Ohio Nurses Review - June 2022
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
The Official Publication of the <strong>Ohio</strong> <strong>Nurses</strong> Association www.ohnurses.org<br />
OHIO NURSES<br />
Volume 97, Issue 2<br />
<strong>June</strong> <strong>2022</strong><br />
1 | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | www.ohnurses.org<br />
<strong>Review</strong><br />
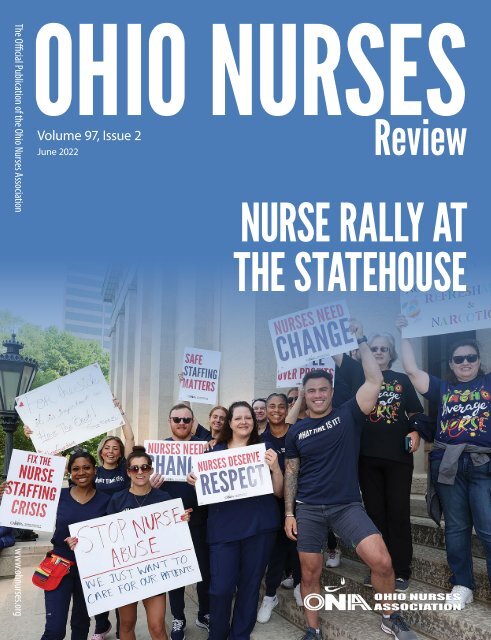
NURSE RALLY AT<br />
THE STATEHOUSE
OHIO NURSES <strong>Review</strong><br />
The <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> (ISSN 0030-0993) is the official<br />
publication of the <strong>Ohio</strong> <strong>Nurses</strong> Association, 3760 Ridge Mill<br />
Drive, Hilliard, OH 43026, (614) 969-3800. Indexed in International<br />
Nursing Index and Cumulative Index to Nursing and Allied Health<br />
Literature. Published quarterly. Circulation approximately 10,000.<br />
Published by ONA Staff and Arthur L. Davis Publishing Agency<br />
Inc., PO Box 216, Cedar Falls, IA 50613. Layout and Design:<br />
Chris Hall<br />
ANNUAL SUBSCRIPTION – Members of ONA, $15, included<br />
in dues as a member benefit; Corporate first class postage<br />
subscription, $40; Agencies, $40; members of the <strong>Ohio</strong><br />
Nursing Students’ Association, $15 with a copy of NSNA<br />
membership card. Replacement copies, $5 prepaid with order.<br />
POSTMASTER – Send address changes to <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong>,<br />
3760 Ridge Mill Drive, Hilliard, OH 43026<br />
MISSION STATEMENT – The mission of the <strong>Ohio</strong> <strong>Nurses</strong><br />
<strong>Review</strong> is: To advance professional nursing practice in <strong>Ohio</strong> in<br />
service of quality health care.<br />
Articles appearing in the <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> are presented<br />
for the information of our members. They are not intended as<br />
legal advice and should not be used in lieu of such advice. For<br />
specific legal advice, readers should contact their legal counsel.<br />
Copyright © <strong>2022</strong> by <strong>Ohio</strong> <strong>Nurses</strong> Association.<br />
ONA BOARD OF DIRECTORS – 2021-2023<br />
OFFICERS<br />
Robert Weitzel, BSN, RN, President, Harrison<br />
Rick Lucas, BSN, RN, OCN, VA-BC, CCRN, First Vice-President,<br />
New Lexington<br />
Jacinta Tucker, MSN, RN, Second Vice-President, Midvale<br />
Michelle Thoman, MSN, RN, Secretary, Cincinnati<br />
Janet Corbin, RN, Treasurer, Urbana<br />
DIRECTORS, UNSTRUCTURED<br />
Tammi Ingledue, BSN, RN, Neatwater<br />
Benitha Garrett, MSN, RN, North Olmsted<br />
Alex Watts, BSN, RN, PCCN, Hilliard<br />
Jamie Burchett, BSN, RN, New Franklin<br />
DIRECTORS, STRUCTURED<br />
Catharyne Henderson, RN, Reynoldsburg,<br />
Deborah Baker-Loyd, RN, Akron<br />
Barbara McGhee, RN, Tallmadge<br />
Amy Pompeii, RN, Med/Surg Cert, Hilliard<br />
Jennifer Hunt, RN, Morning View, KY<br />
NEW NURSE<br />
Taylor Mullin, MSN, RN, CNOR, Galloway<br />
ECONOMIC & GENERAL WELFARE COMMISSIONERS<br />
Amy Pompeii, RN,<br />
Med/Surg Cert.<br />
Chair<br />
Barbara McGhee, RN,<br />
Co-Chair<br />
Michelle Croker, RN,<br />
Secretary<br />
Catharyne Henderson, RN<br />
Deborah Baker-Loyd, RN<br />
Lukas Killian, BSN, RN<br />
Katie Lewis, RN<br />
Jennifer Hunt, RN<br />
2 | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | www.ohnurses.org<br />
COUNCIL ON PRACTICE<br />
Nicole Baltich, MS, APRNC,AGCNS-<br />
AG, CCRN<br />
Kris Cope, DNP, RN, NPD-BC, NE-BC<br />
Catharyne Henderson, RN, BSN,<br />
RNBC<br />
Taylor Mullin, MSN, RN,, CNOR<br />
Kayla Pfeiffer, MSN, CPN, RN<br />
Erin Spies, RN, BS Edu<br />
Nisia Thornton, RN, BSN, MSN, BA,<br />
MEd<br />
CONTINUING EDUCATION<br />
COUNCIL<br />
Barb Brunt, MA, MN, RN, NPDA-BC,<br />
NE-BC (co-chair)<br />
Melanie Morris, MBA, BSN, RN,<br />
NPD-BC, CCRN-K (co-chair)<br />
Lucinda Cave, MSN RN NPD-BC<br />
Stephanie Clubbs, MSN, RN, NPD-<br />
BC, APRN-CNS<br />
Kristine Cope, DNP, RN, NPD-BC<br />
Jacqueline Gierlach, MS, BSN, RN,<br />
CDDN<br />
Amy Knupp, PhD, RN, APRN-CNS,<br />
CPPS<br />
Kayla Pfeiffer, MSN, CPN, RN<br />
Laura Rafeld, MSN, RN, NPD-BC<br />
Deb Shields, PhD, RN, CCRN, QTTT<br />
Sue Smith, MSN, RN, CCHP-RN<br />
Pam Dickerson, PhD, RN, NPD-BC<br />
(MS, BSN), FAAN (Liaison for ANCC)<br />
Nancy Campbell, MS, RN,<br />
MEDSURG-BC, NPD-BC (Liaison for<br />
Indiana)<br />
ONA STAFF<br />
Lisa Ochs, CEO<br />
Kristen Bailey, Labor<br />
Representative<br />
Phillip Bloomer, Organizer<br />
Tiffany Bukoffsky, RN, Director of<br />
Health Policy<br />
Bob Cousins, DEO of Labor<br />
Relations<br />
Michelle Donovan,<br />
Communication and<br />
Development Coordinator<br />
Dodie Dowden, Assistant to CEO<br />
Dennis Dugan, Labor<br />
Representative<br />
Alex Gehrisch, Membership<br />
Controller<br />
Molly Homan, Director of<br />
Communications and Marketing<br />
Technology<br />
James Humphreys, Organizer<br />
Sangita Koparde, Organizer<br />
HEALTH POLICY COUNCIL<br />
MEMBERS<br />
Kay Ball, Chair, PhD, RN, CNOR,<br />
CMLSO, FAAN<br />
Sara Arter, Co-Chair, PhD, RN<br />
Peggy Berry, PHD, MSN, RN,<br />
COHN-S, CLE, PLNC, FAAOHN<br />
Kelly Duffey, MSN, RN, CCRN<br />
Alyssa Figueroa, MPH, BSN, RN<br />
Tina Foster, DNP, MSN, RN, CCRN<br />
Catharyne Henderson, BSN, RN,<br />
ANCC<br />
Kelly Hickman Bigley, RN<br />
Lukas Killian, RN<br />
Janice Lanier, JD, RN<br />
Rick Lucas, BSN, RN, VA-BC, OCN,<br />
CCRN<br />
Barbara McGhee, BSN RN, CNOR<br />
Jeri Milstead, PhD, RN, NEA-BC,<br />
FAAN, ANA Hall of Fame<br />
Gina Severino, DNP, RN, ACNS-BC<br />
Michelle Thoman, MSN, RN<br />
Jacinta Tucker, MSN RN<br />
Alex Watts, BSN, RN, PCCN<br />
PUBLICATIONS COMMITTEE<br />
Barb Brunt, MA, MN, RN, NPD-BC,<br />
NE-BC, Editor<br />
Kristine Cope, DNP, RN, NE-BC,<br />
Lucinda Cave, MSN, RN, BC<br />
Lataya De Jesus, BSN, RN<br />
Elizabeth Digianantoni, RN<br />
Amber Kruzen, RN<br />
Jeri Milstead, PhD, RN, NEA-BC,<br />
FAAN<br />
Tracy Zeller, BSBA, BSN, RN<br />
Angie Lemery, Business Office<br />
Administrator<br />
Cathy McClelland, Finance<br />
Manager<br />
Anne Mueller, Labor<br />
Representative<br />
Anne Ransone, Deputy Executive<br />
Officer - Operations<br />
Kelli Schweitzer, RN, Senior<br />
Director of Professional Practice<br />
Robin Smith, Membership<br />
Controller<br />
Sandy Swearingen, Continuing<br />
Education Specialist<br />
Brittany Turner, Nurse Planner<br />
Lisa Walker, Health Policy and<br />
Nursing Practice Specialist<br />
Jake Whitehurst, Customer<br />
Service, Administrative and<br />
Membership Support Specialist<br />
Rachel Wolfe, Assistant to DEO,<br />
Labor Relations
PRESIDENT’S MESSAGE<br />
Robert Weitzel, BSN, RN<br />
Happy <strong>June</strong>, members! It feels great to finally reach the summer<br />
months. A lot of great things have happened since the last ONR,<br />
including <strong>Nurses</strong> Day at the Statehouse, the ONF’s Virtual<br />
<strong>Nurses</strong> Choice, and National <strong>Nurses</strong>’ Week. The board has also<br />
met several times. During our April 28th meeting in particular,<br />
the Board voted to approve a recommendation to move members<br />
of the Knox-Licking and Mohican Districts into the Mid <strong>Ohio</strong><br />
District. The leaders of each district approached the board<br />
with their intention to dissolve. A committee of the board<br />
was formed, and the board voted to accept this committee’s<br />
recommendation. This transition became effective <strong>June</strong> 1, <strong>2022</strong>.<br />
The board also discussed convening the Leadership Assembly.<br />
A townhall with the board and association leadership will<br />
take place July 28, 8:00pm-9:30pm. The primary focus of the<br />
first townhall will be a review the ONA’s strategic plan. An<br />
invitation to association leadership is forthcoming.<br />
I’m sure many of us have been watching the RaDonda Vaught<br />
case closely, wondering how it may affect the future of our<br />
profession and even possibly persuade nurses who are already<br />
on the brink of leaving nursing to finally make an exit. The<br />
criminal conviction of this circumstance is concerning, and is<br />
why we felt it necessary to release the following statement on<br />
April 5, <strong>2022</strong>.<br />
The Criminal Conviction of RaDonda Vaught<br />
“The ONA stands with many <strong>Ohio</strong> nurses in deep concern<br />
about the dangerous precedent set with the criminal conviction<br />
of former Tennessee nurse, RaDonda Vaught. Ms. Vaught was<br />
convicted of criminally negligent homicide and impaired adult<br />
abuse on March 25 stemming from a 2017 medication error that<br />
resulted in a patient death.<br />
Medical errors are the third leading cause of preventable death<br />
in the United States, resulting in more fatalities than motor<br />
vehicle accidents, breast cancer or AIDS. Given the alarming<br />
number of medical errors, we must begin to question why our<br />
healthcare systems are not better designed to ensure safer patient<br />
care. We must go beyond the individual healthcare workers,<br />
evaluate the entire body of evidence about why medical errors<br />
occur and take heed. We must do all that we can to protect<br />
patients and families from preventable errors.<br />
For example, research has repeatedly pointed to an increase<br />
in medical errors and patient mortality when nurses are<br />
understaffed and work lengthy shifts. Yet, many medical<br />
systems continue to intentionally understaff nurses and mandate<br />
nurses to work extra hours as cost-saving measures, while<br />
federal and state legislatures stall common sense legislation to<br />
curb unsafe nurse staffing.<br />
Already, over 40% of nurses are considering leaving the<br />
profession. Criminally punishing Ms. Vaught, who immediately<br />
reported and took ownership of her error, and who was already<br />
disciplined by the Tennessee Board of Nursing through<br />
licensure revocation, will only further demoralize the nursing<br />
profession, contribute to the nurse staffing crisis, and potentially<br />
dissuade healthcare professionals from being fully transparent<br />
about errors.<br />
Decision makers must start trusting the most trusted profession.<br />
All signs point to a need for change, and the time is now for<br />
meaningful systemic change to happen.”<br />
CONTENTS<br />
President’s Message....................................... 3<br />
CEO’s Message................................................. 4<br />
Anielski Appointed Executive Director<br />
for the <strong>Ohio</strong> Board of Nursing.............. 5<br />
ONA Heritage Hall....................................... 5-7<br />
GCNA Helps MedWish Help the World... 8<br />
<strong>Nurses</strong> Day at the Statehouse and<br />
Virtual Advocacy Week........................... 9<br />
<strong>2022</strong> NDASH Photos...............................10-12<br />
<strong>Ohio</strong> Nurse Attends State of the Union....13<br />
ONA Upcoming Events...............................15<br />
Navigating Virtual Accreditation,<br />
Certification, and Regulatory Visits<br />
During the Pandemic and Beyond...16<br />
Spiderman - A Nurse?..................................18<br />
Small but Mighty!..........................................18<br />
Thank you to our <strong>2022</strong> ONF Nurse<br />
Choice Sponsors!.....................................19<br />
MODNA Executive Committee................19<br />
Local Nursing Legends................................20<br />
Nurse Rally at the Statehouse...................21<br />
National Updates: ANA Position<br />
Statement on Sexual and<br />
Reproductive Health..............................22<br />
www.ohnurses.org | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 |<br />
3
CEO’S MESSAGE<br />
Lisa Ochs, CEO<br />
Dear Members,<br />
It has been a very busy <strong>2022</strong> at the <strong>Ohio</strong> <strong>Nurses</strong> Association<br />
as we have been involved in many projects and numerous<br />
events including <strong>Nurses</strong> Day at the Statehouse, <strong>Nurses</strong> Week,<br />
<strong>Nurses</strong> March and <strong>Nurses</strong> Choice presented by <strong>Ohio</strong> <strong>Nurses</strong><br />
Foundation.<br />
In addition to events, I have been working with the ONA Board<br />
of Directors and Staff to create and execute a meaningful<br />
strategic plan that will strengthen our organization, engage<br />
and grow our members, work on meaningful issues facing our<br />
nurses and ultimately magnify the voice and needs of <strong>Ohio</strong><br />
nurses. As we execute the strategic plan, I look forward to<br />
working with members to move ONA forward.<br />
One critical area of the strategic plan is addressing safe<br />
staffing. According to the <strong>Ohio</strong> Board of Nursing, there are<br />
nearly 250,000 Registered <strong>Nurses</strong> in the state of <strong>Ohio</strong> yet, our<br />
hospitals, skilled nursing facilities, universities and virtually<br />
every area needing Registered <strong>Nurses</strong> is understaffed. While<br />
many employers see this issue resulting from a nursing shortage,<br />
the truth is that <strong>Ohio</strong> has plenty of nurses but they are leaving<br />
their careers behind - especially at the bedside.<br />
The COVID pandemic was instrumental in shining a light on<br />
flaws within the healthcare system. With COVID, the preexisting<br />
staffing gaps in hospitals were much more obvious and<br />
the need to have more nurses at the bedside during the pandemic<br />
became critical. Because of the greed within the healthcare<br />
system to spread staff so thin, it became blatantly apparent to<br />
everyone that the need for effective staffing was vital. With<br />
even more pressure put on nurses to perform under these<br />
circumstances, many nurses chose to leave the bedside.<br />
The trend of nurses leaving the bedside continues with 40%<br />
considering this option. The time is now for our members and<br />
nurses across the state to come together with one strong voice<br />
to take a stand. <strong>Nurses</strong> deserve much better. <strong>Nurses</strong> are the<br />
backbone of the healthcare system and nurses in all walks-of-life<br />
make the system stronger. If nurses from across the state work<br />
together, the power of one voice will make legislators, healthcare<br />
systems and the public take notice.<br />
4 | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | www.ohnurses.org
Anielski Appointed Executive Director for the <strong>Ohio</strong> Board of Nursing<br />
The <strong>Ohio</strong> Board of Nursing voted to appoint Marlene Anielski,<br />
MBA, OCPM, as Executive Director for the <strong>Ohio</strong> Board of<br />
Nursing at their March meeting.<br />
Ms. Anielski previously served for three years as the Executive<br />
Director for the Vision Professionals Board, she also served the<br />
citizens of the state of <strong>Ohio</strong> as a State Representative for <strong>Ohio</strong><br />
District 6 (previously District 17) and as a mayor in northeast<br />
<strong>Ohio</strong>. Ms. Anielski holds a Master’s degree in Business<br />
Administration and her professional background is in project<br />
management, process improvement and operational leadership.<br />
Ms. Anielski brings a demonstrated history of working<br />
successfully in government administration and effectively and<br />
efficiently regulating the practices of health care providers in the<br />
state of <strong>Ohio</strong>.<br />
The Board of Nursing regulates more than 300,000 licenses and<br />
certificates. The Board licenses and regulates registered nurses<br />
(RNs), licensed practical nurses (LPNs), Advanced Practice<br />
Registered <strong>Nurses</strong> (APRNs), Dialysis Technicians (DTs),<br />
Community Health Workers (CHWs) and Medication Aides<br />
(MA-Cs). The Board’s top priorities are to efficiently license<br />
the nursing workforce and remove dangerous practitioners from<br />
practice in a timely manner to protect <strong>Ohio</strong> patients. Public<br />
protection is critical, as nursing touches virtually every citizen<br />
of <strong>Ohio</strong>.<br />
ONA Heritage Hall<br />
By Linda Bass<br />
In 2018 The ONA Board of Directors resurrected ONA Heritage<br />
Committee (HC) to devise a plan to highlight the organization<br />
history in the new headquarters in Hilliard. The HC included:<br />
Linda Bass, Kay Ball, Donna Curry, Joylyn Daniels, Doris<br />
Edwards, Mary Beth Mathews, Carol Sams, and Lisa Walker<br />
(staff). Five large panels displaying the history of the 125 years<br />
of ONA were installed only weeks prior to the fire that destroyed<br />
the headquarters. This was such a loss and few members had<br />
the opportunity to see the panels. The Publication Committee<br />
agreed to print each panel in the next five issues of <strong>Ohio</strong> Nurse<br />
<strong>Review</strong> so members of the organization can see what was<br />
created.<br />
Panel One 1897-1925<br />
At the time the <strong>Ohio</strong> <strong>Nurses</strong> Association was founded almost<br />
125 years ago the nature of nursing was quite different from<br />
what it is today. Hospitals were staffed by student nurses under<br />
the direction of a superintendent of nursing who oversaw the<br />
school of nursing and the hospital. People were hospitalized for<br />
surgery, delivery of a baby, or when there was no one to care for<br />
them at home.<br />
Students dreamed of graduating and working in private duty.<br />
These graduate nurses were entrepreneurs dictating the terms of<br />
their employment, and marketing their skills. Initially graduate<br />
nurses were hired by word of mouth and cared for generations<br />
in the same family when a child was born, or a grandparent<br />
became ill.<br />
The formation of a professional organization with local<br />
districts provided a great service to the nurses by providing a<br />
registry where they could sign up for an assignment. This made<br />
finding work much easier. The registry was like a temporary<br />
employment agency; however, the nurse contracted directly with<br />
the patient and family for terms of the contract. Most graduate<br />
nurses were members of the ONA. A small number of nurses<br />
worked in unique practice areas such as school nursing, public<br />
health, and the operating room. When WWI began, nurses were<br />
recruited to serve in field hospitals in Europe. In 1918 nursing<br />
faced a major public health challenge. The Spanish Flu was a<br />
highly contagious, epidemic, respiratory infection that killed<br />
more US citizens than WWI.<br />
Panel Two 1926- 1950<br />
Following WWI more schools of nursing were founded in<br />
conjunction with hospitals. The student nurses attended more<br />
classroom lectures but they continued to provide most of the<br />
direct care to hospitalized patients. The Great Depression<br />
brought a major shift in nursing roles. Many private duty nurses<br />
were out of work because families could no longer afford their<br />
services. <strong>Nurses</strong> were literally starving. The New Deal provided<br />
support to public health projects that employed graduate<br />
nurses and hospitals to hire more nurses to care for indigent<br />
hospitalized patients. This shift in employment from private<br />
duty to hospital staff increased from the 1920’s to 1940’s. By<br />
1950 private duty nursing was almost nonexistent.<br />
In 1941 the military Cadet Nursing Programs was created to<br />
accelerate nursing education and prepare nurses for military<br />
service. By the end of WWII, more nurses were needed in the<br />
civilian hospitals. Battlefield operations, the use of antibiotics,<br />
and monitoring made their way into post war treatment in many<br />
community hospitals. Hospitals grew in size and technology<br />
following WWII. This justified the hiring of more nurses at the<br />
bedside. By the end of this quarter graduate nurses had moved<br />
from entrepreneurs to employees in large institutions.<br />
www.ohnurses.org | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 |<br />
5
6 | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | www.ohnurses.org
www.ohnurses.org | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 |<br />
7
GCNA Helps MedWish Help the World<br />
By Lucinda Cave, MSN, RN, NPD-BC<br />
Hospitals in the U.S. generate over five million tons of waste<br />
each year. That’s 29 pounds per patient bed per day! Much of<br />
this waste includes unused supplies and equipment which end up<br />
in our landfills (Practice Greenhealth, <strong>2022</strong>).<br />
Worldwide, more than five million children die each year before<br />
reaching their fifth birthday. Many of these deaths could be<br />
prevented with access to adequate health care and medical<br />
supplies (UN, 2021).<br />
MedWish International, based in Cleveland, <strong>Ohio</strong> is a nonprofit<br />
organization which works towards helping both situations. And<br />
nurses from Greater Cleveland <strong>Nurses</strong> Association (GCNA, or<br />
District 16) help MedWish – but more on that later. MedWish<br />
saves lives and our environment by repurposing discarded<br />
medical supplies and equipment to provide humanitarian aid<br />
to people in need, regardless of race, religion, or political<br />
affiliation.<br />
The donated supplies and equipment have come from 136 U.S.<br />
hospitals, clinics, physician offices, surgery centers, homecare,<br />
and individuals. Facilities close, vendors change, and equipment<br />
gets upgraded. All become reasons for having excess stock<br />
which can be donated. Donations are made regularly or onetime.<br />
MedWish accepts and redistributes everything from<br />
2x2s, to urinary catheters, to defibrillators, to patient beds, and<br />
everything in between! They do not distribute expired items<br />
or about-to-expire items or prescription medications. Some<br />
expired items can be re-purposed in an ‘Alternate Recycling’<br />
program. For anyone who works in a facility that might have<br />
items to donate, there is a complete list of accepted supplies and<br />
instructions on the website: www.medwish.org<br />
placed in alternative recycling or are discarded. Other days the<br />
sorting and packing becomes more fine-tuned. GCNA nurses<br />
place all similar items in boxes, weigh them, pack for storage<br />
or shipping, and affix the labels. Why are nurses particularly<br />
good at this effort? Because we are already familiar with the<br />
supplies, and just like with our patient care, we first check<br />
expiration dates! We know the difference between say, Luer-Lok<br />
and slip-tip syringes, and can quickly spot mis-sorted items.<br />
We also exhibit the same concern we share with our own direct<br />
care patients, because after all, we understand these supplies are<br />
going to people in great need.<br />
MedWish accomplishes its work through the actions of many<br />
volunteers. In 2021, there were 7,646 total service hours<br />
performed. GCNA nurses frequently work alongside others from<br />
school, church, and community groups, as well as with helpful<br />
staff. MedWish sets a few rules for volunteers and provides an<br />
orientation for first-timers. Volunteer information may be found<br />
on the MedWish website: www.MedWish.org<br />
At a time when environmental and health justice issues are<br />
forefront, MedWish provides one tangible way for nurses to<br />
take action. Just as we are rewarded through our own direct<br />
and indirect patient care, we benefit by knowing that through<br />
MedWish we are also caring for others in need.<br />
In 2021, MedWish shipped 431,000 lb. of supplies, impacting<br />
nearly two million people here and around the globe. That’s<br />
431,000 lb. of useful materials that did not get buried in our<br />
landfills. MedWish has helped people in Lebanon following<br />
the 2020 explosion, sent PPE to Wuhan, China at the start of<br />
the pandemic, then pivoted to distributing it here in the US<br />
when supplies became sorely needed. Currently, MedWish is<br />
collecting and shipping medical supplies to Ukraine. MedWish<br />
works with a network of international agencies and individuals<br />
to make sure supplies reach the intended recipients. Recipients<br />
pay shipping costs, and supplies donated from MedWish may<br />
not be resold.<br />
So how do GCNA nurses help? By volunteering! Once a month<br />
a group of GCNA members arrive at the MedWish warehouse to<br />
sort, pack, count and weigh thousands of healthcare items. Some<br />
of the nurses from GCNA participate more hours above that.<br />
Donated supplies arrive at MedWish in boxes and bins all<br />
jumbled together – sterile surgical instruments packed between<br />
tubes of toothpaste; defibrillator pads nestled among ostomy<br />
products. Volunteers first sort the items into about two dozen<br />
bins with other like products – respiratory equipment, wound<br />
care products, surgical supplies, and so forth. Expired items are<br />
8 | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | www.ohnurses.org<br />
GCNA nurses (and nurse friends) finish a MedWish volunteer shift. Note all<br />
the boxes and the sorting bins.<br />
References<br />
1. Practice Greenhealth. <strong>2022</strong>. Waste. https://practicegreenhealth.<br />
org/topics/waste/waste Accessed April 8, <strong>2022</strong>.<br />
2. UN Inter-agency Group for Child Mortality Estimation. 2021.<br />
Estimation Child Mortality Report 2021. https://childmortality.<br />
org/wp-content/uploads/2021/12/UNICEF-2021-Child-<br />
Mortality-Report.pdf Accessed April 8, <strong>2022</strong>.
<strong>Nurses</strong> Day at the Statehouse and Virtual Advocacy Week<br />
By Tiffany Bukoffsky, MHA, BSN, RN<br />
While ONA’s <strong>Nurses</strong> Day at the Statehouse looked different<br />
this year, many nurses (and students) took advantage of a<br />
week’s worth of advocacy. On Monday and Tuesday of the<br />
Virtual Advocacy Week, ONA launched a three-part continuing<br />
education series that offered 2.5 contact hours. Presentations<br />
included, The Legislative Process – How Does a Bill Become<br />
a Law in <strong>Ohio</strong>?; Safe Staffing, Workplace Violence, Hospital<br />
Licensure – History and Importance; and Legislative Update on<br />
Issues Impacting <strong>Nurses</strong> in <strong>Ohio</strong>.<br />
Monday also presented the launch of ONA’s #TheTimeIsNow<br />
campaign sign-on letter. This letter and campaign urges elected<br />
leaders in <strong>Ohio</strong> to recognize that nurse staffing is a statewide<br />
crisis and take immediate and robust action, that looks at both<br />
short-term and long-term solutions. While the sign-on letter<br />
began during the advocacy week, nurses and nurse supports can<br />
still sign-on by visiting www.ohnurses.org/the-time-is-now.<br />
On Tuesday, March 8, <strong>2022</strong>, ONA President Robert Weitzel<br />
provided testimony in the House Commerce and Labor<br />
Committee to voice our association’s concerns with House Bill<br />
466. HB 466 would place regulations on healthcare staffing<br />
agencies, cap nurses’ wages, and potentially impede where a<br />
nurse works.<br />
While nurses from across the state could not meet in-person<br />
for the typical <strong>Nurses</strong> Day at the Statehouse, a symbolic day at<br />
<strong>Ohio</strong>’s Statehouse took place in the atrium. Lawmakers, their<br />
aides, and politicos entered the room with sounds of a typical<br />
hospital ICU, while the New York Times opinion piece “Hospital<br />
Greed is Destroying Our <strong>Nurses</strong>. Here’s Why” played on two<br />
large projector screens. As folks navigated through the room,<br />
they read the tragic realities of what it’s like to be nurse through<br />
stories nurses submitted to ONA. Additionally, individuals<br />
walked past three hospital beds that each shared the following<br />
evidence-based statistic: The standard ICU nurse-to-patient<br />
ratio is 1:2. Each additional patient added to a nurse’s workload<br />
has a 7% increase in mortality. The patient’s (your spouse, your<br />
child, your loved one) risk of death increases by 7%. Lastly, the<br />
symbolic day at the statehouse ended with ONA’s vice president,<br />
Rick Lucas, providing a recorded interview with New Channel<br />
4.<br />
On Thursday of the Virtual Advocacy Week, ONA’s Health<br />
Policy Chair Kay Ball and Co-Chair Sara Arter led a virtual<br />
panel discussion with several of <strong>Ohio</strong>’s lawmakers who serve<br />
on the House and Senate Health Committees. Members<br />
who attended the panel discussion included House Minority<br />
Leader Allison Russo, Representatives Brian Stewart, Susan<br />
Manchester, Tom Young, Andrea White and Senator Kristina<br />
Roegner. The discussion topics included questions regarding<br />
keeping nurses at the bedside, the effects of COVID-19, staffing<br />
agencies and capping nurses’ wages, incentivizing nurses to stay<br />
in <strong>Ohio</strong>, workplace violence, and safe nurse to patient limits.<br />
On the last day of the virtual advocacy week, ONA’s Director of<br />
Communications interviewed Ashley Lantto, who is leading the<br />
Nurse March Rally at the <strong>Ohio</strong> Statehouse on May 12th. Ashley<br />
shared why she decided to start this grassroots effort and what<br />
she is planning for this important rally.<br />
Details, pictures, and videos of each of the week’s activities<br />
can be found on ONA’s Facebook and Instagram pages. While<br />
this year’s virtual week of advocacy was a success, a week is<br />
not enough to create change at <strong>Ohio</strong>’s Statehouse. Advocacy is<br />
a marathon, not a sprint! As ONA continues to move forward<br />
with #TheTimeIsNow campaign, please be on the lookout for<br />
opportunities to get involved.<br />
www.ohnurses.org | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 |<br />
9
<strong>2022</strong> NDASH Photos<br />
10 | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | www.ohnurses.org
www.ohnurses.org | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | 11
12 | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | www.ohnurses.org
<strong>Ohio</strong> Nurse attends State of the Union<br />
By Barbara Brunt, MA, MN, RN, NPDA-BC, NE-BC<br />
Refynd Duro, BSN, RN, a nurse from the Progressive Care<br />
Unit at the <strong>Ohio</strong> State Wexner Medical Center, was invited<br />
by Dr. Jill Biden to join her in the viewing box for President<br />
Biden’s State of the Union address on March 1, <strong>2022</strong>. Refynd<br />
has been working for 19 years as a nurse. Over the past two<br />
years, she’s cared for COVID-19 patients who are no longer at<br />
the critical level that warrants intensive care. She was invited<br />
to attend through connections with the ONA, who knew her<br />
as an advocate for patient safety and beside nurses. Refynd,<br />
who was born in the Philippines, said First Lady Jill Biden was<br />
specifically looking for an Asian-American nurse to invite.<br />
When asked about her experience, Refynd said it was<br />
unforgettable, using adjectives such as excited, honored, and<br />
nervous. She felt responsible for representing all nurses in the<br />
US. When she was in Washington, she had dinner at the White<br />
House. Dr. Jill Biden, Doug Harris, and the President’s sister<br />
came out at the end of the dinner to meet all the invited guests,<br />
and there was a photo shoot with Dr. Jill Biden and the Second<br />
Gentleman. Refynd received a surprise at dinner when the group<br />
sang Happy Birthday (her birthday was February 27th and two<br />
of the other guests had birthdays on Feb. 28th). She was allowed<br />
to bring one guest and selected her best friend Tanya Dean, who<br />
enjoyed the ceremony inside the White House in a theater with<br />
a giant screen eating popcorn and drinking champagne. After<br />
dinner the invited guests were shuttled to the Capitol, following<br />
the President’s motorcade. The President came in to meet<br />
everyone after the speech, and Refynd acknowledged that she<br />
froze when she was introduced to the President.<br />
Refynd started out working at Mount Carmel in 1994 and took a<br />
break from school because she was not sure she wanted to be a<br />
nurse. Her father took the Sunday paper, looked at the job hiring<br />
section and circled all the nurses needed. He was the one who<br />
convinced her to become a nurse. Nursing school was difficult<br />
at first because she was just out of high school, so after a couple<br />
years of nursing school, she took a break She wanted to get some<br />
experience, so she became a Patient Care Assistant in 1997. She<br />
worked as a PCA and Dialysis Tech before she went back to<br />
nursing school<br />
After she graduated years later, she started working at the<br />
bedside and has been there ever since. Nursing is her calling<br />
and her passion. She shared some of the stresses she had when<br />
caring for COVID patients. One gentleman who had not been<br />
vaccinated had eight children and she spent two hours in his<br />
room because he was anxious and couldn’t breathe. Initially<br />
she was scared and quarantined from her family for a month,<br />
sending her son to live with her parents. She missed her son’s<br />
birthday during this time. She also has felt the personal loss of<br />
losing a loved one to COVID – her uncle died from COVID.<br />
Refynd graduated from Columbus State Community College in<br />
December of 2002 and got her BSN from Mt. Carmel in 2014.<br />
She has been at <strong>Ohio</strong> State Medical Center for 12 years and<br />
hopes to go back to school once her son is in school all day. Her<br />
son will be five next week and she is looking forward to being<br />
able to get him vaccinated. As a single Mom, she appreciates the<br />
support of her parents and brother and sister-in-law to help her.<br />
She has been part of the union at <strong>Ohio</strong> State since she started<br />
in 2010 but became more involved with the union in 2017 when<br />
the union filed a grievance about the nurse-to-patient ratio. She<br />
helped pass out fliers and helped recruit members. In her spare<br />
time, Refynd enjoys taking care of herself with massages and<br />
manicures. She loves going to dinner with friends, as well as<br />
cooking. She also loves to garden; flowers make her happy and<br />
lift her spirits up. She talks with her plants every morning and<br />
after she retires, she may work at a nursery.<br />
www.ohnurses.org | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | 13
14 | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | www.ohnurses.org
<strong>Ohio</strong> <strong>Nurses</strong> Association<br />
Upcoming Events<br />
<strong>June</strong> 7th and 8th<br />
The Retired <strong>Nurses</strong> Forum Presents: Healthcare Issues<br />
Potpourri <strong>2022</strong><br />
Registration is open for a virtual event for ALL nurses!<br />
$175 for nonmembers and $115 for ONA members.<br />
<strong>June</strong> 22nd<br />
2nd Annual ONA Human Trafficking Awareness Symposium<br />
12pm-1pm<br />
ONA members free<br />
$25 for nonmembers<br />
Monday, September 12th -<br />
Tuesday, September 13<br />
8:00am-5:00pm<br />
E&GW RN Labor Institute<br />
Mohican Lodge & Conference Cernter, Perrysville, OH<br />
October 12th<br />
<strong>2022</strong> Cornelius Leadership Conference<br />
The Blackwell Inn - Columbus<br />
Time: TBA<br />
Save the Date<br />
Monday, October 3, 2023-<br />
Thursday, October 6, 2023<br />
2023 ONA Convention<br />
Details TBA.<br />
The <strong>Ohio</strong> <strong>Nurses</strong> Association is accredited as a provider of<br />
nursing continuing professional development by the American<br />
<strong>Nurses</strong> Credentialing Center’s Commission on Accreditation.<br />
(OBN-001-91).<br />
Visit ohnurses.org/ona-events/ to register for event or to see all<br />
upcoming ONA events.<br />
Medical Disclaimer: This publication’s content is<br />
provided for informational purposes only and is not<br />
intended as medical advice, or as a substitute for the<br />
medical advice of a physician, advanced practice<br />
registered nurse or other qualified healthcare professional.<br />
www.ohnurses.org | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | 15
Navigating Virtual Accreditation, Certification, and<br />
Regulatory Visits During the Pandemic and Beyond<br />
By Khaliah Fisher-Grace, PhD, RN, Jennifer Gonzalez, MSN, RN, Janet Kloos PhD, RN<br />
University Hospitals Cleveland Medical Center, Cleveland, OH<br />
Introduction<br />
Hospitals and health systems have been forced to think<br />
differently about clinical operations during the COVID-19<br />
pandemic. While clinical operations upended, hospitals and<br />
health systems worked tirelessly to ensure patients were safe<br />
and received high quality care despite the challenges brought<br />
on by the pandemic. Accreditation, certification, and regulatory<br />
(ACR) visits were among some of the clinical operations<br />
disrupted in 2020. ACR visits validate the quality of care<br />
provided at an institution and help support quality patient<br />
outcomes. During ACR visits staff and patients are interviewed;<br />
and organizational processes and documents are reviewed to<br />
validate compliance with patient safety and quality standards.<br />
As a large academic medical center our organization averages<br />
more than 20 anticipated and unanticipated ACR visits annually.<br />
During the first two quarters of 2020, our ACR visits were<br />
suspended. As regulatory agencies refined their visit methods,<br />
our health system participated in virtual and hybrid anticipated<br />
and unanticipated visits from our accrediting organizations, our<br />
specialty certification programs, as well as our state inspection<br />
and licensing authorities. The purpose of this article is to share<br />
our experience, as well as best practices defined in literature for<br />
navigating anticipated and unanticipated ACR visits during the<br />
pandemic and beyond.<br />
There is a paucity of information available in the literature to<br />
help organizations prepare for virtual or hybrid ACR visits.<br />
Recent publications have shared information about preparing for<br />
virtual ACR visits from the Accreditation Council for Graduate<br />
Medical Education International (ACGME-I) and the American<br />
<strong>Nurses</strong> Credentialing Center’s Magnet Recognition Program®<br />
(Nasca, 2020; Tomaseki, 2020). This article synthesizes the<br />
themes from these publications as well as our experience<br />
navigating ten virtual or hybrid ACR visits in an academic<br />
medical center with an aim of sharing how to successfully<br />
conduct a virtual or hybrid Accreditation, Certification, or<br />
Regulatory visit in other settings.<br />
Visit Types<br />
Accreditation, certification, and regulatory visits typically occur<br />
in one of four methods. They may be anticipated, announced,<br />
unanticipated, or unannounced (see Figure 1). During the<br />
COVID-19 pandemic, anticipated and unanticipated visits<br />
occurred virtual or in a hybrid format. We learned from our<br />
experience and the existing literature that the core components<br />
of virtual and hybrid visits are the same whether the visit was<br />
anticipated or unanticipated.<br />
Figure 1. Four Visit Types<br />
Anticipated Visit<br />
location: onsite, virtual, hybrid<br />
reason for visit: validation of<br />
compliance with quality and safety<br />
standards set forth by regulatory<br />
agency<br />
Unanticipated Visit<br />
location: onsite, virtual, hybrid<br />
reason for visit: validation of<br />
compliance with quality and safety<br />
standards set forth by regulatory<br />
agency, but may be the result of a<br />
complaint<br />
Announced Visit<br />
dates known; made<br />
in collaboration with<br />
organization<br />
Unannounced Visit<br />
specific date<br />
unknown, date range<br />
may be made in<br />
collaboration with<br />
organization<br />
Core Components of Virtual and Hybrid Visits<br />
We identified equipment, technology support, a visit plan, and<br />
a good communication strategy as the four core components<br />
essential to the success of anticipated and unanticipated virtual<br />
and hybrid ACR visits.<br />
Equipment<br />
Studies about virtual ACR visits described the need to secure<br />
the appropriate equipment as a high priority (Cobourne<br />
&Shellenbarger, 2021; Tomaseki, 2020). Given that ACR visits<br />
can be unanticipated or unannounced we recommend addressing<br />
the equipment needs immediately and planning for periodic<br />
re-testing. Equipment needs include computers with camera and<br />
microphones, conference phones, Electronic Medical Record<br />
(EMR) access, and touchscreen tablets. Computers with cameras<br />
are necessary to verify the identity of the ACR hospital team<br />
members and to help with observation and interviews. Select<br />
equipment participants are comfortable using. Test equipment<br />
to ensure the microphones work, the internet connects in<br />
various areas such as the stairwells, basement, operating room<br />
and radiology departments, and the camera is wide enough to<br />
display the entire audience.<br />
Technology Support<br />
Video conferencing, cybersecurity, and hands on support are<br />
types of technology needed to successfully conduct a virtual<br />
visit.<br />
Video conferencing. Simultaneous video conferencing with<br />
many people in the organization may need to occur. Consider<br />
ACR and hospital team member needs when selecting a video<br />
conferencing platform. Communicate with the ACR agency<br />
to identify the optimal platform. User agreements or product<br />
licenses may need to be obtained. Practice sessions are<br />
16 | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | www.ohnurses.org
ecommended even with platforms that are regularly used to<br />
enhance confidence.<br />
Cyber Security. “Cybersecurity in healthcare involves<br />
protecting electronic information and assets from unauthorized<br />
access, use and disclosure” (Healthcare Information and<br />
Management Systems Society, para 1, 2021). Ensure that<br />
information shared remains confidential and risk for a<br />
cybersecurity breach is minimized. Include your Privacy<br />
Officer and Information Technology team, who can assist in<br />
identifying a secure location to store and share documents, issue<br />
EMR passwords, and provide instructions on how to securely<br />
send protected health and employee information. Identify if<br />
healthcare information can be shared via computer screen or if<br />
it must be electronically transferred. Engaging cybersecurity<br />
experts will save time and minimize risks.<br />
Hands on Support. The IT team can be beneficial to troubleshoot<br />
technology issues with audio, connectivity, or the conferencing<br />
platform. They can assess connectivity before a planned visit.<br />
Based on the results of the IT assessment, they can resolve or<br />
communicate lack of connectivity and plans for reconnecting to<br />
both teams ahead of time.<br />
Visit Plan<br />
ACR leaders collaborate with the organization to develop a<br />
visit plan. Mutual development of the visit plan can enhance<br />
the site visit workflow and agenda. Include phone numbers,<br />
video conference links, and visit locations on the agenda. As<br />
appropriate, plan to include non-clinical team members such as<br />
Finance, and Human Resources. Inform staff of the schedule<br />
and expectations such as virtual etiquette and speaking clearly<br />
through face masks. Establish a team to move equipment<br />
throughout the organization, navigate the meeting platform,<br />
share secure documents, troubleshoot issues, and identify<br />
optimal Wi-Fi spots on each unit (Tomaseki, 2020).<br />
Communication Strategy<br />
The key component for success during any visit is to begin<br />
with a good communication strategy. The communication<br />
strategy should be developed, tested, and activated. This<br />
strategy includes notification of leadership and members of the<br />
organization that a visit has begun, reporting to a designated<br />
location to meet the ACR team, sharing the agenda, identifying<br />
when the visit is complete, and sharing visit outcomes. Call<br />
multiplier, email, and text messaging are communication<br />
tools that can be utilized during an ACR visit. Leveraging<br />
communication tools can facilitate a smooth visit process.<br />
During an unannounced and unanticipated visit communication<br />
from the external ACR agency may be initiated through email<br />
or via phone call. Ensure that your organization has a process to<br />
triage an email or call from an ACR agency.<br />
Obtaining accreditation, certification or designation is often<br />
the focus of an ACR visit. Outcomes of ACR visits are very<br />
important; however, the process is also critical to the success of<br />
the visit. As our organization hosted visits that entailed each of<br />
the four visit methods we took lessons learned and disseminated<br />
them throughout the health system. We improved our processes<br />
so that all subsequent visits used the four components of a<br />
successful visit; ensuring sustainability of our efforts.<br />
A virtual visit can save money on travel expenses and remove<br />
the barrier of geographical location preventing an ACR<br />
visit from being possible. As we move out of the COVID-19<br />
pandemic, accreditation, certification, and regulatory visits<br />
may continue to be virtual, they may resume in person or<br />
there may be a hybrid approach. A healthcare accreditation<br />
organization announced that in person visits would resume<br />
with minimal staff participating in visit related tours and<br />
meetings. Consider how hybrid models may be used by your<br />
accreditation, certification, and regulatory organizations and<br />
plan to be prepared to support each model. This can ensure that<br />
you can move your organization forward to obtain the quality<br />
recognition it deserves, while maintaining safety of the patients<br />
and the team.<br />
References<br />
Cobourne,K, Shellenbarger,T. (2021). Virtual site visits: a new<br />
approach to nursing accreditation, Teaching and Learning in<br />
Nursing, 16(2).162-165. doi:10.1016/j.teln.2020.11.001. Accessed<br />
April 4, <strong>2022</strong>.<br />
Healthcare Information and Management Systems Society<br />
(2021,May 21)Cybersecurity in Healthcare. Retrieved<br />
from https://www.himss.org/resources/cybersecurityhealthcare#:~:text=Cybersecurity%20in%20healthcare%20<br />
involves%20the,as%20the%20%E2%80%9CCIA%20<br />
triad.%E2%80%9D<br />
Nasca T. J. (2020). ACGME's Early Adaptation to the COVID-19<br />
Pandemic: Principles and Lessons Learned. Journal of graduate<br />
medical education, 12(3), 375–378. https://doi.org/10.4300/<br />
JGME-D-20-00302.1<br />
Tomaseki, C. (2020). The inside scoop of a virtual site visit. Plan<br />
and prepare to ensure a successful visit. Retrieved from https://<br />
www.myamericannurse.com/the-inside-scoop-of-a-virtual-sitevisit/<br />
Suggested Reading:<br />
The Joint Commission. (2021,April). New: The Joint Commission<br />
Resumes On-Site, Unannounced Visits; Joint Commission<br />
Perspectives. 41(4),3.<br />
www.ohnurses.org | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | 17
Spiderman—a Nurse?<br />
By Jeri A. Milstead, PhD, RN, NEA-BC, FAAN, ANA Hall of Fame<br />
Yes, Spiderman is a nurse! Introducing Phil Re, a 2021 BSN<br />
graduate of the <strong>Ohio</strong> State University College of Nursing. In<br />
a recent interview, Phil said he has always had a love for the<br />
Marvel comic book hero. He even acquired a costume that he<br />
wore on occasion. On Halloween, 2021, a rainy day, Phil donned<br />
his costume and, with an umbrella in hand, walked across<br />
campus. He approached people walking in the rain and asked,<br />
“If you don’t have an umbrella, would you like to share mine?”<br />
He was received by everyone with good humor and appreciation.<br />
He continued to seek opportunities to make people smile and to<br />
do small good deeds during games in the horseshoe and other<br />
places on campus.<br />
How did he think to combine a comic book hero with nursing?<br />
He admitted to struggling sometimes in his studies and said<br />
he was always “hitting the books” and often did not have time<br />
to socialize with friends. But he noted that one concept kept<br />
showing up throughout many courses: ‘dimensions of wellness.’<br />
He thought one of these, Physical Wellness’ was the easiest<br />
to relate to what he was learning. Then he began to consider<br />
another dimension, Social Wellness, in light of the COVID<br />
pandemic. That is, how people coped with separation and<br />
isolation. During one course, students had to identify how they<br />
actually could use those dimensions in practice. Phil realized<br />
he had an opportunity to combine several dimensions and apply<br />
them not only to his patients but to strangers. That is when he<br />
began to don his costume and make others smile.<br />
Phil is surprised that his persona has become so big. His nurse<br />
manager at OSU Wexner Medical Center heard about his afterhours<br />
activity, spoke to administrators about him, and the set<br />
up an interview with OSU media representatives who, in turn,<br />
set up an interview with Good Morning America. What does<br />
he get out of being Spiderman? Phil says it is satisfying to do<br />
small things that make even strangers smile. As for his nurse<br />
practice in a medical-surgical unit that focuses on bariatrics,<br />
he wants to continue to gain experience. He says his colleagues<br />
are supportive of him and another ‘new’ nurse and their team<br />
approach have helped them learn every day and have made the<br />
transition to practice “easier than school.” He does not have a<br />
plan for more education right now but does not rule it out. He<br />
will continue to do Instagram posts.<br />
So, if you are in the area of OSU and see Spiderman walking<br />
around, don’t think you are hallucinating—you are seeing<br />
a creative, caring Registered Nurse expanding the realm of<br />
practice!<br />
Small but Mighty!<br />
By Tracy Zeller, BSBA, BSN, RN<br />
Two local units of the <strong>Ohio</strong> Nurse Associations have something<br />
to talk about! Mercy Allen Oberlin Hospital and East Liverpool<br />
City Hospital have been able to make economic and fair labor<br />
practice changes happen, proving that even smaller groups of<br />
nurses have the power to achieve big changes. While nurses are<br />
leaving bedside to travel or work in other aspects of healthcare,<br />
those that remain at bedside continue the fight for fairness and<br />
competitiveness.<br />
Oberlin’s Mercy Allen Hospital was able to make significant<br />
gains with their most recent contract negotiations being<br />
primarily economic in nature. While the Oberlin ONA is<br />
comprised of 30 nurses, their small union group has tremendous<br />
power. <strong>Nurses</strong> there will be receiving 5-11% wage increases in<br />
the first year of the new contract based on if that particular nurse<br />
experienced pay freezes noted in the previous contract. The pay<br />
scale cap also increased from 20 years of service to 25 years and<br />
night shift differential tripling from $1.25, increasing every year<br />
until it reaches $3.75. These changes will help the staff thrive<br />
and make the hospital more attractable for nurses.<br />
Over 100 miles away, East Liverpool nurses also fought for and<br />
won against Prime Healthcare regarding not only economic<br />
attractiveness but also fair labor practices. East Liverpool<br />
Hospital employs approximately 125 nurses, having lost<br />
approximately 20 nurses over the last few years. While slightly<br />
larger in size from Mercy Allen, East Liverpool nurses still<br />
showed their strength on a much larger scale by successfully<br />
having the National Labor Relations Board (NLRB) side with<br />
them.<br />
As previously discussed, the NLRB agreed with the ONA that<br />
the hospital failed to properly compensate their nurses. The<br />
hospital will be retroactively paying those nurses who were<br />
employed between <strong>June</strong> 14th and December 13th, 2020. This<br />
retroactive pay totals more than $170,000. The hospital must<br />
also enter contract negotiations in good faith and have union<br />
negotiators well-equipped with negotiation-related information.<br />
Lastly, East Liverpool Hospital will publicly announce that the<br />
hospital will not violate nurses’ federal labor rights and will<br />
not prematurely declare an impasse in negotiations as they had<br />
previously done.<br />
<strong>Nurses</strong> within these two hospital systems should stand proud<br />
that they fought for and won what they truly deserved. With<br />
dedicated nurses, the “David’s” in healthcare can still stand<br />
strong against the “Goliath’s.”<br />
18 | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | www.ohnurses.org
Thank you to our <strong>2022</strong> <strong>Ohio</strong> <strong>Nurses</strong><br />
Foundation’s Nurse Choice Sponsors!<br />
Platinum Plus<br />
Mid-<strong>Ohio</strong> District <strong>Nurses</strong> Association (MODNA)<br />
Platinum<br />
Aon Affinity/NSO<br />
Arthur L. Davis Publishing/HealtheCareers<br />
Case Western<br />
Cloppert, Latanick, Sauter & Washburn<br />
<strong>Ohio</strong> State School of Nursing<br />
Quantum Health<br />
Gold<br />
California Casualty<br />
Kent State University College of Nursing<br />
I Love <strong>Nurses</strong><br />
Southeastern <strong>Ohio</strong> <strong>Nurses</strong> Association (SONA) DOUBLE<br />
SPONSOR<br />
District Three <strong>Nurses</strong> Association<br />
<strong>Ohio</strong> State University <strong>Nurses</strong> Organization (OSUNO)<br />
Greater Cleveland <strong>Nurses</strong> Association (GCNA)<br />
Seeking MODNA<br />
Executive Director<br />
The Mid-<strong>Ohio</strong> District <strong>Nurses</strong> Association (MODNA) (www.<br />
modna.org), Columbus, <strong>Ohio</strong> is seeking a part time (0.6 FTE)<br />
Executive Director. Registered Nurse required; Master’s<br />
degree preferred. A minimum of three years’ experience of<br />
organizational management of a professional organization<br />
related to nursing service, education, professional association,<br />
union or other health care entity preferred. Knowledge of<br />
contemporary issues in nursing, health care, and professional<br />
association operations and management required. Must be<br />
able to work effectively with a 13 member Board of Directors<br />
and other governance structures in a membership driven<br />
organization. The Executive Director directs and is responsible<br />
and accountable for all association operations including hiring<br />
and overseeing an Administrative Assistant/Continuing<br />
Education Coordinator. Excellent interpersonal, fiscal, and<br />
leadership skills required.<br />
Resume and contact information for three references by <strong>June</strong> 30,<br />
<strong>2022</strong> to: executivedirector@modna.org<br />
www.ohnurses.org | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | 19
Local Nursing Legends<br />
By Jeri Milstead, PhD, RN, NEA-BC, FAAN<br />
On May 5, <strong>2022</strong>, the Medical Heritage Center at The <strong>Ohio</strong> State<br />
University Health Sciences Library* paid tribute to 10 nurses<br />
from the Central <strong>Ohio</strong> area. These outstanding nurses were<br />
originally recognized in 2020, but formal acknowledgement<br />
was delayed until <strong>2022</strong> because of COVID-19. Named Local<br />
Nursing Legends, these nurses were cited because they have<br />
made “significant contributions to the nursing profession and<br />
health care.” These “pioneers” have provided “exemplary<br />
service” not only to the local population but through their work<br />
within many organizations. You may know one or more of these<br />
nurses but you may not realize the depth and extent of their gifts<br />
to our professional association. We celebrate several who also<br />
have contributed significantly to the profession through their<br />
contributions to ONA.<br />
Doris Edwards<br />
Early in her career, Doris was active in a number of roles in<br />
SONA including president and recipient of the Mary Hamer<br />
Greenwood Award. Later she became chair of the ONA Nurse<br />
Educator Assembly and was elected to the ONA Board for two<br />
terms. Dr. Edwards served on the Yellow Team of Nursing<br />
2015 (Education) and was subsequently Chair of the Advancing<br />
Nursing Education Task Force, the Caucus on Advancing<br />
Nursing Education and the Heritage Committee. She received<br />
the ONA Outstanding Nursing Education Administrator Award<br />
and the Elaine Martyn Writing Award. She is a member of the<br />
Caucus on Racial Equity and Inclusion in Nursing and was<br />
inducted into the Cornelius Congress.<br />
Sandra Cornett<br />
She served on the first (1994) nursing continuing education<br />
committee for ONA that established criteria for individual<br />
and institutional approval processes for granting continuing<br />
education credits. She also was an active member of the<br />
former ONA Clinical Nurse Specialist Assembly and the Staff<br />
Development <strong>Nurses</strong> Assembly. Sandy also was a leader in<br />
MODNA as first vice president (1990-1996) and member and<br />
often chair of the CE/Program committee.<br />
In 1974, Sandy served on an ONA task force that co-authored<br />
A comprehensive cardiac care curriculum: A guide to course<br />
development for registered nurses.<br />
Janice K. Lanier<br />
In the 1980s, Jan worked with legendary CEO Dorothy<br />
Cornelius as ONA’s policy director. She later earned a Juris<br />
Doctor degree and became a regulatory specialist, associate<br />
executive director and Interim Executive Director for the <strong>Ohio</strong><br />
Board of Nursing (OBN). Upon returning to ONA, she served<br />
as director of health policy and deputy executive officer from<br />
2002–2010. She oversaw health policy activities, developed<br />
position papers and testified before the <strong>Ohio</strong> General Assembly.<br />
During those years, she also oversaw extensive bylaws and<br />
strategic plan revisions and led the redesign of <strong>Ohio</strong> <strong>Nurses</strong><br />
<strong>Review</strong>. Jan worked closely with the Mid-<strong>Ohio</strong> District <strong>Nurses</strong><br />
Association (MODNA) to establish effective communications<br />
with local elected officials, establishing candidates’ night<br />
at MODNA, and ONA’s <strong>Nurses</strong> Day at the Statehouse. She<br />
spearheaded the Nursing 2015 Initiative that brought ONA,<br />
OBN and the <strong>Ohio</strong> Organization for Nurse Executives together<br />
to successfully develop strategies that addressed hospital<br />
staffing levels and nurse education and practice issues including<br />
workplace violence. This collaboration became the subject of<br />
a presentation to congressional staff members on Capitol Hill.<br />
Additional legislative and regulatory work included issues<br />
surrounding health care reform, advance practice nursing, nurse<br />
shortage reporting and other areas of nursing practice.<br />
Deborah Shields<br />
Dr. Shields exemplifies the definition of nursing excellence<br />
by demonstrating caring, holistic practice at every level. Her<br />
passion is infectious. Her member appointments include being a<br />
member of the Continuing Education Council for <strong>Ohio</strong> <strong>Nurses</strong><br />
Association, the CE Advisory Group for the <strong>Ohio</strong> Board of<br />
Nursing, nurse peer review leader (American Holistic <strong>Nurses</strong><br />
Association), and lead nurse planner (AHNA). Debbie was<br />
awarded the Mid-<strong>Ohio</strong> District <strong>Nurses</strong> Association (MODNA)<br />
Expert in Nursing Care Award in 2017.<br />
Let’s give our colleagues a round of applause for their long<br />
commitment to the profession and to ONA.<br />
*The Friends of Nursing History Steering Committee of the<br />
Medical Heritage Center of The <strong>Ohio</strong> State University Health<br />
Sciences Library collects, preserves, promotes, teaches, and<br />
celebrates the legacy of nursing in central <strong>Ohio</strong>. Biosketches of<br />
all 10 recipients can be found at www.go.osu.edu/LNL<br />
20 | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | www.ohnurses.org
Nurse Rally at the Statehouse<br />
ONA was honored to be asked by Nurse March-<strong>Ohio</strong> to help<br />
organize the Nurse Rally at the Statehouse.<br />
www.ohnurses.org | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | 21
National Updates:<br />
ANA Position Statement on Sexual and Reproductive Health<br />
Effective Date: March 7, <strong>2022</strong><br />
Status: Position Statement<br />
Adopted by: ANA Board of Directors<br />
Purpose<br />
The purpose of this Position Statement is to guide ANA’s<br />
advocacy and policy engagement on issues related to nursing<br />
and sexual and reproductive health (SRH), as defined below.<br />
SRH issues include respect for a person’s reproductive choices;<br />
sex education; access to contraception; access to abortion<br />
care; ensuring equity in reproductive health, access, and care<br />
delivery; and matters of conscience for nurses in SRH care.<br />
Background<br />
The term SRH encompasses sexual health as an aspect of<br />
reproductive health. Sexual health is a “state of physical,<br />
emotional, mental and social well-being in relation to sexuality;<br />
it is not merely the absence of disease, dysfunction or infirmity.<br />
Sexual health requires a positive and respectful approach to<br />
sexuality and sexual relationships, as well as the possibility of<br />
having pleasurable and safe sexual experiences, free of coercion,<br />
discrimination and violence.” (WHO) 1<br />
The World Health Organization (WHO) discusses the broader<br />
term reproductive health as “a state of complete physical, mental<br />
and social well-being and not merely the absence of disease or<br />
infirmity, in all matters relating to the reproductive system and<br />
to its functions and processes.” Further, “reproductive health<br />
implies that people are able to have a satisfying and safe sex life<br />
and that they have the capability to reproduce and the freedom<br />
to decide if, when and how often to do so.” 2 (WHO)<br />
This Position Statement also encompasses principles of<br />
reproductive justice, which are related to reproductive health<br />
in ways that could have implications for nursing. Reproductive<br />
justice is “the human right to maintain personal bodily<br />
autonomy, have children, not have children, and parent the<br />
children we have in safe and sustainable communities.” 3<br />
The right to seek and receive reproductive health care in the<br />
United States has often been contested in the law and debated<br />
in public policy at the state and federal levels. For instance,<br />
access to contraception was not constitutionally protected<br />
until 1965 when the Supreme Court ruled in Griswold versus<br />
Connecticut (381 U.S. 479 (1965)). In 1973, the Supreme Court<br />
issued Roe versus Wade (410 U.S. 113 (1973)), which recognized<br />
a constitutional right to abortion during the first trimester of<br />
pregnancy. Since 1973, states and courts have refined abortion<br />
law and clarified the restrictive powers of state legislatures<br />
to regulate abortion care. Advocates in favor of and opposed<br />
to abortion rights have repeatedly sought judicial rulings to<br />
support their positions. In 2021, the Supreme Court agreed to<br />
reconsider Roe versus Wade. 4<br />
The Code of Ethics for <strong>Nurses</strong> acknowledges that patients<br />
under the care of a nurse have the moral and legal right to<br />
22 | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | www.ohnurses.org<br />
self-determination. <strong>Nurses</strong> have a duty to respect the decisions<br />
of their patients, including those decisions that are related to<br />
sexual health and pregnancy. Respect for patient decisions does<br />
not mean that the nurse must agree or support the decision.<br />
The Code of Ethics for <strong>Nurses</strong> requires nurses to provide<br />
their patients with “accurate, complete and understandable<br />
information in a manner that facilitates an informed decision.”<br />
<strong>Nurses</strong> should assist patients with weighing benefits, burdens,<br />
and available options, including the choice of no treatment,<br />
when discussing sexual health issues and pregnancy. ANA<br />
believes that nurses should be aware of the history of misogyny,<br />
racism, sexism and other forms of discrimination that has led to<br />
the existing inequities, inequalities and limited access to SRH<br />
care for certain populations. <strong>Nurses</strong> who provide SRH care<br />
should deliver care that promotes reproductive justice and sexual<br />
health within their scope of practice, such as care coordination<br />
that supports a patient’s decision not to have children, or to<br />
safely have and raise children in a just society.<br />
Statement of ANA Position<br />
ANA affirms:<br />
• Everyone has the right to privacy and the right to make<br />
decisions about SRH based on full information and without<br />
coercion.<br />
• <strong>Nurses</strong> are obligated to share with their patients in an<br />
unbiased manner all relevant information about SRH<br />
choices that are available and to support that patient<br />
regardless of the decisions that patient makes.<br />
• Abortion is a reproductive health alternative that nurses and<br />
other providers can discuss when counseling patients.<br />
• SRH care should be widely available, accessible, and<br />
affordable for all.<br />
• <strong>Nurses</strong> have the right to refuse to participate in SRH<br />
care based on ethical grounds, as long as patient safety is<br />
assured, and alternative sources of care have been arranged.<br />
Policy and Practice Recommendations<br />
• Public programs that fund SRH care should:<br />
o Provide access to the full range of SRH care consistent<br />
with patient choice and other principles such as privacy<br />
and fully informed consent.<br />
o Promote care delivery models that include care<br />
coordination for the health of the whole person, including<br />
the need for SRH and supportive services.<br />
o Allow and support SRH care delivery by nurses<br />
practicing to full extent of their education, training,<br />
and licensing. Policies must not interfere with an SRH<br />
provider’s ethical obligations, including the obligation to<br />
provide complete and accurate information about SRH<br />
and SRH care options.<br />
o Be administered with provisions that guard against<br />
patient coercion in treatment decisions, and ensure that<br />
the rights of minors to choose and access SRH care are<br />
protected consistent with their rights to choose and access<br />
non-SRH care.
• To the extent that federal and state laws regulate the<br />
provision of SRH, providers must not be subject to judicial<br />
process when they act within their scope of practice and<br />
ethical boundaries. Similarly, any such regulation must<br />
not be enforced against patients based on their exercise of<br />
choice in receiving SRH care.<br />
• Health insurance plans should be accountable for providing<br />
access to the full range of services for SRH care. Provider<br />
networks should ensure adequate access to SRH care<br />
providers, including advanced practice registered nurses<br />
who are authorized to provide SRH care.<br />
• <strong>Nurses</strong> should be knowledgeable about principles of<br />
reproductive justice as they relate to nursing care, health<br />
equity, and equitable access to care.<br />
• <strong>Nurses</strong> providing SRH care should strive to create a nonjudgmental<br />
atmosphere of shared decision making based on<br />
mutual respect, adequate factual information, and freedom<br />
from bias or discrimination for the persons in their care and<br />
their families.<br />
• <strong>Nurses</strong> who have concerns about the provision of specific<br />
SRH services have an obligation to notify potential<br />
employers and patients of those concerns, and to assist in<br />
referral to an alternative source of care.<br />
Previous Position Statements<br />
In 2010, the ANA Board of Directors adopted a Position<br />
Statement on Reproductive Health. This 2010 Position Statement<br />
required revision and updating in <strong>2022</strong> to enable ANA to speak<br />
to SRH issues as they are presented in contemporary terms.<br />
For instance, the 2010 Position Statement asserted ANA’s<br />
belief that “abortion is a symptom of social failure.” In this<br />
superseding Position Statement, ANA unequivocally disavows<br />
this perspective, and declines to express any social, professional,<br />
or personal judgment regarding abortion.<br />
Further, the 2010 Position Statement did not acknowledge<br />
principles of reproductive justice. The <strong>2022</strong> Position Statement<br />
was updated accordingly to recognize a person’s right to have<br />
children, not have children, and to parent children in safety; and<br />
further to set expectations for nurses to be familiar with this<br />
approach, as it relates to their provision of SRH care.<br />
In other respects, this superseding Position Statement remains<br />
consistent with core statements in the 2010 document. For<br />
example, ANA retains the view, as expressed in the 2010<br />
Position Statement: “ANA believes that the health care client<br />
has the right to privacy and the right to make decisions about<br />
personal health based on full information and without coercion.<br />
It is the obligation of the health care provider to share with the<br />
client all relevant information about health choices that are legal<br />
and to support that client regardless of the decision the client<br />
makes. … If the state limits the provision of such information<br />
to the client, an unethical and inappropriate restraint will be<br />
imposed on the provider and the provider-client relationship will<br />
be jeopardized.”<br />
References<br />
Note: This section includes sources that informed development of<br />
this statement even if not quoted directly.<br />
American <strong>Nurses</strong> Association (ANA). Code of ethics for nurses<br />
with interpretive statements. 2015.<br />
ANA. Letter to Secretary of Health and Human Services Xavier<br />
Becerra, supporting repeal of 2019 final Title X rule.<br />
American Academy of Nursing (AAN) and ANA. Letter to<br />
Secretary of Health and Human Services Alex Azar, requesting<br />
reconsideration of final Title X rule. March 2019. https://<br />
higherlogicdownload.s3.amazonaws.com/AANNET/c8a8da9e-<br />
918c-4dae-b0c6-6d630c46007f/UploadedImages/Academy_<br />
ANA_Response_to_Title_X_Final_Rule.pdf<br />
American College of Nurse Midwives. Access to Comprehensive<br />
Sexual and Reproductive Health Care Services. 2016.<br />
https://www.midwife.org/acnm/files/ACNMLibraryData/<br />
UPLOADFILENAME/000000000087/Access-to-<br />
Comprehensive-Sexual-and-Reproductive-Health-Care-<br />
Services-FINAL-04-12-17.pdf<br />
Blueprint Collaborative. Blueprint for Sexual and Reproductive<br />
Health, Rights, and Justice. (2019). See https://blackrj.<br />
org/sexual-and-reproductive-health-rights-and-justice-acollaboration/<br />
(not cited in position statement)<br />
Center for Reproductive Rights. Beyond Abortion: Roe and Other<br />
Rights. https://reproductiverights.org/beyond-abortion-roe-andother-rights/<br />
Nurse Practitioners in Women’s Health. Statement on Abortion<br />
Bans. Undated. https://www.npwh.org/lms/announcements/<br />
details/88<br />
Roberts, Dorothy. Killing the Black Body. Vintage Books. 1997.<br />
Ross, Loretta J. and Rickie Solinger. Reproductive Justice: An<br />
Introduction. University of California Press. 2017.<br />
SisterSong. Reproductive Justice. Web Content. https://www.<br />
sistersong.net/reproductive-justice<br />
World Health Organization (WHO). https://www.who.int/teams/<br />
sexual-and-reproductive-health-andresearch-(srh)/overview<br />
WHO. Sexual Health. https://www.who.int/health-topics/sexualhealth#tab=tab_2<br />
1<br />
WHO. Sexual Health. Web content accessed January 19, <strong>2022</strong>.<br />
https://www.who.int/health-topics/sexual-health#tab=tab_2<br />
2<br />
See World Health Organization (WHO). Reproductive Health<br />
Indicators. Guidelines for their generation, interpretation and<br />
analysis for global monitoring. 2006.<br />
3<br />
SisterSong. Reproductive Justice. Web content accessed January<br />
19, <strong>2022</strong>. https://www.sistersong.net/reproductive-justice<br />
4<br />
See Center for Reproductive Rights. Beyond Abortion: Roe and<br />
Other Rights. Web content accessed January 19, <strong>2022</strong>. https://<br />
reproductiverights.org/beyond-abortion-roe-and-other-rights/<br />
Retired statement:<br />
• Reproductive Health<br />
www.ohnurses.org | <strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong> | Volume 97, Issue 2 | 23
<strong>Ohio</strong> <strong>Nurses</strong> <strong>Review</strong><br />
5500 Frantz Rd, Ste 169<br />
Dublin, OH 43017<br />
Presort Standard<br />
U.S. Postage<br />
PAID<br />
Permit #14<br />
Princeton, MN<br />
55371<br />
current resident or