on training, continued education and<br />
professional growth opportunities are also regular<br />
features of <strong>EDI</strong> Journal.<br />
<strong>EDI</strong> Journal<br />
ISSN 1862-2879<br />
European Journal for<br />
Issue 1/2008 Vol. 4<br />
Dental Implantologists<br />
TOPIC<br />
Implantation in the<br />
Atrophied Jaw<br />
Placing implants in atrophic jaws without<br />
grafting procedures<br />
»<strong>EDI</strong> News: European Consensus Conference: Guidelines on Peri-implantitis · BDIZ <strong>EDI</strong><br />
Expert Symposium on Peri-implantitis in Cologne · European Committee Meeting with<br />
Focus on Postgraduate Education · Risk Management Topic at the Second Mediterranean<br />
Symposium of BDIZ <strong>EDI</strong> on Crete · Dental Implantology in Turkey »European Law:<br />
Prohibition of Age Discrimination »Case Studies: Implantation in the Atrophied Jaw ·<br />
“A Completely New Feeling!” »Product Studies: Healthy and Stable · The Reverse Abutment ·<br />
TINY Implants »Product Reports: Clinical Realities with Astra Tech BioManagement Complex<br />
Journal
98 <strong>EDI</strong><br />
Product Reports<br />
Porous titanium granules by Tigran<br />
Successful<br />
Dental Bone Regeneration<br />
The following article presents different indications for Tigran porous titanium granules in dental bone<br />
regeneration.<br />
Sinus lift<br />
A sinus lift makes it possible for edentulous patients<br />
with insufficient mandibular bone volume to receive<br />
dental implants. Tigran porous titanium granules are<br />
placed at the sinus floor to promote new bone formation.<br />
Sinus lifts can be completed in one or two steps.<br />
With the one-step method, the implant is placed intrasurgically.<br />
With the two-step method, new bone is first<br />
generated at the sinus floor before inserting the<br />
implant during a second procedure six to nine months<br />
later. In both cases, the implant can normally be loaded<br />
between three and six months after insertion.<br />
1 2<br />
3 4<br />
Fig. 1 Five years after insertion of the dental prosthesis, the<br />
fixture has become mobile, likely due to excess stress.<br />
Fig. 2 The fixture is removed and the cavity of the fixture<br />
widened and filled with titanium granules. A new fixture<br />
is then screwed into place. At the same time, a sinus lift is<br />
performed at site 14 and a new fixture installed.<br />
Fig. 3 Clinical situation two years after delivery of the new<br />
restoration.<br />
Fig. 4 Radiograph two years after delivery of the new<br />
restoration.<br />
The study “Porous titanium granules used as osteo -<br />
conductive material for sinus floor augmentation: a<br />
clinical pilot study” by Hans Bystedt and Lars Rasmusson<br />
shows that porous titanium granules effectively promote<br />
bone regeneration in conjunction with implant<br />
placement. Their study is followed up by an international<br />
multicentre study aimed at showing that titanium<br />
granules can trigger bone regeneration in connection<br />
with immediate implant placement.<br />
Filling alveolar sockets<br />
An extraction often leads to local resorption of the<br />
alveolar ridge – especially of the buccal bone sections.<br />
This may lead to functional and aesthetic<br />
problems with tooth- or implant-supported dental<br />
prostheses.<br />
Tigran has conducted a number of experiments on<br />
animals showing that an extraction socket filled with<br />
Tigran porous titanium granules will preserve the<br />
volume of the alveolar ridge, resulting in a more predictable<br />
implant treatment and an aesthetically<br />
more attractive result. A study involving 60 patients,<br />
begun in Israel in early 2010 under the direction of<br />
Adi Lorean and Ziv Mazor, aims to show that the titanium<br />
granules can also help preserve and regenerate<br />
the bony walls of alveolar sockets.<br />
5 6<br />
7 8<br />
Fig. 5 Extraction socket.<br />
Fig. 6 Socket filled with titanium granules.<br />
Fig. 7 Inserting an implant ten weeks after bone regeneration.<br />
Fig. 8 Radiograph ten weeks postoperatively.
Peri-implantitis<br />
<strong>EDI</strong> 99<br />
Product Reports<br />
Peri-implantitis results in bone loss around a dental<br />
implant. If the condition is left untreated, there is an<br />
imminent risk that the implant will become mobile<br />
and require removal. In such cases, the jawbone must<br />
be rebuilt before a new implant can be placed. This<br />
takes a long time and is as demanding of the patient<br />
as it is expensive.<br />
Tigran is conducting a number of studies assessing<br />
surgical treatment of bone defects caused by periimplantitis<br />
using Tigran’s porous titanium granules.<br />
One major field study led by Caspar Wohlfahrt is<br />
expected to be submitted in 2010. Tigran has shown,<br />
through human biopsies, that new bone can grow<br />
in and around the titanium granules and help the<br />
affected implant (re)-osseointegrate, restoring periimplant<br />
bone volume.<br />
9 10<br />
11 12<br />
13<br />
Fig. 9 Pocket depth: 7 mm.<br />
Fig. 10 Baseline radiograph.<br />
Fig. 11 Bone defect after debridement.<br />
Fig. 12 After mechanical and chemical decontamination<br />
(H 2O 2, 3%) of the implant and perforation of the defect walls<br />
to improve the blood supply, Tigran porous titanium granules<br />
are inserted. After six months of healing, second-stage surgery<br />
is performed and the crown reseated.<br />
Fig. 13 Radiograph six months after loading.<br />
More Information<br />
Tigran Technologies AB<br />
Medeon Science Park . 205 12 Malmö . SWEDEN<br />
Phone: +46 40 650-1665<br />
info@tigran.se . www.tigran.se<br />
The product information produced here editorially is based on information<br />
provided by the manufacturer and has not been checked by the editor<br />
for its accuracy.<br />
Implant-retained<br />
Dentures<br />
Passive fi t<br />
by using SAE spark erosion<br />
Long-term osseointegration<br />
20 years of<br />
experience!<br />
Latch open<br />
Suprastructure latched to the bar<br />
Latch closed<br />
Naturally beautiful.<br />
I am happy.<br />
Clinical photographs:<br />
Dr. E. Eisenmann,<br />
Free University Berlin,<br />
Benjamin Franklin Medical Center<br />
Catalogue<br />
Implant-retained Dentures<br />
Dentist and Patient<br />
information<br />
including denturescost-estimates<br />
Please order for free!<br />
Rübeling Dental-Labor<br />
Langener Landstr. 173 · 27580 Bremerhaven · Germany<br />
Phone: +49 471 / 984 87-0 · Fax: +49 471 / 984 87-44<br />
E-Mail: info@ruebeling.de · www.ruebeling.de<br />
SAE DENTAL VERTRIEBS GMBH<br />
Langener Landstr. 173 · 27580 Bremerhaven · Germany<br />
Phone: +49 471 - 9 84 87 45 · Fax: +49 471 - 9 84 87 44<br />
E-Mail: info@sae-dental.de · www.sae-dental.de
100 <strong>EDI</strong><br />
Product News<br />
Zest Anchors<br />
Locator Abutment Retaining Sleeve<br />
The new Locator Abutment Retaining Sleeve slips<br />
onto the driver end of a Locator Core Tool to hold a<br />
Locator Implant Abutment while delivering it to the<br />
implant site. This Retaining Sleeve makes it much<br />
easier to deliver a Locator Abutment, and retains the<br />
abutment while threading it into the implant.<br />
The Locator Abutment Delivery Retaining Sleeves<br />
can be autoclaved and are sold separately from the<br />
Locator Core Tool in a 4 Pack or a discounted larger<br />
quantity 20 Pack. The Locator Core Tool contains the<br />
Male Removal Tool, Male Seating Tool, and Abutment<br />
Driver for working with the Locator Attachment<br />
System.<br />
Nobel Biocare has expanded its popular Snappy<br />
Abutment product portfolio with the addition of<br />
taller abutment options. Starting immediately the<br />
Snappy Abutment is available in 4.0 and 5.5 mm<br />
abutment heights. Thanks to its profile and design,<br />
the abutment permits clinical use without any modification.<br />
In addition, the included snap-on impression<br />
coping ensures simplified impression-taking.<br />
The Snappy Abutment is an easy to use prosthetic<br />
solution that is highly suitable for posterior restorations,<br />
especially in partially edentulous jaws, and for<br />
single-crown restorations with an implant. It ensures<br />
optimal precision and in addition, all the prosthetic<br />
components and individual elements required for<br />
restoration are supplied in a single package.<br />
Product:<br />
Locator Abutment Delivery<br />
Retaining Sleeve<br />
Indication:<br />
Abutment retaining sleeve<br />
Distribution:<br />
Zest Anchors, LLC<br />
2061 Wineridge Place<br />
Escondido, CA 92029<br />
USA<br />
Phone: +1 760 743-7744<br />
www.zestanchors.com<br />
Nobel Biocare Snappy Abutments 4.0 and 5.5<br />
Thus, the Snappy Abutment provides<br />
a cost-effective, time-saving<br />
and highly functional prosthetic<br />
solution.<br />
The improved Snappy Abutment<br />
package contains the final<br />
abutment, the impression coping<br />
used to take the impression, and<br />
the temporary coping for fabricating<br />
a provisional restoration. The<br />
available components are designated<br />
with the code 4 or 5-,<br />
depending on the height of the<br />
abutment used: the Snappy Abutment<br />
4.0 or the Snappy Abutment<br />
5.5. The Snappy Abutment<br />
is available for all Nobel Biocare<br />
implant systems, NobelReplace,<br />
Brånemark, Nobel-<br />
Active, and for all platform<br />
diameters NP,<br />
RP, WP, and 6.0.<br />
Products:<br />
Snappy Abutments 4.0 and 5.5<br />
Indication:<br />
Abutments for posterior restorations<br />
Distribution:<br />
Nobel Biocare Holding AG<br />
P.O. Box<br />
CH-8058 Zurich-Airport<br />
SWITZERLAND<br />
Phone: +41 43 2115320<br />
info@nobelbiocare.com<br />
www.nobelbiocare.com
Product:<br />
Restorative Torque Wrench<br />
Indication:<br />
Torque wrench<br />
Distribution:<br />
Zimmer Dental Inc.<br />
USA<br />
Phone Germany: +49 761 15647-0<br />
Phone Spain: +34 93 84605-43<br />
Phone France: +33 1 451235-66<br />
Phone Italy: +39 043 85555-73<br />
Phone Israel: +972 3 612-4242<br />
www.zimmerdental.com<br />
Zimmer Dental Inc. has an -<br />
nounced the availability of the<br />
new Restorative Torque Wrench.<br />
The adjustable tool offers en -<br />
hanced precision and retentiveness<br />
in a simple and intuitive<br />
design – making it easier than<br />
ever to confidently secure Zimmer<br />
Dental’s “friction fit” components.<br />
The Restorative Torque Wrench<br />
replaces the previously offered<br />
TW20 and TW30 models, thereby<br />
reducing the number of required<br />
instruments to one for optimum<br />
simplicity and efficiency. The allin-one<br />
wrench features a ratcheting<br />
head, adjustable preset<br />
torque levels which are indicated<br />
<strong>EDI</strong> 101<br />
Product News<br />
Zimmer Dental<br />
Restorative Torque Wrench<br />
����� ���� �������� ������ ������� �� �����<br />
��� ���� � ����� � ������ ����� � ������������<br />
����� �������� ���� �� ���� ������ ����� � ������� ������������ ������ �����������<br />
����� �������� ����������<br />
���� ��������� ������ ��� �� ��������� ���� ��� ��� ���� � ����� �����������<br />
������� ��� ��������� ������������ �� ��� ���������� ���� �� ��������� ������<br />
��������� ���������� �������� ��� ��� ������� ��� ��������� ����� ������������<br />
���������� ��� ������� ��� ������� ������������� ������� �� ��� �����������<br />
�� ���������<br />
���������� � ������������ � ��������� ����� ������<br />
on the handle with a visible gauge, and meets commonly<br />
used international sterilization requirements.<br />
By streamlining the implant restorative process<br />
with a more user-friendly Torque Wrench design,<br />
Zimmer Dental has again reinforced its commitment<br />
to offering meaningful solutions to clinicians.<br />
������� ������� ���� � �����<br />
������������� ���� �<br />
����� ������ � �������<br />
���� ����� � �� �� � � �� � � ��<br />
��� ����� � �� �� � � �� � � ��<br />
�����������������������<br />
������ ������������������������
102 <strong>EDI</strong><br />
Product News<br />
Kohler Minvalux<br />
It is possible nowadays to extract a tooth or a root<br />
and place an implant immediately afterwards, provided<br />
that the indications for this procedure are<br />
observed. In such cases, it must be ensured that the<br />
extraction is performed as atraumatically as possible.<br />
For this, the surgeon must have suitable instruments<br />
at his disposal. Minvalux instruments with a colourcoded<br />
ergonomic Trinovo instrument handle have<br />
a single working end and have especially been<br />
designed for minimally invasive extraction surgery.<br />
Leader Italia Tixos Implant<br />
The Tixos implant line was developed in many years<br />
of research in cooperation with major national and<br />
international universities and research centres.<br />
Tixos implants, manufactured by the exclusive and<br />
original technique of titanium powder laser microfusion,<br />
are designed in 3D: Around a very compact<br />
core, an iso elastic surface is created that replicates<br />
the spongious morphology of the bone – a structure<br />
that is highly mimetic and accelerates bone<br />
healing and promotes osseointegration, as demonstrated<br />
in various in-vitro and in-vivo studies*. The<br />
mechanical characteristics of these implants are<br />
superior to those of traditional implants, while<br />
their surface morphology promotes bone healing<br />
and enhances the three-dimensional fibrin network<br />
structure, cell adhesion and migration, the exchange<br />
of fluids and nutritional elements and proper<br />
vascularization to improve the organization of the<br />
bone matrix.<br />
The fine working tips are used<br />
to divide the desmodontal fibres<br />
of the tooth or root that is being<br />
extracted without damaging the<br />
bony socket walls. The instruments<br />
with thicker working tips<br />
are used for stronger roots<br />
(canine, premolar or molar). The<br />
slightly curved elevators are of<br />
increasing diameter. For an optimal<br />
effectiveness, with the least<br />
possible trauma during dislocation<br />
of the tooth or root, the<br />
working ends have a very pointed<br />
shape.<br />
The two lancet-shaped instruments<br />
can be introduced smoothly<br />
into the space between the<br />
bony socket walls and the<br />
vestibular and oral approximal<br />
surfaces of the tooth being<br />
extracted.<br />
The three-dimensional geometry<br />
created by micro- and macrocavities<br />
with well-defined sizes<br />
and shapes, interconnected by micropores,<br />
promotes bone formation.<br />
*References available:<br />
www.leaderitalia.it<br />
Product:<br />
Minvalux<br />
Indication:<br />
Minimally invasive extraction<br />
surgery<br />
Distribution:<br />
Kohler Medizintechnik GmbH & Co. KG<br />
Bodenseeallee 14-16<br />
78333 Stockach<br />
GERMANY<br />
Phone: +49 7771 64999-0<br />
info@kohler-medizintechnik.de<br />
www.kohler-medizintechnik.de<br />
Product:<br />
Tixos implant<br />
Indication:<br />
Dental implant<br />
Distribution:<br />
Leader Italia srl<br />
Via Aquileja 49<br />
20092 Cinisello Balsamo (MI)<br />
ITALY<br />
Phone: +39 02 618651<br />
export@leaderitalia.it<br />
www.leaderitalia.it
103 103<br />
Materialise Dental Universal SurgiGuide<br />
Product:<br />
Universal SurgiGuide<br />
Indication:<br />
Drill guidance<br />
Distribution:<br />
Materialise Dental NV –<br />
Headquarters<br />
Technologielaan 15<br />
3001 Leuven<br />
BELGIUM<br />
Phone: +32 16 396620<br />
simplant@materialise.be<br />
www.materialisedental.com<br />
Due to the success of Universal<br />
SurgiGuide since its launch one<br />
year ago, Materialise Dental has<br />
recently expanded its range of<br />
Universal SurgiGuide Drill Key<br />
diameters to include 43 different<br />
Drill Key diameters – 16 “Regular<br />
Platform” drill diameters ranging<br />
from 2.0 to 3.5 mm, and 27 “Wide<br />
Platform” drill diameters ranging<br />
from 2.0 to 4.6 mm. This expansion<br />
of available drill diameters<br />
allows for accurate guidance of<br />
an even wider range of drills,<br />
adding to the flexible nature of<br />
the Universal SurgiGuide system.<br />
A Universal SurgiGuide can be<br />
used with any standard implant<br />
surgery kit. The system is compat-<br />
Since our beginnings, wwe<br />
e ha have ve<br />
alw always ays<br />
been ffocused<br />
ocused on<br />
quality and innovation vation<br />
toward<br />
the battle ba ttle against<br />
against<br />
cross - contamination<br />
and inf infections. ections<br />
tions .<br />
In the last 20 years, we have ensured d safety<br />
and pr protection otection<br />
tto<br />
o yyou<br />
ou and yyour<br />
our patients patients,<br />
with advanced and reliable products. TTools<br />
ools that rrepresent<br />
epresent<br />
the ideal ideal solution ffor<br />
or who is<br />
operating in dentistry, y,<br />
implantology/oral<br />
sur surgery gery<br />
and general surgery. sur ger gery.<br />
www.omniaspa.eu<br />
OMNIA OMNIA S.p S.p.A.<br />
Via F. Delnevo, 190 - 43036 Fidenza (PR) Italy<br />
- Tel. Te el.<br />
+39 0524 527453 - Fax<br />
ax +39 0524 525230<br />
VAT IT 01711860344 4 - R.E.A.<br />
PR 173685 - CCompany<br />
ompan y capital capital € 200.000,00<br />
<strong>EDI</strong> 103<br />
Product News<br />
ible with all implant systems and provides for a<br />
flexible drill sequence thanks to a set of Drill Keys<br />
which is composed based on the clinician’s preferred<br />
drill sequence. Additionally, any angle and any position<br />
in the patient’s mouth can be reached thanks to a<br />
special Universal SurgiGuide Handle.<br />
With<br />
Omnia sure<br />
to t o be safe. saf safe.<br />
© 2010 Materialise Dental
104 <strong>EDI</strong><br />
Product News<br />
Kohler New Set of Retractors<br />
The new sinus retractor by Kohler is a revolutionary<br />
development. The end of the instrument is designed<br />
asymmetrically, consequently there is an R-version<br />
for right and an L-version for left. The sinus retractor<br />
is also suitable for retraction in the anterior region,<br />
therefore only these two instruments are necessary<br />
for the complete upper jaw. Retraction of the<br />
mucoperiosteal flap during lateral sinus window<br />
preparation, lifting the sinus membrane and bone<br />
augmentation with or without simultaneous<br />
implant placement will be facilitated by the use of<br />
Directa Luxator<br />
Directa Luxator is a specially designed periodontal<br />
ligament knife with a fine tapering blade that compresses<br />
the alveolar bone, cuts the membrane and<br />
gently eases the tooth from the socket. It was<br />
invented and designed by a Swedish dentist.<br />
The requirement for an atraumatic tooth extraction<br />
has been much discussed recently. For best<br />
treatment results, bone loss during extraction must<br />
be minimized prior to implant treatment. The increasing<br />
number of patients under anticoagulants –<br />
often not allowed to interrupt their medication<br />
even for a tooth extraction – requires extreme care<br />
to avoid postoperative bleeding. Damage to the<br />
tissues must also be minimized for improved local<br />
haemostasis. Trauma for patients undergoing irradiation<br />
or cytostatic treatment must be reduced to<br />
diminish the risk of postoperative infection.<br />
Avoiding unnecessary trauma when extracting<br />
teeth is simplified considerably if the operation<br />
this new instrument because the<br />
mucosal flap will be secured by<br />
the “shark-teeth”. It will therefore<br />
no longer be necessary to press<br />
the retractor firmly against the<br />
jaw bone. Additionally, the shape<br />
of the instrument end prevents<br />
the instrument from sliding into<br />
the sinus window and the<br />
anatomical handle ensures that<br />
the assistant needs only moderate<br />
retraction force. This optimises<br />
working efficiency according to<br />
the slogan: optimised security,<br />
simplicity and efficiency.<br />
The newly designed cheek<br />
retractors consisting of two side<br />
and one front retractor make the<br />
retractor set perfect. The sinus<br />
retractors are indicated for the<br />
upper jaw and the cheek retractors<br />
can be used for upper and<br />
lower jaw in equal measure.<br />
is initiated or<br />
accomplished with a<br />
Directa Luxator to widen the<br />
alveolus and loosen the perio -<br />
dontal ligaments. The delicate<br />
tip of Luxator Original can be inserted<br />
deeply along the root, allowing<br />
final tooth loosening and<br />
removal with a minimal amount<br />
of force.<br />
Product:<br />
New set of retractors according to<br />
Professor (NYU) Manfred Lang,<br />
Nuremberg, Germany<br />
Indication:<br />
Sinus and cheek retraction<br />
Distribution:<br />
Kohler Medizintechnik GmbH & Co. KG<br />
Bodenseeallee 14-16<br />
78333 Stockach<br />
GERMANY<br />
Phone: +49 7771 64999-0<br />
info@kohler-medizintechnik.de<br />
www.kohler-medizintechnik.de<br />
Product:<br />
Luxator<br />
Indication:<br />
Tooth extraction<br />
Distribution:<br />
Directa AB<br />
P.O. Box 723<br />
194 27 Upplands Väsby<br />
SWEDEN<br />
Phone: +46 8506 505-75<br />
info@directadental.com<br />
www.directadental.com
105<br />
Soredex Digora Optime<br />
Product:<br />
Digora Optime<br />
Indication:<br />
Digital intraoral<br />
imaging plate system<br />
Distribution:<br />
Soredex<br />
Nahkelantie 160<br />
P.O.Box 148<br />
04301 Tuusula<br />
FINLAND<br />
Phone: +358 45 7882-2000<br />
info@soredex.com<br />
www.soredex.com<br />
Soredex is introducing new features<br />
to the Digora Optime digital<br />
intraoral imaging plate system.<br />
The Digora Optime is easy to use,<br />
fast, provides excellent clinical<br />
results and now even a new level<br />
of hygiene and Comfort Occlusal<br />
imaging.<br />
The Opticlean concept sets a<br />
new standard in hygiene in dental<br />
radiology. It includes a smart and<br />
automated internal ultraviolet<br />
(UV) disinfection system that<br />
inactivates harmful viruses and<br />
bacteria on the plate transport<br />
mechanism. This new feature provides<br />
germicidal safety minimizing<br />
the risk of cross-contamination<br />
and protects the users of the<br />
system. In addition, the Opticlean<br />
hygiene concept provides effortless<br />
end-to-end hygienic workflow<br />
with touchless operation<br />
and enhanced Optibag hygiene<br />
bags. In the Digora Optime imaging<br />
plate system there is never a<br />
need to touch the re-usable imaging<br />
plate during the imaging procedure.<br />
Omnia Circular Scalpel<br />
Product:<br />
Circular scalpel<br />
Indication:<br />
Dental implantology<br />
Distribution:<br />
Omnia S.p.A<br />
Via F. Delnevo 190<br />
43036 Fidenza (PR) · ITALY<br />
Phone: +39 0524 527453<br />
info@omniaspa.eu<br />
www.omniaspa.eu<br />
The circular scalpel or soft-tissue<br />
punch is used to precisely incise<br />
the mucosal rim around the<br />
implant. Omnia offers scalpels<br />
with three different diameters<br />
(4.1, 5.2, 6.2 mm) for easier adaptation<br />
to major implants brands.<br />
The disposable circular scalpel<br />
causes less mucosal trauma than<br />
traditional scalpels, since the incision<br />
is limited to the dimensions<br />
of the implant cap.<br />
<strong>EDI</strong> 105<br />
Product News<br />
The Comfort Occlusal provides a pleasant imaging<br />
procedure for the occlusal projection imaging, even<br />
with pediatric patients. The optimized size and shape<br />
of the Comfort Occlusal bite protector enables easy<br />
positioning and shields the imaging plates effectively<br />
from wear and damage.<br />
The latest Digora Optime digital imaging plate system,<br />
with the new version of the Digora for Windows<br />
software, includes also several additional improvements,<br />
like showing the patient name on the unit’s<br />
display and drag-and-drop support to and from the<br />
soft ware.
106 <strong>EDI</strong><br />
Calendar of Events<br />
CALENDAR OF EVENTS<br />
2010 Event Location Date Details/Registration<br />
July 88 th General Session & Exhibition<br />
of the International Association<br />
for Dental Research (IADR)<br />
August 8 th International Dental Ethics<br />
and Law Congress<br />
DGOI International Congress/<br />
ICOI World Congress<br />
September FDI Annual World Dental Congress<br />
2010<br />
Barcelona, Spain July 14 – 17, 2010 International Association for Dental<br />
Research (IADR)<br />
www.iadr.com<br />
Helsinki, Finland August 18–20, 2010 International Dental Ethics and Law<br />
Society<br />
www.ideals.ac<br />
Hamburg, Germany August 26–28, 2010 DGOI e.V.<br />
Phone: +49 7251 618996-0<br />
www.icoi-worldcongress-2010.com<br />
Salvador da Bahia,<br />
Brazil<br />
September 2–5, 2010 FDI World Dental Federation<br />
congress@fdiworldental.org<br />
www.fdiworldental.org<br />
October EAO Meeting 2010 Glasgow, Scotland October 6–9, 2010 Colloquium<br />
Phone: +33 144 64-1515<br />
www.eao.org<br />
Reunión de SEPES 2010 Santander, Spain October 8–11, 2010 SEPES – Sociedad Española de Prótesis<br />
Estomatológica<br />
Phone: +34 91 576-5340<br />
www.sepes.org<br />
BDTA Dental Showcase 2010 London, England October 14–16, 2010 British Dental Trade Association<br />
www.dentalshowcase.com<br />
14 th BDIZ <strong>EDI</strong> Symposium Munich, Germany October 15–16, 2010 BDIZ <strong>EDI</strong><br />
Phone: +49 228 9359-244<br />
www.bdizedi.org<br />
November Future Trends in Implantology (FTI)<br />
2010<br />
Florence, Italy November 11–13, 2010 FTI Dental<br />
Phone: +41 22 5330-948<br />
www.ftidental.com<br />
Swedental 2010 Gothenburg, Sweden November 18–20, 2010 Svenska Mässan<br />
www.swedental.org<br />
<strong>EDI</strong> – Information for Authors<br />
<strong>EDI</strong> – the interdisciplinary journal for prosthetic dental implantology is<br />
aimed at dentists (and technicians) interested in prosthetics implantology.<br />
All contributions submitted should be focused on this aspect in content<br />
and form. Suggested contributions may include:<br />
. Case studies<br />
. Original scientific research<br />
. Overviews<br />
Manuscript Submission<br />
Submissions should include the following:<br />
. two hard copies of the manuscript<br />
. a disk copy of the manuscript,<br />
. a complete set of illustrations<br />
Original articles will be considered for publication only on the condition<br />
that they have not been published elsewhere in part or in whole and are<br />
not simultaneously under consideration elsewhere.<br />
Manuscripts<br />
Pages should be numbered consecutively, starting with the cover page.<br />
The cover page should include the title of the manuscript and the name<br />
and degree for all authors. Also included should be the full postal address,<br />
telephone number, fax number, and electronic mail address of the contact<br />
author. The second page should contain an abstract that summarizes the<br />
article in approximately 100 words.<br />
Manuscripts can be organized in a manner that best fits the specific goals<br />
of the article, but should always include an introductory section, the body<br />
of the article and a conclusion.<br />
Figures and Tables<br />
Each article should contain a minimum of 20 and a maximum of 50 origi -<br />
nal color slides (35 mm) or digital photos, except in unusual circumstances.<br />
The slides will be returned to the author after publication. Slides<br />
should be numbered on the mount in the sequential numerical order in<br />
which they appear in the text (Fig. 1, Fig. 2, etc.).<br />
Editors Office: teamwork media GmbH . Hauptstr. 1 . 86925 Fuchstal/Germany<br />
Phone: +49 8243 9692-0 . Fax: +49 8243 9692-22 . E-mail: service@teamwork-media.de<br />
Radiographs, charts, graphs, and drawn figures are also accepted.<br />
Figure legends should be brief one or two-line descriptions of each figure,<br />
typed on a separate sheet following the references. Legends should be<br />
numbered in the same numerical order as the figures.<br />
Tables should be typed on separate sheets and numbered consecutively,<br />
according to citation in the text. The title of the table and its caption<br />
should be on the same sheet as the table itself.<br />
References<br />
Each article should contain a minimum of 10 and a maximum of 30 references,<br />
except in unusual circumstances. Citations in the body of the text<br />
should be made in numerical order. The reference list should be typed on<br />
a separate sheet and should provide complete bibliographical information<br />
in the format exemplified below:<br />
[1] Albrektsson, T.: A multicenter report on osseointegrated oral implants.<br />
J Prosthet Dent 1988; 60, 75-82.<br />
[2] Hildebrand, H. F., Veron, Chr., Martin, P.: Nickel, chromium, cobalt dental<br />
alloys and allergic reactions: an overview. Biomaterials 10, 545-548, (1989).<br />
[3] Johanson, B., Lucas, L., Lemons, J.: Corrosion of copper, nickel and gold<br />
dental alloys: an in vitro and in vivo study. J Biomed Mater Res 23, 349,<br />
(1989).<br />
Review Process<br />
Manuscripts will be reviewed by three members of the editorial board.<br />
Authors are not informed of the identity of the reviewers and reviewers<br />
are not provided with the identity of the author. The review cycle will be<br />
completed within 60 days. Publication is expected within 9 months.<br />
Page Charges and Reprints<br />
There are no page charges. The publisher will cover all costs of production.<br />
The journal will provide the primary author with 20 tear sheets and a free<br />
copy of the journal issue in which the article appears.
The Planmeca ProMax concept offers a full range of imaging<br />
volumes providing detailed information on patient anatomy.<br />
The comprehensive Planmeca ProMax platform complies<br />
with every need in dental radiology, offering digital<br />
panoramic, cephalometric, and 3D imaging together with<br />
advanced imaging software. At the heart of the concept<br />
is the robotic SCARA technology: the unique robotic arm<br />
enables any movement pattern required by existing or<br />
future program, eliminating all imaging restrictions. With<br />
the Planmeca ProMax concept superior maxillofacial<br />
radiography can be performed with a single platform, today<br />
and in the decades to come.<br />
Perfect fi eld size for all needs<br />
Planmeca Oy, Asentajankatu 6, 00880 Helsinki, Finland<br />
tel. +358 20 7795 500, fax +358 20 7795 555<br />
sales@planmeca.com, www.planmeca.com<br />
Planmeca ProMax<br />
all volume sizes