Clinical evaluation of monitor unit software and the application of ...
Clinical evaluation of monitor unit software and the application of ...
Clinical evaluation of monitor unit software and the application of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
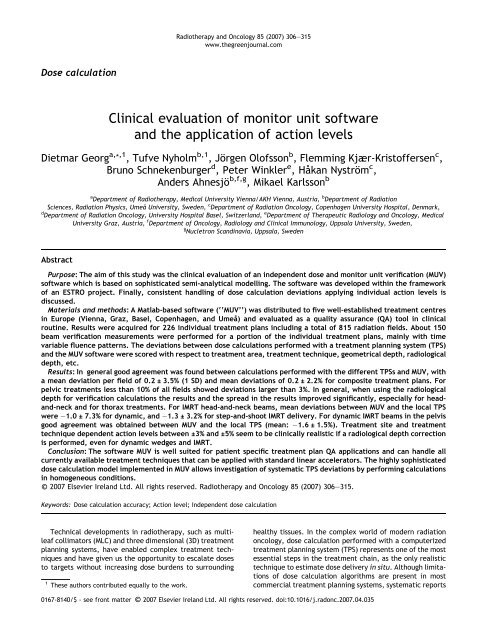
Dose calculation<br />
<strong>Clinical</strong> <strong>evaluation</strong> <strong>of</strong> <strong>monitor</strong> <strong>unit</strong> s<strong>of</strong>tware<br />
<strong>and</strong> <strong>the</strong> <strong>application</strong> <strong>of</strong> action levels<br />
Dietmar Georg a, * ,1 , Tufve Nyholm b,1 ,Jörgen Ol<strong>of</strong>sson b , Flemming Kjær-Krist<strong>of</strong>fersen c ,<br />
Bruno Schnekenburger d , Peter Winkler e ,Ha˚kan Nyström c ,<br />
Anders Ahnesjö b,f,g , Mikael Karlsson b<br />
a Department <strong>of</strong> Radio<strong>the</strong>rapy, Medical University Vienna/AKH Vienna, Austria, b Department <strong>of</strong> Radiation<br />
Sciences, Radiation Physics, Umea˚ University, Sweden, c Department <strong>of</strong> Radiation Oncology, Copenhagen University Hospital, Denmark,<br />
d Department <strong>of</strong> Radiation Oncology, University Hospital Basel, Switzerl<strong>and</strong>, e Department <strong>of</strong> Therapeutic Radiology <strong>and</strong> Oncology, Medical<br />
University Graz, Austria, f Department <strong>of</strong> Oncology, Radiology <strong>and</strong> <strong>Clinical</strong> Immunology, Uppsala University, Sweden,<br />
g Nucletron Sc<strong>and</strong>inavia, Uppsala, Sweden<br />
Abstract<br />
Purpose: The aim <strong>of</strong> this study was <strong>the</strong> clinical <strong>evaluation</strong> <strong>of</strong> an independent dose <strong>and</strong> <strong>monitor</strong> <strong>unit</strong> verification (MUV)<br />
s<strong>of</strong>tware which is based on sophisticated semi-analytical modelling. The s<strong>of</strong>tware was developed within <strong>the</strong> framework<br />
<strong>of</strong> an ESTRO project. Finally, consistent h<strong>and</strong>ling <strong>of</strong> dose calculation deviations applying individual action levels is<br />
discussed.<br />
Materials <strong>and</strong> methods: A Matlab-based s<strong>of</strong>tware (‘‘MUV’’) was distributed to five well-established treatment centres<br />
in Europe (Vienna, Graz, Basel, Copenhagen, <strong>and</strong> Umea˚) <strong>and</strong> evaluated as a quality assurance (QA) tool in clinical<br />
routine. Results were acquired for 226 individual treatment plans including a total <strong>of</strong> 815 radiation fields. About 150<br />
beam verification measurements were performed for a portion <strong>of</strong> <strong>the</strong> individual treatment plans, mainly with time<br />
variable fluence patterns. The deviations between dose calculations performed with a treatment planning system (TPS)<br />
<strong>and</strong> <strong>the</strong> MUV s<strong>of</strong>tware were scored with respect to treatment area, treatment technique, geometrical depth, radiological<br />
depth, etc.<br />
Results: In general good agreement was found between calculations performed with <strong>the</strong> different TPSs <strong>and</strong> MUV, with<br />
a mean deviation per field <strong>of</strong> 0.2 ± 3.5% (1 SD) <strong>and</strong> mean deviations <strong>of</strong> 0.2 ± 2.2% for composite treatment plans. For<br />
pelvic treatments less than 10% <strong>of</strong> all fields showed deviations larger than 3%. In general, when using <strong>the</strong> radiological<br />
depth for verification calculations <strong>the</strong> results <strong>and</strong> <strong>the</strong> spread in <strong>the</strong> results improved significantly, especially for head<strong>and</strong>-neck<br />
<strong>and</strong> for thorax treatments. For IMRT head-<strong>and</strong>-neck beams, mean deviations between MUV <strong>and</strong> <strong>the</strong> local TPS<br />
were 1.0 ± 7.3% for dynamic, <strong>and</strong> 1.3 ± 3.2% for step-<strong>and</strong>-shoot IMRT delivery. For dynamic IMRT beams in <strong>the</strong> pelvis<br />
good agreement was obtained between MUV <strong>and</strong> <strong>the</strong> local TPS (mean: 1.6 ± 1.5%). Treatment site <strong>and</strong> treatment<br />
technique dependent action levels between ±3% <strong>and</strong> ±5% seem to be clinically realistic if a radiological depth correction<br />
is performed, even for dynamic wedges <strong>and</strong> IMRT.<br />
Conclusion: The s<strong>of</strong>tware MUV is well suited for patient specific treatment plan QA <strong>application</strong>s <strong>and</strong> can h<strong>and</strong>le all<br />
currently available treatment techniques that can be applied with st<strong>and</strong>ard linear accelerators. The highly sophisticated<br />
dose calculation model implemented in MUV allows investigation <strong>of</strong> systematic TPS deviations by performing calculations<br />
in homogeneous conditions.<br />
c 2007 Elsevier Irel<strong>and</strong> Ltd. All rights reserved. Radio<strong>the</strong>rapy <strong>and</strong> Oncology 85 (2007) 306–315.<br />
Keywords: Dose calculation accuracy; Action level; Independent dose calculation<br />
Technical developments in radio<strong>the</strong>rapy, such as multileaf<br />
collimators (MLC) <strong>and</strong> three dimensional (3D) treatment<br />
planning systems, have enabled complex treatment techniques<br />
<strong>and</strong> have given us <strong>the</strong> opport<strong>unit</strong>y to escalate doses<br />
to targets without increasing dose burdens to surrounding<br />
1 These authors contributed equally to <strong>the</strong> work.<br />
Radio<strong>the</strong>rapy <strong>and</strong> Oncology 85 (2007) 306–315<br />
www.<strong>the</strong>greenjournal.com<br />
healthy tissues. In <strong>the</strong> complex world <strong>of</strong> modern radiation<br />
oncology, dose calculation performed with a computerized<br />
treatment planning system (TPS) represents one <strong>of</strong> <strong>the</strong> most<br />
essential steps in <strong>the</strong> treatment chain, as <strong>the</strong> only realistic<br />
technique to estimate dose delivery in situ. Although limitations<br />
<strong>of</strong> dose calculation algorithms are present in most<br />
commercial treatment planning systems, systematic reports<br />
0167-8140/$ - see front matter c 2007 Elsevier Irel<strong>and</strong> Ltd. All rights reserved. doi:10.1016/j.radonc.2007.04.035
<strong>of</strong> <strong>the</strong>se limitations are limited <strong>and</strong> practical guidelines for<br />
QA <strong>of</strong> TPS have become available only recently. From previous<br />
ESTRO projects on quality assurance (QA) aspects in<br />
radio<strong>the</strong>rapy that include <strong>the</strong> treatment planning system<br />
(e.g. ESTRO-EQUAL or QUASIMODO) it can be concluded that<br />
<strong>the</strong>re are uncertainties related to <strong>the</strong> dose calculation models<br />
[4,7,9]. Ano<strong>the</strong>r example is <strong>the</strong> study <strong>of</strong> Venselaar <strong>and</strong><br />
Welleweerd [21], where it is shown that especially asymmetric<br />
wedged beams are not properly modelled in some<br />
commercial treatment planning systems.<br />
On <strong>the</strong> o<strong>the</strong>r h<strong>and</strong>, it is generally accepted that deviations<br />
larger than 5% between delivered <strong>and</strong> prescribed doses<br />
may influence <strong>the</strong> clinical outcome <strong>of</strong> <strong>the</strong> treatment [2,14].<br />
For specific tumours <strong>and</strong> situations, such as in clinical trials,<br />
even higher dem<strong>and</strong>s might be required in terms <strong>of</strong> dosimetric<br />
accuracy. Because errors <strong>and</strong> large uncertainties in dose<br />
calculations reduce <strong>the</strong> quality <strong>of</strong> a treatment, independent<br />
dose or MU calculations have been recommended <strong>and</strong> also<br />
used for a long time as a routine quality assurance (QA) procedure<br />
when verifying individual treatment plans<br />
[3,11,15,16]. During <strong>the</strong> last years commercial products<br />
providing independent dose calculations that can h<strong>and</strong>le<br />
all advanced treatment techniques have become available.<br />
However, to our knowledge no reports have been published<br />
that describes <strong>the</strong>ir accuracy or o<strong>the</strong>r aspects <strong>of</strong> <strong>the</strong>ir clinical<br />
<strong>application</strong>.<br />
Verification calculations are traditionally performed by<br />
applying empirical algorithms in a manual calculation procedure,<br />
or utilizing s<strong>of</strong>tware based on fairly simple dose calculation<br />
algorithms. With <strong>the</strong> advent <strong>of</strong> advanced treatment<br />
techniques that are based on <strong>the</strong> availability <strong>of</strong> multileaf<br />
collimators, asymmetric jaws <strong>and</strong> dynamic or virtual<br />
wedges, empirical dose calculation procedures become<br />
much more complex <strong>and</strong> <strong>the</strong>ir accuracy is <strong>of</strong>ten limited by<br />
<strong>the</strong> simplicity <strong>of</strong> <strong>the</strong> model itself [6]. To achieve high accuracy<br />
with an independent dose calculation tool also for <strong>the</strong><br />
most complex treatment techniques, more sophisticated<br />
models are required [12,13,22]. On <strong>the</strong> o<strong>the</strong>r h<strong>and</strong>, only<br />
models that allow detailed investigations <strong>of</strong> <strong>the</strong> dosimetric<br />
accuracy, <strong>and</strong> consequently enable more strict action levels<br />
(AL), will be effective in catching systematic uncertainties<br />
<strong>of</strong> <strong>the</strong> TPS. Moreover, misinterpretations <strong>of</strong> TPS results,<br />
<strong>and</strong> <strong>the</strong> occurrence <strong>of</strong> errors associated with <strong>the</strong> limited<br />
accuracy <strong>of</strong> empirical verification models can be greatly<br />
reduced.<br />
As a general requirement, an ideal verification dose calculation<br />
model should be as independent as possible <strong>of</strong> <strong>the</strong><br />
TPS, <strong>and</strong> should be based on physical effects which are<br />
accurately described <strong>and</strong> tuned by an independent set <strong>of</strong><br />
algorithm input data [10]. Additionally, <strong>the</strong> verification<br />
s<strong>of</strong>tware implementation should provide high accuracy<br />
uncorrelated to <strong>the</strong> radio<strong>the</strong>rapy equipment in use, i.e. its<br />
accuracy should nei<strong>the</strong>r depend on <strong>the</strong> type <strong>of</strong> linear accelerator<br />
nor <strong>the</strong> photon beam energy for which it has been<br />
commissioned. To be able to verify multiple beams in an<br />
efficient way, it should manage to import treatment plan<br />
data (e.g. MLC settings) directly from <strong>the</strong> TPS or <strong>the</strong> record<br />
<strong>and</strong> verify (R&V) system.<br />
Ideally, a full QA-procedure should include verification <strong>of</strong><br />
all parameters including <strong>the</strong> patient anatomy <strong>and</strong> positioning.<br />
In <strong>the</strong> procedure suggested here <strong>the</strong> patient geometry<br />
D. Georg et al. / Radio<strong>the</strong>rapy <strong>and</strong> Oncology 85 (2007) 306–315 307<br />
is verified separately on an everyday basis. The MU verification<br />
tool will thus be used only prior to <strong>the</strong> treatment start,<br />
provided that <strong>the</strong> integrity <strong>of</strong> <strong>the</strong> database can be secured<br />
by o<strong>the</strong>r methods during <strong>the</strong> duration <strong>of</strong> <strong>the</strong> treatment<br />
period.<br />
The overall intention in modern radiation <strong>the</strong>rapy is to<br />
keep <strong>the</strong> dose delivered to <strong>the</strong> patient as close as possible<br />
to <strong>the</strong> prescribed dose, i.e. to fulfil a tight dosimetric tolerance<br />
level. Such a dosimetric tolerance level should be<br />
based on clinical considerations related to radiobiological<br />
parameters. In order to secure that a treatment falls within<br />
this dosimetric tolerance level at a given probability an action<br />
level must be derived. This action level will <strong>the</strong>n also<br />
be dependent on <strong>the</strong> accuracy <strong>of</strong> <strong>the</strong> verification tool.<br />
Hence, for a given dosimetric tolerance level <strong>and</strong> a known<br />
uncertainty in <strong>the</strong> verification, <strong>the</strong> action level that should<br />
be applied for that individual treatment plan can be estimated.<br />
Correctly applied, this concept will always result<br />
in an action level that is narrower than <strong>the</strong> dosimetric tolerance<br />
level. An MU s<strong>of</strong>tware should <strong>the</strong>refore be designed to<br />
give a high degree <strong>of</strong> accuracy, including an estimation <strong>of</strong><br />
<strong>the</strong> overall uncertainty in <strong>the</strong> dose calculation.<br />
The aim <strong>of</strong> <strong>the</strong> present work was to test <strong>and</strong> evaluate a<br />
fluence-based independent dose calculation (or MU) algorithm<br />
(for point dose calculations) against calculations from<br />
various commercial 3D treatment planning systems under<br />
clinical conditions. For that purpose clinically accepted<br />
<strong>and</strong> approved treatment plans were considered. For a subgroup,<br />
deviations were fur<strong>the</strong>r analysed by measurements.<br />
The clinical <strong>application</strong>s covered open beams, wedged<br />
beams with both physical <strong>and</strong> dynamic wedges, <strong>and</strong> step<strong>and</strong>-shoot<br />
as well as dynamic IMRT. The underlying model<br />
for independent calculations was implemented in such a<br />
way that only a few input data are needed for commissioning<br />
<strong>and</strong> tuning; thus <strong>the</strong> workload for basic algorithm input<br />
data acquisition <strong>and</strong> commissioning is reduced to a minimum.<br />
Fur<strong>the</strong>rmore, <strong>the</strong> risk for commissioning errors is largely<br />
reduced with a minimum number <strong>of</strong> input data. By<br />
analysing <strong>the</strong> resulting deviations between dose calculations<br />
performed with a TPS <strong>and</strong> MUV we have tried to assess <strong>the</strong><br />
<strong>application</strong> <strong>of</strong> action levels for independent dose checks<br />
for advanced conformal radio<strong>the</strong>rapy.<br />
Methods <strong>and</strong> materials<br />
Independent dose calculation s<strong>of</strong>tware MUV<br />
The semi-analytical model implemented in <strong>the</strong> s<strong>of</strong>tware<br />
MUV, which st<strong>and</strong>s for <strong>monitor</strong> <strong>unit</strong> verification, was based<br />
on a two step procedure: (i) calculation <strong>of</strong> <strong>the</strong> energy fluence<br />
per <strong>monitor</strong> <strong>unit</strong> exiting <strong>the</strong> treatment head, <strong>and</strong> (ii)<br />
calculation <strong>of</strong> <strong>the</strong> dose deposition in <strong>the</strong> phantom resulting<br />
from <strong>the</strong> incident energy fluence. The energy fluence part<br />
in <strong>the</strong> dose calculation takes into account <strong>the</strong> direct energy<br />
fluence, scattered radiation from an extra-focal source <strong>and</strong><br />
scattered fluence from secondary collimators, as well as<br />
backscattered radiation to <strong>the</strong> <strong>monitor</strong> chamber [19,20].<br />
The dose deposition was based on a pencil beam model, with<br />
a radial parameterisation [1,17,18]. For dose calculations,<br />
collimator transmission <strong>and</strong> <strong>the</strong> effect <strong>of</strong> rounded leaf ends
308 <strong>Clinical</strong> <strong>evaluation</strong> <strong>of</strong> fluence based MU s<strong>of</strong>tware<br />
are taken into account. These geometries were modelled<br />
equally if <strong>the</strong>y occurred in IMRT, or in asymmetric fields.<br />
The model <strong>and</strong> <strong>the</strong> s<strong>of</strong>tware were developed with <strong>the</strong><br />
intention <strong>of</strong> creating a dose per MU verification tool that requires<br />
a minimum <strong>of</strong> commissioned input data. For tuning<br />
<strong>the</strong> fluence model for open beams, only 10 measured output<br />
factors in air are recommended <strong>and</strong> <strong>the</strong> pencil beam model<br />
is solely based on <strong>the</strong> beam quality index TPR20,10 [17,19].<br />
For physical wedges, <strong>the</strong> wedge angle needs to be specified<br />
by <strong>the</strong> user. In addition, <strong>the</strong> position <strong>of</strong> <strong>the</strong> wedge in <strong>the</strong><br />
treatment head (i.e. distance from <strong>the</strong> focal source) needs<br />
to be given <strong>and</strong> two wedge factors need to be measured at<br />
10 cm depth for two different field sizes, e.g. for<br />
10 · 10 cm 2 <strong>and</strong> 20 · 20 cm 2 . From all this information a lateral<br />
wedge modulation matrix, a lateral wedge scatter matrix,<br />
<strong>and</strong> a lateral shift <strong>of</strong> beam quality are derived <strong>and</strong> used<br />
in <strong>the</strong> calculations.<br />
Ano<strong>the</strong>r novel feature <strong>of</strong> <strong>the</strong> dose verification tool MUV is<br />
its uncertainty estimation. The uncertainty prediction was<br />
based on thorough testing <strong>of</strong> <strong>the</strong> individual components <strong>of</strong><br />
<strong>the</strong> model against measurements under different treatment<br />
conditions for a variety <strong>of</strong> existing treatment machines. For<br />
example, for open beams <strong>the</strong> calculation model for <strong>the</strong> total<br />
energy fluence provided results within 1% (2 SD) [19] <strong>and</strong><br />
for irregular MLC shaped beams <strong>the</strong> total output factor<br />
(OF total) had an average absolute deviation <strong>of</strong> 0.4% <strong>and</strong> a<br />
maximum deviation <strong>of</strong> 1.7% [20]. This was lower than <strong>the</strong><br />
deviations found in a comparable investigation <strong>of</strong> a commercial<br />
treatment planning system [8]. The pencil beam<br />
model in MUV includes effects <strong>of</strong> lateral beam quality variations,<br />
which is not <strong>the</strong> case for most commercial TPSs<br />
according to <strong>the</strong> knowledge <strong>of</strong> <strong>the</strong> authors [18]. A more detailed<br />
description <strong>of</strong> <strong>the</strong> experimental benchmarking tests,<br />
which included head scatter calculations on <strong>and</strong> <strong>of</strong>f axis in<br />
open fields, dose calculations on axis in irregular MLC<br />
shaped fields at different depths, <strong>and</strong> <strong>the</strong> influence <strong>of</strong> <strong>of</strong>faxis<br />
beam s<strong>of</strong>tening (including pencil beam corrections)<br />
can be found elsewhere e.g. [17–20]. The actual uncertainty<br />
estimation implemented in MUV was based on collimator/MLC<br />
settings <strong>and</strong> treatment depth. Uncertainty<br />
estimations are desirable from any dose calculation module<br />
because <strong>the</strong>y can be helpful when defining action levels for<br />
clinical QA routine. However, <strong>the</strong> clinical implementation <strong>of</strong><br />
action levels depending on a semi-analytical uncertainty<br />
analysis <strong>and</strong> subsequent automatic warning <strong>of</strong> <strong>the</strong> user requires<br />
fur<strong>the</strong>r investigations <strong>and</strong> is beyond <strong>the</strong> scope <strong>of</strong><br />
<strong>the</strong> present study.<br />
A DICOM interface allows extracting <strong>and</strong> importing <strong>of</strong> all<br />
dosimetric (e.g. energy, MU) <strong>and</strong> geometric (e.g. leaf <strong>and</strong><br />
jaw positions) treatment data for an entire treatment plan<br />
instantaneously <strong>and</strong> automatically, which is a pre-requisite<br />
for an efficient QA process for more complex treatment<br />
techniques, such as conformal <strong>the</strong>rapy utilizing an MLC or<br />
IMRT. The final result <strong>of</strong> <strong>the</strong> dose calculation in <strong>the</strong> MUV<br />
s<strong>of</strong>tware is <strong>the</strong> dose to water in a pre-defined point <strong>of</strong> interest<br />
in a homogeneous phantom, for a composite treatment<br />
plan as well as for each individual beam. The depth <strong>of</strong> <strong>the</strong><br />
dose specification (normalisation) point in a treatment plan<br />
that is automatically exported by a TPS is <strong>the</strong> geometric<br />
depth. If a simple inhomogeneity correction is desirable<br />
because <strong>of</strong> <strong>the</strong> actual treatment situation, <strong>the</strong> calculation<br />
depth can be modified, e.g. by using some sort <strong>of</strong> radiological<br />
path length correction with respect to <strong>the</strong> dose specification<br />
point. In cases where it was obvious that depth<br />
corrections were needed, <strong>the</strong> radiological depth was used<br />
for calculations with MUV. The radiological depth (or equivalent<br />
path length – EPL) was calculated manually by measuring<br />
distances <strong>and</strong> dimensions <strong>of</strong> bulk densities directly<br />
on <strong>the</strong> final treatment plan, or could be taken from <strong>the</strong><br />
TPS if verified. If taken from <strong>the</strong> TPS, spot checks were<br />
made <strong>and</strong> <strong>the</strong> agreement between manual <strong>and</strong> computerized<br />
calculation was generally within 1–2 mm, which did<br />
not influence <strong>the</strong> final results. The point <strong>of</strong> interest in <strong>the</strong><br />
patient can be modified in all directions in MUV by <strong>the</strong> user<br />
(anterior–posterior, lateral <strong>and</strong> longitudinal) so that finally<br />
multiple points can be verified if needed.<br />
Radio<strong>the</strong>rapy equipment<br />
The independent <strong>monitor</strong> <strong>unit</strong> verification s<strong>of</strong>tware<br />
‘‘MUV’’ was distributed to five well-established radio<strong>the</strong>rapy<br />
departments across Europe (Medical University Vienna, Medical<br />
University Graz, University Hospital Basel, University<br />
Hospital Copenhagen, <strong>and</strong> University Umea˚). Algorithm input<br />
data were measured for dedicated accelerators in various<br />
photon beams. For beam configuration in MUV, <strong>the</strong> treatment<br />
head configuration (i.e. distances <strong>and</strong> thickness <strong>of</strong> field defining<br />
elements, position <strong>of</strong> <strong>the</strong> physical wedge, etc.) could be<br />
selected from a pre-defined linac database which covers all<br />
state-<strong>of</strong>-<strong>the</strong>-art accelerator br<strong>and</strong>s. The database was established<br />
taking vendor information into account <strong>and</strong> by measuring<br />
certain distances directly on <strong>the</strong> respective treatment<br />
machine. The centres <strong>and</strong> <strong>the</strong> respective equipment (treatment<br />
planning systems including applied algorithms <strong>and</strong> linear<br />
accelerators) used are listed in Table 1. All linear<br />
accelerators were equipped with an MLC <strong>and</strong> represent <strong>the</strong><br />
most common types used clinically today.<br />
For verification <strong>of</strong> calculations in homogeneous conditions<br />
measurements were performed with ionisation chambers<br />
in water phantoms or solid verification phantoms. At<br />
<strong>the</strong> Medical University Vienna, measurements were carried<br />
out in a Solid Water TM phantom with a calibrated ionisation<br />
chamber (Nuclear Enterprises, type 2611A, Volume<br />
0.3 cm 3 ) connected to a NE electrometer (Nuclear Enterprises,<br />
type 2620). In Basel a Farmer type chamber (volume<br />
0.6 cm 3 PTW Freiburg, Germany) connected to PTW Unidos<br />
electrometer was used in a scanning water phantom, while<br />
in Graz a small volume ionisation chamber (PTW, type<br />
31002, 0.125 cm 3 ) was used for verification measurements<br />
in water. The Copenhagen centre used <strong>the</strong> same type <strong>of</strong><br />
chamber but placed in a Solid Water TM phantom.<br />
<strong>Clinical</strong> testing <strong>of</strong> MUV<br />
In each centre, MUV was evaluated as a QA tool in clinical<br />
routine, i.e. MUV calculations were compared with<br />
calculations performed by <strong>the</strong> local TPS. As typically done<br />
for such independent verification calculations, ei<strong>the</strong>r a<br />
semi-infinite water phantom was assumed or <strong>the</strong> calculations<br />
were performed in a dedicated solid verification<br />
phantom. Note that for <strong>the</strong> involved TPS, only full 3D<br />
treatment plans based on CT information were considered<br />
in this study.
Table 1<br />
Overview <strong>of</strong> institutions <strong>and</strong> <strong>the</strong> respective radio<strong>the</strong>rapy equipment for clinical testing <strong>and</strong> <strong>evaluation</strong> <strong>of</strong> <strong>the</strong> independent dose verification<br />
s<strong>of</strong>tware ‘MUV’<br />
Radio<strong>the</strong>rapy institution TPS <strong>and</strong> applied algorithm Linacs Energies (MV)<br />
University Umea˚ Helax TMS (V6.1) pencil beam or collapsed cone a<br />
Siemens Primus 6/18<br />
Medical University Vienna Helax TMS (V6.1) pencil beam or collapsed cone a<br />
ELEKTA Precise 6/10/25<br />
GE SAT 43 6/10/25<br />
Medical University Graz Pinnacle (V6.2b) superposition Varian Clinac 2300 CD 6/18<br />
University Basel XiO (V4.2) convolution/superposition ELEKTA Precise 6/18<br />
University Copenhagen Eclipse (V7.3.10) pencil beam Varian Clinac 2300 EX 6/18<br />
a<br />
...applied for lung treatments only.<br />
Results were acquired for 226 individual treatment plans<br />
including a total <strong>of</strong> 815 radiation fields. Table 2 gives an<br />
overview <strong>of</strong> <strong>the</strong> considered cases as a function <strong>of</strong> treatment<br />
technique <strong>and</strong> treatment area. All different treatment techniques,<br />
ranging from regular <strong>and</strong> irregular open fields to<br />
wedged fields using a physical or dynamic wedge, <strong>and</strong> dynamic<br />
as well as step-<strong>and</strong>-shoot IMRT could be h<strong>and</strong>led with<br />
MUV <strong>and</strong> were included in this study.<br />
The accuracy <strong>of</strong> MUV against measurements, performed<br />
in a homogeneous water phantom, has been demonstrated<br />
during <strong>the</strong> design <strong>and</strong> pre-clinical testing phase [17–20].<br />
For example, for irregular MLC shaped fields a st<strong>and</strong>ard<br />
deviation <strong>of</strong> 0.47% was obtained between calculated <strong>and</strong><br />
measured output factors (in water or air) for about 300 test<br />
Table 2<br />
Summary <strong>of</strong> treatment fields, treatment techniques, treatment<br />
sites, etc., for clinical testing <strong>of</strong> <strong>the</strong> independent dose verification<br />
s<strong>of</strong>tware ‘MUV’<br />
Treatment area # <strong>of</strong> plans # <strong>of</strong> fields Techniques<br />
Pelvis 98 364 Open 273<br />
Physical wedge 46<br />
Dynamic wedge 38<br />
Step-shoot IMRT 0<br />
Dynamic IMRT 7<br />
Thorax 46 155 Open 95<br />
Physical wedge 17<br />
Dynamic wedge 36<br />
Step-shoot IMRT 7<br />
Dynamic IMRT 0<br />
Head-<strong>and</strong>-neck 71 271 Open 75<br />
Physical wedge 48<br />
Dynamic wedge 22<br />
Step-shoot IMRT 63<br />
Dynamic IMRT 63<br />
O<strong>the</strong>r 11 25 Open 3<br />
Physical wedge 20<br />
Dynamic wedge 2<br />
Step-shoot IMRT 0<br />
Dynamic IMRT 0<br />
Total 226 815 Open 446<br />
Physical wedge 131<br />
Dynamic wedge 98<br />
Step-shoot IMRT 70<br />
Dynamic IMRT 70<br />
D. Georg et al. / Radio<strong>the</strong>rapy <strong>and</strong> Oncology 85 (2007) 306–315 309<br />
cases, where 5, 10, <strong>and</strong> 20 cm depth were considered toge<strong>the</strong>r<br />
with four different MLC designs. Maximum deviations<br />
did not exceed 1.7%, even for <strong>the</strong> most irregular field shapes<br />
[20]. Therefore, <strong>the</strong> main focus <strong>of</strong> this study was <strong>the</strong> clinical<br />
<strong>application</strong> <strong>of</strong> <strong>the</strong> independent MUV s<strong>of</strong>tware. However,<br />
verification measurements were also performed for a small<br />
number <strong>of</strong> individual treatment plans encompassing in total<br />
150 beams. Of <strong>the</strong>se more than 100 beams with segmentally<br />
modulated fluence patterns (dynamic wedges <strong>and</strong> IMRT)<br />
were specifically tested as <strong>the</strong>y were not considered in detail<br />
in previous tests.<br />
Finally, all observed deviations between MUV <strong>and</strong> <strong>the</strong> different<br />
TPSs were analysed in order to assess <strong>the</strong> clinical<br />
<strong>application</strong> <strong>of</strong> realistic action levels (AL). For that purpose<br />
current results <strong>and</strong> previously performed experimental<br />
benchmarking tests <strong>of</strong> <strong>the</strong> algorithm implemented in MUV<br />
were combined [17–20].<br />
Results<br />
In general good overall agreement was found between<br />
calculations performed with <strong>the</strong> different TPS <strong>and</strong> MUV calculations,<br />
with a mean deviation per field <strong>of</strong> 0.2 ± 3.5%<br />
(1 SD), <strong>and</strong> mean deviations <strong>of</strong> 0.2 ± 2.2% for a composite<br />
treatment. For a more detailed analysis all treatments<br />
<strong>and</strong>/or fields were binned with respect to treatment area,<br />
treatment technique, <strong>and</strong> <strong>the</strong> use <strong>of</strong> geometrical depth or<br />
radiological depth, respectively.<br />
Treatment site specific deviations<br />
Fig. 1a <strong>and</strong> b present <strong>the</strong> fraction <strong>of</strong> beams with deviations<br />
between <strong>the</strong> local TPS <strong>and</strong> MUV that are exceeding a<br />
certain limit, separated for treatment site (pelvis, thorax,<br />
head-<strong>and</strong>-neck, o<strong>the</strong>r) <strong>and</strong> whe<strong>the</strong>r any depth corrections<br />
were performed. While for pelvic treatments less than 10%<br />
<strong>of</strong> all fields showed deviations larger than 3%, irrespective<br />
<strong>of</strong> radiological depth corrections, this fraction was almost<br />
40% for thorax fields <strong>and</strong> 30% for head-<strong>and</strong>-neck fields.<br />
When using <strong>the</strong> radiological depth, <strong>the</strong> fraction <strong>of</strong> beams<br />
with deviations larger than 3% could be reduced to about<br />
10% for head-<strong>and</strong>-neck <strong>and</strong> to 30% for thorax treatments.<br />
For <strong>the</strong> latter <strong>application</strong> an agreement between TPS <strong>and</strong><br />
MUV calculations for about 90% <strong>of</strong> all fields could be<br />
achieved only at <strong>the</strong> 4.5% deviation level (when applying<br />
<strong>the</strong> radiological depth).
310 <strong>Clinical</strong> <strong>evaluation</strong> <strong>of</strong> fluence based MU s<strong>of</strong>tware<br />
a<br />
Exception fraction<br />
b<br />
Exception fraction<br />
1.0<br />
0.9<br />
0.8<br />
0.7<br />
0.6<br />
0.5<br />
0.4<br />
0.3<br />
0.2<br />
0.1<br />
0.0<br />
1.0<br />
0.9<br />
0.8<br />
0.7<br />
0.6<br />
0.5<br />
0.4<br />
0.3<br />
0.2<br />
0.1<br />
0.0<br />
When analysing only those fields where information on<br />
both depths was available, <strong>the</strong> following mean values <strong>and</strong><br />
st<strong>and</strong>ard deviations were obtained when using geometric<br />
or radiological depth: 1.1 ± 5.8% versus 0.8 ± 1.7% for pelvic<br />
fields (total 157), 3.7 ± 6.6% versus 1.5 ± 2.1% for thorax<br />
fields (total 65) <strong>and</strong> 0.5 ± 7.5% versus 0.8 ± 1.4% for<br />
head-<strong>and</strong>-neck fields (total 83), respectively. Fig. 2 illustrates<br />
<strong>the</strong> improvements for radiological depth corrections<br />
<strong>and</strong> shows median <strong>and</strong> quartiles for <strong>the</strong>se <strong>application</strong>s.<br />
Treatment technique specific deviations<br />
Table 3 summarizes <strong>the</strong> observed deviations between<br />
calculations performed with MUV <strong>and</strong> with <strong>the</strong> local TPS<br />
as a function <strong>of</strong> treatment technique <strong>and</strong> treatment site.<br />
Columns ‘‘all data’’ refer to calculations where ei<strong>the</strong>r <strong>the</strong><br />
ALL DATA<br />
Pelvic<br />
Thorax<br />
Head & Neck<br />
O<strong>the</strong>r<br />
ALL sites<br />
0 1 2 3 4 5 6 7 8 9 10<br />
Deviation [%] (MUV-TPS)/MUV<br />
ONLY RAD DEPTH DATA<br />
Pelvic<br />
Thora<br />
Head & Neck<br />
ALL sites<br />
0 1 2 3 4 5 6 7 8 9 10<br />
Deviation [%] (MUV-TPS)/MUV<br />
Fig. 1. Fraction <strong>of</strong> beams with dose deviations that were exceeding a certain deviation limit, for <strong>the</strong> major treatment areas. (a) Using input<br />
data based on ei<strong>the</strong>r geometric or radiological depth, (b) using input data based on radiological depth only.<br />
geometric or <strong>the</strong> radiological depth was used while columns<br />
denoted as ‘‘RL’’ refer to calculations where solely information<br />
on <strong>the</strong> radiological depth was applied in independent<br />
calculations. Verification calculations performed for<br />
wedged beams with physical wedges were obviously done<br />
using radiological path length correction, because mean values<br />
<strong>and</strong> st<strong>and</strong>ard deviation are very similar in columns ‘‘all<br />
data’’ <strong>and</strong> ‘‘RL’’, irrespective <strong>of</strong> treatment site. This was<br />
not <strong>the</strong> case for open beams <strong>and</strong> dynamic wedges; <strong>the</strong>se<br />
techniques show much better agreement when using RL<br />
(for comparison see columns for thorax fields <strong>and</strong> head<strong>and</strong>-neck<br />
fields). In general, slightly larger deviations were<br />
obtained for wedged beams compared to open beams.<br />
In all five centres contributing to this study <strong>the</strong> most frequent<br />
IMRT <strong>application</strong> was head-<strong>and</strong>-neck, where each 63
DEVIATION [%]<br />
6%<br />
4%<br />
2%<br />
0%<br />
-2%<br />
-4%<br />
-6%<br />
-8%<br />
-10%<br />
Pelvic fields<br />
(157)<br />
fields were checked for step-<strong>and</strong>-shoot IMRT delivery <strong>and</strong><br />
dynamic MLC IMRT delivery. Mean deviations (incl. st<strong>and</strong>ard<br />
deviations) between MUV <strong>and</strong> <strong>the</strong> local TPS were<br />
1.0 ± 7.3% for dynamic IMRT delivery <strong>and</strong> 1.3 ± 3.2% for<br />
step-<strong>and</strong>-shoot IMRT delivery, respectively. Step-<strong>and</strong>-shoot<br />
IMRT results in <strong>the</strong> thorax were again biased by tissue inhomogeneity;<br />
no dynamic IMRT was performed in <strong>the</strong> thoracic<br />
region. For dynamic IMRT cases in <strong>the</strong> pelvis good agreement<br />
was obtained between MUV <strong>and</strong> <strong>the</strong> local TPS (mean:<br />
1.6 ± 1.5%).<br />
In order to verify IMRT fields against ionisation chamber<br />
measurements <strong>and</strong> to compare <strong>the</strong> achievable accuracy<br />
for IM fields with <strong>the</strong> one for open beams, a few treatment<br />
plans were recalculated in a homogeneous phantom with<br />
both MUV <strong>and</strong> <strong>the</strong> TPS. In o<strong>the</strong>r words, recalculated IMRT<br />
verification plans were considered in this part. Table 4 summarizes<br />
<strong>the</strong> results for open static beams <strong>and</strong> IMRT cases,<br />
both on an individual field basis <strong>and</strong> for composite treatment<br />
plans. These results confirm <strong>the</strong> high accuracy <strong>of</strong> <strong>the</strong><br />
independent dose/MU calculation s<strong>of</strong>tware MUV in homogeneous<br />
conditions, i.e. when comparing ionisation chamber<br />
measurements with dose calculations in identical conditions<br />
D. Georg et al. / Radio<strong>the</strong>rapy <strong>and</strong> Oncology 85 (2007) 306–315 311<br />
Thoracic fields<br />
(65)<br />
Head & neck<br />
fields (83)<br />
Fig. 2. Illustration <strong>of</strong> <strong>the</strong> improvements for radiological depth corrections at <strong>the</strong> field level. Median <strong>and</strong> quartiles for pelvic fields (total 157),<br />
thoracic fields (total 65) <strong>and</strong> head-<strong>and</strong>-neck fields (total 83) when using geometric or radiological depth for independent dose calculations<br />
(filled circles...with radiological path length correction, filled diamonds...all data).<br />
Table 3<br />
Summary <strong>of</strong> deviations between MUV <strong>and</strong> <strong>the</strong> local treatment planning system, as a function <strong>of</strong> conformal treatment technique <strong>and</strong><br />
treatment site (RL... radiological depth)<br />
Pelvic fields Thorax fields Head-<strong>and</strong>-neck fields<br />
All data RL data All data RL data All data RL data<br />
Open beams 0.5 ± 1.3% (273) 0.6 ± 1.3% (107) 2.6 ± 7.6% (95) 1.6 ± 2.2% (51) 0.5 ± 2.1% (75) 1.0 ± 1.1% (45)<br />
Physical wedges 0.9 ± 2.3% (46) 1.3 ± 2.6% (31) 1.1 ± 1.0% (17) 1.2 ± 0.9% (8) 0.6 ± 1.5% (48) 1.1 ± 1.5% (24)<br />
Dynamic wedges 0.2 ± 2.6% (38) 1.3 ± 1.5% (19) 3.2 ± 7.8% (36) 0.6 ± 2.5% (6) 0.0 ± 2.0% (22) 0.3 ± 1.4% (14)<br />
The numbers in brackets indicate <strong>the</strong> total number <strong>of</strong> fields per category<br />
in a water phantom or a solid verification phantom without<br />
homogeneities. There are, however, additional uncertainties<br />
in both TPS calculations <strong>and</strong> calculations performed<br />
with MUV, due to <strong>the</strong> extent <strong>and</strong> accuracy in modelling<br />
rounded leaf ends, tongue-<strong>and</strong>-groove effects, leaf transmission<br />
or <strong>the</strong> distribution <strong>of</strong> <strong>the</strong> direct source (X-ray target).<br />
When compared to open beams, larger mean<br />
deviations <strong>and</strong> st<strong>and</strong>ard deviations for individual IMRT fields<br />
(see Table 4a) are also influenced by <strong>the</strong> larger overall<br />
experimental uncertainty for ionisation chamber measurements<br />
in IMRT treatments [24]. Large relative deviations<br />
are also influenced by <strong>the</strong> beam contribution to <strong>the</strong> overall<br />
treatment plan <strong>and</strong> for composite treatment plans excellent<br />
agreement was found between ionisation chamber measurements<br />
<strong>and</strong> calculations performed with MUV, see Table 4b.<br />
<strong>Clinical</strong> action levels<br />
Fig. 3a <strong>and</strong> b show treatment site dependent frequency<br />
distributions <strong>of</strong> deviations between MUV <strong>and</strong> TPS calculations.<br />
The dashed lines indicate a deviation level <strong>of</strong> ±3% or<br />
±5%. For all treatment sites <strong>the</strong>re were systematic deviations<br />
which are biased by dose calculation uncertainties
312 <strong>Clinical</strong> <strong>evaluation</strong> <strong>of</strong> fluence based MU s<strong>of</strong>tware<br />
Table 4<br />
Comparison <strong>of</strong> dose calculations <strong>and</strong> ionisation chamber (IC) measurements for individual treatment fields performed under identical<br />
conditions in a water phantom or a solid water equivalent verification phantom<br />
Treatment technique<br />
(a) Individual fields<br />
Number <strong>of</strong> fields (MUV IC)/IC (mean ± 1 SD) (%) (TPS IC)/IC (mean ± 1 SD) (%)<br />
Open irregular fields 47 0.7 ± 0.6 0.3 ± 1.0<br />
Dynamic IMRT 56 0.7 ± 4.1 1.0 ± 5.8<br />
Step-<strong>and</strong>-shoot IMRT 48 0.6 ± 2.5 1.1 ± 3.3<br />
Number <strong>of</strong> plans (MUV IC)/IC (mean ± 1 SD) (%) (TPS IC)/IC (mean ± 1 SD) (%)<br />
(b) Composite treatment plan<br />
Open irregular fields 12 0.4 ± 0.6 0.4 ± 1.1<br />
Dynamic IMRT 9 0.1 ± 1.1 1.5 ± 3.0<br />
Step-<strong>and</strong>-shoot IMRT 7 0.3 ± 1.0 1.7 ± 0.9<br />
<strong>and</strong> <strong>the</strong> fact that dose calculations in a homogeneous flat<br />
water equivalent medium were compared with dose calculations<br />
that were based on CT information. Best agreement<br />
between TPS <strong>and</strong> independent dose calculations was observed<br />
for pelvic fields. When using radiological depth information<br />
<strong>the</strong> majority (98%) <strong>of</strong> all deviations was within ±5%,<br />
for pelvic <strong>and</strong> head-<strong>and</strong>-neck fields even within ±3% ( 92%<br />
<strong>of</strong> all fields).<br />
From <strong>the</strong> results <strong>of</strong> ionisation chamber measurements<br />
presented in Table 4a <strong>and</strong> from previously published experimental<br />
verification <strong>of</strong> MUV in homogeneous conditions,<br />
treatment technique dependent confidence intervals were<br />
defined as follows. For open beams <strong>the</strong> confidence interval<br />
in a homogeneous medium was even as small as ±2%. However,<br />
for <strong>the</strong> implementation <strong>of</strong> clinical action levels additional<br />
uncertainties need to be considered that account<br />
for different dose calculation conditions for <strong>the</strong> TPS <strong>and</strong><br />
independent verification calculations, i.e. effects related<br />
to patient anatomy <strong>and</strong> inhomogeneities. These additional<br />
tolerances were estimated from <strong>the</strong> results presented in<br />
Figs. 1–3 <strong>and</strong> Table 3. When applying radiological depth<br />
corrections a clinical action level <strong>of</strong> ±3% (open) <strong>and</strong> ±5%<br />
(wedged <strong>and</strong> IMRT), respectively, seems to be suitable for<br />
pelvic <strong>and</strong> head-<strong>and</strong>-neck treatments. For thorax treatments,<br />
even with radiological depth correction, a site specific<br />
additional uncertainty <strong>of</strong> 3% seems to be necessary<br />
for all treatment techniques. If no radiological depth correction<br />
is performed site dependent additional uncertainties<br />
<strong>of</strong> 2% are recommended for head-<strong>and</strong>-neck treatments<br />
<strong>and</strong> 5% for thorax treatments.<br />
Discussion<br />
Dose calculations performed with a treatment planning<br />
system (TPS) can be verified with different approaches.<br />
Although quality assurance (QA) <strong>of</strong> TPS has been recognized<br />
as an important topic for many years, practical guidelines or<br />
recommendations for performance verification <strong>and</strong> periodic<br />
QA <strong>of</strong> TPS have become available only recently [10,15,16].<br />
The detection <strong>of</strong> systematic errors in TPS calculations requires<br />
extensive or ‘‘stress’’ testing, which is difficult to<br />
perform in practice because no specific recommendation<br />
is available addressing <strong>the</strong> number <strong>of</strong> tests, test conditions,<br />
etc. On <strong>the</strong> o<strong>the</strong>r h<strong>and</strong>, if systematic uncertainties under<br />
specific conditions remain overlooked, <strong>the</strong> quality <strong>of</strong> a<br />
radio<strong>the</strong>rapy treatment is limited <strong>and</strong> no corrective actions<br />
can be set. An intelligent design to carry out such stress<br />
tests in an efficient way for a particular TPS requires a priori<br />
knowledge <strong>of</strong> <strong>the</strong> dose calculation algorithm. For those reasons<br />
stress tests are very <strong>of</strong>ten based on experimental techniques.<br />
In that aspect dedicated dose calculation s<strong>of</strong>tware,<br />
which is designed to achieve as high dose calculation accuracy<br />
in homogeneous conditions as possible, can be very<br />
helpful in order to keep <strong>the</strong> workload at an acceptable level.<br />
From <strong>the</strong> results obtained within <strong>the</strong> present study<br />
<strong>and</strong> from previously published articles from <strong>the</strong> same<br />
authors [17–20], we conclude that MUV can be considered<br />
as such a tool.<br />
Besides systematic TPS tests <strong>and</strong> QA during <strong>the</strong> commissioning<br />
phase it is also recommended to use a second independent<br />
MU calculation to verify <strong>the</strong> MU data produced by<br />
<strong>the</strong> TPS as part <strong>of</strong> patient specific QA. For many years<br />
empirical factor based formalisms or in-vivo dosimetry have<br />
been in use for independent dose verification e.g. [3,5].<br />
These procedures were governed by fairly simple treatment<br />
techniques with ra<strong>the</strong>r uncomplicated planning procedures.<br />
In <strong>the</strong> light <strong>of</strong> advanced treatment techniques based on MLC<br />
technology <strong>and</strong> complex planning procedures <strong>the</strong> general<br />
properties <strong>of</strong> independent dose calculation need to be<br />
reconsidered. Dem<strong>and</strong>s on accuracy could be shifted towards<br />
<strong>the</strong> st<strong>and</strong>ards <strong>of</strong> today’s planning dose calculations<br />
or even higher; single point dose verification in a semi-infinite<br />
slab approximation could be replaced by 2D (or 3D) calculations<br />
taking into account <strong>the</strong> patients’ anatomy. In<br />
o<strong>the</strong>r words, independent dose calculation algorithms can<br />
be designed to provide a high level <strong>of</strong> accuracy, even when<br />
patient anatomy is included. Depending on how well <strong>the</strong><br />
independent dose calculation is integrated into <strong>the</strong> clinical<br />
workflow long calculation times may not constitute an actual<br />
problem. For example, QA-procedures for dose calculation<br />
can be designed to run automatically, i.e. without<br />
dem<strong>and</strong>ing any manual operations, by executing verification<br />
calculations on all treatment plans prior to <strong>the</strong> treatment<br />
start from a ‘‘QA robot’’, which is for example linked to<br />
<strong>the</strong> database <strong>of</strong> <strong>the</strong> record <strong>and</strong> verify (R&V) system. Treatment<br />
plans exceeding a certain deviation could be marked<br />
in <strong>the</strong> database <strong>and</strong> a notification is sent to clinical physicists.<br />
This is also an attractive concept to fulfil QA <strong>and</strong> pa-
a<br />
b<br />
Frequency<br />
Frequency<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
0<br />
-11%<br />
-10%<br />
-11%<br />
-10%<br />
-9%<br />
-8%<br />
-7%<br />
-6%<br />
-5%<br />
-4%<br />
-3%<br />
-2%<br />
tient safety regulations because all treatment plans would<br />
be subjected to automated independent dose calculations.<br />
Ideally, such an automated procedure is followed by a retrospective<br />
analysis that continuously scans through <strong>the</strong><br />
database looking for systematic sources <strong>of</strong> dose calculation<br />
error/uncertainties. This may consequently be an additional<br />
QA strategy where small but systematic error/uncertainties,<br />
ei<strong>the</strong>r in <strong>the</strong> planning calculation or in <strong>the</strong> independent dose<br />
calculation, can be found <strong>and</strong> possibly also explained <strong>and</strong><br />
fixed. However, for such an automated QA-procedure it is<br />
still necessary to check <strong>the</strong> treatment plan by an experi-<br />
D. Georg et al. / Radio<strong>the</strong>rapy <strong>and</strong> Oncology 85 (2007) 306–315 313<br />
All data<br />
Deviation (MUV-TPS)/MUV [%]<br />
Only radiological depth data<br />
-9%<br />
-8%<br />
-7%<br />
-6%<br />
-5%<br />
-4%<br />
-3%<br />
-2%<br />
-1%<br />
0%<br />
1%<br />
2%<br />
3%<br />
Deviation (MUV-TPS)/MUV [%]<br />
thorax<br />
HN<br />
pelvic<br />
-1%<br />
0%<br />
1%<br />
2%<br />
3%<br />
4%<br />
5%<br />
6%<br />
7%<br />
8%<br />
9%<br />
RD thorax<br />
RD HN<br />
RD pelvis<br />
enced pr<strong>of</strong>essional in order to avoid hot spots, dose prescription<br />
<strong>and</strong> plan normalisation errors. Independent dose<br />
calculations based on export files from TPS do not check<br />
correct data file transfer from <strong>the</strong> TPS to <strong>the</strong> treatment <strong>unit</strong><br />
<strong>and</strong> <strong>the</strong> actual performance <strong>of</strong> <strong>the</strong> treatment <strong>unit</strong>, which<br />
are o<strong>the</strong>r sources <strong>of</strong> error in <strong>the</strong> radio<strong>the</strong>rapy chain. However,<br />
<strong>the</strong>se aspects could be included by measuring leaf settings<br />
<strong>and</strong> MU measured with an EPID [23]. Moreover, such<br />
information could be used as well as input information for<br />
an independent dose calculation. Finally, <strong>the</strong>re is also a tangible<br />
risk for errors to be introduced by <strong>the</strong> user(s) during<br />
10%<br />
4%<br />
5%<br />
6%<br />
7%<br />
8%<br />
9%<br />
10%<br />
Fig. 3. Treatment site dependent frequency distributions <strong>of</strong> deviations between dose calculations performed with MUV <strong>and</strong> <strong>the</strong> local TPS. (a)<br />
Using input data based on ei<strong>the</strong>r geometric or radiological depth, (b) using input data based on radiological depth only.
314 <strong>Clinical</strong> <strong>evaluation</strong> <strong>of</strong> fluence based MU s<strong>of</strong>tware<br />
<strong>the</strong> planning <strong>and</strong> preparation procedure [25], <strong>of</strong>ten due to<br />
simple human mistakes in combination with inappropriate<br />
clinical routines.<br />
As long as patient anatomy is not included in verification<br />
calculations <strong>the</strong> accuracy <strong>of</strong> independent dose checks is influenced<br />
by treatment site specific factors. This is <strong>the</strong> most<br />
striking limitation <strong>of</strong> independent dose calculation procedures<br />
that are employed in clinics today. For some treatment<br />
areas, such as thorax <strong>and</strong> head-<strong>and</strong>-neck, accurate results<br />
cannot be achieved in simple calculation conditions, i.e. a<br />
semi-infinite homogeneous phantom. With radiological depth<br />
corrections, for head-<strong>and</strong>-neck treatments almost as good results<br />
as for pelvic treatment could be achieved (see Fig. 1a<br />
<strong>and</strong> b). Interestingly, <strong>the</strong> impact <strong>of</strong> radiological depth correction<br />
was limited for pelvic treatments. This might be biased<br />
by <strong>the</strong> class solutions, i.e. beam geometry, applied in <strong>the</strong> centres<br />
participating in <strong>the</strong> study. Although for thorax fields <strong>the</strong><br />
agreement between TPS <strong>and</strong> independent MU calculations<br />
was largely improved when using radiological depth information,<br />
<strong>the</strong> overall agreement was inferior compared to <strong>the</strong><br />
o<strong>the</strong>r treatment areas. This can be explained by <strong>the</strong> overestimated<br />
scatter when performing calculations in a water equivalent<br />
homogeneous medium <strong>and</strong> comparing <strong>the</strong>m with<br />
calculations accounting for differences in scatter conditions<br />
from inhomogeneous media.<br />
When defining action levels for any QA process <strong>the</strong> uncertainties<br />
<strong>of</strong> procedures or calculations, which are used to derive<br />
a certain value, need to be considered. A proper<br />
selection <strong>of</strong> action level is a compromise between probabilities<br />
<strong>of</strong> dose deviations outside <strong>the</strong> clinical tolerance level<br />
<strong>and</strong> workload generated by false alarms. To ensure narrow<br />
tolerance levels with an acceptable workload it is important<br />
to use a verification tool capable <strong>of</strong> high accuracy. Fur<strong>the</strong>r,<br />
when <strong>the</strong> accuracy <strong>of</strong> <strong>the</strong> verification tool is dependent on<br />
irradiation parameters inherent uncertainty estimation will<br />
help optimising <strong>the</strong> QA-procedure.<br />
Unfortunately, uncertainties are not accounted for in an<br />
open <strong>and</strong> sincere manner, even though <strong>the</strong>y are inevitable<br />
when aiming to model complex processes such as dose deposition<br />
in a patient. A well-known fact concerning computer<br />
calculations is that in practice some sort <strong>of</strong> ‘‘priority-compromise’’<br />
needs to be found between speed <strong>and</strong> accuracy. In that<br />
aspect <strong>the</strong> importance <strong>of</strong> presenting also flaws <strong>and</strong> weaknesses<br />
<strong>of</strong> a dose calculations model by <strong>the</strong> companies that<br />
market TPSs must be emphasized. Such issues are <strong>of</strong>ten discussed<br />
in a scientific context, but probably not as frequently<br />
in <strong>the</strong> clinical routine work. Because <strong>the</strong> accuracy <strong>of</strong> independent<br />
dose verification depends on input data (e.g. geometric<br />
versus radiological depth), treatment area (e.g. missing tissue),<br />
<strong>and</strong> treatment specific beam data (e.g. beam weight<br />
to overall plan, weight <strong>of</strong> wedge) clinical AL should be defined<br />
treatment site <strong>and</strong> treatment technique specific.<br />
Conclusion<br />
The s<strong>of</strong>tware MUV is well suited for patient specific treatment<br />
plan QA <strong>application</strong>s <strong>and</strong> can h<strong>and</strong>le all currently<br />
available treatment techniques that can be applied with<br />
st<strong>and</strong>ard linear accelerators, such as regular <strong>and</strong> irregular<br />
open beams, physical <strong>and</strong> dynamic wedges, step-<strong>and</strong>-shoot<br />
<strong>and</strong> dynamic IMRT. The highly accurate dose calculation<br />
model implemented in MUV allows investigating systematic<br />
TPS deviations by performing calculations in homogeneous<br />
conditions.<br />
Information on <strong>the</strong> uncertainty from any dose calculation<br />
algorithm would both enhance <strong>and</strong> simplify <strong>the</strong> process<br />
<strong>of</strong> setting clinical action levels that identify cases<br />
where <strong>the</strong> discrepancies between planning <strong>and</strong> independent<br />
dose calculations need follow up. However, fur<strong>the</strong>r<br />
research is needed in that aspect. Based on <strong>the</strong> current<br />
findings treatment site <strong>and</strong> treatment technique dependent<br />
action levels between 3% <strong>and</strong> 5% seem to be clinically<br />
realistic if a radiological depth correction is<br />
performed.<br />
Acknowledgements<br />
This work was partly supported by ESTRO <strong>and</strong> performed within<br />
<strong>the</strong> framework <strong>of</strong> <strong>the</strong> ESQUIRE project <strong>and</strong> partly supported by <strong>the</strong><br />
Cancer Research foundation in Nor<strong>the</strong>rn Sweden.<br />
* Corresponding author. Dietmar Georg, Division <strong>of</strong> Medical<br />
Radiation Physics, Department <strong>of</strong> Radio<strong>the</strong>rapy, Medical University<br />
Vienna/AKH Vienna, Währinger Gürtel 18-20, A-1090 Vienna,<br />
Austria. E-mail address: Dietmar.Georg@akhwien.at<br />
Received 13 September 2006; received in revised form 9 March<br />
2007; accepted 24 April 2007; Available online 27 September 2007<br />
References<br />
[1] Ahnesjö A, Saxner M, Trepp A. A pencil beam model for photon<br />
dose calculation. Med Phys 1992;19:263–73.<br />
[2] Brahme A. Dosimetric precision requirements in radiation<br />
<strong>the</strong>rapy. Acta Radiol Oncol 1984;23:379–91.<br />
[3] Dutreix A, Svensson H, Bjärngard BE, Bridier A, Mijnheer A,<br />
Shaw J. Monitor <strong>unit</strong> calculation for high energy photon<br />
beams, Physics for clinical radio<strong>the</strong>rapy. Booklet No. 3,<br />
ESTRO; 1997.<br />
[4] Ferreira IH, Dutreix A, Bridier A, Chavaudra J, Svensson H. The<br />
ESTRO-QUALity assurance network (EQUAL). Radio<strong>the</strong>r Oncol<br />
2000;55:273–84.<br />
[5] Fiorino C, Corletto D, Mangili P, Broggi S, Bonini A, Cattaneo<br />
GM, et al. Quality assurance by systematic in vivo dosimetry:<br />
results on a large cohort <strong>of</strong> patients. Radio<strong>the</strong>r Oncol<br />
2000;56:85–95.<br />
[6] Georg D, Ol<strong>of</strong>sson J, Künzler T, Karlsson M. On empirical<br />
methods to determine scatter factors for irregular MLC shaped<br />
beams. Med Phys 2004;31:2222–9.<br />
[7] Gillis S, De Wagter C, Bohsung J, Perrin B, Williams P, Mijnheer<br />
BJ. An inter-centre quality assurance network for IMRT<br />
verification: results <strong>of</strong> <strong>the</strong> ESTRO QUASIMODO project. Radio<strong>the</strong>r<br />
Oncol 2005;76:340–53.<br />
[8] Hansson H, Bjork P, Knöös T, Nilsson P. Verification <strong>of</strong> a pencil<br />
beam based treatment planning system: output factors for<br />
open photon beams shaped with MLC or blocks. Phys Med Biol<br />
1999;44:N201–7.<br />
[9] Heeren G. The bright but ephemeral life <strong>of</strong> a rainbow: a<br />
chronicle <strong>of</strong> seventeen years <strong>of</strong> intensive ESTRO-EU cooperation.<br />
Radio<strong>the</strong>r Oncol 2005;75:253–7.<br />
[10] IAEA Technical Reports Series No. 430: Commissioning <strong>and</strong><br />
quality assurance <strong>of</strong> computerized planning systems for radiation<br />
treatment <strong>of</strong> cancer. International atomic energy<br />
agency, IAEA; 2005.
[11] Knöös T, Johnsson SA, Ceberg CP, Tomaszewicz A, Nilsson<br />
P. Independent checking <strong>of</strong> <strong>the</strong> delivered dose for highenergy<br />
X-rays using a h<strong>and</strong>-held PC. Radio<strong>the</strong>r Oncol<br />
2001;58:201–8.<br />
[12] Linthout N, Verellen D, Van Acker S, Storme G. A simple<br />
<strong>the</strong>oretical verification <strong>of</strong> <strong>monitor</strong> <strong>unit</strong> calculation for intensity<br />
modulated beams using dynamic mini-multileaf collimation.<br />
Radio<strong>the</strong>r Oncol 2004;71:235–41.<br />
[13] Ma CM, Price RA, Li JS, Chen L, Wang L, Forkal E, et al.<br />
Monitor <strong>unit</strong> calculation for Monte Carlo treatment planning.<br />
Phys Med Biol 2004:1671–87.<br />
[14] Mijnheer B, Battermann JJ, Wambersie A. What degree <strong>of</strong><br />
accuracy is required <strong>and</strong> can be achieved in photon <strong>and</strong><br />
neutron <strong>the</strong>rapy? Radio<strong>the</strong>r Oncol 1987;8:237–52.<br />
[15] Mijnheer B, Olszewska A, Fiorino C, Hartmann G, Knöös T.A<br />
practical guide to quality control <strong>of</strong> brachy<strong>the</strong>rapy equipment.<br />
ESTRO Booklet No. 8; 2004.<br />
[16] NCS Report 15, Quality assurance <strong>of</strong> 3-D treatment planning<br />
systems for external photon <strong>and</strong> electron beams: practical<br />
guidelines for acceptance testing, commissioning <strong>and</strong> periodic<br />
quality control <strong>of</strong> radiation <strong>the</strong>rapy treatment planning<br />
systems. Ne<strong>the</strong>rl<strong>and</strong>s commission on radiation dosimetry;<br />
2006.<br />
[17] Nyholm T, Ol<strong>of</strong>sson J, Ahnesjö A, Karlsson M. Photon pencil<br />
kernel parameterisation based on beam quality index. Radio<strong>the</strong>r<br />
Oncol 2006;78:347–51.<br />
D. Georg et al. / Radio<strong>the</strong>rapy <strong>and</strong> Oncology 85 (2007) 306–315 315<br />
[18] Nyholm T, Ol<strong>of</strong>sson J, Ahnesjö A, Karlsson M. Modelling lateral<br />
beam quality variations in pencil beam kernel based photon<br />
dose calculations. Phys Med Biol 2006;51:4111–8.<br />
[19] Ol<strong>of</strong>sson J, Georg D, Karisson M. A widely tested model for<br />
head scatter influence on photon beam output. Radio<strong>the</strong>r<br />
Oncol 2003;67:225–38.<br />
[20] Ol<strong>of</strong>sson J, Nyholm T, Georg D, Ahnesjö A, Karlsson M.<br />
Evaluation <strong>of</strong> uncertainty predictions <strong>and</strong> dose output for<br />
model based dose calculations in photon beams from multiple<br />
linacs. Med Phys 2006;33:2548–56.<br />
[21] Venselaar J, Welleweerd H. Application <strong>of</strong> a test package in an<br />
intercomparison <strong>of</strong> <strong>the</strong> photon dose calculation performance<br />
<strong>of</strong> treatment planning systems used in a clinical setting.<br />
Radio<strong>the</strong>r Oncol 2001;60:203–13.<br />
[22] Watanabe Y. Point dose calculations using an analytical pencil<br />
beam kernel for IMRT plan checking. Phys Med Biol<br />
2001:1013–38.<br />
[23] Winkler P, Hefner A, Georg D. Dose-response characteristics <strong>of</strong><br />
an amorphous silicon EPID. Med Phys 2005;32:3095–105.<br />
[24] Woo MK, Nico A. Impact <strong>of</strong> multileaf collimator leaf positioning<br />
accuracy on intensity modulation radiation <strong>the</strong>rapy quality<br />
assurance ion chamber measurements. Med Phys<br />
2005;32:1440–5.<br />
[25] Yeung KT, Bortolotto K, Cosby S, Hoar M, Lederer E. Quality<br />
assurance in radio<strong>the</strong>rapy: <strong>evaluation</strong> <strong>of</strong> errors <strong>and</strong> incidents<br />
recorded over a 10 year period. Radio<strong>the</strong>r Oncol 2005;74:283–91.