3 - World Journal of Gastroenterology
3 - World Journal of Gastroenterology
3 - World Journal of Gastroenterology
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Radiology<br />
<strong>World</strong> J Radiol 2011 March 28; 3(3): 55-84<br />
www.wjgnet.com<br />
ISSN 1949-8470 (online)
W J R<br />
PRESIDENT AND EDITOR-IN-<br />
CHIEF<br />
Lian-Sheng Ma, Beijing<br />
STRATEGY ASSOCIATE<br />
EDITORS-IN-CHIEF<br />
Ritesh Agarwal, Chandigarh<br />
Kenneth Coenegrachts, Bruges<br />
Mannudeep K Kalra, Boston<br />
Meng Law, Lost Angeles<br />
Ewald Moser, Vienna<br />
Aytekin Oto, Chicago<br />
AAK Abdel Razek, Mansoura<br />
Àlex Rovira, Barcelona<br />
Yi-Xiang Wang, Hong Kong<br />
Hui-Xiong Xu, Guangzhou<br />
GUEST EDITORIAL BOARD<br />
MEMBERS<br />
Wing P Chan, Taipei<br />
Wen-Chen Huang, Taipei<br />
Shi-Long Lian, Kaohsiung<br />
Chao-Bao Luo, Taipei<br />
Shu-Hang Ng, Taoyuan<br />
Pao-Sheng Yen, Haulien<br />
MEMBERS OF THE EDITORIAL<br />
BOARD<br />
Australia<br />
Karol Miller, Perth<br />
Tomas Kron, Melbourne<br />
Zhonghua Sun, Perth<br />
Austria<br />
Herwig R Cerwenka, Graz<br />
Editorial Board<br />
2009-2013<br />
The <strong>World</strong> <strong>Journal</strong> <strong>of</strong> Radiology Editorial Board consists <strong>of</strong> 319 members, representing a team <strong>of</strong> worldwide experts<br />
in radiology. They are from 40 countries, including Australia (3), Austria (4), Belgium (5), Brazil (3), Canada (9),<br />
Chile (1), China (25), Czech (1), Denmark (1), Egypt (4), Estonia (1), Finland (1), France (6), Germany (17), Greece<br />
(8), Hungary (1), India (9), Iran (5), Ireland (1), Israel (4), Italy (28), Japan (14), Lebanon (1), Libya (1), Malaysia (2),<br />
Mexico (1), Netherlands (4), New Zealand (1), Norway (1), Saudi Arabia (3), Serbia (1), Singapore (2), Slovakia (1),<br />
South Korea (16), Spain (8), Switzerland (5), Thailand (1), Turkey (20), United Kingdom (16), and United States (82).<br />
WJR|www.wjgnet.com<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Radiology<br />
Daniela Prayer,Vienna<br />
Siegfried Trattnig, Vienna<br />
Belgium<br />
Piet R Dirix, Leuven<br />
Yicheng Ni, Leuven<br />
Piet Vanhoenacker, Aalst<br />
Jean-Louis Vincent, Brussels<br />
Brazil<br />
Emerson L Gasparetto, Rio de Janeiro<br />
Edson Marchiori, Petrópolis<br />
Wellington P Martins, São Paulo<br />
Canada<br />
Sriharsha Athreya, Hamilton<br />
Mark Otto Baerlocher, Toronto<br />
Martin Charron, Toronto<br />
James Chow, Toronto<br />
John Martin Kirby, Hamilton<br />
Piyush Kumar, Edmonton<br />
Catherine Limperpoulos, Quebec<br />
Ernest K Osei, Kitchener<br />
Weiguang Yao, Sudbury<br />
Chile<br />
Masami Yamamoto, Santiago<br />
China<br />
Feng Chen, Nanjing<br />
Ying-Sheng Cheng, Shanghai<br />
Woei-Chyn Chu, Taipei<br />
Guo-Guang Fan, Shenyang<br />
Shen Fu, Shanghai<br />
Gang Jin, Beijing<br />
Tak Yeung Leung, Hong Kong<br />
Wen-Bin Li, Shanghai<br />
Rico Liu, Hong Kong<br />
Yi-Yao Liu, Chengdu<br />
Wei Lu, Guangdong<br />
Fu-Hua Peng, Guangzhou<br />
Li-Jun Wu, Hefei<br />
Zhi-Gang Yang, Chengdu<br />
Xiao-Ming Zhang, Nanchong<br />
Chun-Jiu Zhong, Shanghai<br />
Czech<br />
Vlastimil Válek, Brno<br />
Denmark<br />
Poul Erik Andersen, Odense<br />
Egypt<br />
Mohamed Abou El-Ghar, Mansoura<br />
Mohamed Ragab Nouh, Alexandria<br />
Ahmed A Shokeir, Mansoura<br />
Estonia<br />
Tiina Talvik, Tartu<br />
Finland<br />
Tove J Grönroos, Turku<br />
I March 28, 2011
France<br />
Alain Chapel, Fontenay-Aux-Roses<br />
Nathalie Lassau, Villejuif<br />
Youlia M Kirova, Paris<br />
Géraldine Le Duc, Grenoble Cedex<br />
Laurent Pierot, Reims<br />
Frank Pilleul, Lyon<br />
Pascal Pommier, Lyon<br />
Germany<br />
Ambros J Beer, München<br />
Thomas Deserno, Aachen<br />
Frederik L Giesel, Heidelberg<br />
Ulf Jensen, Kiel<br />
Markus Sebastian Juchems, Ulm<br />
Kai U Juergens, Bremen<br />
Melanie Kettering, Jena<br />
Jennifer Linn, Munich<br />
Christian Lohrmann, Freiburg<br />
David Maintz, Münster<br />
Henrik J Michaely, Mannheim<br />
Oliver Micke, Bielefeld<br />
Thoralf Niendorf, Berlin-Buch<br />
Silvia Obenauer, Duesseldorf<br />
Steffen Rickes, Halberstadt<br />
Lars V Baron von Engelhardt, Bochum<br />
Goetz H Welsch, Erlangen<br />
Greece<br />
Panagiotis Antoniou, Alexandroupolis<br />
George C Kagadis, Rion<br />
Dimitris Karacostas, Thessaloniki<br />
George Panayiotakis, Patras<br />
Alexander D Rapidis, Athens<br />
C Triantopoulou, Athens<br />
Ioannis Tsalafoutas, Athens<br />
Virginia Tsapaki, Anixi<br />
Ioannis Valais, Athens<br />
Hungary<br />
Peter Laszlo Lakatos, Budapest<br />
India<br />
Anil Kumar Anand, New Delhi<br />
Surendra Babu, Tamilnadu<br />
Sandip Basu, Bombay<br />
Kundan Singh Chufal, New Delhi<br />
Shivanand Gamanagatti, New Delhi<br />
Vimoj J Nair, Haryana<br />
R Prabhakar, New Delhi<br />
Sanjeeb Kumar Sahoo, Orissa<br />
Iran<br />
Vahid Reza Dabbagh Kakhki, Mashhad<br />
Mehran Karimi, Shiraz<br />
Farideh Nejat, Tehran<br />
Alireza Shirazi, Tehran<br />
Hadi Rokni Yazdi, Tehran<br />
WJR|www.wjgnet.com<br />
Ireland<br />
Joseph Simon Butler, Dublin<br />
Israel<br />
Amit Gefen, Tel Aviv<br />
Eyal Sheiner, Be’er-Sheva<br />
Jacob Sosna, Jerusalem<br />
Simcha Yagel, Jerusalem<br />
Italy<br />
Mohssen Ansarin, Milan<br />
Stefano Arcangeli, Rome<br />
Tommaso Bartalena, Imola<br />
Filippo Cademartiri, Parma<br />
Sergio Casciaro, Lecce<br />
Laura Crocetti, Pisa<br />
Alberto Cuocolo, Napoli<br />
Mirko D’On<strong>of</strong>rio, Verona<br />
Massimo Filippi, Milan<br />
Claudio Fiorino, Milano<br />
Alessandro Franchello, Turin<br />
Roberto Grassi, Naples<br />
Stefano Guerriero, Cagliari<br />
Francesco Lassandro, Napoli<br />
Nicola Limbucci, L'Aquila<br />
Raffaele Lodi, Bologna<br />
Francesca Maccioni, Rome<br />
Laura Martincich, Candiolo<br />
Mario Mascalchi, Florence<br />
Roberto Miraglia, Palermo<br />
Eugenio Picano, Pisa<br />
Antonio Pinto, Naples<br />
Stefania Romano, Naples<br />
Luca Saba, Cagliari<br />
Sergio Sartori, Ferrara<br />
Mariano Scaglione, Castel Volturno<br />
Lidia Strigari, Rome<br />
Vincenzo Valentini, Rome<br />
Japan<br />
Shigeru Ehara, Morioka<br />
Nobuyuki Hamada, Chiba<br />
Takao Hiraki, Okayama<br />
Akio Hiwatashi, Fukuoka<br />
Masahiro Jinzaki, Tokyo<br />
Hiroshi Matsuda, Saitama<br />
Yasunori Minami, Osaka<br />
Jun-Ichi Nishizawa, Tokyo<br />
Tetsu Niwa, Yokohama<br />
Kazushi Numata, Kanagawa<br />
Kazuhiko Ogawa, Okinawa<br />
Hitoshi Shibuya, Tokyo<br />
Akira Uchino, Saitama<br />
Haiquan Yang, Kanagawa<br />
Lebanon<br />
Aghiad Al-Kutoubi, Beirut<br />
Libya<br />
Anuj Mishra, Tripoli<br />
Malaysia<br />
R Logeswaran, Cyberjaya<br />
Kwan-Hoong Ng, Kuala Lumpur<br />
Mexico<br />
Heriberto Medina-Franco, Mexico City<br />
Netherlands<br />
Jurgen J Fütterer, Nijmegen<br />
Raffaella Rossin, Eindhoven<br />
Paul E Sijens, Groningen<br />
Willem Jan van Rooij, Tilburg<br />
New Zealand<br />
W Howell Round, Hamilton<br />
Norway<br />
Arne Sigmund Borthne, Lørenskog<br />
Saudi Arabia<br />
Mohammed Al-Omran, Riyadh<br />
Ragab Hani Donkol, Abha<br />
Volker Rudat, Al Khobar<br />
Serbia<br />
Djordjije Saranovic, Belgrade<br />
Singapore<br />
Uei Pua, Singapore<br />
Lim CC Tchoyoson, Singapore<br />
Slovakia<br />
František Dubecký, Bratislava<br />
South Korea<br />
Bo-Young Choe, Seoul<br />
Joon Koo Han, Seoul<br />
Seung Jae Huh, Seoul<br />
Chan Kyo Kim, Seoul<br />
Myeong-Jin Kim, Seoul<br />
Seung Hyup Kim, Seoul<br />
Kyoung Ho Lee, Gyeonggi-do<br />
Won-Jin Moon, Seoul<br />
Wazir Muhammad, Daegu<br />
Jai Soung Park, Bucheon<br />
Noh Hyuck Park, Kyunggi<br />
Sang-Hyun Park, Daejeon<br />
Joon Beom Seo, Seoul<br />
Ji-Hoon Shin, Seoul<br />
Jin-Suck Suh, Seoul<br />
Hong-Gyun Wu, Seoul<br />
II March 28, 2011
Spain<br />
Eduardo J Aguilar, Valencia<br />
Miguel Alcaraz, Murcia<br />
Juan Luis Alcazar, Pamplona<br />
Gorka Bastarrika, Pamplona<br />
Rafael Martínez-Monge, Pamplona<br />
Alberto Muñoz, Madrid<br />
Joan C Vilanova, Girona<br />
Switzerland<br />
Nicolau Beckmann, Basel<br />
Silke Grabherr, Lausanne<br />
Karl-Ol<strong>of</strong> Lövblad, Geneva<br />
Tilo Niemann, Basel<br />
Martin A Walter, Basel<br />
Thailand<br />
Sudsriluk Sampatchalit, Bangkok<br />
Turkey<br />
Olus Api, Istanbul<br />
Kubilay Aydin, İstanbul<br />
Işıl Bilgen, Izmir<br />
Zulkif Bozgeyik, Elazig<br />
Barbaros E Çil, Ankara<br />
Gulgun Engin, Istanbul<br />
M Fatih Evcimik, Malatya<br />
Ahmet Kaan Gündüz, Ankara<br />
Tayfun Hakan, Istanbul<br />
Adnan Kabaalioglu, Antalya<br />
Fehmi Kaçmaz, Ankara<br />
Musturay Karcaaltincaba, Ankara<br />
Osman Kizilkilic, Istanbul<br />
Zafer Koc, Adana<br />
Cem Onal, Adana<br />
Yahya Paksoy, Konya<br />
Bunyamin Sahin, Samsun<br />
Ercument Unlu, Edirne<br />
Ahmet Tuncay Turgut, Ankara<br />
Ender Uysal, Istanbul<br />
WJR|www.wjgnet.com<br />
United Kingdom<br />
K Faulkner, Wallsend<br />
Peter Gaines, Sheffield<br />
Balaji Ganeshan, Brighton<br />
Nagy Habib, London<br />
Alan Jackson, Manchester<br />
Pradesh Kumar, Portsmouth<br />
Tarik F Massoud, Cambridge<br />
Igor Meglinski, Bedfordshire<br />
Robert Morgan, London<br />
Ian Negus, Bristol<br />
Georgios A Plataniotis, Aberdeen<br />
N J Raine-Fenning, Nottingham<br />
Manuchehr Soleimani, Bath<br />
MY Tseng, Nottingham<br />
Edwin JR van Beek, Edinburgh<br />
Feng Wu, Oxford<br />
United States<br />
Athanassios Argiris, Pittsburgh<br />
Stephen R Baker, Newark<br />
Lia Bartella, New York<br />
Charles Bellows, New Orleans<br />
Walter L Biffl, Denver<br />
Homer S Black, Houston<br />
Wessam Bou-Assaly, Ann Arbor<br />
Owen Carmichael, Davis<br />
Shelton D Caruthers, St Louis<br />
Yuhchyau Chen, Rochester<br />
Melvin E Clouse, Boston<br />
Ezra Eddy Wyssam Cohen, Chicago<br />
Aaron Cohen-Gadol, Indianapolis<br />
Patrick M Colletti, Los Angeles<br />
Kassa Darge, Philadelphia<br />
Abhijit P Datir, Miami<br />
Delia C DeBuc, Miami<br />
Russell L Deter, Houston<br />
Adam P Dicker, Phil<br />
Khaled M Elsayes, Ann Arbor<br />
Steven Feigenberg, Baltimore<br />
Christopher G Filippi, Burlington<br />
Victor Frenkel, Bethesda<br />
Thomas J George Jr, Gainesville<br />
Patrick K Ha, Baltimore<br />
Robert I Haddad, Boston<br />
Walter A Hall, Syracuse<br />
Mary S Hammes, Chicago<br />
John Hart Jr, Dallas<br />
Randall T Higashida, San Francisco<br />
Juebin Huang, Jackson<br />
Andrei Iagaru, Stanford<br />
Craig Johnson, Milwaukee<br />
Ella F Jones, San Francisco<br />
Csaba Juhasz, Detroit<br />
Riyad Karmy-Jones, Vancouver<br />
Daniel J Kelley, Madison<br />
Amir Khan, Longview<br />
Euishin Edmund Kim, Houston<br />
Vikas Kundra, Houston<br />
Kennith F Layton, Dallas<br />
Rui Liao, Princeton<br />
CM Charlie Ma, Philadelphia<br />
Nina A Mayr, Columbus<br />
Thomas J Meade, Evanston<br />
Steven R Messé, Philadelphia<br />
Nathan Olivier Mewton, Baltimore<br />
Feroze B Mohamed, Philadelphia<br />
Koenraad J Mortele, Boston<br />
Mohan Natarajan, San Antonio<br />
John L Nosher, New Brunswick<br />
Chong-Xian Pan, Sacramento<br />
Dipanjan Pan, St Louis<br />
Martin R Prince, New York<br />
Reza Rahbar, Boston<br />
Carlos S Restrepo, San Antonio<br />
Veronica Rooks, Honolulu<br />
Maythem Saeed, San Francisco<br />
Edgar A Samaniego, Palo Alto<br />
Kohkan Shamsi, Doylestown<br />
Jason P Sheehan, Charlottesville<br />
William P Sheehan, Willmar<br />
Charles Jeffrey Smith, Columbia<br />
Monvadi B Srichai-Parsia, New York<br />
Dan Stoianovici, Baltimore<br />
Janio Szklaruk, Houston<br />
Dian Wang, Milwaukee<br />
Jian Z Wang, Columbus<br />
Liang Wang, New York<br />
Shougang Wang, Santa Clara<br />
Wenbao Wang, New York<br />
Aaron H Wolfson, Miami<br />
Gayle E Woloschak, Chicago<br />
Ying Xiao, Philadelphia<br />
Juan Xu, Pittsburgh<br />
Benjamin M Yeh, San Francisco<br />
Terry T Yoshizumi, Durham<br />
Jinxing Yu, Richmond<br />
Jianhui Zhong, Rochester<br />
III March 28, 2011
W J R<br />
Contents<br />
EDITORIAL<br />
REVIEW<br />
ORIGINAL ARTICLES<br />
CASE REPORT<br />
WJR|www.wjgnet.com<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Radiology<br />
55 A promising diagnostic method: Terahertz pulsed imaging and spectroscopy<br />
Sun Y, Sy MY, Wang YXJ, Ahuja AT, Zhang YT, Pickwell-MacPherson E<br />
66 Applications <strong>of</strong> new irradiation modalities in patients with lymphoma:<br />
Promises and uncertainties<br />
Kirova YM, Chargari C<br />
70 Estimation <strong>of</strong> intra-operator variability in perfusion parameter measurements<br />
using DCE-US<br />
Gauthier M, Leguerney I, Thalmensi J, Chebil M, Parisot S, Peronneau P, Roche A,<br />
Lassau N<br />
Monthly Volume 3 Number 3 March 28, 2011<br />
82 Paraparesis induced by extramedullary haematopoiesis<br />
Savini P, Lanzi A, Marano G, Moretti CC, Poletti G, Musardo G, Foschi FG, Stefanini GF<br />
March 28, 2011|Volume 3| ssue 3|
Contents<br />
ACKNOWLEDGMENTS<br />
APPENDIX<br />
ABOUT COVER<br />
AIM AND SCOPE<br />
FLYLEAF<br />
EDITORS FOR<br />
THIS ISSUE<br />
NAME OF JOURNAL<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Radiology<br />
LAUNCH DATE<br />
December 31, 2009<br />
SPONSOR<br />
Beijing Baishideng BioMed Scientific Co., Ltd.,<br />
Room 903, Building D, Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu, Chaoyang District,<br />
Beijing 100025, China<br />
Telephone: +86-10-8538-1892<br />
Fax: +86-10-8538-1893<br />
E-mail: baishideng@wjgnet.com<br />
http://www.wjgnet.com<br />
EDITING<br />
Editorial Board <strong>of</strong> <strong>World</strong> <strong>Journal</strong> <strong>of</strong> Radiology,<br />
Room 903, Building D, Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu, Chaoyang District,<br />
Beijing 100025, China<br />
Telephone: +86-10-8538-1892<br />
Fax: +86-10-8538-1893<br />
E-mail: wjr@wjgnet.com<br />
http://www.wjgnet.com<br />
PUBLISHING<br />
Baishideng Publishing Group Co., Limited,<br />
Room 1701, 17/F, Henan Building,<br />
No.90 Jaffe Road, Wanchai, Hong Kong, China<br />
Fax: +852-3115-8812<br />
Telephone: 00852-5804-2046<br />
WJR|www.wjgnet.com<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Radiology<br />
Volume 3 Number 3 March 28, 2011<br />
I Acknowledgments to reviewers <strong>of</strong> <strong>World</strong> <strong>Journal</strong> <strong>of</strong> Radiology<br />
I Meetings<br />
I-V Instructions to authors<br />
Sun Y, Sy MY, Wang YXJ, Ahuja AT, Zhang YT, Pickwell-MacPherson E. A<br />
promising diagnostic method: Terahertz pulsed imaging and spectroscopy.<br />
<strong>World</strong> J Radiol 2011; 3(3): 55-65<br />
http://www.wjgnet.com/1949-8470/full/v3/i3/55.htm<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Radiology (<strong>World</strong> J Radiol, WJR, online ISSN 1949-8470, DOI: 10.4329) is<br />
a monthly peer-reviewed, online, open-access, journal supported by an editorial board<br />
consisting <strong>of</strong> 319 experts in radiology from 40 countries.<br />
The major task <strong>of</strong> WJR is to rapidly report the most recent improvement in the<br />
research <strong>of</strong> medical imaging and radiation therapy by the radiologists. WJR accepts<br />
papers on the following aspects related to radiology: Abdominal radiology, women<br />
health radiology, cardiovascular radiology, chest radiology, genitourinary radiology,<br />
neuroradiology, head and neck radiology, interventional radiology, musculoskeletal<br />
radiology, molecular imaging, pediatric radiology, experimental radiology, radiological<br />
technology, nuclear medicine, PACS and radiology informatics, and ultrasound. We also<br />
encourage papers that cover all other areas <strong>of</strong> radiology as well as basic research.<br />
I-III Editorial Board<br />
Responsible Assistant Editor: Na Liu Responsible Science Editor: Jian-Xia Cheng<br />
Responsible Electronic Editor: Wen-Hua Ma<br />
Pro<strong>of</strong>ing Editor-in-Chief: Lian-Sheng Ma<br />
E-mail: baishideng@wjgnet.com<br />
http://www.wjgnet.com<br />
SUBSCRIPTION<br />
Beijing Baishideng BioMed Scientific Co., Ltd.,<br />
Room 903, Building D, Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu, Chaoyang District,<br />
Beijing 100025, China<br />
Telephone: +86-10-8538-1892<br />
Fax: +86-10-8538-1893<br />
E-mail: baishideng@wjgnet.com<br />
http://www.wjgnet.com<br />
PUBLICATION DATE<br />
March 28, 2011<br />
SERIAL PUBLICATION NUMBER<br />
ISSN 1949-8470 (online)<br />
PRESIDENT AND EDITOR-IN-CHIEF<br />
Lian-Sheng Ma, Beijing<br />
STRATEGY ASSOCIATE EDITORS-IN-CHIEF<br />
Ritesh Agarwal, Chandigarh<br />
Kenneth Coenegrachts, Bruges<br />
Adnan Kabaalioglu, Antalya<br />
Meng Law, Lost Angeles<br />
Ewald Moser, Vienna<br />
Aytekin Oto, Chicago<br />
AAK Abdel Razek, Mansoura<br />
Àlex Rovira, Barcelona<br />
Yi-Xiang Wang, Hong Kong<br />
Hui-Xiong Xu, Guangzhou<br />
EDITORIAL OFFICE<br />
Na Ma, Director<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Radiology<br />
Room 903, Building D, Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu, Chaoyang District,<br />
Beijing 100025, China<br />
Telephone: +86-10-8538-1892<br />
Fax: +86-10-8538-1893<br />
E-mail: wjr@wjgnet.com<br />
http://www.wjgnet.com<br />
COPYRIGHT<br />
© 2011 Baishideng. Articles published by this Open-<br />
Access journal are distributed under the terms <strong>of</strong><br />
the Creative Commons Attribution Non-commercial<br />
License, which permits use, distribution, and reproduction<br />
in any medium, provided the original work<br />
is properly cited, the use is non commercial and is<br />
otherwise in compliance with the license.<br />
SPECIAL STATEMENT<br />
All articles published in this journal represent the<br />
viewpoints <strong>of</strong> the authors except where indicated<br />
otherwise.<br />
INSTRUCTIONS TO AUTHORS<br />
Full instructions are available online at http://www.<br />
wjgnet.com/1949-8470/g_info_20100316162358.htm.<br />
ONLINE SUBMISSION<br />
http://www.wjgnet.com/1949-8470<strong>of</strong>fice<br />
March 28, 2011|Volume 3| ssue 3|
W J R<br />
Online Submissions: http://www.wjgnet.com/1949-8470<strong>of</strong>fice<br />
wjr@wjgnet.com<br />
doi:10.4329/wjr.v3.i3.55<br />
A promising diagnostic method: Terahertz pulsed imaging<br />
and spectroscopy<br />
Yiwen Sun, Ming Yiu Sy, Yi-Xiang J Wang, Anil T Ahuja, Yuan-Ting Zhang, Emma Pickwell-MacPherson<br />
Yiwen Sun, Ming Yiu Sy, Yuan-ting Zhang, Department <strong>of</strong><br />
Electronic Engineering, The Chinese University <strong>of</strong> Hong Kong,<br />
Hong Kong, China<br />
Yi-Xiang J Wang, Anil T Ahuja, Department <strong>of</strong> Imaging and<br />
Interventional Radiology, The Chinese University <strong>of</strong> Hong Kong,<br />
Hong Kong, China<br />
Yuan-ting Zhang, The Institute <strong>of</strong> Biomedical and Health Engineering,<br />
Shenzhen Instituted <strong>of</strong> Advanced Technology, Chinese<br />
Academy <strong>of</strong> Sciences, Shenzhen 518000, Guangdong Province,<br />
China<br />
Yuan-Tng Zhang, Key Laboratory for Biomedical Informatics<br />
and Health Engineering, Chinese Academy <strong>of</strong> Sciences, Shenzhen<br />
518000, Guangdong Province, China<br />
Emma Pickwell-MacPherson, Department <strong>of</strong> Electronic and<br />
Computer Engineering, Hong Kong University <strong>of</strong> Science and<br />
Technology, Hong Kong, China<br />
Author contributions: Wang YXJ gave the idea <strong>of</strong> the paper was<br />
given; Sun Y, Sy MY and Pickwell-MacPherson E collected the<br />
data presented; all authors were involved in writing and editing<br />
the paper.<br />
Supported by in part for this work from the Research Grants<br />
Council <strong>of</strong> the Hong Kong Government and the Shun Hing Institute<br />
<strong>of</strong> Advanced Engineering, Hong Kong<br />
Correspondence to: Dr. Emma Pickwell-MacPherson, Department<br />
<strong>of</strong> Electronic and Computer Engineering, Hong Kong<br />
University <strong>of</strong> Science and Technology, Hong Kong,<br />
China. eeemma@ust.hk<br />
Telephone: +852-23585034 Fax: +852-23581485<br />
Received: November 18, 2010 Revised: January 19, 2010<br />
Accepted: January 26, 2010<br />
Published online: March 28, 2011<br />
Abstract<br />
The terahertz band lies between the microwave and infrared<br />
regions <strong>of</strong> the electromagnetic spectrum. This radiation<br />
has very low photon energy and thus it does not<br />
pose any ionization hazard for biological tissues. It is<br />
strongly attenuated by water and very sensitive to water<br />
content. Unique absorption spectra due to intermolecular<br />
vibrations in this region have been found in different<br />
biological materials. These unique features make tera-<br />
WJR|www.wjgnet.com<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Radiology<br />
hertz imaging very attractive for medical applications in<br />
order to provide complimentary information to existing<br />
imaging techniques. There has been an increasing interest<br />
in terahertz imaging and spectroscopy <strong>of</strong> biologically<br />
related applications within the last few years and more<br />
and more terahertz spectra are being reported. This<br />
paper introduces terahertz technology and provides a<br />
short review <strong>of</strong> recent advances in terahertz imaging<br />
and spectroscopy techniques, and a number <strong>of</strong> applications<br />
such as molecular spectroscopy, tissue characterization<br />
and skin imaging are discussed.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Biomedical; Imaging; Spectroscopy; Terahertz<br />
Peer reviewer: Yicheng Ni, MD, PhD, Pr<strong>of</strong>essor, Biomedical<br />
Imaging, Interventional Therapy and Contrast Media Research,<br />
Department <strong>of</strong> Radiology, University Hospitals, K.U. Leuven,<br />
Herestraat 49, B-3000, Leuven, Belgium<br />
Sun Y, Sy MY, Wang YXJ, Ahuja AT, Zhang YT, Pickwell-<br />
MacPherson E. A promising diagnostic method: Terahertz pulsed<br />
imaging and spectroscopy. <strong>World</strong> J Radiol 2011; 3(3): 55-65<br />
Available from: URL: http://www.wjgnet.com/1949-8470/full/<br />
v3/i3/55.htm DOI: http://dx.doi.org/10.4329/wjr.v3.i3.55<br />
INTRODUCTION<br />
<strong>World</strong> J Radiol 2011 March 28; 3(3): 55-65<br />
ISSN 1949-8470 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
EDITORIAL<br />
Terahertz (THz, 1 THz = 10 12 Hz) radiation, also known<br />
as THz waves, THz light, or T-rays, is situated in the frequency<br />
regime between optical and electronic techniques.<br />
This regime is typically defined as 0.1-10 THz and has<br />
become a new area for research in physics, chemistry, biology,<br />
materials science and medicine. Experiments with<br />
THz radiation date back to measurements <strong>of</strong> black body<br />
radiation using a bolometer in the 1890s [1,2] . However,<br />
for a long time, this region remained unexplored due to a<br />
lack <strong>of</strong> good sources and detectors, and it was commonly<br />
55 March 28, 2011|Volume 3|Issue 3|
Sun Y et al . Terahertz pulsed imaging and spectroscopy<br />
referred to as the “THz gap”. In 1975, David Auston at<br />
AT&T Bell Laboratories developed a photoconductive<br />
emitter gated with an optical pulse that led towards bridging<br />
this gap - the ‘Auston switch’ emitted broadband THz<br />
radiation up to 1 mW. A coherent method to detect THz<br />
pulses in the time domain was also proposed [3] . This became<br />
the foundation <strong>of</strong> THz time-domain spectroscopy<br />
(THz-TDS) [4] , since then many improvements in the generation<br />
and detection <strong>of</strong> coherent THz radiation enabled<br />
THz-TDS and imaging techniques to be pioneered for<br />
applications in various fields such as biomedical engineering,<br />
physics, astronomy, security screening, communications,<br />
genetic engineering, pharmaceutical quality control<br />
and medical imaging [5] . In this paper, THz technology is<br />
introduced and some emerging applications in biology<br />
and medicine including molecular spectroscopy, tissue<br />
characterization and skin imaging are presented.<br />
The aim <strong>of</strong> this article is to review the potential <strong>of</strong><br />
THz pulsed imaging and spectroscopy as a promising<br />
diagnostic method. Several unique features make THz<br />
very suitable for medical applications. (1) THz radiation<br />
has very low photon energy, which is insufficient to cause<br />
chemical damage to molecules, or knock particles out<br />
<strong>of</strong> atoms. Thus, it will not cause harmful ionization in<br />
biological tissues; this makes it very attractive for medical<br />
applications; (2) THz radiation is very sensitive to polar<br />
substances, such as water and hydration state. For this<br />
reason, THz waves can provide a better contrast for s<strong>of</strong>t<br />
tissues than X-rays; (3) THz-TDS techniques use coherent<br />
detection to record the THz wave’s temporal electric<br />
fields, which means both the amplitude and phase <strong>of</strong> the<br />
THz wave can be obtained simultaneously. The temporal<br />
waveforms can be further Fourier transformed to give the<br />
spectra. This allows precise measurements <strong>of</strong> the refractive<br />
index and absorption coefficient <strong>of</strong> samples without<br />
resorting to the Kramers-Kronig relations; and (4) The<br />
energy <strong>of</strong> rotational and vibrational transitions <strong>of</strong> molecules<br />
lies in the THz region and intermolecular vibrations<br />
such as hydrogen bonds exhibit different spectral characteristics<br />
in the THz range. These unique spectral features<br />
can be used to distinguish between different materials or<br />
even isomers.<br />
PRINCIPLES OF THZ PULSED IMAGING<br />
AND SPECTROSCOPY<br />
THz systems<br />
Over the past two decades, technology for generating and<br />
detecting THz radiation has advanced considerably. Several<br />
commercialized systems are now available [6-10] and THz<br />
systems have been set up by many groups all over the<br />
world. According to the laser source used, THz systems<br />
can be divided into two general classes: continuous wave<br />
(CW) and pulsed.<br />
A typical CW system can produce a single fixed frequency<br />
or several discrete frequency outputs. Some <strong>of</strong><br />
them can be tunable. Generation <strong>of</strong> CW THz radiation<br />
can be achieved by approaches such as photomixing [11] ,<br />
WJR|www.wjgnet.com<br />
Laser diode1<br />
Laser diode2<br />
BS<br />
Emitter<br />
cw THz<br />
Sample<br />
Detector<br />
Delay<br />
Figure 1 Schematic illustration <strong>of</strong> a continuous wave THz imaging system<br />
in transmission geometry.<br />
Vitesse<br />
femtosecond<br />
pulsed laser<br />
Delay stage<br />
Probe<br />
beam<br />
Sample<br />
Quartz imaging plate<br />
Photoconductive<br />
emitter<br />
free-electron lasers [12] and quantum cascade lasers [13] .<br />
Figure 1 illustrates a CW THz system which photomixes<br />
two CW lasers in a photoconductor as an example [14] . The<br />
mixing <strong>of</strong> two above-bandgap (visible or near-infrared)<br />
wavelengths produces beating, which can modulate the<br />
conductance <strong>of</strong> a photoconductive switch at the THz<br />
difference frequency. The photomixing device is labeled<br />
“emitter” in Figure 1. Since the source spectrum <strong>of</strong> the<br />
CW system is narrow and sometimes only the intensity<br />
information is <strong>of</strong> interest, the data structures and postprocessing<br />
are relatively simple. It is possible now to<br />
drive a whole CW system by laser diodes and thus it can<br />
be made compact and inexpensive. However, due to the<br />
limited information that CW systems provide, they are<br />
sometimes confined to those applications where only features<br />
at some specific frequencies are <strong>of</strong> interest.<br />
In pulsed systems, broadband emission up to several<br />
THz can be achieved. Currently, there are a number <strong>of</strong><br />
ways to generate and detect pulsed THz radiation, such<br />
as ultrafast switching <strong>of</strong> photoconductive antennas [3] , rectification<br />
<strong>of</strong> optical pulses in crystals [15] , rapid screening<br />
<strong>of</strong> the surface field via photoexcitation <strong>of</strong> dense electron<br />
hole plasma in semiconductors [16] and carrier tunneling in<br />
coupled double quantum well structures [17] . Among them,<br />
the most established approaches based on photoconductive<br />
antennas, where an expensive femtosecond laser is<br />
required and configured as shown in Figure 2. Unlike CW<br />
THz imaging system, coherent detection in pulsed THz<br />
imaging techniques can record THz waves in the time do-<br />
56 March 28, 2011|Volume 3|Issue 3|<br />
30°<br />
Photoconductive<br />
detector<br />
Pump beam<br />
Figure 2 Schematic illustration <strong>of</strong> a pulsed THz imaging system with reflection<br />
geometry.
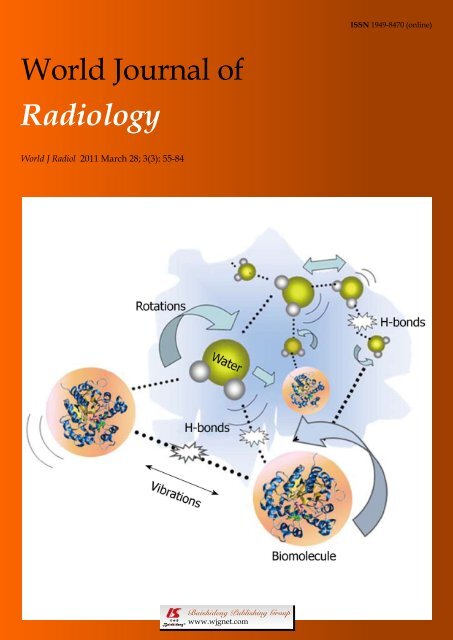
Rotations<br />
Vibrations<br />
Water<br />
H-bonds<br />
main, including both the intensity and phase information,<br />
which can be further used to obtain more details <strong>of</strong> the<br />
target such as spectral and depth information [18] . This key<br />
advantage lends coherent THz imaging to a wider range<br />
<strong>of</strong> applications.<br />
Molecular interactions in the THz regime<br />
There has been an increased interest in understanding the<br />
interactions between molecules and THz radiation. Many<br />
<strong>of</strong> the intricate interactions on a molecular level rely on<br />
changes in biomolecular conformation <strong>of</strong> the basic units<br />
<strong>of</strong> proteins such as α helices and β sheets. In recent years,<br />
dynamic signatures <strong>of</strong> the THz frequency vibrations in<br />
RNA and DNA strands have been characterized [19,20] .<br />
Furthermore, studies <strong>of</strong> water molecule interactions with<br />
proteins have attracted significant research interest [21] . In<br />
a protein-water network, the protein’s structure and dynamics<br />
are affected by the surrounding water which is<br />
called biological water, or hydration water. As illustrated<br />
in Figure 3, hydrogen bonds, which are weak attractive<br />
forces, form between the hydrated water molecules and<br />
the side chains <strong>of</strong> protein. These affect the dynamic relaxation<br />
properties <strong>of</strong> protein and enable distinction between<br />
the hydration water layer and bulk water. The remarkable<br />
effects <strong>of</strong> the hydrogen bonds associated with the intermolecular<br />
information are able to be detected using THz<br />
spectroscopy. THz spectra contain information about intermolecular<br />
modes as well as intra-molecular bonds and<br />
thus usually carry more structural information than vibrations<br />
in the mid-infrared spectral region which tend to be<br />
dominated by intra-molecular vibrations.<br />
Unique advantages and challenges for biomedical<br />
applications<br />
The energy level <strong>of</strong> 1 THz is only about 4.14 meV (which<br />
is much less than the energy <strong>of</strong> X-rays 0.12 to 120 keV),<br />
it therefore does not pose an ionization hazard as in X-ray<br />
WJR|www.wjgnet.com<br />
Biomolecule<br />
H-bonds<br />
Figure 3 Schematic representation <strong>of</strong> H-bond interactions between water<br />
and biomolecules.<br />
Sun Y et al . Terahertz pulsed imaging and spectroscopy<br />
radiation. Research into safe levels <strong>of</strong> exposure has also<br />
been carried out through studies on keratinocytes [22] and<br />
blood leukocytes [23,24] , neither <strong>of</strong> which has revealed any<br />
detectable alterations. This non-ionizing nature is a crucial<br />
property that lends THz techniques to medical applications.<br />
The fundamental period <strong>of</strong> THz-frequency electromagnetic<br />
radiation is around 1ps, and so it is uniquely<br />
suited to investigate biological systems with mechanisms<br />
at picosecond timescales. The energy levels <strong>of</strong> THz light<br />
are very low, therefore damage to cells or tissue should<br />
be limited to generalized thermal effects, i.e. strong resonant<br />
absorption seems unlikely. From a spectroscopy<br />
standpoint, biologically important collective modes <strong>of</strong><br />
proteins vibrate at THz frequencies, in addition, frustrated<br />
rotations and collective modes cause polar liquids (such<br />
as water) to absorb at THz frequencies. Many organic<br />
substances have characteristic absorption spectra in this<br />
frequency range [25,26] enabling research into THz spectroscopy<br />
for biomedical applications.<br />
THz wavelengths have a diffraction limited spot size<br />
consistent with the resolution <strong>of</strong> a 1990’s vintage laser<br />
printer (1.22λ0 = 170 μm at 2.160 THz or 150 dots/in).<br />
At 1 THz, the resolution could be as good as a decent<br />
computer monitor (70 dots/in). Submillimeter-wavelength<br />
means that THz signals pass through tissue with only Mie<br />
or Tyndall scattering (proportional to f 2 ) rather than much<br />
stronger Rayleigh scattering (proportional to f 4 ) that dominates<br />
in the IR and optical since cell size is less than the<br />
wavelength.<br />
Since most tissues are immersed in, dominated by, or<br />
preserved in polar liquids, the exceptionally high absorption<br />
losses at THz frequencies make penetration through<br />
biological materials <strong>of</strong> any substantial thickness infeasible.<br />
However, the same high absorption coefficient that limits<br />
penetration in tissue also promotes extreme contrast between<br />
substances with lesser or higher degrees <strong>of</strong> water<br />
content which can help to show distinctive contrast in<br />
medical imaging.<br />
IMAGING VS SPECTROSCOPY<br />
THz pulsed imaging<br />
Early applications <strong>of</strong> THz technology were confined<br />
mostly to space science [27] and molecular spectroscopy [28,29] ,<br />
but interest in biomedical applications has been increasing<br />
since the first introduction <strong>of</strong> THz pulsed imaging (TPI)<br />
in 1995 by Hu and Nuss [30] . Their THz images <strong>of</strong> porcine<br />
tissue demonstrated a contrast between muscle and fats.<br />
This initial study promoted later research on the application<br />
<strong>of</strong> THz imaging to other biological samples. THz pulsed<br />
imaging actually can be viewed as an extension <strong>of</strong> the THz-<br />
TDS method. In addition to providing valuable spectral<br />
information, 2D images can be obtained with THz-TDS by<br />
spatial scanning <strong>of</strong> either the THz beam or the object itself.<br />
In this way, geometrical images <strong>of</strong> the sample can be produced<br />
to reveal its inner structures [31] . Thus, it is possible to<br />
obtain three-dimensional views <strong>of</strong> a layered structure.<br />
57 March 28, 2011|Volume 3|Issue 3|
A<br />
B<br />
Sun Y et al . Terahertz pulsed imaging and spectroscopy<br />
Intensity (a.u., × 10 4 )<br />
Spectral amplitude (a.u.)<br />
2.5<br />
2.0<br />
1.5<br />
1.0<br />
0.5<br />
0.0<br />
-0.5<br />
-1.0<br />
10 6<br />
10 5<br />
10 4<br />
10 3<br />
10 2<br />
10 1<br />
0.0<br />
-0.2<br />
-0.4<br />
15 25<br />
5 10 15 20 25 30<br />
Optical delay (ps)<br />
0 1 2 3 4 5<br />
Frequency (THz)<br />
Figure 4 Typical terahertz pulse and corresponding spectrum. A: Temporal<br />
waveform <strong>of</strong> a sample (drawn by raw data with the inset representing its corresponding<br />
processed data after deconvolution with a reference measurement);<br />
B: The corresponding spectrum <strong>of</strong> the raw data with the noise floor (indicated<br />
by dashed line).<br />
When a THz pulse is incident on such a target, a train<br />
<strong>of</strong> pulses will be reflected back from the various interfaces.<br />
For each individual pulse in the detected signal, the<br />
amplitude and timing are different and can be measured<br />
precisely. The principle <strong>of</strong> time <strong>of</strong> flight technique is to<br />
estimate the depth information <strong>of</strong> the internal dielectric<br />
pr<strong>of</strong>iles <strong>of</strong> the target through the time that is required to<br />
travel over a certain distance. This permits looking into<br />
the inside <strong>of</strong> optically opaque material and it has been<br />
used for THz 3D imaging. Among the earliest demonstrations<br />
<strong>of</strong> THz 3D imaging, Mittleman et al [31] imaged<br />
a conventional floppy disk. In their work the various<br />
parts inside the disk were identified and the discontinuous<br />
refractive index pr<strong>of</strong>ile was derived. This method was<br />
further extended into THz reflection computed tomography<br />
[32,33] , where the target was rotated to provide back<br />
reflection from different angles. In a similar way to X-ray<br />
CT imaging, the filtered back projection algorithm was<br />
applied to reconstruct the edge map <strong>of</strong> the target’s crosssection.<br />
With advances in interactive publishing, Wallace<br />
et al [34] highlighted the ability <strong>of</strong> 3-D THz imaging in a<br />
number <strong>of</strong> niche applications. For example they were<br />
able to resolve two layers <strong>of</strong> drugs beneath the protective<br />
coating <strong>of</strong> a pharmaceutical tablet.<br />
THz spectroscopy<br />
THz spectroscopy is typically done with a single point<br />
WJR|www.wjgnet.com<br />
measurement (with transmission geometry in most cases)<br />
<strong>of</strong> a homogenous sample and the resulting THz electric<br />
field can be recorded as a function <strong>of</strong> time. Thus, it can<br />
be Fourier transformed to <strong>of</strong>fer meaningful spectroscopic<br />
information due to the broadband nature <strong>of</strong> pulsed THz<br />
radiation, shown in Figure 4. Although the spectral resolution<br />
is not as good as that with narrowband techniques,<br />
coherent detection <strong>of</strong> THz-TDS can provide both high<br />
sensitivity and time-resolved phase information [35] . This<br />
spectroscopic technique is primarily used to probe material<br />
properties and it is helpful to see where it lies in the<br />
electromagnetic spectrum in relation to atomic and molecular<br />
transitions.<br />
THz spectroscopy is complementary to THz imaging<br />
and is primarily used to determine optical properties in<br />
the frequency domain. Since THz pulses are created and<br />
detected using short pulsed visible lasers with pulse widths<br />
varying from approximately 200 fs down to approximately<br />
10 fs, it is now possible to make time resolved far-infrared<br />
studies with sub-picosecond temporal resolution [36] . This<br />
was not achievable with conventional far-infrared studies.<br />
An important aspect <strong>of</strong> THz time-domain spectroscopy<br />
is that both the phase and amplitude <strong>of</strong> the spectral components<br />
<strong>of</strong> the pulse are determined. The amplitude and<br />
phase are directly related to the absorption coefficient and<br />
refractive index <strong>of</strong> a sample and thus the complex permittivity<br />
is obtained without requiring Kramers-Kronig analysis.<br />
Furthermore, another advantage <strong>of</strong> THz spectroscopy<br />
is that it is able to non-destructively detect differences<br />
because it uses radiation <strong>of</strong> sufficiently long wavelength<br />
and low energy that does not induce any phase changes or<br />
photochemical reactions to living organisms.<br />
BIOLOGICAL APPLICATIONS<br />
Pharmaceuticals<br />
There has been a strong drive in the pharmaceutical industry<br />
for comprehensive quality assurance monitoring.<br />
This motivates development <strong>of</strong> new tools providing useful<br />
analysis <strong>of</strong> tablet formulations. The ability <strong>of</strong> THz<br />
technology to determine both spectral and structural<br />
information has fuelled interest in the pharmaceutical<br />
applications <strong>of</strong> this technique [37] . For example THz spectroscopy<br />
has been employed for polymorph identification<br />
and quantification [38] , phase transition monitoring [39] , and<br />
distinguishing between behaviors <strong>of</strong> hydrated forms [40] .<br />
THz radiation can penetrate through plastic packaging<br />
materials. To illustrate this we give an example using<br />
Maalox PlusTM - an over the counter medicine for stomach<br />
upsets. Each tablet has “Rorer” engraved on one side<br />
and “Maalox Plus” on the other side. Figure 5A contains<br />
a photo <strong>of</strong> a tablet in its packaging as well as a THz image<br />
taken after removing it from the packaging - the engraved<br />
lettering is clearly seen in the THz image. Figure 5C is a<br />
THz image <strong>of</strong> the tablet taken through the packaging - we<br />
can still see the lettering on the surface <strong>of</strong> the tablet. The<br />
cross-section <strong>of</strong> the tablet is better conveyed by an image<br />
<strong>of</strong> the depth pr<strong>of</strong>ile. THz pulses are reflected first <strong>of</strong>f the<br />
58 March 28, 2011|Volume 3|Issue 3|
A<br />
C D<br />
Figure 5 Terahertz imaging <strong>of</strong> the tablet. A: Photograph <strong>of</strong> the tablet in the plastic package and THz C-Scan section imaging without the packaging; B: THz B-Scan<br />
image shows the structure <strong>of</strong> the cross-section <strong>of</strong> the tablet and the THz light paths at the edge <strong>of</strong> the tablet (path a) and the centre (path b); C: THz C-Scan image<br />
shows the tablet face inside the plastic package; D: THz deconvolved waveforms in the time-domain reflected from the paths a and b in Figure 5B.<br />
front surface <strong>of</strong> the package and then from any subsurface<br />
structure within it resulting in multiple pulses returning to<br />
the detector. The dashed arrows in Figure 5B mark out<br />
the THz light paths at the edge <strong>of</strong> the tablet (path A) and<br />
the center (path B). In path A the beveled edge means that<br />
there is an air gap between the packaging and the tablet<br />
and this corresponds to a greater optical delay between the<br />
reflected peaks in the waveforms illustrated in Figure 5D.<br />
Thus, THz imaging has non-destructively revealed the<br />
structure <strong>of</strong> the tablet through the packaging.<br />
Protein spectroscopy<br />
Towards the higher frequency end <strong>of</strong> the THz range (from<br />
about 1 THz and above) there are vibrational modes corresponding<br />
to protein tertiary structural motion; such<br />
intermolecular interactions are present in many biomolecules.<br />
Other molecular properties that can be probed in<br />
the THz range include bulk dielectric relaxation modes [41]<br />
and phonon modes [42] these can be difficult to probe using<br />
other techniques. For instance nuclear magnetic resonance<br />
(NMR) spectroscopy can determine the presence<br />
<strong>of</strong> various carbon bonds, but it cannot be used to distinguish<br />
between molecules with the same molecular formula,<br />
but with different structural forms (isomers) [10] . THz<br />
spectroscopy is able to distinguish between isomers and<br />
polymorphs [43] and is therefore emerging as an important<br />
and highly sensitive tool to determine biomolecular structure<br />
and dynamics [44,45] . Indeed THz spectroscopy can<br />
WJR|www.wjgnet.com<br />
Amplitude (a.u.)<br />
B<br />
0.07<br />
0.06<br />
0.05<br />
0.04<br />
0.03<br />
0.02<br />
0.01<br />
0.00<br />
-0.01<br />
-0.02<br />
-0.03<br />
Sun Y et al . Terahertz pulsed imaging and spectroscopy<br />
Surface <strong>of</strong> tablet Gap between tablet<br />
and package<br />
a b<br />
Dt = 2.14 ps<br />
Dt = 4.86 ps<br />
Surface <strong>of</strong> plastic<br />
package<br />
Path a<br />
Path b<br />
8 10 12 14 16 18 20 22 24 26 28<br />
Time (ps)<br />
distinguish between two types <strong>of</strong> artificial RNA strands<br />
when measured in dehydrated form [46] . Furthermore,<br />
Fischer et al [47] demonstrated that even when the molecular<br />
structure differs only in the orientation <strong>of</strong> a single hydroxyl<br />
group with respect to the ring plane, a pronounced<br />
difference in the THz spectra is observed. Intermolecular<br />
interactions are present in all biomolecules, and since biomolecules<br />
are the fundamental components <strong>of</strong> biological<br />
samples, they can be used to provide a natural source <strong>of</strong><br />
image contrast in biomedical THz imaging [48] .<br />
Biomolecules, especially proteins, which play an essential<br />
structural and catalytic role in cells and tissues, <strong>of</strong>ten<br />
require an aqueous phase in order to be transported to their<br />
target sites. In the protein-water system, the characteristic<br />
water structure induced near the surfaces <strong>of</strong> proteins arises<br />
not only through hydrogen bonding <strong>of</strong> the water molecules<br />
to available proton donor and proton acceptor sites, but<br />
also through electrostatic forces associated with the water<br />
molecule that arise from its large electric dipole moment.<br />
If an electric field is applied to such a system <strong>of</strong> proteinassociated<br />
water, there will be a torque exerted on each water<br />
dipole moment inducing them to attempt to align along<br />
the direction <strong>of</strong> the field vector. The dielectric spectrum<br />
has been widely used to describe the interaction between<br />
protein and its solvent molecule in THz frequency [49] . A<br />
dielectric orientational relaxation time τ can then be defined<br />
as the time required for 1/e <strong>of</strong> the field-oriented water<br />
molecules to become randomly reoriented on removing<br />
59 March 28, 2011|Volume 3|Issue 3|
A<br />
ε'<br />
B<br />
ε''<br />
Sun Y et al . Terahertz pulsed imaging and spectroscopy<br />
7.0<br />
6.5<br />
6.0<br />
5.5<br />
5.0<br />
4.5<br />
4.0<br />
3.5<br />
0.2 0.4 0.6 0.8 1.0 1.2<br />
Frequency (THz)<br />
3.0<br />
2.5<br />
2.0<br />
1.5<br />
0.76 THz<br />
the applied field. Measurements may be analyzed in terms<br />
<strong>of</strong> the complex dielectric constant ε(ω) (where ω denotes<br />
angular frequency) or the complex refractive index n(ω).<br />
The degree <strong>of</strong> orientational polarization and the rate <strong>of</strong><br />
reorientational relaxation depend on how the water dipoles<br />
are influenced by local electrostatic forces and the extent<br />
to which the breaking and/or reforming <strong>of</strong> local hydrogen<br />
bonds is required to accommodate the changes in orientation.<br />
Relaxations <strong>of</strong> polar side-groups, vibrations <strong>of</strong> the<br />
polypeptide backbone, and fluctuating proton transfer<br />
between ionized side-groups <strong>of</strong> the protein also contribute<br />
to the overall polarizability <strong>of</strong> the protein-water system.<br />
If dielectric measurements are made on protein solutions,<br />
then orientational relaxations <strong>of</strong> the protein molecule itself<br />
will also be observed [50] . Figure 6 shows that the vibration<br />
mode <strong>of</strong> two types <strong>of</strong> labeled antibodies (peroxidase conjugated<br />
IgG and the fluorescein conjugated IgG) can be<br />
distinguished at 0.76 and 1.18 THz using the THz dielectric<br />
spectrum. By investigating the concentration dependence<br />
<strong>of</strong> the spectra it is also possible to obtain an estimate <strong>of</strong> the<br />
hydration shell thickness around the protein molecules [51] .<br />
MEDICAL APPLICATIONS<br />
Tissue characterization<br />
There is also interest in tissue contrast for in vivo and ex vivo<br />
WJR|www.wjgnet.com<br />
Gly/water (1:1)<br />
PX-IgG (0.8 mg/mL)<br />
FITC-IgG (0.8 mg/mL)<br />
PX-IgG (0.8 mg/mL)<br />
Gly/water (1:1)<br />
FITC-IgG (0.8 mg/mL)<br />
1.18 THz<br />
1.0<br />
0.2 0.4 0.6 0.8 1.0 1.2<br />
Frequency (THz)<br />
Figure 6 Dielectric constant spectra (A) and dielectric loss spectra (B) <strong>of</strong><br />
water/ glycerol mix (black line with circles), peroxidase conjugated IgG<br />
(red line with triangles) and the fluorescein conjugated IgG (green line<br />
with crosses) dissolved in the water/glycerol solution at the concentration<br />
<strong>of</strong> 0.8 mg/mL in the frequency range <strong>of</strong> 0.1-1.3 THz. PX: Peroxidase conjugated;<br />
FITC: Fluorescein conjugated.<br />
identification <strong>of</strong> abnormalities, hydration, and subdermal<br />
probing. Only a small number <strong>of</strong> measurements<br />
have been made to date, and systematic investigations to<br />
catalogue absorption coefficients, refractive indices and<br />
contrast mechanisms are just beginning to accumulate.<br />
Measurements on the absorption and refractive index <strong>of</strong><br />
biological materials in the THz region go back at least to<br />
1976 [52] . Several research groups have investigated excised<br />
and fixed tissue samples, either alcohol perfused [8] , formalin<br />
fixed [53-57] , or freeze dried and wax mounted [58] looking<br />
for inherent contrast to define unique modalities. One <strong>of</strong><br />
the first applications on human ex vivo wet tissue involved<br />
imaging <strong>of</strong> excised basal cell carcinoma [59,60] . In vivo work<br />
has focused on the skin [61] and accessible external surfaces<br />
<strong>of</strong> the body for measuring hydration [62] and tumor infiltration<br />
[60] . A catalogue <strong>of</strong> unfixed tissue properties (including<br />
blood constituents) was compiled by the University <strong>of</strong><br />
Leeds, UK [54] for frequencies between 500-1500 GHz using<br />
a pulsed time-domain system. Difficulties in extrapolating<br />
measurements on excised tissue to in vivo results<br />
are numerous and include for example uptake <strong>of</strong> saline<br />
from the sample storage environment, changes in hydration<br />
level during measurement, temperature-dependent<br />
loss, measurement chamber interactions, and scattering<br />
effects. In our previous work [63] , we performed reflection<br />
geometry spectroscopy to investigate the properties<br />
<strong>of</strong> several types <strong>of</strong> healthy organ tissues, including liver,<br />
kidney, heart muscle, leg muscle, pancreas and abdominal<br />
fat tissues using THz pulsed imaging. The frequency dependent<br />
refractive index and the absorption coefficient <strong>of</strong><br />
the tissues are shown in Figure 7. All the results are the<br />
mean values <strong>of</strong> the ten samples and error bars represent<br />
the 95% confidence intervals. We found clear differences<br />
between the tissue properties, particularly the absorption<br />
coefficient. Since fatty tissue largely consists <strong>of</strong> hydrocarbon<br />
chains and relatively few polar molecules, the absorption<br />
coefficient and refractive index <strong>of</strong> the fatty tissue are<br />
much lower that those <strong>of</strong> the kidney and liver tissues.<br />
We have also investigated the optical properties <strong>of</strong><br />
fresh and formalin fixed samples in the THz frequency<br />
range using THz reflection spectroscopy [64] . As seen in<br />
Figure 8A, when the fixing time increased the waveform<br />
amplitude <strong>of</strong> the adipose tissue also increased. This was<br />
primarily because the refractive index <strong>of</strong> the adipose tissue<br />
was decreasing over the majority <strong>of</strong> the bandwidth<br />
(due to the fixing) and this meant there was a greater<br />
difference between the refractive index <strong>of</strong> the quartz (n<br />
approximately 2.1) and that <strong>of</strong> the adipose tissue (e.g. 1.5<br />
at 1 THz when fixed compared to 1.6 when it was fresh).<br />
From Fresnel theory, this increased difference in refractive<br />
indices resulted in a greater reflected amplitude. As the<br />
fixing time increased for the muscle, three main changes<br />
were apparent. A small peak started to appear preceding<br />
the trough and the width and magnitude <strong>of</strong> the trough<br />
decreased (Figure 8B). These changes can also be explained<br />
by considering the effects <strong>of</strong> the formalin on the<br />
refractive index and absorption coefficient <strong>of</strong> the muscle.<br />
For the muscle, the formalin significantly reduced both<br />
60 March 28, 2011|Volume 3|Issue 3|
A<br />
Absorption coefficient (cm -1 )<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
0.25 0.50 0.75 1.00 1.25 1.50<br />
Frequency (THz)<br />
the refractive index and the absorption coefficient. Before<br />
fixing, the refractive index <strong>of</strong> the fresh muscle was greater<br />
than that <strong>of</strong> quartz over the whole <strong>of</strong> the frequency range<br />
measured (Figure 8C). The fixing reduced the refractive<br />
index so much that the refractive index became lower than<br />
that <strong>of</strong> quartz at higher frequencies (Figure 8D) and this<br />
was the cause for the small peak which appeared (arrow in<br />
Figure 8B) and increased as the fixing time was increased.<br />
Skin cancer, breast tumors and dental caries<br />
Due to the low penetration depth <strong>of</strong> THz in biological<br />
tissues, THz biomedical applications investigated to date<br />
WJR|www.wjgnet.com<br />
Fat<br />
Liver<br />
Kidney<br />
B<br />
Refractive index<br />
2.8<br />
2.6<br />
2.4<br />
2.2<br />
2.0<br />
1.8<br />
1.6<br />
0.25 0.50 0.75 1.00 1.25 1.50<br />
Frequency (THz)<br />
Fat<br />
Liver<br />
Kidney<br />
Figure 7 Tissue characterization using THz spectroscopy. A: Mean absorption coefficients <strong>of</strong> kidney, liver and abdominal fat; B: Mean refractive indices <strong>of</strong> all the<br />
tissue samples. Error bars represent 95% confidence intervals.<br />
A<br />
C<br />
Amplitude (a.u.)<br />
Refractive index<br />
0.08<br />
0.07<br />
0.06<br />
0.05<br />
0.04<br />
0.03<br />
0.02<br />
0.01<br />
0.00<br />
Fresh fat<br />
Fixed fat (24 h)<br />
Fixed fat (48 h)<br />
Fixed fat (72 h)<br />
-0.01<br />
16.0 16.5 17.0 17.5 18.0<br />
Optical delay (ps)<br />
3.3<br />
3.0<br />
2.7<br />
2.4<br />
2.1<br />
1.8<br />
1.5<br />
1.2<br />
Bulk water<br />
Fresh muscle<br />
Fresh fat<br />
0.1 0.3 0.5 0.7 0.9 1.1<br />
Frequency (THz)<br />
B<br />
D<br />
Amplitude (a.u.)<br />
Refractive index<br />
0.03<br />
0.02<br />
0.01<br />
0.00<br />
-0.01<br />
-0.02<br />
-0.03<br />
-0.04<br />
-0.05<br />
Fresh muscle<br />
Fixed muscle (24 h)<br />
Fixed muscle (48 h)<br />
Fixed muscle (72 h)<br />
-0.06<br />
15.5 16.0 16.5 17.0 17.5 18.0 18.5 19.0 19.5<br />
Optical delay (ps)<br />
3.3<br />
3.0<br />
2.7<br />
2.4<br />
2.1<br />
1.8<br />
1.5<br />
Sun Y et al . Terahertz pulsed imaging and spectroscopy<br />
Fixed muscle<br />
Fixed fat<br />
Quartz<br />
0.1 0.3 0.5 0.7 0.9 1.1<br />
Frequency (THz)<br />
Figure 8 The deconvolved mean waveforms for adipose tissue (A) and skeletal muscle (B) as the fixing time progressed and the mean refractive index for<br />
fresh (C) and fixed samples (D) <strong>of</strong> adipose tissue and skeletal muscle. The dot-dash line indicates the refractive index <strong>of</strong> the quartz window on which the sample<br />
was measured. Error bars represent 95% CI. The water data were acquired in transmission and the error bars are too small to be seen on this graph.<br />
have been limited to easily accessible parts <strong>of</strong> the body,<br />
such as skin and teeth, or those that would benefit from<br />
intra-operative imaging such as breast cancer. Figure 9 is a<br />
photograph <strong>of</strong> the reflection geometry THz probe from<br />
TeraView Ltd. which we use in Hong Kong.<br />
One potential application <strong>of</strong> THz imaging is the diagnosis<br />
<strong>of</strong> skin cancer. Work by Woodward et al [60] has demonstrated<br />
the potential to use THz imaging to determine<br />
regions <strong>of</strong> skin cancer non-invasively using a reflection<br />
geometry imaging system. The first ex vivo measurements<br />
on skin cancer revealing the ability <strong>of</strong> TPI to differentiate<br />
basal cell carcinoma (BCC) from normal skin were pro-<br />
61 March 28, 2011|Volume 3|Issue 3|
Sun Y et al . Terahertz pulsed imaging and spectroscopy<br />
Figure 9 Photograph <strong>of</strong> the THz hand-held probe.<br />
Incident<br />
THz pulse<br />
Gum<br />
Enamel<br />
Dentin<br />
Pulp<br />
duced by Woodward et al [59] .<br />
Breast-conserving surgery is also an area <strong>of</strong> medicine<br />
which may benefit from THz imaging. Fitzgerald et al [65]<br />
conducted ex vivo studies <strong>of</strong> breast cancer to investigate the<br />
potential <strong>of</strong> THz imaging to aid the removal <strong>of</strong> breast cancer<br />
intra-operatively. In particular, they studied the feasibility<br />
<strong>of</strong> THz pulsed imaging to map the tumor margins on<br />
freshly excised human breast tissue. Good correlation was<br />
found for the area and shape <strong>of</strong> tumor in the THz images<br />
compared with that <strong>of</strong> histology. They also performed a<br />
spectroscopy study comparing the THz optical properties<br />
(absorption coefficient and refractive index) <strong>of</strong> the excised<br />
normal breast tissue and breast tumor. Both the absorption<br />
coefficient and refractive index were higher for tissue that<br />
contained tumor and this is a very positive indication that<br />
THz imaging could be used to detect margins <strong>of</strong> tumor<br />
and provide complementary information to techniques<br />
such as infrared and optical imaging, thermography, electrical<br />
impedance, and magnetic resonance imaging [66,67] .<br />
Since in vivo THz imaging is currently limited to sur-<br />
WJR|www.wjgnet.com<br />
1<br />
Detected pulse<br />
Figure 10 Schematic representation <strong>of</strong> the THz reflections from enamel.<br />
Reflection 1 is the reflection from the surface <strong>of</strong> the enamel and reflection 2 is<br />
the reflection from within the enamel due to tooth decay causing mineral loss.<br />
2<br />
1<br />
2<br />
Intensity (v)<br />
0.025<br />
0.015<br />
0.005<br />
-0.005<br />
-0.015<br />
-0.025<br />
-0.035<br />
14 16 18 20 22 24<br />
Optical delay (ps)<br />
From palm and plaster<br />
From palm only<br />
Figure 11 Measured pulses from the palm. The blue line is the measurement<br />
<strong>of</strong> the palm through a tegaderm plaster and the red dotted line is the measurement<br />
<strong>of</strong> the palm alone. In both cases, two troughs are seen - they are the<br />
reflections from the top and bottom surfaces <strong>of</strong> the stratum corneum.<br />
face features, another potential application <strong>of</strong> THz imaging<br />
is the diagnosis <strong>of</strong> dental caries [68,69] . Figure 10 is a<br />
schematic diagram <strong>of</strong> a THz reflection from the outer<br />
layer <strong>of</strong> enamel. Caries are a result <strong>of</strong> mineral loss from<br />
enamel, and this causes a change in refractive index within<br />
the enamel. The change in refractive index means that<br />
small lesions, smaller than those detected by the naked<br />
eye, can be detected [70] . However, in practice THz imaging<br />
systems are large and cumbersome - even structures<br />
as obvious as teeth can make a challenging target. In this<br />
respect THz imaging is still some way <strong>of</strong>f <strong>of</strong>fering a nonionizing<br />
alternative to X-rays in dentistry.<br />
Burn depth diagnosis<br />
Since THz waves can penetrate several hundreds <strong>of</strong> microns<br />
into the skin and most burn injuries are superficial,<br />
this opens up the possibility <strong>of</strong> employing THz techniques<br />
for burn assessment [71] . The waveforms and optical<br />
parameters <strong>of</strong> the burn wounds were investigated and<br />
THz images have shown contrast between burn-damaged<br />
tissue and healthy tissue. Their results indicate that THz<br />
imaging may be promising in evaluating skin burn severity,<br />
especially for characterizing burn areas. Moreover, the<br />
time <strong>of</strong> flight technique is able to reveal the depth pr<strong>of</strong>ile<br />
thus could be used to evaluate burn depth.<br />
The potential <strong>of</strong> THz imaging as a burn diagnostic<br />
has been demonstrated using chicken breast [6] . It is also<br />
conceivable that THz imaging could be <strong>of</strong> use in monitoring<br />
treatment <strong>of</strong> skin conditions (like psoriasis), since<br />
THz imaging is cheaper than MRI and does not require a<br />
coupling gel like ultrasound [72] .<br />
THz light can penetrate many materials: we have investigated<br />
whether it can resolve skin layers beneath a<br />
Tegaderm ® plaster as this would also be <strong>of</strong> benefit in<br />
monitoring burn wounds. Normal skin comprises three<br />
different layers: the stratum corneum, epidermis, and<br />
dermis. The stratum corneum on the palm <strong>of</strong> the hand<br />
is 100-200 μm thick and thus has been resolved in previous<br />
in vivo skin studies. We placed the plaster on the palm<br />
<strong>of</strong> the hand and the resulting THz reflected waveform<br />
62 March 28, 2011|Volume 3|Issue 3|
A<br />
B<br />
Optical delay (ps)<br />
14<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
2 4 6 8 10 12<br />
Position number<br />
Figure 12 In vivo measurement <strong>of</strong> the variation in stratum corneum<br />
thickness <strong>of</strong> the palm. A: Photograph <strong>of</strong> the palm, indicating where the THz<br />
measurements were taken; B: A b-scan image showing the variation in stratum<br />
corneum thickness with palm position. The white dashed line indicates the<br />
interface between the quartz window and the stratum corneum; and the black<br />
dashed line indicates the interface between the stratum corneum and the epidermis.<br />
The grey bar represents the ratio <strong>of</strong> the electric field at a given optical<br />
delay, t, over the maximum electric field [E(t)/Emax].<br />
is shown in Figure 11. For comparison the measurement<br />
<strong>of</strong> the palm alone is also plotted. In the figure, there are 2<br />
troughs, which correspond to the top and bottom surface<br />
<strong>of</strong> the stratum corneum. The optical delay between them<br />
can be used to calculate the thickness <strong>of</strong> this layer. These<br />
results show that THz light is able to penetrate through<br />
wound dressings with only slight attenuation to reveal<br />
the skin depth information. This therefore indicates that<br />
THz imaging is likely to be able to detect and measure<br />
changes to the stratum corneum and epidermis which<br />
could for example, be caused by burns. To illustrate how<br />
sensitive THz imaging is to the stratum corneum, we have<br />
also imaged the side <strong>of</strong> a healthy hand. As the position<br />
<strong>of</strong> the measurement changes, as indicated by the arrow in<br />
Figure 12A, the optical delay between the reflections from<br />
the top and bottom <strong>of</strong> the stratum corneum increases. This<br />
is because the stratum corneum is thicker at the tip <strong>of</strong> the<br />
arrow than at the arrow foot. By plotting the reflected amplitude<br />
intensity against position we obtain the depth pr<strong>of</strong>ile<br />
image <strong>of</strong> the palm in Figure 12B. By using frequency<br />
and wavelet domain deconvolution we are able to resolve<br />
thinner layers <strong>of</strong> skin than if basic deconvolution is used [73] .<br />
WJR|www.wjgnet.com<br />
1.0<br />
0.5<br />
0.0<br />
-0.5<br />
-1.0<br />
Sun Y et al . Terahertz pulsed imaging and spectroscopy<br />
COMPARISON WITH OTHER<br />
TECHNOLOGIES<br />
Numerous groups have investigated direct transmission<br />
or reflection THz imaging as a means <strong>of</strong> distinguishing<br />
tissue types [30,55,74] and recognizing diseases including<br />
tumors penetrating below the surface layers <strong>of</strong> skin or<br />
into organs [56,58,75] . Although progress is being made, the<br />
competition from other more developed imaging modalities<br />
is fierce. Optical coherence tomography, ultrasound,<br />
near-IR, and Raman spectroscopy, MRI, positron emission<br />
tomography, in situ confocal microscopy, and X-ray<br />
techniques have all received much more attention and<br />
currently <strong>of</strong>fer enhanced resolution, greater penetration,<br />
higher acquisition speeds, and specifically targeted contrast<br />
mechanisms. This does not preclude THz imaging<br />
from finding a niche in this barrage <strong>of</strong> already favorable<br />
modalities. There is still no technique that can readily distinguish<br />
benign from malignant lesions macroscopically<br />
at the surface or subdermally. The sensitivity <strong>of</strong> THz signals<br />
to skin moisture, which is <strong>of</strong>ten a key indictor, is very<br />
high, and competing techniques such as high-resolution<br />
MRI are less convenient and more costly.<br />
The resolution <strong>of</strong> ordinary THz imaging is diffraction<br />
limited, however, its high sensitivity to water content and<br />
great surface imaging capability provide motivation for further<br />
development and sub-wavelength resolution has been<br />
achieved in near-field studies [76] . Indeed shallow subsurface<br />
images can be very revealing and the first few hundred<br />
micrometers are hard to image with other modalities. The<br />
high sensitivity <strong>of</strong> THz radiation to fluid composition and<br />
the variable conductivity in tissue [77] is likely to lead to statistically<br />
significant differences between nominally identical<br />
samples taken at different locations in the body at different<br />
times or from different subjects. This may ultimately prove<br />
advantageous; however, in the short term, it will tend to<br />
mask sought for differences that are indicative <strong>of</strong> diseases.<br />
CONCLUSION<br />
THz imaging is still in its early stage <strong>of</strong> development, but<br />
as this paper has shown, has great potential to be a valuable<br />
imaging technique in the future. In the past decade,<br />
THz imaging applications in biomedical fields have drawn<br />
extensive interest and advancements in imaging methods<br />
and theoretical analysis continue to enable further applications<br />
to be investigated.<br />
REFERENCES<br />
1 Nichols EF. A method for energy measurements in the<br />
infra-red spectrum and the properties <strong>of</strong> the ordinary ray<br />
in quartz for waves <strong>of</strong> great wave length. Phys Rev (Series I)<br />
1897; 4: 297-313<br />
2 Rubens H, Nichols EF. Heat rays <strong>of</strong> great wave length. Phys<br />
Rev (Series I) 1897; 4: 314-323<br />
3 Auston DH. Picosecond optoelectronic switching and gating<br />
in silicon. Appl Phys Lett 1975; 26: 101-103<br />
4 Grischkowsky D, Keiding S, van Exter M, Fattinger C. Far-<br />
63 March 28, 2011|Volume 3|Issue 3|
Sun Y et al . Terahertz pulsed imaging and spectroscopy<br />
infrared time-domain spectroscopy with terahertz beams<br />
<strong>of</strong> dielectrics and semiconductors. J Opt Soc Am B 1990; 7:<br />
2006-2015<br />
5 Wallace VP, Arnone DA, Woodward RM, Pye RJ. Biomedical<br />
applications <strong>of</strong> terahertz pulse imaging. Houston, TX:<br />
Engineering in Medicine and Biology, 2002. 24th Annual<br />
Conference and the Annual Fall Meeting <strong>of</strong> the Biomedical<br />
Engineering Society. Proceedings <strong>of</strong> the Second Joint<br />
EMBS/BMES Conference, 2002: 2333-2334<br />
6 Mittleman DM, Gupta M, Neelamani R, Baraniuk RG,<br />
Rudd JV, Koch M. Recent advances in terahertz imaging.<br />
Applied Physics B 1999; 68: 1085-1094<br />
7 Zhang XC. Terahertz wave imaging: horizons and hurdles.<br />
Phys Med Biol 2002; 47: 3667-3677<br />
8 Siegel PH. Terahertz technology in biology and medicine.<br />
IEEE T Micro Theory 2004; 52: 2438-2447<br />
9 Wallace VP, Taday PF, Fitzgerald AJ, Woodward RM, Cluff<br />
J, Pye RJ, Arnone DD. Terahertz pulsed imaging and spectroscopy<br />
for biomedical and pharmaceutical applications.<br />
Faraday Discuss 2004; 126: 255-263; discussion 303-311<br />
10 Withayachumnankul W, Png GM, Yin X, Atakaramians S,<br />
Jones I, Lin H, Ung SY, Balakrishnan J, Ng BWH, Ferguson B,<br />
Mickan SP, Fischer BM, Abbott D. T-ray sensing and imaging.<br />
Proc IEEE 2007; 95: 1528-1558<br />
11 Brown ER, McIntosh KA, Nichols KB, Dennis CL. Photomixing<br />
up to 3.8 THz in low-temperature-grown GaAs. Appl<br />
Phys Lett 1995; 66: 285-287<br />
12 Jeong YU, Lee BC, Kim SK, Cho SO, Cha BH, Lee J, Kazakevitch<br />
GM, Vobly PD, Gavrilov NG, Kubarev VV, Kulipanov<br />
GN. First lasing <strong>of</strong> the KAERI compact far-infrared<br />
free-electron laser driven by a magnetron-based microtron.<br />
Nucl Instr Meth 2001; 475: 47-50<br />
13 Smet JH, Fonstad CG, Hu Q. Intrawell and interwell intersubband<br />
transitions in multiple quantum wells for farinfrared<br />
sources. J Appl Phys 1996; 79: 9305-9320<br />
14 Baker C, Gregory IS, Tribe WR, Evans MJ, Missous M, Linfield<br />
EH. Continuous-Wave Terahertz Photomixing in Low-<br />
Temperature InGaAs. Conference Digest <strong>of</strong> the 2004 Joint<br />
29th International Conference on Infrared and Millimeter<br />
Waves, 2004 and 12th International Conference on Terahertz<br />
Electronics, 2004: 367-368<br />
15 Zhang XC, Ma XF, Jin Y, Lu TM, Boden EP, Phelps PD,<br />
Stewart KR, Yakymyshyn CP. Terahertz optical rectification<br />
from a nonlinear organic crystal. Appl Phys Lett 1992; 61:<br />
3080-3082<br />
16 Huber R, Tauser F, Brodschelm A, Bichler M, Abstreiter G,<br />
Leitenstorfer A. How many-particle interactions develop<br />
after ultrafast excitation <strong>of</strong> an electron-hole plasma. Nature<br />
2001; 414: 286-289<br />
17 Roskos HG, Nuss MC, Shah J, Leo K, Miller DA, Fox AM,<br />
Schmitt-Rink S, Köhler K. Coherent submillimeter-wave<br />
emission from charge oscillations in a double-well potential.<br />
Phys Rev Lett 1992; 68: 2216-2219<br />
18 McClatchey K, Reiten MT, Cheville RA. Time resolved synthetic<br />
aperture terahertz impulse imaging. Appl Phys Lett<br />
2001; 79: 4485-4487<br />
19 Woolard DL, Globus TR, Gelmont BL, Bykhovskaia M,<br />
Samuels AC, Cookmeyer D, Hesler JL, Crowe TW, Jensen JO,<br />
Jensen JL, Loerop WR. Submillimeter-wave phonon modes in<br />
DNA macromolecules. Phys Rev E 2002; 65: 051903<br />
20 Globus T, Bykhovskaia M, Woolard D, Gelmont B. Sub-millimetre<br />
wave absorption spectra <strong>of</strong> artificial RNA molecules.<br />
J Phys D 2003; 36: 1314<br />
21 Pal SK, Peon J, Zewail AH. Biological water at the protein<br />
surface: Dynamical solvation probed directly with femtosecond<br />
resolution. Proc Natl Acad Sci USA 2002; 99: 1763-1768<br />
22 Bourne N, Clothier RH, D'Arienzo M, Harrison P. The effects<br />
<strong>of</strong> terahertz radiation on human keratinocyte primary<br />
cultures and neural cell cultures. Altern Lab Anim 2008; 36:<br />
667-684<br />
WJR|www.wjgnet.com<br />
23 Berry E, Walker GC, Fitzgerald AJ, Zinov’ev NN, Chamberlain<br />
M, Smye SW, Miles RE, Smith MA. Do in vivo terahertz<br />
imaging systems comply with safety guidelines? J Laser Appl<br />
2003; 15: 192-198<br />
24 Zeni O, Gallerano GP, Perrotta A, Romanò M, Sannino A,<br />
Sarti M, D'Arienzo M, Doria A, Giovenale E, Lai A, Messina<br />
G, Scarfì MR. Cytogenetic observations in human peripheral<br />
blood leukocytes following in vitro exposure to THz radiation:<br />
a pilot study. Health Phys 2007; 92: 349-357<br />
25 Kawase K, Ogawa Y, Watanabe Y, Inoue H. Non-destructive<br />
terahertz imaging <strong>of</strong> illicit drugs using spectral fingerprints.<br />
Opt Express 2003; 11: 2549-2554<br />
26 Ning L, Shen J, Jinhai S, Laishun L, Xu X, Lu M, Yan J. Study<br />
on the THz spectrum <strong>of</strong> methamphetamine. Opt Express 2005;<br />
13: 6750-6755<br />
27 Walker CK, Kulesa CA. Terahertz Astronomy From The<br />
Coldest Place on Earth. The Joint 30th International Conference,<br />
2005: 3-4<br />
28 Møller U, Cooke DG, Tanaka K, Jepsen PU. Terahertz reflection<br />
spectroscopy <strong>of</strong> Debye relaxation in polar liquids. J Opt<br />
Soc Am B 2009; 26: A113-A125<br />
29 Davies A, Linfield E. Molecular and organic interactions. In:<br />
Miles RE, Zhang XC, Eisele H, Krotkus A, editors. Terahertz<br />
frequency detection and identification <strong>of</strong> materials and objects.<br />
The Netherlands: Springer, 2007: 91-106<br />
30 Hu BB, Nuss MC. Imaging with terahertz waves. Opt Lett<br />
1995; 20: 1716<br />
31 Mittleman DM, Hunsche S, Boivin L, Nuss MC. T-ray tomography.<br />
Opt Lett 1997; 22: 904-906<br />
32 Pearce J, Choi H, Mittleman DM, White J, Zimdars D. T-ray<br />
reflection computed tomography. Opt Lett 2005; 30: 1653-1655<br />
33 Pearce J, Choi H, Mittleman DM, White J, Zimdars D. Terahertz<br />
wide aperture reflection tomography. Opt Lett 2005; 30:<br />
1653-1655<br />
34 Wallace VP, Macpherson E, Zeitler JA, Reid C. Three-dimensional<br />
imaging <strong>of</strong> optically opaque materials using nonionizing<br />
terahertz radiation. J Opt Soc Am A Opt Image Sci Vis 2008;<br />
25: 3120-3133<br />
35 Ferguson B, Zhang XC. Materials for terahertz science and<br />
technology. Nat Mater 2002; 1: 26-33<br />
36 Beard MC, Turner GM, Schmuttenmaer CA. Subpicosecond<br />
carrier dynamics in low-temperature grown. GaAs as measured<br />
by time-resolved terahertz spectroscopy. J Appl Phys<br />
2001; 90: 5915-5923<br />
37 Ho L, Müller R, Römer M, Gordon KC, Heinämäki J,<br />
Kleinebudde P, Pepper M, Rades T, Shen YC, Strachan CJ,<br />
Taday PF, Zeitler JA. Analysis <strong>of</strong> sustained-release tablet film<br />
coats using terahertz pulsed imaging. J Control Release 2007;<br />
119: 253-261<br />
38 Strachan CJ, Rades T, Newnham DA, Gordon KC, Pepper<br />
M, Taday PF. Using terahertz pulsed spectroscopy to study<br />
crystallinity <strong>of</strong> pharmaceutical materials. Chem Phys Lett 2004;<br />
390: 20-24<br />
39 Zeitler JA, Newnham DA, Taday PF, Strachan CJ, Pepper<br />
M, Gordon KC, Rades T. Temperature dependent Terahertz<br />
Pulsed Spectroscopy <strong>of</strong> carbamazepine. Thermochimica Acta<br />
2005; 436: 71-77<br />
40 Zeitler JA, Kogermann K, Rantanen J, Rades T, Taday PF,<br />
Pepper M, Aaltonen J, Strachan CJ. Drug hydrate systems<br />
and dehydration processes studied by terahertz pulsed spectroscopy.<br />
Int J Pharm 2007; 334: 78-84<br />
41 Kindt JT, Schmuttenmaer CA. Far-infrared dielectric properties<br />
<strong>of</strong> polar liquids probed by femtosecond terahertz pulse<br />
spectroscopy. J Phys chem 1996; 100: 10373-10379<br />
42 Tielrooij KJ, Timmer RL, Bakker HJ, Bonn M. Structure dynamics<br />
<strong>of</strong> the proton in liquid water probed with terahertz<br />
time-domain spectroscopy. Phys Rev Lett 2009; 102: 198303<br />
43 Strachan CJ, Taday PF, Newnham DA, Gordon KC, Zeitler<br />
JA, Pepper M, Rades T. Using terahertz pulsed spectroscopy<br />
to quantify pharmaceutical polymorphism and crystallinity. J<br />
64 March 28, 2011|Volume 3|Issue 3|
Pharm Sci 2005; 94: 837-846<br />
44 Mittleman DM, Nuss MC, Colvin VL. Terahertz spectroscopy<br />
<strong>of</strong> water in inverse micelles. Chem Phys Lett 1997; 275: 332-338<br />
45 Walther M, Fischer B, Schall M, Helm H, Jepsen PU. Far-infrared<br />
vibrational spectra <strong>of</strong> all-trans, 9-cis and 13-cis retinal<br />
measured by THz time-domain spectroscopy. Chem Phys Lett<br />
2000; 332: 389-395<br />
46 Fischer B, H<strong>of</strong>fmann M, Helm H, Wilk R, Rutz F, Kleine-<br />
Ostmann T, Koch M, Jepsen P. Terahertz time-domain spectroscopy<br />
and imaging <strong>of</strong> artificial RNA. Opt Express 2005; 13:<br />
5205-5215<br />
47 Fischer BM, Helm H, Jepsen PU. Chemical recognition with<br />
broadband THz spectroscopy. Proc IEEE 2007; 95: 1592-1604<br />
48 Woodward RM, Wallace VP, Arnone DD, Linfield EH, Pepper<br />
M. Terahertz pulsed imaging <strong>of</strong> skin cancer in the time<br />
and frequency domain. J Bio Phys 2003; 29: 257-259<br />
49 Grant EH, Sheppard RJ, South GP. Dielectric behaviour <strong>of</strong><br />
biological molecules in solution. Oxford: Clarendon Press,<br />
1978<br />
50 Pethig R. Protein-water interactions determined by dielectric<br />
methods. Annu Rev Phys Chem 1992; 43: 177-205<br />
51 Sun Y, Zhang Y, Pickwell-Macpherson E. Investigating antibody<br />
interactions with a polar liquid using terahertz pulsed<br />
spectroscopy. Biophys J 2011; 100: 225-231<br />
52 Hartwick TS, Hodges DT, Barker DH, Foote FB. Far infrared<br />
imagery. Appl Opt 1976; 15: 1919-1922<br />
53 Siebert KJ, Löffler T, Quast H, Thomson M, Bauer T, Leonhardt<br />
R, Czasch S, Roskos HG. All-optoelectronic continuous<br />
wave THz imaging for biomedical applications. Phys Med Biol<br />
2002; 47: 3743-3748<br />
54 Fitzgerald AJ, Berry E, Zinov'ev NN, Homer-Vanniasinkam S,<br />
Miles RE, Chamberlain JM, Smith MA. Catalogue <strong>of</strong> human<br />
tissue optical properties at terahertz frequencies. J Biol Phys<br />
2003; 29: 123-128<br />
55 Löffler T, Siebert K, Czasch S, Bauer T, Roskos HG. Visualization<br />
and classification in biomedical terahertz pulsed imaging.<br />
Phys Med Biol 2002; 47: 3847<br />
56 Löffler T, Bauer T, Siebert K, Roskos H, Fitzgerald A, Czasch<br />
S. Terahertz dark-field imaging <strong>of</strong> biomedical tissue. Opt Express<br />
2001; 9: 616-621<br />
57 Kan WC, Lee WS, Cheung WH, Wallace VP, Pickwell-<br />
Macpherson E. Terahertz pulsed imaging <strong>of</strong> knee cartilage.<br />
Biomed Opt Express 2010; 1: 967-974<br />
58 Knobloch P, Schmalstieg K, Koch M, Rehberg E, Vauti F,<br />
Donhuijsen K. THz imaging <strong>of</strong> histo-pathological samples.<br />
Proc SPIE 2001; 4434: 239-245<br />
59 Woodward RM, Wallace VP, Pye RJ, Cole BE, Arnone DD,<br />
Linfield EH, Pepper M. Terahertz pulse imaging <strong>of</strong> ex vivo<br />
basal cell carcinoma. J Invest Dermatol 2003; 120: 72-78<br />
60 Woodward RM, Cole BE, Wallace VP, Pye RJ, Arnone DD,<br />
Linfield EH, Pepper M. Terahertz pulse imaging in reflection<br />
geometry <strong>of</strong> human skin cancer and skin tissue. Phys Med Biol<br />
2002; 47: 3853-3863<br />
61 Pickwell E, Cole BE, Fitzgerald AJ, Pepper M, Wallace VP. In<br />
vivo study <strong>of</strong> human skin using pulsed terahertz radiation.<br />
Phys Med Biol 2004; 49: 1595-1607<br />
62 Cole BE, Woodward RM, Crawley D, Wallace VP, Arnone<br />
DD, Pepper M. Terahertz imaging and spectroscopy <strong>of</strong> hu-<br />
WJR|www.wjgnet.com<br />
Sun Y et al . Terahertz pulsed imaging and spectroscopy<br />
man skin, in vivo. Proc SPIE 2001; 4276: 1-10<br />
63 Huang SY, Wang YX, Yeung DK, Ahuja AT, Zhang YT, Pickwell-Macpherson<br />
E. Tissue characterization using terahertz<br />
pulsed imaging in reflection geometry. Phys Med Biol 2009;<br />
54: 149-160<br />
64 Sun Y, Fischer BM, Pickwell-MacPherson E. Effects <strong>of</strong> formalin<br />
fixing on the terahertz properties <strong>of</strong> biological tissues. J<br />
Biomed Opt 2009; 14: 064017<br />
65 Fitzgerald AJ, Wallace VP, Jimenez-Linan M, Bobrow L, Pye<br />
RJ, Purushotham AD, Arnone DD. Terahertz pulsed imaging<br />
<strong>of</strong> human breast tumors. Radiology 2006; 239: 533-540<br />
66 Bolan PJ, Meisamy S, Baker EH, Lin J, Emory T, Nelson M,<br />
Everson LI, Yee D, Garwood M. In vivo quantification <strong>of</strong><br />
choline compounds in the breast with 1H MR spectroscopy.<br />
Magn Reson Med 2003; 50: 1134-1143<br />
67 Boppart SA, Luo W, Marks DL, Singletary KW. Optical coherence<br />
tomography: feasibility for basic research and imageguided<br />
surgery <strong>of</strong> breast cancer. Breast Cancer Res Treat 2004;<br />
84: 85-97<br />
68 Knobloch P, Schildknecht C, Kleine-Ostmann T, Koch M,<br />
H<strong>of</strong>fmann S, H<strong>of</strong>mann M, Rehberg E, Sperling M, Donhuijsen<br />
K, Hein G, Pierz K. Medical THz imaging: an investigation<br />
<strong>of</strong> histo-pathological samples. Phys Med Biol 2002; 47:<br />
3875-3884<br />
69 Pickwell E, Wallace VP, Cole BE, Ali S, Longbottom C, Lynch<br />
RJ, Pepper M. Using terahertz pulsed imaging to measure<br />
enamel demineralisation in teeth. Shanghai: Joint 31st International<br />
Conference on Infrared Millimeter Waves and 14th<br />
International Conference on Teraherz Electronics, 2006: 578<br />
70 MacPherson EP. Biological applications <strong>of</strong> terahertz pulsed<br />
imaging and spectroscopy. Cambridge: Cambridge University<br />
Press, 2005<br />
71 Huang SY, Macpherson E, Zhang YT. A feasibility study <strong>of</strong><br />
burn wound depth assessment using terahertz pulsed imaging.<br />
Cambridge: 4th IEEE/EMBS International Summer<br />
School and Symposium on Medical Devices and Biosensors,<br />
2007: 132-135<br />
72 Fitzgerald AJ, Berry E, Zinovev NN, Walker GC, Smith MA,<br />
Chamberlain JM. An introduction to medical imaging with<br />
coherent terahertz frequency radiation. Phys Med Biol 2002;<br />
47: R67-R84<br />
73 Chen Y, Huang S, Pickwell-MacPherson E. Frequency-Wavelet<br />
Domain Deconvolution for terahertz reflection imaging<br />
and spectroscopy. Opt Express 2010; 18: 1177-1190<br />
74 Ferguson B, Wang S, Gray D, Abbott D, Zhang XC. Towards<br />
functional 3D T-ray imaging. Phys Med Biol 2002; 47:<br />
3735-3742<br />
75 Woodward RM, Wallace VP, Cole BE, Pye RJ, Arnone DD,<br />
Linfield EH, Pepper M. Terahertz pulse imaging in reflection<br />
geometry <strong>of</strong> skin tissue using time-domain analysis<br />
techniques. In: Cohn GE, Editor. Clinical Diagnostic Systems:<br />
Technologies and Instrumentation. San Jose, CA: SPIE, 2002:<br />
160-169<br />
76 Chen HT, Kersting R, Cho GC. Terahertz imaging with nanometer<br />
resolution. Appl Phys Lett 2003; 83: 3009-3011<br />
77 Ülgen Y, Sezdi M. Electrical parameters <strong>of</strong> human blood.<br />
Hong Kong: Proceedings <strong>of</strong> the IEEE/EMBS 20th Annual International<br />
Conference, 1998: 2983-2986<br />
S- Editor Cheng JX L- Editor Webster JR E- Editor Zheng XM<br />
65 March 28, 2011|Volume 3|Issue 3|
W J R<br />
Online Submissions: http://www.wjgnet.com/1949-8470<strong>of</strong>fice<br />
wjr@wjgnet.com<br />
doi:10.4329/wjr.v3.i3.66<br />
Applications <strong>of</strong> new irradiation modalities in patients with<br />
lymphoma: Promises and uncertainties<br />
Youlia M Kirova, Cyrus Chargari<br />
Youlia M Kirova, Cyrus Chargari, Department <strong>of</strong> Radiation<br />
Oncology, Institut Curie 26, rue d’Ulm, 75248 Paris, Cedex 05,<br />
France<br />
Author contributions: Kirova YM designed the study; Kirova<br />
YM and Chargari C wrote the paper.<br />
Correspondence to: Youlia M Kirova, MD, Department <strong>of</strong><br />
Radiation Oncology, Institut Curie 26, rue d’Ulm, 75248 Paris,<br />
Cedex 05, France. youlia.kirova@curie.net<br />
Telephone: +33-1-44324193 Fax: +33-1-53102653<br />
Received: January 15, 2011 Revised: March 2, 2011<br />
Accepted: March 9, 2011<br />
Published online: March 28, 2011<br />
Abstract<br />
New highly conformal irradiation modalities have emerged<br />
for treatment <strong>of</strong> Hodgkin lymphoma. Helical Tomotherapy<br />
<strong>of</strong>fers both intensity-modulated irradiation and accurate<br />
patient positioning and was shown to significantly decrease<br />
radiation doses to the critical organs. Here we review<br />
some <strong>of</strong> the most promising applications <strong>of</strong> helical<br />
tomotherapy in Hodgkin disease. By decreasing doses to<br />
the heart or the breast, helical tomotherapy might decrease<br />
the risk <strong>of</strong> long-term cardiac toxicity or secondary<br />
breast cancers, which are major concerns in patients<br />
receiving chest radiotherapy. Other strategies, such as<br />
debulking radiotherapy prior to stem cell transplantation<br />
or total lymphoid irradiation may be clinically relevant.<br />
However, helical tomotherapy may also increase the volume<br />
<strong>of</strong> tissues that receive lower doses, which has been<br />
implicated in the carcinogenesis process. Prospective<br />
assessments <strong>of</strong> these new irradiation modalities <strong>of</strong> helical<br />
tomotherapy are required to confirm the potential<br />
benefits <strong>of</strong> highly conformal therapies applied to hematological<br />
malignancies.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Hodgkin lymphoma; Helical tomotherapy;<br />
Cardiac toxicity; Secondary cancers<br />
Peer reviewer: Ying Xiao, PhD, Pr<strong>of</strong>essor, Director, Medical<br />
WJR|www.wjgnet.com<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Radiology<br />
Physics, Department <strong>of</strong> Radiation Oncology, Thomas Jefferson<br />
University Hospital, Philadelphia, PA 19107-5097, United States<br />
Kirova YM, Chargari C. Applications <strong>of</strong> new irradiation modalities<br />
in patients with lymphoma: Promises and uncertainties.<br />
<strong>World</strong> J Radiol 2011; 3(3): 66-69 Available from: URL: http://<br />
www.wjgnet.com/1949-8470/full/v3/i3/66.htm DOI: http://<br />
dx.doi.org/10.4329/wjr.v3.i3.66<br />
INTRODUCTION<br />
Radiation therapy still plays a major role in the management<br />
<strong>of</strong> hematological malignancies. Its place and modalities<br />
for treatment <strong>of</strong> lymphoma have evolved over recent<br />
decades. First, randomized studies supported reduction<br />
<strong>of</strong> field size and dose radiation in treatment programs for<br />
Hodgkin disease [1] . These developments were encouraged<br />
by reports that mediastinal radiotherapy was associated<br />
with cardiac toxicity and second malignancies, particularly<br />
when chemotherapy agents were used concomitantly or<br />
sequentially. Second, sophisticated imaging technologies<br />
and new radiation delivery techniques have become available<br />
[2] . With the recent advances in irradiation devices, new<br />
intensity modulated irradiation modalities have emerged.<br />
Those <strong>of</strong>fer both increased target dose conformality and<br />
improved normal tissue avoidance. Helical tomotherapy<br />
combines inversely planned intensity modulated radiotherapy<br />
(IMRT) with on-board megavoltage imaging<br />
devices [3] . In this way, it has become possible to tailor very<br />
sharp dose distributions around the target volumes, close<br />
to critical organs [4] . It has emerged as one <strong>of</strong> the most<br />
promising techniques for IMRT delivery.<br />
Here we summarize some <strong>of</strong> the most promising applications<br />
<strong>of</strong> helical tomotherapy in patients with hematological<br />
malignancies.<br />
CLINICAL APPLICATIONS<br />
<strong>World</strong> J Radiol 2011 March 28; 3(3): 66-69<br />
ISSN 1949-8470 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
REVIEW<br />
For lymphoma irradiation, it is now the standard <strong>of</strong> care<br />
66 March 28, 2011|Volume 3|Issue 3|
to use involved-field radiotherapy rather than the extended<br />
radiation fields <strong>of</strong> the past [5] . In this setting <strong>of</strong> volume<br />
reduction, implementation <strong>of</strong> new strategies aimed at<br />
further improving target coverage is promising. Helical<br />
tomotherapy combines inversely planned IMRT with<br />
on-board megavoltage imaging devices [3] . In this way, it<br />
has become possible to tailor very sharp dose distributions<br />
around the target volumes, close to critical organs.<br />
Improving dose conformality around the volumes has<br />
become an important end-point for radiation oncologists.<br />
Dosimetric results from planning studies <strong>of</strong> helical tomotherapy<br />
have demonstrated its ability in better sparing<br />
critical organs from irradiation, in comparison with more<br />
conventional irradiation modalities. Helical tomotherapy<br />
was shown to provide similar target coverage, and to<br />
improve both dose conformality and dose homogeneity<br />
within the target volume. This modern irradiation<br />
device allows accurate repositioning and critical organs<br />
visualization. Tomita et al [6] compared radiation treatment<br />
plans that used IMRT with helical tomotherapy or threedimensional<br />
conformal radiation therapy for nasal natural<br />
killer/T-cell lymphoma. Authors found that IMRT<br />
achieved significantly better coverage <strong>of</strong> the planning<br />
target volume (PTV), with more than 99% <strong>of</strong> the PTV<br />
receiving 90% <strong>of</strong> the prescribed dose, whereas 3D-CRT<br />
could not provide adequate coverage <strong>of</strong> the PTV, with<br />
only 90.0% receiving 90% (P < 0.0001). These results<br />
and others demonstrated that helical tomotherapy could<br />
significantly improve target coverage when the PTV was<br />
close to critical organs.<br />
Prospective data with long-term follow-up evidenced<br />
that heart dose exposure may cause cardiac disease and<br />
adversely affect quality <strong>of</strong> life, particularly in young patients<br />
with mediastinal radiotherapy for Hodgkin lymphoma.<br />
Hudson et al [7] assessed the impact <strong>of</strong> treatment<br />
toxicity on long-term survival in pediatric Hodgkin’s<br />
disease, and reported an excess mortality from cardiac disease<br />
in survivors <strong>of</strong> pediatric Hodgkin’s disease (22, 95%<br />
CI: 8-48), compared with age- and sex-matched control<br />
populations. Cardiac irradiation contributes to this excess<br />
<strong>of</strong> risk [8] . Recent data reported that helical tomotherapy<br />
could decrease radiation dose exposure for breasts, lung,<br />
heart and thyroid gland in patients treated for advanced<br />
Hodgkin’s disease [9] .<br />
Since radiation-induced cardiovascular pathology<br />
is a major concern in patients undergoing therapeutic<br />
chest irradiation, helical tomotherapy has been logically<br />
investigated for improving heart avoidance. The physiopathology<br />
and manifestations <strong>of</strong> radiation-induced heart<br />
disease may considerably vary according to the dose,<br />
volume and technique <strong>of</strong> irradiation, and every effort<br />
should be made to avoid irradiating cardiac structures [10] .<br />
In this way, it will be possible to substantially decrease<br />
the risk <strong>of</strong> death from ischemic heart disease associated<br />
with radiation, which is particularly significant in patients<br />
receiving other cardiotoxic agents, such as anthracyclines.<br />
Actually, helical tomotherapy also allows treatments<br />
that would be difficult for conventional radiotherapy<br />
WJR|www.wjgnet.com<br />
Kirova YM et al . Modern radiotherapy <strong>of</strong> lymphomas<br />
machines to deliver, such as treating mediastinal lymph<br />
nodes [11] . Figure 1 shows the distribution dose during radiotherapy<br />
<strong>of</strong> a patient who was diagnosed with multiple<br />
pleural and mediastinal locations from lymphoma. Dosevolumes<br />
histograms evidence accurate sparing <strong>of</strong> some<br />
organs at risk, with the possibility to treat multiple targets<br />
simultaneously.<br />
Several other promising applications for helical tomotherapy<br />
have emerged. These strategies include treatment<br />
<strong>of</strong> patients who are at high risk <strong>of</strong> radiation-induced toxicity<br />
because <strong>of</strong> individual susceptibility, such as patients<br />
with acquired immunodeficiency [12] . Helical tomotherapy<br />
could also be used for decreasing the doses to critical<br />
structures in patients treated with concurrent targeted<br />
agents, which might potentially increase the risk <strong>of</strong> side<br />
effects [13] . Moreover, it permits re-irradiation <strong>of</strong> relapsed<br />
disease, a setting that considerably increases the risk <strong>of</strong><br />
consequent delayed toxicity. Introducing helical tomotherapy<br />
to the field <strong>of</strong> lymphoma may also provide safer<br />
and more accurate radiotherapy to selected patients with<br />
bulky residual disease [1] . We previously reported the feasibility<br />
<strong>of</strong> helical tomotherapy to decrease the acute toxicity<br />
<strong>of</strong> debulking irradiation before allograft in patients<br />
with refractory lymphoma. In other malignancies, our<br />
retrospective data in patients with solitary plasmocytoma<br />
demonstrated that doses to critical organs, including the<br />
heart, lungs, or kidneys could be decreased [14] . This may<br />
be clinically relevant in heavily pretreated patients who<br />
are at risk for subsequent treatment-related cardiac toxicity.<br />
High response rates were also reported and encouraged<br />
further prospective assessment, and most patients<br />
experienced a complete response prior to stem cell allograft.<br />
An increased risk <strong>of</strong> secondary malignancies has been<br />
reported after radiotherapy for lymphoma. In particular,<br />
young patients have a high risk <strong>of</strong> developing breast cancer<br />
in their life after mediastinal radiotherapy for a lymphoma<br />
[15] . The improved outcome among patients with<br />
Hodgkin’s lymphoma has been associated with increased<br />
incidence <strong>of</strong> second malignancies. This risk becomes<br />
significantly elevated 5 to 10 years after irradiation for<br />
Hodgkin lymphoma [16,17] and the incidence <strong>of</strong> breast cancer<br />
has been reported to increase by a factor <strong>of</strong> 4.3 (95%<br />
CI: 2.0-8.4) for patients treated with mantle irradiation [18] .<br />
Koh et al [19] quantified the reduction in radiation dose to<br />
normal tissues and modeled the reduction in secondary<br />
breast cancer risk, and suggested significant relative<br />
risk reduction for second cancers with involved field<br />
radiotherapy. While the dose response for radiation dose<br />
above 10 Gy remains uncertain, carcinogenesis after radiation<br />
is exacerbated by the large dose gradient across the<br />
breast and treatment field position [20] . Although helical<br />
tomotherapy might significantly decrease high doses delivered<br />
to the breast, it increases the volume that receives<br />
lower doses, which has also been implicated in the carcinogenesis<br />
process. For that reason, intensity-modulated<br />
irradiation should not be delivered in children outside <strong>of</strong><br />
a clinical trial.<br />
67 March 28, 2011|Volume 3|Issue 3|
proton therapy is very low and only a few patients could<br />
benefit from this highly conformal irradiation modality.<br />
CONCLUSION<br />
There is growing dosimetric evidence that highly conformal<br />
irradiation modalities may improve critical organs<br />
sparing, with clinically relevant consequences. Prospective<br />
clinical evaluation <strong>of</strong> helical tomotherapy modalities is<br />
required to confirm the potential benefits <strong>of</strong> highly conformal<br />
therapies applied to hematological malignancies.<br />
REFERENCES<br />
1 Yahalom J. Transformation in the use <strong>of</strong> radiation therapy <strong>of</strong><br />
Hodgkin lymphoma: new concepts and indications lead to<br />
modern field design and are assisted by PET imaging and intensity<br />
modulated radiation therapy (IMRT). Eur J Haematol<br />
Suppl 2005; 90-97<br />
2 Girinsky T, Ghalibafian M. Radiotherapy <strong>of</strong> hodgkin lymphoma:<br />
indications, new fields, and techniques. Semin Radiat<br />
Oncol 2007; 17: 206-222<br />
3 Welsh JS, Patel RR, Ritter MA, Harari PM, Mackie TR, Mehta<br />
MP. Helical tomotherapy: an innovative technology and<br />
approach to radiation therapy. Technol Cancer Res Treat 2002;<br />
1: 311-316<br />
4 Beavis AW. Is tomotherapy the future <strong>of</strong> IMRT? Br J Radiol<br />
2004; 77: 285-295<br />
5 Fermé C, Eghbali H, Meerwaldt JH, Rieux C, Bosq J, Berger F,<br />
Girinsky T, Brice P, van't Veer MB, Walewski JA, Lederlin P,<br />
Tirelli U, Carde P, Van den Neste E, Gyan E, Monconduit M,<br />
Diviné M, Raemaekers JM, Salles G, Noordijk EM, Creemers<br />
GJ, Gabarre J, Hagenbeek A, Reman O, Blanc M, Thomas J,<br />
Vié B, Kluin-Nelemans JC, Viseu F, Baars JW, Poortmans P,<br />
Lugtenburg PJ, Carrie C, Jaubert J, Henry-Amar M. Chemotherapy<br />
plus involved-field radiation in early-stage Hodgkin's<br />
disease. N Engl J Med 2007; 357: 1916-1927<br />
6 Tomita N, Kodaira T, Tachibana H, Nakamura T, Nakahara<br />
R, Inokuchi H, Mizoguchi N, Takada A. A comparison <strong>of</strong><br />
radiation treatment plans using IMRT with helical tomotherapy<br />
and 3D conformal radiotherapy for nasal natural<br />
killer/T-cell lymphoma. Br J Radiol 2009; 82: 756-763<br />
7 Hudson MM, Poquette CA, Lee J, Greenwald CA, Shah A,<br />
Luo X, Thompson EI, Wilimas JA, Kun LE, Crist WM. Increased<br />
mortality after successful treatment for Hodgkin's<br />
disease. J Clin Oncol 1998; 16: 3592-3600<br />
8 Prosnitz RG, Chen YH, Marks LB. Cardiac toxicity following<br />
thoracic radiation. Semin Oncol 2005; 32: S71-S80<br />
9 Vlachaki MT, Kumar S. Helical tomotherapy in the radiotherapy<br />
treatment <strong>of</strong> Hodgkin's disease - a feasibility study. J<br />
Appl Clin Med Phys 2010; 11: 3042<br />
10 Gagliardi G, Constine LS, Moiseenko V, Correa C, Pierce LJ,<br />
Allen AM, Marks LB. Radiation dose-volume effects in the<br />
heart. Int J Radiat Oncol Biol Phys 2010; 76: S77-S85<br />
11 Chargari C, Vernant JP, Tamburini J, Zefkili S, Fayolle M,<br />
Campana F, Fourquet A, Kirova YM. Feasibility <strong>of</strong> Helical<br />
Tomotherapy for Debulking Irradiation Before Stem Cell<br />
Transplantation in Malignant Lymphoma. Int J Radiat Oncol<br />
Biol Phys 2010; Epub ahead <strong>of</strong> print<br />
12 Chargari C, Zefkili S, Kirova YM. Potential <strong>of</strong> helical tomotherapy<br />
for sparing critical organs in a patient with AIDS<br />
who was treated for Hodgkin lymphoma. Clin Infect Dis<br />
2009; 48: 687-689<br />
WJR|www.wjgnet.com<br />
Kirova YM et al . Modern radiotherapy <strong>of</strong> lymphomas<br />
13 Kirova YM, Chargari C, Amessis M, Vernant JP, Dhedin N.<br />
Concurrent involved field radiation therapy and temsirolimus<br />
in refractory mantle cell lymphoma (MCL). Am J Hematol<br />
2010; 85: 892<br />
14 Chargari C, Kirova YM, Zefkili S, Caussa L, Amessis M,<br />
Dendale R, Campana F, Fourquet A. Solitary plasmocytoma:<br />
improvement in critical organs sparing by means <strong>of</strong> helical<br />
tomotherapy. Eur J Haematol 2009; 83: 66-71<br />
15 Henderson TO, Amsterdam A, Bhatia S, Hudson MM, Meadows<br />
AT, Neglia JP, Diller LR, Constine LS, Smith RA, Mahoney<br />
MC, Morris EA, Montgomery LL, Landier W, Smith<br />
SM, Robison LL, Oeffinger KC. Systematic review: surveillance<br />
for breast cancer in women treated with chest radiation<br />
for childhood, adolescent, or young adult cancer. Ann Intern<br />
Med 2010; 152: 444-455; W144-W154<br />
16 Alm El-Din MA, El-Badawy SA, Taghian AG. Breast cancer<br />
after treatment <strong>of</strong> Hodgkin's lymphoma: general review. Int<br />
J Radiat Oncol Biol Phys 2008; 72: 1291-1297<br />
17 Metayer C, Lynch CF, Clarke EA, Glimelius B, Storm H, Pukkala<br />
E, Joensuu T, van Leeuwen FE, van't Veer MB, Curtis<br />
RE, Holowaty EJ, Andersson M, Wiklund T, Gospodarowicz<br />
M, Travis LB. Second cancers among long-term survivors <strong>of</strong><br />
Hodgkin's disease diagnosed in childhood and adolescence. J<br />
Clin Oncol 2000; 18: 2435-2443<br />
18 Zellmer DL, Wilson JF, Janjan NA. Dosimetry <strong>of</strong> the breast<br />
for determining carcinogenic risk in mantle irradiation. Int J<br />
Radiat Oncol Biol Phys 1991; 21: 1343-1351<br />
19 Koh ES, Tran TH, Heydarian M, Sachs RK, Tsang RW,<br />
Brenner DJ, Pintilie M, Xu T, Chung J, Paul N, Hodgson DC.<br />
A comparison <strong>of</strong> mantle versus involved-field radiotherapy<br />
for Hodgkin's lymphoma: reduction in normal tissue dose<br />
and second cancer risk. Radiat Oncol 2007; 2: 13<br />
20 Hodgson DC, Koh ES, Tran TH, Heydarian M, Tsang R,<br />
Pintilie M, Xu T, Huang L, Sachs RK, Brenner DJ. Individualized<br />
estimates <strong>of</strong> second cancer risks after contemporary<br />
radiation therapy for Hodgkin lymphoma. Cancer 2007; 110:<br />
2576-2586<br />
21 McCutchen KW, Watkins JM, Eberts P, Terwilliger LE, Ashenafi<br />
MS, Jenrette JM 3rd. Helical tomotherapy for total lymphoid<br />
irradiation. Radiat Med 2008; 26: 622-626<br />
22 Wong JY, Liu A, Schultheiss T, Popplewell L, Stein A,<br />
Rosenthal J, Essensten M, Forman S, Somlo G. Targeted total<br />
marrow irradiation using three-dimensional image-guided<br />
tomographic intensity-modulated radiation therapy: an<br />
alternative to standard total body irradiation. Biol Blood Marrow<br />
Transplant 2006; 12: 306-315<br />
23 Goodman KA, Toner S, Hunt M, Wu EJ, Yahalom J. Intensity-modulated<br />
radiotherapy for lymphoma involving the<br />
mediastinum. Int J Radiat Oncol Biol Phys 2005; 62: 198-206<br />
24 Cella L, Liuzzi R, Magliulo M, Conson M, Camera L, Salvatore<br />
M, Pacelli R. Radiotherapy <strong>of</strong> large target volumes in<br />
Hodgkin's lymphoma: normal tissue sparing capability <strong>of</strong><br />
forward IMRT versus conventional techniques. Radiat Oncol<br />
2010; 5: 33<br />
25 Weber DC, Peguret N, Dipasquale G, Cozzi L. Involvednode<br />
and involved-field volumetric modulated arc vs. fixed<br />
beam intensity-modulated radiotherapy for female patients<br />
with early-stage supra-diaphragmatic Hodgkin lymphoma:<br />
a comparative planning study. Int J Radiat Oncol Biol Phys<br />
2009; 75: 1578-1586<br />
26 Chera BS, Rodriguez C, Morris CG, Louis D, Yeung D, Li Z,<br />
Mendenhall NP. Dosimetric comparison <strong>of</strong> three different<br />
involved nodal irradiation techniques for stage II Hodgkin's<br />
lymphoma patients: conventional radiotherapy, intensitymodulated<br />
radiotherapy, and three-dimensional proton radiotherapy.<br />
Int J Radiat Oncol Biol Phys 2009; 75: 1173-1180<br />
S- Editor Cheng JX L- Editor O’Neill M E- Editor Zheng XM<br />
69 March 28, 2011|Volume 3|Issue 3|
W J R<br />
Online Submissions: http://www.wjgnet.com/1949-8470<strong>of</strong>fice<br />
wjr@wjgnet.com<br />
doi:10.4329/wjr.v3.i3.70<br />
Estimation <strong>of</strong> intra-operator variability in perfusion<br />
parameter measurements using DCE-US<br />
Marianne Gauthier, Ingrid Leguerney, Jessie Thalmensi, Mohamed Chebil, Sarah Parisot, Pierre Peronneau,<br />
Alain Roche, Nathalie Lassau<br />
Marianne Gauthier, Ingrid Leguerney, Jessie Thalmensi,<br />
Sarah Parisot, Pierre Peronneau, Alain Roche, Nathalie<br />
Lassau, IR4M, UMR 8081, CNRS, Paris-Sud 11 Univ, Gustave<br />
Roussy Institute, Villejuif 94805, France<br />
Mohamed Chebil, Nathalie Lassau, Department <strong>of</strong> Imaging,<br />
Ultrasonography Unit, Gustave Roussy Institute, Villejuif<br />
94805, France<br />
Author contributions: Gauthier M performed the majority<br />
<strong>of</strong> experiments, designed the study and wrote the manuscript;<br />
Leguerney I was involved in analyzing results and editing the<br />
manuscript; Thalmensi J, Parisot S and Peronneau P provided<br />
substantial contributions to conception and design, acquisition<br />
<strong>of</strong> data, analysis, and interpretation <strong>of</strong> the data; Chebil M was<br />
involved in the design <strong>of</strong> the study; Roche A supervised the<br />
project; Lassau N managed each step <strong>of</strong> the study, provided<br />
contribution to data analyses and was involved in editing the<br />
manuscript.<br />
Correspondence to: Marianne Gauthier, MSc, IR4M, UMR<br />
8081, CNRS, Paris-Sud 11 Univ, Gustave Roussy Institute,<br />
Villejuif 94805, France. marianne.gauthier@igr.fr<br />
Telephone: +33-1-42116215 Fax: +33-1-42115495<br />
Received: December 24, 2010 Revised: March 2, 2011<br />
Accepted: March 9, 2011<br />
Published online: March 28, 2011<br />
Abstract<br />
AIM: To investigate intra-operator variability <strong>of</strong> semiquantitative<br />
perfusion parameters using dynamic contrast-enhanced<br />
ultrasonography (DCE-US), following<br />
bolus injections <strong>of</strong> SonoVue ® .<br />
METHODS: The in vitro experiments were conducted<br />
using three in-house sets up based on pumping a fluid<br />
through a phantom placed in a water tank. In the in vivo<br />
experiments, B16F10 melanoma cells were xenografted<br />
to five nude mice. Both in vitro and in vivo , images<br />
were acquired following bolus injections <strong>of</strong> the ultrasound<br />
contrast agent SonoVue ® (Bracco, Milan, Italy)<br />
and using a Toshiba Aplio ® ultrasound scanner connected<br />
to a 2.9-5.8 MHz linear transducer (PZT, PLT 604AT<br />
WJR|www.wjgnet.com<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Radiology<br />
probe) (Toshiba, Japan) allowing harmonic imaging<br />
(“Vascular Recognition Imaging”) involving linear raw<br />
data. A mathematical model based on the dye-dilution<br />
theory was developed by the Gustave Roussy Institute,<br />
Villejuif, France and used to evaluate seven perfusion<br />
parameters from time-intensity curves. Intra-operator<br />
variability analyses were based on determining perfusion<br />
parameter coefficients <strong>of</strong> variation (CV).<br />
RESULTS: In vitro , different volumes <strong>of</strong> SonoVue ®<br />
were tested with the three phantoms: intra-operator<br />
variability was found to range from 2.33% to 23.72%.<br />
In vivo , experiments were performed on tumor tissues<br />
and perfusion parameters exhibited values ranging<br />
from 1.48% to 29.97%. In addition, the area under the<br />
curve (AUC) and the area under the wash-out (AUWO)<br />
were two <strong>of</strong> the parameters <strong>of</strong> great interest since<br />
throughout in vitro and in vivo experiments their variability<br />
was lower than 15.79%.<br />
CONCLUSION: AUC and AUWO appear to be the most<br />
reliable parameters for assessing tumor perfusion using<br />
DCE-US as they exhibited the lowest CV values.<br />
© 2011 Baishideng. All rights reserved.<br />
<strong>World</strong> J Radiol 2011 March 28; 3(3): 70-81<br />
ISSN 1949-8470 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
ORIGINAL ARTICLE<br />
Key words: Dynamic contrast-enhanced ultrasonography;<br />
Intra-operator variability; Functional imaging; Semi-quantitative<br />
perfusion parameters; Linear raw data; Quantification<br />
Peer reviewers: Chan Kyo Kim, MD, Assistant Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Radiology, Samsung Medical Center, Sungkyunkwan<br />
University School <strong>of</strong> Medicine, 50 Ilwon-dong, Kangnamgu,<br />
Seoul 135-710, South Korea; Sergio Casciaro, PhD, Institute<br />
<strong>of</strong> Clinical Physiology - National Research Council,Campus<br />
Universitario Ecotekne, Via Monteroni, 73100 Lecce, Italy<br />
Gauthier M, Leguerney I, Thalmensi J, Chebil M, Parisot S,<br />
Peronneau P, Roche A, Lassau N. Estimation <strong>of</strong> intra-operator<br />
variability in perfusion parameter measurements using DCE-<br />
70 March 28, 2011|Volume 3|Issue 3|
US. <strong>World</strong> J Radiol 2011; 3(3): 70-81 Available from: URL:<br />
http://www.wjgnet.com/1949-8470/full/v3/i3/70.htm DOI:<br />
http://dx.doi.org/10.4329/wjr.v3.i3.70<br />
INTRODUCTION<br />
Tumor angiogenesis is a process involving the proliferation<br />
<strong>of</strong> new blood vessels which penetrate tumors supplying<br />
them with nutrients and oxygen [1,2] . Nowadays, research<br />
is focused on the development <strong>of</strong> anti-angiogenic<br />
treatments whose aim is to destroy neoblood vessels<br />
which <strong>of</strong>ten occur initially without any morphological<br />
changes [3,4] .<br />
Until now, treatment evaluation has been based on<br />
Response Evaluation Criteria in Solid Tumors (RECIST) [5] .<br />
Even though RECIST criteria were recently revised, they<br />
still only concern morphological information [6] . It is commonly<br />
recognized that this criterion is no longer optimal<br />
for the early assessment <strong>of</strong> anti-angiogenic treatments<br />
which primarily target microvascularization. Functional<br />
imaging is currently establishing itself as the best modality<br />
for evaluating such therapies, by determining a series <strong>of</strong><br />
semi-quantitative perfusion parameters related to tumor<br />
perfusion. These were defined as semi-quantitative as they<br />
only provided a relative evaluation <strong>of</strong> the physiological<br />
parameters such as blood flow or blood volume based on<br />
the dye dilution theory.<br />
Nowadays, dynamic contrast-enhanced ultrasonography<br />
(DCE-US) is becoming increasingly widespread [7,8] as<br />
it allows functional imaging [9,10] . However, one <strong>of</strong> its major<br />
drawbacks is its intra-operator variability which could<br />
have a major impact on measurements, leading to erroneous<br />
interpretations. A small difference in perfusion could<br />
be interpreted as a functional change but might simply be<br />
due to operator variability.<br />
Until now, information on intra-operator variability has<br />
been lacking. Consequently, the purpose <strong>of</strong> our study was<br />
to evaluate the intra-operator variability <strong>of</strong> semi-quantitative<br />
perfusion parameter measurements using DCE-US,<br />
both in vitro and in vivo, following bolus injections <strong>of</strong> SonoVue<br />
® (Bracco, Milan, Italy).<br />
MATERIALS AND METHODS<br />
Contrast agents<br />
DCE-US studies were performed using bolus injections<br />
<strong>of</strong> SonoVue ® , a second generation contrast agent, consisting<br />
<strong>of</strong> microbubbles <strong>of</strong> sulphur hexafluoride (SF6)<br />
stabilized by a shell <strong>of</strong> amphiphilic phospholipids [11,12] .<br />
The SF6 gas does not interact with any other molecules<br />
found in the body as it is a very inert gas. The size <strong>of</strong> the<br />
microbubbles, ranging from 1 to 10 μm [12] , allows them<br />
to circulate through the whole blood volume. In addition,<br />
SonoVue ® is a purely intravascular contrast agent which<br />
makes it ideal for the evaluation <strong>of</strong> perfusion [12] . Insonated<br />
at low acoustic power, SonoVue ® , whose nonlinear<br />
harmonic response is high [13] , provides continuous real-<br />
WJR|www.wjgnet.com<br />
Gauthier M et al . Variability <strong>of</strong> perfusion parameters using DCE-US<br />
time ultrasonographic (US) imaging without destroying<br />
the microbubbles [14] .<br />
Before any US exam, the contrast agent was reconstituted<br />
by introducing 5 mL <strong>of</strong> 0.9% sodium chloride into<br />
the vial, containing a pyrogen-free lyophilized product,<br />
followed by manual shaking for at least 20 s. One experiment<br />
involved several injections <strong>of</strong> SonoVue ® . As the<br />
microbubbles tended to accumulate at the upper surface<br />
because <strong>of</strong> buoyancy, the preparation was systematically<br />
manually checked before each injection in order to recover<br />
the required homogeneous solution. Each experiment<br />
lasted less than 2 h on account <strong>of</strong> the stability <strong>of</strong> SonoVue<br />
® over time which is 6 h after its reconstitution [11] .<br />
Time-intensity method<br />
The time intensity method is essentially based on the dye<br />
dilution theory: after the injection <strong>of</strong> the indicators, contrast<br />
agent concentration is monitored as a function <strong>of</strong><br />
time, generating a time intensity curve (TIC) from which<br />
a series <strong>of</strong> semi-quantitative perfusion parameters is extracted<br />
and analyzed [15,16] . To be valid, a series <strong>of</strong> assumptions<br />
must be verified [17] : (1) Flow has to be constant so<br />
that the amount <strong>of</strong> microbubbles injected has no effect<br />
on the flux; (2) Blood and contrast agent must be adequately<br />
mixed to obtain a homogeneous concentration;<br />
(3) Recirculation should not interfere with the first pass;<br />
and (4) The mixing <strong>of</strong> the contrast agent must exhibit<br />
linearity and a stable condition [18] . Linearity refers to the<br />
linear relationship between bubble concentration and signal<br />
intensity and was previously confirmed for low doses<br />
by Greis [12] as well as by Lampaskis et al [19] in the context<br />
<strong>of</strong> bolus injection.<br />
In our study, conditions were assumed to be satisfied.<br />
The semi-quantitative perfusion parameters that we analyzed<br />
were therefore directly extracted from the TIC.<br />
In vitro studies<br />
US protocol: SonoVue ® bolus injections were performed<br />
through a 1-mL syringe (Terumo ® , Belgium) and a<br />
“26Gx1/2” needle (Terumo ® , Belgium). The injection<br />
site was marked so that the same site was used for all the<br />
in vitro studies. It was positioned at a distance <strong>of</strong> 30 cm<br />
from the input <strong>of</strong> the phantom.<br />
According to the Guidelines for Evaluating and Expressing<br />
the Uncertainty <strong>of</strong> NIST (National Institute <strong>of</strong><br />
Standards and Technology) Measurements Results, intraoperator<br />
variability studies must be performed under the<br />
following conditions: (1) The same measurement procedure;<br />
(2) The same observer; (3) The same measuring instrument,<br />
used under the same conditions; (4) The same<br />
location; and (5) Repetition over a short period <strong>of</strong> time.<br />
Thus, all the experimental conditions as well as the<br />
operators injecting the SonoVue ® and manipulating the<br />
ultrasound scanner were the same for all acquisitions.<br />
To minimize errors which might have been due to<br />
possible SonoVue ® residues in the injection materials, a<br />
new syringe and a new needle were used for each injection.<br />
In addition, the circuit was entirely emptied, rinsed<br />
71 March 28, 2011|Volume 3|Issue 3|
Gauthier M et al . Variability <strong>of</strong> perfusion parameters using DCE-US<br />
6<br />
3<br />
4<br />
Figure 1 Schematic diagram <strong>of</strong> the closed-circuit. No contact with ambient<br />
air was possible. In addition, as water was degassed, no significant amount <strong>of</strong><br />
gas was trapped in the circuit. Based on the same set-up, three phantoms were<br />
used throughout the in vitro experiments: (a) a single straight pipe phantom; (b)<br />
a three intertwined pipe phantom; (c) a dialyzer. The Gustave Roussy Institute<br />
(IGR) ratio was tested throughout the in vitro experiments as it corresponded<br />
to the ratio (4.8 mL per patient) previously validated and routinely used at the<br />
IGR. 1: Peristaltic pump; 2: Syringe; 3: PZT, PLT 604AT probe; 4: Phantom; 5:<br />
Custom-made water tank; 6: Reservoir; 7: Tubing (silicone pipe; internal diameter:<br />
2 mm; wall thickness: 1 mm).<br />
and reset with degassed water between each acquisition.<br />
Thus, no contrast agent residues were present in the circuit<br />
so that the initial conditions were exactly the same<br />
for all the experiments.<br />
The three phantoms consisted <strong>of</strong> a closed-circuit flow<br />
model as no contact with ambient air was possible. Consequently,<br />
as the water was degassed and the circuit was<br />
closed, no significant amount <strong>of</strong> gas was trapped in the<br />
set-up (Figure 1).<br />
Images were acquired using a Toshiba Aplio ® ultrasound<br />
scanner (Toshiba, Japan) version 6, release 5, connected<br />
to a 2.9-5.8 MHz linear transducer (PZT, PLT<br />
604AT probe). Harmonic imaging was performed using<br />
the “Vascular Recognition Imaging” (VRI) mode combining:<br />
(1) Fundamental B mode imaging, which allows<br />
simultaneous but independent grey scale visualization <strong>of</strong><br />
morphological structures; (2) Doppler imaging, which<br />
provides vascular information; and (3) Harmonic imaging,<br />
based on the pulse inversion mode, which consists<br />
<strong>of</strong> summing echoes resulting from two waves which are<br />
inverted copies <strong>of</strong> each other. As microbubbles exhibit<br />
non-linear responses, the resulting sum <strong>of</strong> the echoes will<br />
be different from 0 implying a non-null signal [20] .<br />
Acquisitions lasting 50 s were obtained at a low mechanical<br />
index (MI = 0.1) and at a rate <strong>of</strong> 5 frames per second<br />
(fps).<br />
Single straight pipe phantom: The first assembly consisted<br />
<strong>of</strong> a single straight silicone pipe phantom, immersed<br />
in a custom-made water tank which was connected to a<br />
peristaltic pump (SP vario/PD 5101, Heidolph ® , Germany)<br />
providing a defined water flow rate <strong>of</strong> 42.4 mL/min.<br />
This phantom was used to mimic blood flow. Tubing was<br />
made <strong>of</strong> a 1 mm thick silicone pipe with a 2 mm internal<br />
diameter. A custom-made probe holder was used to keep<br />
the probe still throughout the experiments.<br />
A region <strong>of</strong> interest (ROI) was set in the upper part<br />
WJR|www.wjgnet.com<br />
5<br />
7<br />
2<br />
1<br />
B<br />
7.6<br />
A<br />
Power (a.u.)<br />
140<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
0 20 40<br />
t/s<br />
1<br />
5 fps<br />
VRh5.8<br />
9.2<br />
MI 0.1<br />
Linear raw data<br />
Figure 2 Single straight pipe phantom. A: Image extracted from an acquisition<br />
obtained after the bolus injection <strong>of</strong> SonoVue ® . Harmonic imaging was<br />
done based on the Vascular Recognition Imaging mode. The region <strong>of</strong> interest<br />
was set in the upper part <strong>of</strong> the pipe. Each acquisition involved a new manually<br />
drawn region <strong>of</strong> interest. Once the region <strong>of</strong> interest was selected, the ultrasound<br />
scanner directly allowed access to the time intensity curve associated<br />
with the selected region <strong>of</strong> interest. The linear raw data to be modeled were<br />
converted through text files generated by the ultrasound scanner and extracted<br />
to obtain a graph using Excel ® ; B: The graph displays the Excel ® curve to be fitted<br />
and analyzed in order to obtain the perfusion parameters.<br />
<strong>of</strong> the pipe (Figure 2A). Each injection involved a new<br />
ROI and its associated TIC (Figure 2B). Three volumes<br />
<strong>of</strong> SonoVue ® were tested. The first experiment involved<br />
five 0.02 mL bolus injections <strong>of</strong> contrast agent for a<br />
total amount <strong>of</strong> water set at 50 mL in the closed-circuit.<br />
This ratio respected that granted by marketing approval<br />
(“Autorisation de Mise sur le Marché”: AMM) (2.4 mL <strong>of</strong><br />
SonoVue ® for 5 L <strong>of</strong> blood). The second experiment was<br />
performed by injecting five times a 0.05 mL bolus <strong>of</strong> SonoVue<br />
® . This volume involved a ratio routinely used for<br />
clinical exams (4.8 mL <strong>of</strong> SonoVue ® for 5 L <strong>of</strong> blood)<br />
and particularly in four studies performed at the Gustave<br />
Roussy Institute (IGR), involving 117 patients and 823<br />
DCE-US exams [21,22] as well as a national project supported<br />
by the “Institut National du Cancer” (French National<br />
Cancer Institute) [23] . The last experiment involved five<br />
0.08 mL bolus injections <strong>of</strong> SonoVue ® . As the phantom<br />
became more complex, we focused on the IGR ratio previously<br />
validated in IGR studies.<br />
Three intertwined pipe phantom: A second phantom<br />
consisted <strong>of</strong> three intertwined silicone pipes immersed in<br />
a custom-made water tank. Two <strong>of</strong> the three tubes were<br />
72 March 28, 2011|Volume 3|Issue 3|
6.9<br />
B<br />
C<br />
A<br />
Power (a.u.)<br />
6000<br />
4500<br />
3000<br />
1500<br />
0<br />
in silicone with an internal diameter <strong>of</strong> 2 mm and a 1 mm<br />
thick wall as in the case <strong>of</strong> the previous phantom. The<br />
third one, originating from a catheter (Surflo ® winged infusion<br />
set, Terumo ® , Belgium), had a 1 mm internal diameter<br />
and a 0.5 mm thick wall. The input and the output <strong>of</strong><br />
the phantom were composed <strong>of</strong> three-way taps (Disc<strong>of</strong>ix ® ,<br />
B. Braun, Melsungen, Germany) allowing linkage between<br />
the three pipes (Figure 3A). The phantom was connected<br />
to the same pump as previously described, providing a<br />
defined water flow rate set at 42.4 mL/min. Such an as-<br />
WJR|www.wjgnet.com<br />
1<br />
0 5 10 15 20<br />
t /s<br />
Linear raw data<br />
5 fps<br />
VRh5.8<br />
9.2<br />
MI 0.1<br />
Figure 3 Three intertwined pipe phantom. A: Picture <strong>of</strong> the phantom: three<br />
pipes (2 pipes with a 2 mm internal diameter and a 1 mm thick wall, 1 pipe with<br />
a 1 mm internal diameter and a 0.5 mm thick wall ) were intertwined to mimic a<br />
complex structure akin to that <strong>of</strong> vessels in the microvascularization; B: Image<br />
extracted from an acquisition obtained after a bolus injection <strong>of</strong> SonoVue ® . As<br />
in the case <strong>of</strong> the first phantom, harmonic imaging was based on the Vascular<br />
Recognition Imaging mode. The region <strong>of</strong> interest contained both pipes and<br />
water and was manually drawn for each <strong>of</strong> the five injections; C: Based on the<br />
selected region <strong>of</strong> interest, the ultrasound scanner provided the time intensity<br />
curve converted through text files. These were used to display the associated<br />
Excel ® curve to be analyzed.<br />
Gauthier M et al . Variability <strong>of</strong> perfusion parameters using DCE-US<br />
sembly was designed to mimic a complex structure akin to<br />
that <strong>of</strong> vessels in tumors.<br />
A new ROI containing both pipes and water spaces<br />
(Figure 3B), was drawn for each injection and the associated<br />
TIC was obtained (Figure 3C). The total amount<br />
<strong>of</strong> water in the circuit was set at 60 mL. Two series <strong>of</strong><br />
acquisitions were obtained involving, respectively, five<br />
0.03 mL (AMM ratio) and 0.06 mL (IGR ratio) bolus injections<br />
<strong>of</strong> contrast agent.<br />
Dialyzer: The third assembly was composed <strong>of</strong> a dialyzer<br />
(FX PAED, Fresenius Medical Care, France). The dialysis<br />
cartridge, consisting <strong>of</strong> about 1550 capillaries with an<br />
internal diameter <strong>of</strong> 220 μm, was connected to the peristaltic<br />
pump providing a water flow rate <strong>of</strong> 42.4 mL/min<br />
and was immersed in water. To minimize attenuation due<br />
to the original plastic case <strong>of</strong> the dialyzer, a rectangular<br />
part <strong>of</strong> it was removed and replaced by a cellophane sheet<br />
to maintain the circuit closed [24] . The advantage <strong>of</strong> such a<br />
phantom was that the capillaries <strong>of</strong> the dialyzer were comparable<br />
in dimension to that <strong>of</strong> one type <strong>of</strong> vessel found<br />
in the microvascularization (arteriole diameter < 300 μm).<br />
In addition, as the size <strong>of</strong> SonoVue ® microbubbles ranged<br />
from 1 to 10 μm [12] , they were about a thousand-fold the<br />
dimensions <strong>of</strong> capillary pores (2.4 nm), thus ensuring the<br />
intravascular property <strong>of</strong> the ultrasound contrast agent.<br />
As shown in Figure 4A, attenuation occurs in the lower<br />
part <strong>of</strong> the dialyzer: it is characterized by a strong decrease<br />
in amplitude and a loss <strong>of</strong> the contrast signal. An<br />
ROI was drawn for each <strong>of</strong> the repeated measurements<br />
and only contained the upper part <strong>of</strong> the dialyzer so that<br />
the acquisition was not prone to attenuation phenomena<br />
[25] . Based on the selected ROI, the associated time<br />
intensity curve was obtained for the analysis (Figure 4B).<br />
The total amount <strong>of</strong> water was 100 mL and a volume <strong>of</strong><br />
0.10 mL <strong>of</strong> SonoVue ® was tested five times (IGR ratio).<br />
In vivo studies<br />
Animals and tumor model: Experiments were conducted<br />
with nude female mice aged from 6 to 8 wk with the<br />
approval <strong>of</strong> the European Convention for the Protection<br />
<strong>of</strong> Vertebrate Animals used for experimental and other<br />
scientific purposes (Strasbourg, 18.III.1986; text amended<br />
according to the provisions <strong>of</strong> protocol ETS No. 170 as<br />
<strong>of</strong> its entry into force on 2nd December 2005).<br />
The selected tumor model was the B16F10 (CRL-6475,<br />
ATCC, American Type Culture Collection) melanoma cell<br />
line which is a murine skin cancer. The tumor cells were<br />
cultured in DMEM (Dulbecco minimum essential medium)<br />
(Gibco Life Technologies, France) combined with<br />
10% fetal bovine serum, 1% penicillin/streptomycin and<br />
glutamate (Invitrogen Life Technologies, Inc., France)<br />
to avoid bacterial contamination <strong>of</strong> the solution. While<br />
growing, cells were maintained in an incubator at 37℃.<br />
Tumors were xenografted onto the right flank <strong>of</strong> five<br />
mice (Figure 5A) through a subcutaneous injection <strong>of</strong> 2<br />
× 10 6 melanoma cells in 0.2 mL <strong>of</strong> Phosphate Buffered<br />
Saline (PBS). DCE-US exams were performed following<br />
three 0.02 mL, 0.05 mL or 0.1 mL retro-orbital bolus<br />
73 March 28, 2011|Volume 3|Issue 3|
B<br />
Power (a.u.)<br />
7.6<br />
A<br />
Gauthier M et al . Variability <strong>of</strong> perfusion parameters using DCE-US<br />
Attenuated part<br />
1030<br />
930<br />
830<br />
730<br />
630<br />
530<br />
430<br />
0 10 20 30 40<br />
t /s<br />
injections <strong>of</strong> SonoVue ® according to the methodology<br />
used in our lab.<br />
Settings: During the experiments, mice were placed on<br />
the left flank and maintained at a constant temperature<br />
through a warming pad (TEM, Bordeaux, France) connected<br />
to a Gaymar T/Pump ® (Gaymar Industries, Inc.,<br />
USA). The temperature was regulated with the adjustable<br />
thermostat <strong>of</strong> the pump and was set at 40°C (internal<br />
mouse temperature: 39℃). Each mouse was weighed and<br />
the tumor volume was determined before each DCE-<br />
US exam. The ROI was set to exclusively include the<br />
tumor (Figure 5B-C). An ROI was drawn for each <strong>of</strong><br />
the repeated measurements and once it was selected, the<br />
ultrasound scanner directly allowed access to the time intensity<br />
curve associated with the selected ROI. The linear<br />
raw data to be modeled were converted through text files<br />
and extracted to obtain a graph using Excel ® (Figure 5D).<br />
A break <strong>of</strong> at least 15 min was observed between each<br />
injection in addition to 3 min <strong>of</strong> insonation at a high<br />
mechanical index (MI = 1.4), so that contrast agent could<br />
be eliminated. Mice were kept asleep no more than 2 h.<br />
This duration included the time required for the mice to<br />
obtain a stationary heart rate after the administration <strong>of</strong><br />
anesthesia, acquisition time and the duration <strong>of</strong> the break<br />
WJR|www.wjgnet.com<br />
5 fps<br />
VRh5.8<br />
9.2<br />
MI 0.1<br />
Linear raw data<br />
Figure 4 Dialyzer. A: Image extracted from an acquisition obtained after a<br />
bolus injection <strong>of</strong> SonoVue ® . As in the case <strong>of</strong> the first two phantoms, harmonic<br />
imaging was based on the Vascular Recognition Imaging mode. The region <strong>of</strong><br />
interest contained the upper part <strong>of</strong> the dialyzer to avoid attenuation phenomena<br />
in the lower parts. This was manually drawn for each injection; B: To determine<br />
perfusion parameters from the time intensity curve obtained following the<br />
selection <strong>of</strong> the region <strong>of</strong> interest, this was converted through text files so that<br />
the analysis could be performed using the Solver program in Excel ® .<br />
between each injection. Three injections per mouse were<br />
considered for the data analysis. Mice underwent either<br />
chemical or gaseous anesthesia.<br />
Chemical anesthesia: The amount <strong>of</strong> chemical anesthesia<br />
was determined based upon mouse body weight. Once<br />
weighed, the required amount <strong>of</strong> anesthesia was prepared<br />
and injected intraperitoneally using the 1-mL syringe and a<br />
“30Gx1/2” needle (Microlance, Ireland). The solution<br />
consisted <strong>of</strong> ketamine (10 mg/mL, Ketalar ® , Parapharm,<br />
France) and xylazine (2%, Rompun ® , Bayer, France). To<br />
ensure that the mice remained asleep throughout the<br />
experiment, 150 µL/g per mouse were systematically injected.<br />
Gaseous anesthesia: Mice were anaesthetized through<br />
a 2 L/min inhalation <strong>of</strong> O2 combined with 2.5% <strong>of</strong> is<strong>of</strong>lurane.<br />
It was possible to modify the flow rate during the<br />
experiment so that mice could be maintained asleep without<br />
being endangered throughout the experiment.<br />
US protocol: Preliminary fundamental B-mode imaging<br />
using a 14 MHz PLT 1204AT (Toshiba, Japan) probe<br />
was performed to determine the tumor volume prior to<br />
the SonoVue ® injection (Figure 5B). The largest longitudinal<br />
and transversal sections allowed us to determine<br />
the tumor volume by measuring the three perpendicular<br />
tumor diameters [26] according to the following formula:<br />
V = 1/2 × (depth × width × length).<br />
Harmonic imaging was performed in the same way<br />
as for the in vitro experiments with a mechanical index set<br />
at 0.1 and a rate <strong>of</strong> 5 fps. Acquisitions lasting 3 min were<br />
recorded allowing visualization <strong>of</strong> both the wash-in and<br />
wash-out parts <strong>of</strong> the TICs.<br />
Data analysis<br />
As already described in the literature, linear raw data (uncompressed<br />
linear data obtained before standard videovisualization)<br />
have the advantage <strong>of</strong> exhibiting a linear<br />
dynamic range which is the essential part <strong>of</strong> the evaluation<br />
<strong>of</strong> semi-quantitative perfusion parameters from<br />
TICs [27] . Acquisitions involved recording harmonic images<br />
after the SonoVue ® injection, using dedicated s<strong>of</strong>tware,<br />
CHI-Q ® , on the Toshiba Aplio ® ultrasound scanner. In<br />
a manually outlined ROI, the mean US signal intensity<br />
induced by contrast uptake was obtained and expressed<br />
in arbitrary units. This was linearly linked to the number<br />
and size <strong>of</strong> microbubbles in the ROI (Aplio ® procedure)<br />
[28,29] . Then, the corresponding TIC to be modeled<br />
was converted through text files generated by the ultrasound<br />
scanner and extracted to obtain a graph using Excel<br />
® . Seven semi-quantitative perfusion parameters were<br />
extracted from this curve: the peak intensity (PI) was the<br />
difference between Vmax [maximal intensity value: V(Tmax)]<br />
and V0 [Initial intensity value: V(T0)] and represented the<br />
highest intensity value attained by the TIC for the defined<br />
ROI. The time to peak intensity (TPI), corresponding<br />
to Time to Peak Intensity, was the time required for the<br />
contrast agent to arrive in the tumor and reach the PI. It<br />
74 March 28, 2011|Volume 3|Issue 3|
D<br />
A<br />
Power (a.u.)<br />
140<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
0 20 40 60 80 100 120<br />
t /s<br />
corresponded to the difference between the latency time<br />
(TL), defined as the time between the injection <strong>of</strong> the<br />
product and the beginning <strong>of</strong> contrast uptake, and Tmax.<br />
From a mathematical point <strong>of</strong> view, TL corresponded to<br />
the time at the intersection between y=V0 and the tangent<br />
at Tmax/2. The AUC, AUWI and AUWO corresponded to<br />
the area under the curve, the area under the wash-in (from<br />
T0 to Tmax) and the area under the wash-out (from Tmax to<br />
Tend corresponding to the end <strong>of</strong> the acquisition) <strong>of</strong> the<br />
TIC. The area calculations were based on the trapezoidal<br />
rule: the region under the graph <strong>of</strong> the fitted curve was<br />
approximated by trapezoids whose areas were calculated<br />
to provide approximations <strong>of</strong> the areas under the curve,<br />
the wash-in or the wash-out. An additional operation <strong>of</strong><br />
subtracting the <strong>of</strong>fset on the y-axis was performed so that<br />
the total area under the curve was independent <strong>of</strong> it. The<br />
limits <strong>of</strong> integration were defined as follows:<br />
[ 0 ] , X ∈ T Tend<br />
Where T0 is the initial time. The slope coefficient <strong>of</strong><br />
the wash-in (WI) was literally defined as the slope <strong>of</strong> the<br />
tangent <strong>of</strong> the wash-in at half maximum. Finally, the<br />
full-width at half maximum (FWHM) was defined as the<br />
time interval during which the value <strong>of</strong> the intensity was<br />
higher than Vmax/2. This parameter is commonly considered<br />
as a first approximation <strong>of</strong> the mean transit time<br />
(MTT) (Figure 6) [8,26,30] . However, as the linear raw data<br />
provided by the ultrasound scanner were too noisy, ex-<br />
WJR|www.wjgnet.com<br />
B<br />
Gauthier M et al . Variability <strong>of</strong> perfusion parameters using DCE-US<br />
9.11 mm<br />
12.18 mm<br />
Linear raw data<br />
7.6<br />
C<br />
traction was performed after TIC fitting. This was based<br />
on the mathematical model developed at the IGR (Patent:<br />
WO/2008/053268 entitled “Method and system for<br />
quantification <strong>of</strong> tumoral vascularization”).<br />
p<br />
⎛ ⎞<br />
5 fps<br />
VRh5.8<br />
9.2<br />
Figure 5 In vivo. A: Experiments were conducted with nude female mice aged from 6 to 8 wk. The selected tumor model was the B16F10 melanoma cell line which<br />
is a murine skin cancer; B, C: The region <strong>of</strong> interest contained only the tumor and was drawn for each injection performed. If the image was not well defined using the<br />
harmonic mode, the B-mode image was used to correctly define the region <strong>of</strong> interest; D: As in the case <strong>of</strong> the in vitro experiments, the ultrasound scanner displayed<br />
the associated time intensity curve. This was extracted and converted through an Excel ® file so that the analysis could be performed to obtain the required perfusion<br />
parameters.<br />
MI 0.1<br />
⎛ t ⎞<br />
⎜ A + ⎜ ⎟ ⎟<br />
⎜ a2<br />
⎟<br />
I( t) = a0 + ( a1 − a0<br />
) ∗<br />
⎝ ⎠<br />
⎜ q ⎟<br />
⎜ ⎛ t ⎞<br />
B ⎟<br />
⎜<br />
+ ⎜ ⎟<br />
a ⎟<br />
⎝ ⎝ 2 ⎠ ⎠<br />
where I(t) describes the variation in the intensity <strong>of</strong><br />
contrast uptake as a function <strong>of</strong> time; a0 is the intensity<br />
before the arrival <strong>of</strong> the contrast agent; a1 is linked to<br />
the maximum value <strong>of</strong> contrast uptake; a2 is linked to the<br />
rise time to the peak intensity; p is a coefficient related to<br />
the increase in intensity; q is a coefficient related to the<br />
decrease in intensity; A and B are arbitrary parameters.<br />
The fitted curve was obtained by adjusting all the<br />
coefficients <strong>of</strong> the equation (called the IGR equation)<br />
to obtain a sum <strong>of</strong> the least-squares differences between<br />
the linear raw data and the modeled values as close to 0<br />
as possible. Equation parameters were derived through<br />
the mathematical model so that asymptotic values were<br />
properly defined. This fitting was performed using the<br />
Solver program in Excel ® . Through this modeling step, it<br />
was possible to avoid recirculation so that the conditions<br />
required to apply the time intensity method were fulfilled.<br />
Indeed, the IGR equation was used to perfectly fit the<br />
wash-in part <strong>of</strong> the curve while the wash-out part was<br />
75 March 28, 2011|Volume 3|Issue 3|
Vmax<br />
PI<br />
V0<br />
Power (a.u.)<br />
140<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
Slope coefficient <strong>of</strong> the WI<br />
0<br />
-20 0 20 40 60 80 100 120 140<br />
TL Tmax<br />
t /s<br />
TPI<br />
FWHM<br />
adjusted so that recirculation was not taken into account<br />
in the final fitted curve (Figure 7). This adjustment is <strong>of</strong>ten<br />
performed [31] to ensure that the conditions required<br />
for the time intensity method are adequately verified.<br />
Once the fitted curve was determined, the semi-quantitative<br />
perfusion parameters were derived according to their<br />
previously described definitions.<br />
Statistical analysis<br />
Intra-operator variability was measured as the coefficient<br />
<strong>of</strong> variation (CV) which is the ratio <strong>of</strong> the SD <strong>of</strong> a specific<br />
parameter to its mean. CV = SD/mean.<br />
For each set <strong>of</strong> experiments, the CV was evaluated<br />
and recorded for each <strong>of</strong> the seven semi-quantitative<br />
perfusion parameters. An overall range <strong>of</strong> variation was<br />
additionally provided in the “Results” part.<br />
WJR|www.wjgnet.com<br />
Linear raw data<br />
Fitted curve<br />
Figure 6 The graph displays an example <strong>of</strong> a time intensity curve with 4 <strong>of</strong><br />
its 7 associated perfusion parameters: the peak intensity or peak intensity<br />
(difference between Vmax and V0), the time to peak intensity or time to peak<br />
intensity (the difference between Tmax and TL), the slope coefficient <strong>of</strong> the<br />
wash-in (the slope <strong>of</strong> the tangent <strong>of</strong> the wash-in at half maximum) and the<br />
full width at half maximum or FWHM (corresponding to a first approximation<br />
<strong>of</strong> the mean transit time). The three other perfusion parameters extracted<br />
from the time intensity curve were the area under the curve, the area under the<br />
wash-in and the area under the wash-out. PI: Peak intensity; TPI: Time to peak<br />
intensity.<br />
Power (a.u.)<br />
Gauthier M et al . Variability <strong>of</strong> perfusion parameters using DCE-US<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Linear raw data<br />
Fitted curve<br />
Recirculation<br />
0 20 40 60<br />
t/s<br />
Figure 7 This graph displays both a time intensity curve and its associated<br />
fitted curve. Recirculation is avoided through the modeling process so<br />
that the conditions required to apply the time intensity method are fulfilled: the<br />
Gustave Roussy Institute equation perfectly fits the wash-in part <strong>of</strong> the curve<br />
while the wash-out part is adjusted so that recirculation is not taken into account<br />
in the final fitted curve.<br />
Table 1 Single straight pipe phantom: intra-operator variability<br />
<strong>of</strong> semi-quantitative perfusion parameters following five<br />
0.02/0.05/0.08 mL bolus injections <strong>of</strong> SonoVue ®<br />
0.02 mL/<br />
CV (%)<br />
0.05 mL/<br />
CV (%)<br />
0.08 mL/<br />
CV (%)<br />
RESULTS<br />
PI TPI Slope <strong>of</strong><br />
the WI<br />
FWHM AUC AUWI AUWO<br />
6.03 9.78 9.57 6.43 9.40 9.97 11.11<br />
9.27 10.14 8.28 13.24 5.23 12.76 6.84<br />
20.87 10.10 23.52 17.43 5.87 23.72 2.94<br />
CV: Coefficient <strong>of</strong> variation; PI: Peak intensity; TPI: Time to peak intensity;<br />
FWHM: Full width at half maximum; AUC: Area under the curve; AUWI:<br />
Area under the wash-in; AUWO: Area under the wash-out.<br />
In vitro experiments<br />
Three different phantoms were tested. Acquisitions were<br />
obtained after five injections <strong>of</strong> SonoVue ® .<br />
1st phantom - Single straight pipe phantom results:<br />
Three volumes <strong>of</strong> SonoVue ® were tested: 0.02, 0.05 and<br />
0.08 mL. For each volume, five fitted TICs were obtained<br />
following the five contrast agent injections. Data analysis<br />
was performed according to the protocol detailed in the<br />
“Materials and Methods” part: semi-quantitative perfusion<br />
parameters were extracted directly from the fitted TICs and<br />
their associated CV values were evaluated. The 0.02, 0.05<br />
and 0.08 mL five injections respectively led to CV values<br />
ranging from 6.03% to 11.11%, from 5.23% to 13.24% and<br />
from 2.94% to 23.72%. Table 1 shows perfusion parameter<br />
CV values obtained following each set <strong>of</strong> experiments.<br />
2nd phantom - Three intertwined pipe phantom results:<br />
The five fitted TICs resulting from the series <strong>of</strong> 0.03 and<br />
0.06 mL bolus injections <strong>of</strong> SonoVue ® were analyzed using<br />
the IGR model. Intra-operator variability values were<br />
found to respectively range from 2.33% to 9.65% and<br />
from 6.12% to 11.62%. CV values associated with each<br />
perfusion parameter are shown in Table 2.<br />
For both these phantoms, maximum CV values were<br />
found in correspondence with the highest injected dose<br />
<strong>of</strong> SonoVue ® . This observation might impact on the linear<br />
assumption. However, as previously mentioned in the<br />
“Time Intensity Method” part, to transfer in vitro results<br />
into clinical context, the concentration <strong>of</strong> interest is the<br />
IGR one which remains in the linear range.<br />
3rd phantom - Dialyzer results: Data analysis was performed<br />
following five 0.10 mL bolus injections <strong>of</strong> SonoVue<br />
® . This series <strong>of</strong> experiments led to intra-operator<br />
variability values ranging from 8.11% to 19.11%. Table 3<br />
provides more detailed results associated with each evaluated<br />
semi-quantitative perfusion parameter.<br />
In vivo experiments<br />
Intra-operator variability studies were performed on five<br />
76 March 28, 2011|Volume 3|Issue 3|
Variability (%)<br />
Variability (%)<br />
30<br />
20<br />
10<br />
0<br />
30<br />
20<br />
10<br />
0<br />
Table 2 Three intertwined pipe phantom: intra-operator variability<br />
<strong>of</strong> semi-quantitative perfusion parameters following<br />
five 0.03/0.06 mL bolus injections <strong>of</strong> SonoVue ®<br />
0.03 mL/<br />
CV (%)<br />
0.06 mL/<br />
CV (%)<br />
PI<br />
FWMH<br />
PI TPI Slope <strong>of</strong><br />
the WI<br />
mice following three 0.02 mL, 0.05 mL or 0.1 mL bolus<br />
injections <strong>of</strong> SonoVue ® . Experiments were performed<br />
over 5 d.<br />
Chemical anesthesia: Four mice underwent chemical<br />
anesthesia. The body weight was found to be 23.5 g (min:<br />
22.6 g; max: 25 g) throughout the experiments. As experiments<br />
lasted over 5 d and due to the rapid doubling time<br />
<strong>of</strong> melanoma cells [32-34] , tumor volume ranged from 93.8<br />
to 599.7 mm 3 with a mean tumor value <strong>of</strong> 339.39 mm 3 . We<br />
calculated the semi-quantitative perfusion parameters directly<br />
from the TICs using the IGR mathematical model.<br />
CV values ranged from 1.48% to 29.97%. Table 4 shows<br />
variability values associated with each perfusion parameter<br />
for each mouse.<br />
Gaseous anesthesia: One mouse underwent gaseous<br />
anesthesia. It weighed 24.6 g. The tumor volume was<br />
503.56 mm 3 . CV values were determined based on the<br />
fitted TICs and ranged from 1.90% to 24.96%. More detailed<br />
results are provided in Table 4.<br />
WJR|www.wjgnet.com<br />
FWHM AUC AUWI AUWO<br />
3.16 7.69 9.65 5.56 2.33 8.55 5.32<br />
7.85 8.60 11.62 7.53 6.73 9.52 6.12<br />
CV: Coefficient <strong>of</strong> variation; PI: Peak intensity; TPI: Time to peak intensity;<br />
FWHM: Full width at half maximum; AUC: Area under the curve; AUWI:<br />
Area under the wash-in; AUWO: Area under the wash-out.<br />
Variability (%)<br />
Variability (%)<br />
30<br />
20<br />
10<br />
0<br />
30<br />
20<br />
10<br />
0<br />
TPI<br />
AUC<br />
Gauthier M et al . Variability <strong>of</strong> perfusion parameters using DCE-US<br />
Variability (%)<br />
30<br />
20<br />
10<br />
0<br />
Table 3 Dialyzer: intra-operator variability <strong>of</strong> semi-quantitative<br />
perfusion parameters following five 0.10 mL bolus injections<br />
<strong>of</strong> SonoVue ®<br />
0.10 mL/<br />
CV (%)<br />
Slope to PI<br />
PI TPI Slope <strong>of</strong><br />
the WI<br />
Single pipe: 0.02 mL SonoVue ®<br />
Single pipe: 0.05 mL SonoVue ®<br />
Single pipe: 0.08 mL SonoVue ®<br />
Three pipes: 0.03 mL SonoVue ®<br />
Three pipes: 0.06 mL SonoVue ®<br />
Dialyser: 0.10 mL SonoVue ®<br />
Mouse 1: 0.10 mL SonoVue ®<br />
Mouse 2: 0.05 mL SonoVue ®<br />
Mouse 3: 0.02 mL SonoVue ®<br />
Mouse 4: 0.10 mL SonoVue ®<br />
Mouse 5: 0.10 mL SonoVue ®<br />
Figure 8 This graph shows the variability <strong>of</strong> perfusion parameters involved in both the in vitro and in vivo experiments. Five injections were recorded for<br />
each <strong>of</strong> the three phantoms and three for each mouse. The results demonstrated less than 30% overall variability, whatever the perfusion parameter. CV: Coefficient<br />
<strong>of</strong> variation; PI: Peak intensity; TPI: Time to peak intensity; FWHM: Full width at half maximum; AUC: Area under the curve; AUWI: Area under the wash-in; AUWO:<br />
Area under the wash-out.<br />
Variability (%)<br />
30<br />
20<br />
10<br />
0<br />
AUWI<br />
FWHM AUC AUWI AUWO<br />
9.66 8.11 10.27 19.11 9.31 13.89 13.36<br />
CV: Coefficient <strong>of</strong> variation; PI: Peak intensity; TPI: Time to peak intensity;<br />
FWHM: Full width at half maximum; AUC: Area under the curve; AUWI:<br />
Area under the wash-in; AUWO: Area under the wash-out.<br />
DISCUSSION<br />
In this study, intra-operator variability was assessed through<br />
the determination <strong>of</strong> the coefficients <strong>of</strong> variation <strong>of</strong> semiquantitative<br />
perfusion parameters using three distinct<br />
phantoms as well as in vivo. Throughout the experiments,<br />
CV values were consistently lower than 30% (Figure 8).<br />
The area under the curve and the area under the wash-out<br />
exhibited CV values below 15.79% both in vitro and in vivo.<br />
Sources <strong>of</strong> variability<br />
For each set <strong>of</strong> experiments, conditions such as the probe,<br />
the phantom, the whole circuit and the settings <strong>of</strong> the ultrasound<br />
scanner were maintained unchanged so that the<br />
assembly remained identical throughout the acquisitions.<br />
The first source <strong>of</strong> variation could come from the ultrasound<br />
contrast agent itself. Indeed, before each injection, SonoVue<br />
® was reconstituted by manual agitation. Consequently,<br />
the solution may not have been identically homogeneous<br />
throughout the experiments. In addition, the precision <strong>of</strong><br />
the syringe used to administer SonoVue ® (within 0.01 mL)<br />
was low compared to the injected doses. Consequently,<br />
variations may have occurred even prior to any acquisition.<br />
77 March 28, 2011|Volume 3|Issue 3|<br />
Variability (%)<br />
30<br />
20<br />
10<br />
0<br />
AUWO
Gauthier M et al . Variability <strong>of</strong> perfusion parameters using DCE-US<br />
Table 4 In vivo studies: intra-operator variability <strong>of</strong> semi-quantitative perfusion parameters following three 0.02/0.05/0.1 mL bolus<br />
injections <strong>of</strong> SonoVue ®<br />
0.02 mL/<br />
0.05 mL/<br />
0.1 mL/<br />
CV (%)<br />
The second source <strong>of</strong> variation could come from the<br />
injection step. Manual injections were performed by the<br />
same operator and a mark was drawn on the injection<br />
site so that the same site was used throughout the experiment.<br />
A new syringe was used for each injection. However,<br />
even if the mark allowed us to maintain the same<br />
injection site, it did not provide information concerning<br />
the exact position <strong>of</strong> the syringe within the pipe. In addition,<br />
even though the injection was administered by<br />
the same operator, variations could have occurred as it<br />
was performed manually (rate or angle <strong>of</strong> the injection).<br />
Other errors may have affected the data analysis part.<br />
A region <strong>of</strong> interest had to be selected to compute the<br />
TICs. It had to be the same for all TICs. However, as a<br />
new ROI was manually drawn for each injection, results<br />
may have been tarnished because <strong>of</strong> mistakes. Additional<br />
sources <strong>of</strong> variation can occur in vivo. Indeed, even if<br />
mice were maintained asleep, their physiological parameters<br />
were not entirely monitorable and variations may<br />
have occurred during the experiments.<br />
The next step concerned TIC fitting. To ensure that<br />
no variations could come from the solver itself, a series<br />
<strong>of</strong> ten fittings were performed on the same TIC. The parameters<br />
provided by the IGR mathematical model were<br />
exactly the same for all the curves which allowed us to<br />
conclude that only the first three steps mentioned above<br />
may have induced variations in the results.<br />
Study limitations<br />
First, in vitro, the fluid used was water at ambient temperature<br />
which did not exhibit the same ultrasound<br />
properties as blood [35-37] (Table 5). In addition, none <strong>of</strong><br />
the phantoms contained tissue-mimicking material [38,39] :<br />
the first two were composed <strong>of</strong> silicone pipes leading to<br />
the same remark as with the fluid: the ultrasound properties<br />
<strong>of</strong> the silicone are different from those <strong>of</strong> vessels.<br />
WJR|www.wjgnet.com<br />
Mouse PI TPI Slope <strong>of</strong> the WI FWHM AUC AUWI AUWO<br />
Chemical anaesthesia 1 18.99 14.04 23.85 28.87 15.79 18.43 15.46<br />
2 27.60 8.33 25.75 18.90 9.06 28.39 8.12<br />
3 11.39 4.41 1.48 18.44 10.76 14.73 13.58<br />
4 27.88 5.68 28.82 29.97 11.21 26.22 12.42<br />
Gaseous anaesthesia 5 1.90 17.63 10.09 24.96 12.32 12.43 12.79<br />
CV: Coefficient <strong>of</strong> variation; PI: Peak intensity; TPI: Time to peak intensity; FWHM: Full width at half maximum; AUC: Area under the curve; AUWI: Area<br />
under the wash-in; AUWO: Area under the wash-out.<br />
Table 5 Acoustic properties <strong>of</strong> different media<br />
Density<br />
(kg/m 3 )<br />
Velocity<br />
(m/s)<br />
Attenuation coefficient<br />
(dB/cm at 1 MHz)<br />
Impedance<br />
(MRayl)<br />
Blood 1057 1575 0.18 1.61<br />
Water 1000 1480 0.0022 1<br />
1.51 (50℃)<br />
1 Quadratic frequency dependence <strong>of</strong> this attenuation coefficient. Sources:<br />
Hedrick et al [36] , Gupta et al [35] , Goldstein et al [37] .<br />
The properties <strong>of</strong> the third phantom were more similar<br />
to those <strong>of</strong> the microvascularization due to its dimensions.<br />
However, the parallelism with the capillaries did<br />
not reflect the complex and irregular structure <strong>of</strong> tumor<br />
microvascularization. Consequently, the three increasingly<br />
complex phantoms we worked with were mainly used for<br />
intra-operator variability evaluations and their properties<br />
tend to mimic only some in vivo properties which might<br />
induce difficulties in transferring in vitro results to in vivo<br />
ones. Moreover, in vivo, variability measures were based<br />
on three injections. Having more injections to interpret<br />
might have provided us with a better statistical analysis:<br />
this last limitation was <strong>of</strong>fset by the number <strong>of</strong> mice<br />
we worked on. Another limitation might concern the<br />
stability <strong>of</strong> the ultrasound contrast agent. Indeed, each<br />
experiment duration was less than 2 h on account <strong>of</strong><br />
the stability <strong>of</strong> SonoVue ® over time which is 6 h after its<br />
reconstitution as described by Schneider [11] . However, recent<br />
studies reported a significant incidence <strong>of</strong> spontaneous<br />
gas diffusion phenomena on temporal evolution <strong>of</strong><br />
contrast microbubble size [40-42] . In the following study, gas<br />
diffusion phenomena occurring for 2 h from initial formation<br />
<strong>of</strong> contrast agent was neglected: this assumption<br />
might impact the results. Finally, as previously mentioned,<br />
the precision <strong>of</strong> the syringe was a source <strong>of</strong> variability<br />
and the absence <strong>of</strong> any measurements performed to accurately<br />
evaluate microbubble concentration at the injection<br />
time might be a limitation.<br />
Intra-operator variability studies using MRI, CT, PET and<br />
US<br />
Several intra-operator variability studies using MRI, CT<br />
and PET have been described in the literature. These reported<br />
an overall intra-observer variability ranging from<br />
3% to 30% [43-50] . The ranges <strong>of</strong> the semi-quantitative<br />
perfusion parameters we evaluated were consistent with<br />
those reported in the literature. Evelhoch et al [45] analyzed<br />
CV for the initial area under the gadolinium diethylenetriaminepentaacetate<br />
uptake vs time curve (IAUC) in 19 patients<br />
examined with two scans. The CV was found to be<br />
18%. Wells et al [47] evaluated regional flow and the volume<br />
<strong>of</strong> tissue distribution <strong>of</strong> the contrast agent in tumor and<br />
normal tissue in 5 patients who underwent two PET-CT<br />
using inhaled C 15 O2 1 wk apart. They obtained CV values<br />
ranging from 9% to 14% (11% in the tumor) for the flow<br />
and from 3% to 13% (6% in the tumor) for the volume<br />
78 March 28, 2011|Volume 3|Issue 3|
distribution. Myocardial perfusion values using CT imaging<br />
were determined by Groves et al [49] using two different<br />
approaches: the maximum-slope method and the peak<br />
method. CV values ranging from 12.6% to 23.7% for<br />
intra-observer agreement were observed. No published<br />
studies on intra-operator variability using DCE-US were<br />
found in the literature. Our results are concordant with<br />
these previous findings since the overall intra-operator<br />
variability <strong>of</strong> the semi-quantitative parameters observed<br />
both in vivo and in vitro ranged from 1.48% to 29.97%.<br />
Anti-angiogenesis therapies and DCE-US imaging<br />
Anti-angiogenic treatments inhibit the formation <strong>of</strong> neoblood<br />
vessels in tumors obstructing their dissemination<br />
because <strong>of</strong> the lack <strong>of</strong> a blood supply. Such drugs exert<br />
activity primarily on the microvascularization: they may<br />
be effective even if no obvious change in tumor shape<br />
is observed after their administration. In order for functional<br />
imaging to be efficient in assessing such treatments,<br />
the variability <strong>of</strong> any semi-quantitative perfusion parameters<br />
should be lower than any reduction in perfusion.<br />
Thomas et al [51] found a decrease <strong>of</strong> 40% in AUC values,<br />
using DCE-MRI, at day 28 in 43 patients suffering from<br />
advanced cancers (24 colorectal, 1 breast, 2 mesothelioma,<br />
6 neuroendocrine, 2 renal and 8 others) and who received<br />
single-agent PTK/ZK. Other studies demonstrated that<br />
reductions in perfusion following anti-angiogenesis treatments,<br />
using MRI, CT, PET or US, range from 30% to<br />
greater than 90% [26,52-55] . For example, Lavisse et al [26] studied<br />
the evolution <strong>of</strong> the peak intensity (PI), the TPI and<br />
the FWHM after the administration <strong>of</strong> AVE8062. They<br />
found that 6 h after the injection, the PI value represented<br />
7% <strong>of</strong> the initial PI, TPI was three-fold higher than the initial<br />
TPI and FHWM was twice the initial FWHM.<br />
In the light <strong>of</strong> these data, the CV values found in<br />
the current DCE-US study justified its use as an imaging<br />
method for assessing anti-angiogenic treatments.<br />
In addition, in this study, the AUC and AUWO exhibited<br />
both in vitro and in vivo CV values below 15.79%.<br />
This is a major result considering the previous findings<br />
reported by Lassau et al [22,56,57] in different types <strong>of</strong> tumors<br />
such as GIST or RCC: among the seven semi-quantitative<br />
perfusion parameters evaluated, the two parameters which<br />
always correlated with the RECIST response and overall<br />
survival were the AUC and the AUWO. These two complementary<br />
observations highlight the reliability <strong>of</strong> such<br />
parameters in assessing anti-angiogenic treatments: AUC<br />
and AUWO are associated to a good correlation to RE-<br />
CIST response as well as to low intra-operator variability<br />
values. The TPI may also be considered a parameter <strong>of</strong> interest<br />
as it exhibited CV values in a range noticeably similar<br />
to AUC and AUWO: it ranged from 4.41% to 17.63%.<br />
Dynamic T1-weighted MRI and CT are commonly<br />
used in assessing tumor angiogenesis as DCE-US suffers<br />
from some limitations. One <strong>of</strong> its major drawbacks<br />
is its operator dependence. In addition, CV values might<br />
depend on the organ as some can be more challenging<br />
to image such as the liver suffering from respiration artifacts.<br />
There is also a limited depth penetration making<br />
imaging <strong>of</strong> deepest regions difficult [50,58] . Finally, some<br />
WJR|www.wjgnet.com<br />
Gauthier M et al . Variability <strong>of</strong> perfusion parameters using DCE-US<br />
anti-angiogenic treatments mainly involve change in tumor<br />
vasculature permeability without tumor flow. Consequently,<br />
as ultrasound contrast agents are purely intravascular,<br />
DCE-US can only provide tumor blood flow<br />
information: no information concerning tumor permeability<br />
can be determined [50] .<br />
On the other hand, further studies involving intraoperator<br />
variability might support DCE-US as the imaging<br />
method <strong>of</strong> choice for the early evaluation <strong>of</strong> antiangiogenic<br />
drugs because it also has many additional<br />
specific advantages. Contrast agents used in DCE-MRI<br />
are extracellular ones and no linear relationship exists,<br />
whatever the dose between the measured signal and the<br />
concentration <strong>of</strong> the MRI contrast agents [50] . DCE-US<br />
involves working with purely intravascular contrast agents.<br />
In addition, within a certain range, the measured intensity<br />
exhibits a linear relationship with microbubble concentration<br />
making it possible to assess perfusion parameters. In<br />
spite <strong>of</strong> the advantage <strong>of</strong> a linear relationship between<br />
the change in CT intensity and the concentration <strong>of</strong> the<br />
contrast agent as well as a high spatial resolution, DCE-<br />
CT has a low sensitivity and high concentrations <strong>of</strong> contrast<br />
agent can be toxic [50] . PET and SPECT modalities<br />
are highly sensitive to very low tracer concentrations but<br />
exhibit a poor resolution [50] compared to that <strong>of</strong> DCE-US.<br />
In addition DCE-US has advantages linked to ultrasound<br />
imaging: it is non-invasive, easy to use, not expensive,<br />
rapid and widely available.<br />
Further studies<br />
In this study, intra-operator variability measurements<br />
were based on semi-quantitative parameters, i.e. parameters<br />
extracted from the measured TIC within phantoms<br />
or tumors. Such parameters are <strong>of</strong>ten determined to<br />
estimate physiological parameters but do not take into account<br />
variations linked to physiological effects [31] . Blood<br />
flow and blood volume could be determined using methods<br />
that take into account patient hemodynamic conditions<br />
as well as the way the contrast agent is injected [31]<br />
which are elements included in the arterial input function.<br />
Consequently, further studies including the arterial input<br />
function will have to be performed to determine its influence<br />
on the DCE-US technique.<br />
This work performed using in vitro and in vivo models<br />
demonstrated that among the seven semi-quantitative<br />
perfusion parameters, two (the AUC and the AUWO)<br />
linked to the blood volume and blood flow [9,10] exhibited<br />
an intra-operator variability value below 15.79% and<br />
could be the most reliable for early evaluation <strong>of</strong> antiangiogenic<br />
treatments.<br />
ACKNOWLEDGMENTS<br />
The authors thank Lorna Saint Ange for editing.<br />
COMMENTS<br />
Background<br />
Early functional imaging <strong>of</strong> anti-angiogenesis treatments in oncology is <strong>of</strong> major<br />
importance. Dynamic contrast-enhanced ultrasonography (DCE-US) is now<br />
79 March 28, 2011|Volume 3|Issue 3|
Gauthier M et al . Variability <strong>of</strong> perfusion parameters using DCE-US<br />
commonly recognized as a functional imaging technique able to evaluate such<br />
therapies as it is a sensitive and highly available modality allowing early prediction<br />
<strong>of</strong> tumor response to treatments based on changes in vascularity before<br />
any morphological ones occur.<br />
Research frontiers<br />
Microbubble contrast agents for DCE-US have developed during the past 10 years<br />
and are currently approved in Europe, Asia and Canada. Nowadays, ultrasound<br />
provides an ideal imaging modality for angiogenesis: it is widely available, not<br />
ionizing, low cost and provides real time imaging. However, until now, information<br />
on intra-operator variability in perfusion parameter measurements performed<br />
using DCE-US is lacking. In this study, the authors evaluated such variability and<br />
highlighted values similar to previous findings using other imaging modalities.<br />
Innovations and breakthroughs<br />
DCE-US is supported by the French National Cancer Institute which is currently<br />
studying the technique in several pathologies to establish the optimal perfusion<br />
parameters and timing for quantitative anticancer efficacy assessments: currently<br />
400 patients with 1096 DCE-US demonstrated that the area under the<br />
curve quantified at 1 mo could be a robust parameter to predict response at<br />
6 mo. The following study is the first one analyzing intra-operator variability in<br />
perfusion parameter measurements performed using DCE-US. Our study would<br />
suggest that DCE-US technique has comparable intra-operator variability than<br />
other functional imaging modalities that are currently used in routine.<br />
Applications<br />
By evaluating intra-operator variability in perfusion parameter measurements<br />
performed using DCE-US, this study may confirm the interest <strong>of</strong> dynamic<br />
contrast enhanced-ultrasonography as functional imaging in anti-angiogenic<br />
therapy evaluations.<br />
Terminology<br />
DCE-US involves the use <strong>of</strong> microbubble contrast agents and specialized imaging<br />
techniques to evaluate blood flow and tissue perfusion. Intra-operator variability<br />
studies aim to determine the variation in measurements performed by a<br />
single operator and instrument on the same item and under the same conditions.<br />
Peer review<br />
This is an interesting study and may draw the readers’ attention because the<br />
authors evaluated the feasibility and reproducibility <strong>of</strong> DCE-US through in vitro<br />
and in vivo. Moreover, I think that this study would guide the readers about the<br />
methods <strong>of</strong> basic research in the areas <strong>of</strong> radiology. Unfortunately, strength <strong>of</strong><br />
reported findings is limited by some experimental constraints and manuscript<br />
presentation needs several improvements before publication.<br />
REFERENCES<br />
1 Lanza GM, Caruthers SD, Winter PM, Hughes MS, Schmieder<br />
AH, Hu G, Wickline SA. Angiogenesis imaging with<br />
vascular-constrained particles: the why and how. Eur J Nucl<br />
Med Mol Imaging 2010; 37 Suppl 1: S114-S126<br />
2 Eisenbrey JR, Forsberg F. Contrast-enhanced ultrasound for<br />
molecular imaging <strong>of</strong> angiogenesis. Eur J Nucl Med Mol Imaging<br />
2010; 37 Suppl 1: S138-S146<br />
3 Kalva SP, Namasivayam S, Vasuedo Sahani D. Imaging<br />
Angiogenesis. In: Teicher BA, Ellis LM, editors. Cancer Drug<br />
Discovery and Development: Antiangiogenic Agents in Cancer<br />
Therapy. Totowa, NJ: Humana Press, 2008: 189-203<br />
4 Lassau N, Chami L, Péronneau P. Imagerie de contraste ultrasonore<br />
pour l’évaluation précoce des thérapeutiques ciblées.<br />
In: Tranquart F, Correas JM, Bouakaz A, editors. Echographie<br />
de contraste. Paris: Springer, 2007: 81-86<br />
5 Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan<br />
RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom<br />
AT, Christian MC, Gwyther SG. New guidelines to evaluate<br />
the response to treatment in solid tumors. European Organization<br />
for Research and Treatment <strong>of</strong> Cancer, National Cancer<br />
Institute <strong>of</strong> the United States, National Cancer Institute <strong>of</strong><br />
Canada. J Natl Cancer Inst 2000; 92: 205-216<br />
6 Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D,<br />
Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein<br />
L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J. New<br />
response evaluation criteria in solid tumours: revised RECIST<br />
guideline (version 1.1). Eur J Cancer 2009; 45: 228-247<br />
7 Quaia E. Microbubble ultrasound contrast agents: an update.<br />
WJR|www.wjgnet.com<br />
Eur Radiol 2007; 17: 1995-2008<br />
8 Ignee A, Jedrejczyk M, Schuessler G, Jakubowski W, Dietrich<br />
CF. Quantitative contrast enhanced ultrasound <strong>of</strong> the liver<br />
for time intensity curves-Reliability and potential sources <strong>of</strong><br />
errors. Eur J Radiol 2010; 73: 153-158<br />
9 Claassen L, Seidel G, Algermissen C. Quantification <strong>of</strong> flow<br />
rates using harmonic grey-scale imaging and an ultrasound<br />
contrast agent: an in vitro and in vivo study. Ultrasound Med<br />
Biol 2001; 27: 83-88<br />
10 Schwarz KQ, Bezante GP, Chen X, Mottley JG, Schlief R. Volumetric<br />
arterial flow quantification using echo contrast. An in<br />
vitro comparison <strong>of</strong> three ultrasonic intensity methods: radio<br />
frequency, video and Doppler. Ultrasound Med Biol 1993; 19:<br />
447-460<br />
11 Schneider M. Characteristics <strong>of</strong> SonoVuetrade mark. Echocardiography<br />
1999; 16: 743-746<br />
12 Greis C. Technology overview: SonoVue (Bracco, Milan). Eur<br />
Radiol 2004; 14 Suppl 8: P11-P15<br />
13 Quaia E, Calliada F, Bertolotto M, Rossi S, Garioni L, Rosa L,<br />
Pozzi-Mucelli R. Characterization <strong>of</strong> focal liver lesions with<br />
contrast-specific US modes and a sulfur hexafluoride-filled<br />
microbubble contrast agent: diagnostic performance and confidence.<br />
Radiology 2004; 232: 420-430<br />
14 von Herbay A, Vogt C, Willers R, Häussinger D. Real-time<br />
imaging with the sonographic contrast agent SonoVue: differentiation<br />
between benign and malignant hepatic lesions. J<br />
Ultrasound Med 2004; 23: 1557-1568<br />
15 Hamilton WF, Moore JW, Kinsman MJ, Spurling RG. Studies<br />
on the circulation. IV. Further analysis <strong>of</strong> the injection<br />
method, and <strong>of</strong> changes in hemodynamics under physiological<br />
and pathological conditions. Am J Physiol 1932: 99: 534-551<br />
16 Kinsman JM, Moore JW, Hamilton WF. Studies on the circulation.<br />
I. Injection method: physical and mathematical considerations.<br />
Am J Physiol 1929; 89: 322-330<br />
17 Mischi M, Del Prete Z, Korsten HHM. Indicator dilution techniques<br />
in cardiovascular quantification. In: Leondes CT, editor.<br />
Biomechanical Systems Technology: Cardiovascular Systems.<br />
Singapore: <strong>World</strong> Scientific Publishing Company, 2007: 89-156<br />
18 Li PC, Yang MJ. Transfer function analysis <strong>of</strong> ultrasonic<br />
time-intensity measurements. Ultrasound Med Biol 2003; 29:<br />
1493-1500<br />
19 Lampaskis M, Averkiou M. Investigation <strong>of</strong> the relationship<br />
<strong>of</strong> nonlinear backscattered ultrasound intensity with microbubble<br />
concentration at low MI. Ultrasound Med Biol 2010; 36:<br />
306-312<br />
20 Whittingham TA. Contrast-specific imaging techniques:<br />
technical perspective. In: Quaia E, editor. Contrast media in<br />
ultrasonography: basic principles and clinical applications.<br />
Berlin, Heidelberg, New-York: Springer, 2005: 43-70<br />
21 Lassau N, Koscielny S, Chebil M, Chami L, Bendjilali R, Roche.<br />
A, Escudier B, Le Cesne A, Soria J () Functional imaging using<br />
DCE-US: which parameters for the early evaluation <strong>of</strong> antiangiogenetic<br />
therapies? J Clin Oncol 2009; 27 (15 Suppl): 3524<br />
22 Lassau N, Koscielny S, Albiges L, Chami L, Benatsou B, Chebil<br />
M, Roche A, Escudier BJ. Metastatic renal cell carcinoma<br />
treated with sunitinib: early evaluation <strong>of</strong> treatment response<br />
using dynamic contrast-enhanced ultrasonography. Clin Cancer<br />
Res 2010; 16: 1216-1225<br />
23 Lassau N, Lacroix J, Aziza R, Vilgrain V, Taeb S, Koscielny<br />
S. French Multicentric Prospective Evaluation <strong>of</strong> Dynamic<br />
Contrast-enhanced Ultrasound (DCE-US) for the Evaluation<br />
<strong>of</strong> Antiangiogenic Treatments. Radiological Society <strong>of</strong> North<br />
America. 95th Scientific Assembly and Annual Meeting; 2009<br />
No 29-Dec 4; Mc Cormick Place, Chicago<br />
24 Veltmann C, Lohmaier S, Schlosser T, Shai S, Ehlgen A, Pohl<br />
C, Becher H, Tiemann K. On the design <strong>of</strong> a capillary flow<br />
phantom for the evaluation <strong>of</strong> ultrasound contrast agents at<br />
very low flow velocities. Ultrasound Med Biol 2002; 28: 625-634<br />
25 Meyer-Wiethe K, Cangür H, Seidel GU. Comparison <strong>of</strong> different<br />
mathematical models to analyze diminution kinetics <strong>of</strong><br />
ultrasound contrast enhancement in a flow phantom. Ultrasound<br />
Med Biol 2005; 31: 93-98<br />
80 March 28, 2011|Volume 3|Issue 3|
26 Lavisse S, Lejeune P, Rouffiac V, Elie N, Bribes E, Demers<br />
B, Vrignaud P, Bissery MC, Brulé A, Koscielny S, Péronneau<br />
P, Lassau N. Early quantitative evaluation <strong>of</strong> a tumor vasculature<br />
disruptive agent AVE8062 using dynamic contrastenhanced<br />
ultrasonography. Invest Radiol 2008; 43: 100-111<br />
27 Verbeek XA, Willigers JM, Prinzen FW, Peschar M, Ledoux<br />
LA, Hoeks AP. High-resolution functional imaging with<br />
ultrasound contrast agents based on RF processing in an in<br />
vivo kidney experiment. Ultrasound Med Biol 2001; 27: 223-233<br />
28 Correas JM, Burns PN, Lai X, Qi X. Infusion versus bolus <strong>of</strong><br />
an ultrasound contrast agent: in vivo dose-response measurements<br />
<strong>of</strong> BR1. Invest Radiol 2000; 35: 72-79<br />
29 Gorce JM, Arditi M, Schneider M. Influence <strong>of</strong> bubble size<br />
distribution on the echogenicity <strong>of</strong> ultrasound contrast<br />
agents: a study <strong>of</strong> SonoVue. Invest Radiol 2000; 35: 661-671<br />
30 Vicenzini E, Delfini R, Magri F, Puccinelli F, Altieri M, Santoro<br />
A, Giannoni MF, Bozzao L, Di Piero V, Lenzi GL. Semiquantitative<br />
human cerebral perfusion assessment with ultrasound<br />
in brain space-occupying lesions: preliminary data. J<br />
Ultrasound Med 2008; 27: 685-692<br />
31 de Marco G, Dassonvalle P, M.C. H-F, Onen F, Idy-Peretti I.<br />
Cerebral perfusion: dynamic suceptibility contrast MR imaging.<br />
Part 2: vascular models and data extraction. Med Nucl<br />
2004; 28: 35-48<br />
32 Kwee JK, Mitidieri E, Affonso OR. Lowered superoxide dismutase<br />
in highly metastatic B16 melanoma cells. Cancer Lett<br />
1991; 57: 199-202<br />
33 Ohira T, Ohe Y, Heike Y, Podack ER, Olsen KJ, Nishio K,<br />
Nishio M, Miyahara Y, Funayama Y, Ogasawara H. In vitro<br />
and in vivo growth <strong>of</strong> B16F10 melanoma cells transfected<br />
with interleukin-4 cDNA and gene therapy with the transfectant.<br />
J Cancer Res Clin Oncol 1994; 120: 631-635<br />
34 Yerlikaya A, Erin N. Differential sensitivity <strong>of</strong> breast cancer<br />
and melanoma cells to proteasome inhibitor Velcade. Int J<br />
Mol Med 2008; 22: 817-823<br />
35 Gupta LC, Sahu UC. Diagnostic ultrasound. New Delhi: Jaypee<br />
Brothers Publishers, 2007<br />
36 Hedrick W, Hykes D, Starchman D. Ultrasound physics and<br />
instrumentation. 3rd ed. Saint-Louis, MO: Mosby, 1995<br />
37 Goldstein A, Powis RL. Medical ultrasonic diagnostics. In:<br />
Papadakis P, editor. Ultrasonic instruments and devices: reference<br />
for modern instrumentation, techniques, and technology.<br />
San Diego, CA: Academic Press, 1999: 46-193<br />
38 Casciaro S, Demitri C, Conversano F, Casciaro E, Distante A.<br />
Experimental investigation and theoretical modelling <strong>of</strong> the<br />
nonlinear acoustical behaviour <strong>of</strong> a liver tissue and comparison<br />
with a tissue mimicking hydrogel. J Mater Sci Mater Med<br />
2008; 19: 899-906<br />
39 Casciaro S, Conversano F, Musio S, Casciaro E, Demitri C,<br />
Sannino A. Full experimental modelling <strong>of</strong> a liver tissue mimicking<br />
phantom for medical ultrasound studies employing<br />
different hydrogels. J Mater Sci Mater Med 2009; 20: 983-989<br />
40 Sarkar K, Katiyar A, Jain P. Growth and dissolution <strong>of</strong> an<br />
encapsulated contrast microbubble: effects <strong>of</strong> encapsulation<br />
permeability. Ultrasound Med Biol 2009; 35: 1385-1396<br />
41 Kwan JJ, Borden MA. Microbubble dissolution in a multigas<br />
environment. Langmuir 2010; 26: 6542-6548<br />
42 Casciaro S, Errico RP, Conversano F, Demitri C, Distante A.<br />
Experimental investigations <strong>of</strong> nonlinearities and destruction<br />
mechanisms <strong>of</strong> an experimental phospholipid-based ultrasound<br />
contrast agent. Invest Radiol 2007; 42: 95-104<br />
43 Ng CS, Raunig DL, Jackson EF, Ashton EA, Kelcz F, Kim<br />
KB, Kurzrock R, McShane TM. Reproducibility <strong>of</strong> perfusion<br />
parameters in dynamic contrast-enhanced MRI <strong>of</strong> lung and<br />
liver tumors: effect on estimates <strong>of</strong> patient sample size in<br />
clinical trials and on individual patient responses. AJR Am J<br />
Roentgenol 2010; 194: W134-W140<br />
44 Marcus CD, Ladam-Marcus V, Cucu C, Bouché O, Lucas L,<br />
WJR|www.wjgnet.com<br />
Gauthier M et al . Variability <strong>of</strong> perfusion parameters using DCE-US<br />
Hoeffel C. Imaging techniques to evaluate the response to<br />
treatment in oncology: current standards and perspectives.<br />
Crit Rev Oncol Hematol 2009; 72: 217-238<br />
45 Evelhoch JL, LoRusso PM, He Z, DelProposto Z, Polin L,<br />
Corbett TH, Langmuir P, Wheeler C, Stone A, Leadbetter J,<br />
Ryan AJ, Blakey DC, Waterton JC. Magnetic resonance imaging<br />
measurements <strong>of</strong> the response <strong>of</strong> murine and human tumors<br />
to the vascular-targeting agent ZD6126. Clin Cancer Res<br />
2004; 10: 3650-3657<br />
46 Morgan B, Utting JF, Higginson A, Thomas AL, Steward WP,<br />
Horsfield MA. A simple, reproducible method for monitoring<br />
the treatment <strong>of</strong> tumours using dynamic contrast-enhanced<br />
MR imaging. Br J Cancer 2006; 94: 1420-1427<br />
47 Wells P, Jones T, Price P. Assessment <strong>of</strong> inter- and intrapatient<br />
variability in C15O2 positron emission tomography<br />
measurements <strong>of</strong> blood flow in patients with intra-abdominal<br />
cancers. Clin Cancer Res 2003; 9: 6350-6356<br />
48 Cenic A, Nabavi DG, Craen RA, Gelb AW, Lee TY. Dynamic<br />
CT measurement <strong>of</strong> cerebral blood flow: a validation study.<br />
AJNR Am J Neuroradiol 1999; 20: 63-73<br />
49 Groves AM, Goh V, Rajasekharan S, Kayani I, Endozo R,<br />
Dickson JC, Menezes LJ, Shastry M, Habib SB, Ell PJ, Hutton<br />
BF. CT coronary angiography: quantitative assessment <strong>of</strong><br />
myocardial perfusion using test bolus data-initial experience.<br />
Eur Radiol 2008; 18: 2155-2163<br />
50 Miller JC, Pien HH, Sahani D, Sorensen AG, Thrall JH. Imaging<br />
angiogenesis: applications and potential for drug development.<br />
J Natl Cancer Inst 2005; 97: 172-187<br />
51 Thomas AL, Morgan B, Horsfield MA, Higginson A, Kay A,<br />
Lee L, Masson E, Puccio-Pick M, Laurent D, Steward WP.<br />
Phase I study <strong>of</strong> the safety, tolerability, pharmacokinetics,<br />
and pharmacodynamics <strong>of</strong> PTK787/ZK 222584 administered<br />
twice daily in patients with advanced cancer. J Clin Oncol<br />
2005; 23: 4162-4171<br />
52 Willett CG, Boucher Y, di Tomaso E, Duda DG, Munn LL,<br />
Tong RT, Chung DC, Sahani DV, Kalva SP, Kozin SV, Mino<br />
M, Cohen KS, Scadden DT, Hartford AC, Fischman AJ, Clark<br />
JW, Ryan DP, Zhu AX, Blaszkowsky LS, Chen HX, Shellito<br />
PC, Lauwers GY, Jain RK. Direct evidence that the VEGFspecific<br />
antibody bevacizumab has antivascular effects in human<br />
rectal cancer. Nat Med 2004; 10: 145-147<br />
53 Meijerink MR, van Cruijsen H, Hoekman K, Kater M, van<br />
Schaik C, van Waesberghe JH, Giaccone G, Manoliu RA. The<br />
use <strong>of</strong> perfusion CT for the evaluation <strong>of</strong> therapy combining<br />
AZD2171 with gefitinib in cancer patients. Eur Radiol 2007;<br />
17: 1700-1713<br />
54 Lassau N, Lamuraglia M, Vanel D, Le Cesne A, Chami L,<br />
Jaziri S, Terrier P, Roche A, Leclere J, Bonvalot S. Doppler US<br />
with perfusion s<strong>of</strong>tware and contrast medium injection in the<br />
early evaluation <strong>of</strong> isolated limb perfusion <strong>of</strong> limb sarcomas:<br />
prospective study <strong>of</strong> 49 cases. Ann Oncol 2005; 16: 1054-1060<br />
55 Miles KA, Griffiths MR. Perfusion CT: a worthwhile enhancement?<br />
Br J Radiol 2003; 76: 220-231<br />
56 Lassau N, Chebil M, Koscielny S, Chami L, Bendjilali R, Roche<br />
A. Dynamic Contrast-enhanced Ultrasonography (DCE-US)<br />
with Quantification for the Early Evaluation <strong>of</strong> HCC Treated<br />
by Bevacizumab: Which Parameters? Radiological Society <strong>of</strong><br />
North America. 95th Scientific Assembly and Annual Meeting;<br />
2009 Nov 29-Dec 4; Chicago: Mc Cormick Place<br />
57 Lassau N, Chebil M, Chami L, Bidault S, Girard E, Roche A.<br />
Dynamic contrast-enhanced ultrasonography (DCE-US): a<br />
new tool for the early evaluation <strong>of</strong> antiangiogenic treatment.<br />
Target Oncol 2010; 5: 53-58<br />
58 Quaia E, D'On<strong>of</strong>rio M, Palumbo A, Rossi S, Bruni S, Cova<br />
M. Comparison <strong>of</strong> contrast-enhanced ultrasonography versus<br />
baseline ultrasound and contrast-enhanced computed<br />
tomography in metastatic disease <strong>of</strong> the liver: diagnostic performance<br />
and confidence. Eur Radiol 2006; 16: 1599-1609<br />
S- Editor Cheng JX L- Editor O’Neill M E- Editor Zheng XM<br />
81 March 28, 2011|Volume 3|Issue 3|
W J R<br />
Online Submissions: http://www.wjgnet.com/1949-8470<strong>of</strong>fice<br />
wjr@wjgnet.com<br />
doi:10.4329/wjr.v3.i3.82<br />
Paraparesis induced by extramedullary haematopoiesis<br />
Paolo Savini, Arianna Lanzi, Giorgio Marano, Chiara Carli Moretti, Giovanni Poletti, Giuseppe Musardo,<br />
Francesco Giuseppe Foschi, Giuseppe Francesco Stefanini<br />
Paolo Savini, Arianna Lanzi, Giorgio Marano, Giuseppe<br />
Musardo, Francesco Giuseppe Foschi, Giuseppe Francesco<br />
Stefanini, Department <strong>of</strong> Internal Medicine, Faenza Hospital,<br />
viale Stradone 9, 48018 Faenza, Italy<br />
Chiara Carli Moretti, Department <strong>of</strong> Radiology, Faenza Hospital,<br />
viale Stradone 9, 48018 Faenza, Italy<br />
Giovanni Poletti, Department <strong>of</strong> Pathology, Ravenna Hospital,<br />
viale Randi 5, 48121 Ravenna, Italy<br />
Author contributions: Savini P refer to physician <strong>of</strong> the clinical<br />
case; Lanzi A and Marano G contributes to writing the manuscript;<br />
Carli Moretti C provided radiologic images <strong>of</strong> the case;<br />
Poletti performed laboratory analysis; Musardo G and Foschi FG<br />
screened the literature and contributed to writing the first draft <strong>of</strong><br />
the paper; Stefanini GF was responsible for the final approval <strong>of</strong><br />
the manuscript.<br />
Correspondence to: Paolo Savini, MD, Department <strong>of</strong> Internal<br />
Medicine, Faenza Hospital, viale Stradone 9, 48018 Faenza,<br />
Italy. p.savini@ausl.ra.it<br />
Telephone: +39-546-601111 Fax: +39-546-601517<br />
Received: November 13, 2010 Revised: January 10, 2011<br />
Accepted: January 17, 2011<br />
Published online: March 28, 2011<br />
Abstract<br />
We describe a case <strong>of</strong> worsening paraparesis induced<br />
by spinal cord compression at T6-T7 levels associated<br />
with compensatory extramedullary haematopoiesis from<br />
a compound heterozygote for haemoglobin E and for<br />
β-thalassemia. An emergency T3-T9 laminectomy was<br />
performed with excision <strong>of</strong> the masses and complete<br />
rehabilitation <strong>of</strong> the patient.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Extramedullary hematopoiesis; Thalassemia;<br />
Anemia; Spinal cord compression; Laminectomy<br />
Peer reviewers: Yi-Xiang Wang, MMed, PhD, Associate Pr<strong>of</strong>essor,<br />
Department <strong>of</strong> Diagnostic Radiology and Organ Imaging,<br />
Prince <strong>of</strong> Wales Hospital, The Chinese University <strong>of</strong> Hong Kong,<br />
Shatin, NT, Hong Kong, China; Kennith F Layton, MD, FAHA,<br />
Division <strong>of</strong> Neuroradiology and Director <strong>of</strong> Interventional Neu-<br />
WJR|www.wjgnet.com<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Radiology<br />
roradiology, Department <strong>of</strong> Radiology, Baylor University Medical<br />
Center, 3500 Gaston Avenue, Dallas, TX 75246, United States<br />
Savini P, Lanzi A, Marano G, Moretti CC, Poletti G, Musardo G,<br />
Foschi FG, Stefanini GF. Paraparesis induced by extramedullary<br />
haematopoiesis. <strong>World</strong> J Radiol 2011; 3(3): 82-84 Available<br />
from: URL: http://www.wjgnet.com/1949-8470/full/v3/i3/<br />
82.htm DOI: http://dx.doi.org/10.4329/wjr.v3.i3.82<br />
INTRODUCTION<br />
Extramedullary haematopoiesis (EMH) is a physiologic response<br />
to chronic anemia, observed in various hematologic<br />
disorders such as thalassemias [1] , myel<strong>of</strong>ibrosis and polycythemia.<br />
Since the first description by Gatto et al [2] , several<br />
cases <strong>of</strong> EMH at different sites have been reported.<br />
The EMH, as a tumor-like mass, is commonly seen<br />
in the liver, spleen and lymph nodes. Involvement <strong>of</strong> the<br />
epidural space causing spinal cord compression has rarely<br />
been reported [3] .<br />
Because <strong>of</strong> its rarity, there are no evidence-based guidelines<br />
for the treatment <strong>of</strong> paraspinal pseudotumors caused<br />
by EMH. Management options include hypertransfusion,<br />
radiotherapy, surgery or a combination <strong>of</strong> these modalities.<br />
Recently, hydroxyurea or erythropoietin in combination<br />
with radiotherapy as treatment was described [4-6] , but<br />
management still remains controversial.<br />
Decompressive laminectomy, as in our case, has been<br />
used in patients with rapid neurological deterioration [7] .<br />
We hereby present a case <strong>of</strong> EMH in a 21-year-old man<br />
with thalassemia presenting with paraplegia due to a spinal<br />
cord compression that was treated successfully with surgery.<br />
CASE REPORT<br />
<strong>World</strong> J Radiol 2011 March 28; 3(3): 82-84<br />
ISSN 1949-8470 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
CASE REPORT<br />
A 21-year-old man with a not well defined history <strong>of</strong><br />
transfusion-dependent microcytic anemia in his native<br />
country, Bangladesh, presented to the emergency department<br />
with worsening paraparesis.<br />
82 March 28, 2011|Volume 3|Issue 3|
Figure 1 Pre-operative computed tomography scan <strong>of</strong> the chest without contrast<br />
media showing the large bilateral costal masses (white arrows) and an<br />
intracanalicular extradural mass (black arrow).<br />
Figure 2 Pre-operative “bone window” computed tomography scan <strong>of</strong> the<br />
chest without contrast media shows large bilateral, well circumscribed<br />
lobulated s<strong>of</strong>t tissue masses that cause widening <strong>of</strong> the ribs (short arrows)<br />
and periosteal reaction, without interruption <strong>of</strong> cortical bone (thin long<br />
arrow). Coexisting involvement <strong>of</strong> the sternum body (thick long arrow).<br />
Figure 3 Pre-operative “bone window” computed tomography scan without<br />
contrast media: the vertebral body is devoid <strong>of</strong> bony erosion and has a<br />
lacey appearance.<br />
Computed tomography (Figures 1-3) and magnetic resonance<br />
imaging (MRI, Figures 4-6) revealed bilateral paravertebral<br />
s<strong>of</strong>t-tissue masses at T4-L1 levels and a mass with<br />
the same features was seen inside the vertebral canal inducing<br />
spinal cord compression at T4-T9 levels. Furthermore,<br />
a marked medullary expansion <strong>of</strong> the bony structures was<br />
WJR|www.wjgnet.com<br />
Savini P et al . Extramedullary haematopoiesis with paraparesis<br />
Figure 4 Preoperative axial magnetic resonance imaging, T2 weighted,<br />
shows paravertebral and intracanal masses, isointense with the spinal<br />
cord, widening the ribs (short arrows) and causing cord compression (long<br />
arrow).<br />
Figure 5 Preoperative sagittal MRI, T2 weighted, shows masses extending<br />
from T4 to T9 with cord compression (white arrows), embedded within the epidural<br />
fat and isointense with the spinal cord.<br />
A<br />
Figure 6 Preoperative sagittal magnetic resonance imaging, T1 weighted,<br />
without contrast media (A) (long arrows), and after Gadolinium administration<br />
(B) (short arrows) shows poor and homogeneous contrast enhancement<br />
<strong>of</strong> the masses.<br />
present. Laboratory analyses showed a haemoglobin (Hb)<br />
level <strong>of</strong> 8.5 g/dL and mean corpuscular volume (MCV) <strong>of</strong><br />
68 fL. Hb electrophoresis revealed HbE at 45%, HbF at<br />
30% and HbA2 at 20%.<br />
Molecular analysis showed the patient was a compound<br />
heterozygote for HbE (β-26 glutamine → lysine)<br />
83 March 28, 2011|Volume 3|Issue 3|<br />
B
Savini P et al . Extramedullary haematopoiesis with paraparesis<br />
and for β-thalassemia (β+IVS1-nt5). All these findings<br />
appeared to be associated with compensatory extramedullary<br />
haematopoiesis.<br />
An emergency T3-T9 laminectomy was performed<br />
with a complete excision <strong>of</strong> the masses. A morphological<br />
and immunohistochemical analysis was then carried out.<br />
The masses were composed <strong>of</strong> a heterogeneous cellular<br />
population resembling physiological haematopoiesis in all<br />
its components.<br />
The patient received a rehabilitation cycle and five<br />
months after the surgery, with continuing red blood cell<br />
transfusions, remains free <strong>of</strong> symptoms.<br />
DISCUSSION<br />
HbE (β26Glu → Lys) is the most common Hb variant in<br />
Southeast Asia and the second most prevalent worldwide.<br />
HbE, when associated with β thalassemia (HbE/β-thalassemia)<br />
in a compound heterozygous state, results in a<br />
clinically severe condition. HbE activates a cryptic splice<br />
site that produces non-functional mRNAs. Hb IVS1-1 is<br />
a Mediterranean mutation that affects mRNA processing<br />
giving rise to β (o)-thalassemia. HbE/β thalassemia has a<br />
very variable clinical phenotype. HbE/β-thalassemia generally<br />
manifests with severe anemia where individuals exhibit<br />
β-thalassemia major with regular blood transfusions<br />
or β-thalassemia intermedia with periodic blood transfusions.<br />
Extramedullary haematopoiesis is a consequence <strong>of</strong><br />
insufficient bone marrow function that is unable to meet<br />
circulatory demands. Thalassemia major or intermedia,<br />
congenital spherocytosis, congenital haemolytic anemia<br />
and sickle cell anemia account for most cases <strong>of</strong> EMH. It<br />
is rarely seen in myel<strong>of</strong>ibrosis and Gaucher’s disease.<br />
Intrathoracic EMH is most <strong>of</strong>ten visualized on the<br />
chest roentgenogram or the chest computed tomography<br />
(CT) scan as single or multiple paravertebral mass lesions.<br />
While a paravertebral mass may represent EMH, other<br />
disorders <strong>of</strong> the posterior mediastinum, such as neurogenic<br />
tumor, lymphoma, primary and metastatic malignancy,<br />
paravertebral abscess, lateral meningocele, and<br />
extrapleural cyst, must be considered.<br />
The characteristic features observed in the chest roentgenogram<br />
and the chest CT scan were helpful in recogniz-<br />
WJR|www.wjgnet.com<br />
ing intrathoracic EMH. These included the following 8] : (1)<br />
Widening <strong>of</strong> the ribs by expansion <strong>of</strong> the medullary cavity<br />
or by periosteal elevation, without bony erosion; (2) The<br />
presence <strong>of</strong> a unilateral or bilateral well-circumscribed lobulated,<br />
paravertebral mass lesion usually located caudal to<br />
the sixth thoracic vertebrae; and (3) The absence <strong>of</strong> calcification<br />
and the presence <strong>of</strong> adipose tissue within the mass.<br />
MRI is currently the technique <strong>of</strong> choice in evaluating<br />
spinal EMH. On MRI, EMH is usually characterized by<br />
lobular masses with increased signal intensity compared to<br />
that <strong>of</strong> the red marrow in the adjacent vertebral bodies [7] .<br />
The lack <strong>of</strong> gadolinium enhancement allows its differentiation<br />
from other epidural masses such as abscesses or<br />
metastases.<br />
REFERENCES<br />
1 Cappellini MD, Musallam KM, Taher AT. Insight onto the<br />
pathophysiology and clinical complications <strong>of</strong> thalassemia<br />
intermedia. Hemoglobin 2009; 33 Suppl 1: S145-S159<br />
2 Gatto I, Terrana V, Biondi L. [Compression <strong>of</strong> the spinal cord<br />
due to proliferation <strong>of</strong> bone marrow in epidural space in a<br />
splenectomized person with Cooley's disease]. Haematologica<br />
1954; 38: 61-76<br />
3 Logothetis J, Constantoulakis M, Economidou J, Stefanis C,<br />
Hakas P, Augoustaki O, S<strong>of</strong>roniadou K, Loewenson R, Bilek<br />
M. Thalassemia major (homozygous beta-thalassemia). A<br />
survey <strong>of</strong> 138 cases with emphasis on neurologic and muscular<br />
aspects. Neurology 1972; 22: 294-304<br />
4 Cario H, Wegener M, Debatin KM, Kohne E. Treatment with<br />
hydroxyurea in thalassemia intermedia with paravertebral<br />
pseudotumors <strong>of</strong> extramedullary hematopoiesis. Ann Hematol<br />
2002; 81: 478-482<br />
5 Cianciulli P, Sorrentino F, Morino L, Massa A, Sergiacomi<br />
GL, Donato V, Amadori S. Radiotherapy combined with<br />
erythropoietin for the treatment <strong>of</strong> extramedullary hematopoiesis<br />
in an alloimmunized patient with thalassemia intermedia.<br />
Ann Hematol 1996; 72: 379-381<br />
6 Malik M, Pillai LS, Gogia N, Puri T, Mahapatra M, Sharma<br />
DN, Kumar R. Paraplegia due to extramedullary hematopoiesis<br />
in thalassemia treated successfully with radiation<br />
therapy. Haematologica 2007; 92: e28-e30<br />
7 Dibbern DA Jr, Loevner LA, Lieberman AP, Salhany KE,<br />
Freese A, Marcotte PJ. MR <strong>of</strong> thoracic cord compression<br />
caused by epidural extramedullary hematopoiesis in myelodysplastic<br />
syndrome. AJNR Am J Neuroradiol 1997; 18: 363-366<br />
8 Alam R, Padmanabhan K, Rao H. Paravertebral mass in a<br />
patient with thalassemia intermedia. Chest 1997; 112: 265-267<br />
S- Editor Cheng JX L- Editor Lutze M E- Editor Zheng XM<br />
84 March 28, 2011|Volume 3|Issue 3|
W J R<br />
Online Submissions: http://www.wjgnet.com/1949-8470<strong>of</strong>fice<br />
wjr@wjgnet.com<br />
www.wjgnet.com<br />
ACKNOWLEDGMENTS<br />
Acknowledgments to reviewers <strong>of</strong> <strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Radiology<br />
Many reviewers have contributed their expertise and time<br />
to the peer review, a critical process to ensure the quality<br />
<strong>of</strong> <strong>World</strong> <strong>Journal</strong> <strong>of</strong> Radiology. The editors and authors <strong>of</strong><br />
the articles submitted to the journal are grateful to the<br />
following reviewers for evaluating the articles (including<br />
those published in this issue and those rejected for this<br />
issue) during the last editing time period.<br />
Charles Bellows, MD, Associate Pr<strong>of</strong>essor, Chief <strong>of</strong> General<br />
Surgery, Tulane University, Department <strong>of</strong> Surgery SL-22, 1430<br />
Tulane Ave, New Orleans, LA 70112, United States<br />
Filippo Cademartiri, MD, PhD, Departmento <strong>of</strong> Radiology -<br />
c/o Piastra Tecnica - Piano 0, Azienda Ospedaliero-Universitaria di<br />
Parma, Via Gramsci, 14 - 43100 Parma, Italy<br />
Sergio Casciaro, PhD, Institute <strong>of</strong> Clinical Physiology - National<br />
Research Council,Campus Universitario Ecotekne, Via Monteroni,<br />
73100 Lecce, Italy<br />
Chan Kyo Kim, MD, Assistant Pr<strong>of</strong>essor, Department <strong>of</strong> Radiology,<br />
Samsung Medical Center, Sungkyunkwan University School <strong>of</strong><br />
Medicine, 50 Ilwon-dong, Kangnam-gu, Seoul 135-710, South Korea<br />
WJR|www.wjgnet.com<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Radiology<br />
<strong>World</strong> J Radiol 2011 March 28; 3(3): I<br />
ISSN 1949-8470 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
Stefania Romano, MD, A. Cardarelli Hospital, Department <strong>of</strong><br />
Diagnostic Imaging, Section <strong>of</strong> General and Emergency Radiology,<br />
Viale Cardarelli, 9, 80131 Naples, Italy<br />
Francesco Lassandro, MD, Department <strong>of</strong> Radiology, Monaldi<br />
Hospital, via Leonardo Bianchi, Napoli, 80129, Italy<br />
Kennith F Layton, MD, FAHA, Division <strong>of</strong> Neuroradiology<br />
and Director <strong>of</strong> Interventional Neuroradiology, Department <strong>of</strong><br />
Radiology, Baylor University Medical Center, 3500 Gaston Avenue,<br />
Dallas, TX 75246, United States<br />
Yicheng Ni, MD, PhD, Pr<strong>of</strong>essor, Biomedical Imaging, Interventional<br />
Therapy and Contrast Media Research, Department<br />
<strong>of</strong> Radiology, University Hospitals, K.U. Leuven, Herestraat 49,<br />
B-3000, Leuven, Belgium<br />
Yi-Xiang Wang, MMed, PhD, Associate Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Diagnostic Radiology and Organ Imaging, Prince <strong>of</strong><br />
Wales Hospital, The Chinese University <strong>of</strong> Hong Kong, Shatin,<br />
NT, Hong Kong, China<br />
Ying Xiao, PhD, Pr<strong>of</strong>essor, Director, Medical Physics, Department<br />
<strong>of</strong> Radiation Oncology, Thomas Jefferson University Hospital,<br />
Philadelphia, PA 19107-5097, United States<br />
I March 28, 2011|Volume 3|Issue 3|
W J R<br />
Online Submissions: http://www.wjgnet.com/1949-8470<strong>of</strong>fice<br />
wjr@wjgnet.com<br />
www.wjgnet.com<br />
Meetings<br />
Events Calendar 2011<br />
January 23-27<br />
Radiology at Snowbird<br />
San Diego, Mexico<br />
January 24-28<br />
Neuro/ENT at the Beach<br />
Palm Beach, FL, United States<br />
February 28-29<br />
MIAD 2011 - 2nd International<br />
Workshop on Medical Image<br />
Analysis and Description for<br />
Diagnosis System<br />
Rome, Italy<br />
February 5-6<br />
Washington Neuroradiology Review<br />
Arlington, VA, United States<br />
February 12-17<br />
MI11 - SPIE Medical Imaging 2011<br />
Lake Buena Vista, FL, United States<br />
February 17-18<br />
2nd National Conference Diagnostic<br />
and Interventional Radiology 2011<br />
London, United Kingdom<br />
Februrary 17-18<br />
VII National Neuroradiology Course<br />
Lleida, Spain<br />
February 18<br />
Radiology in child protection<br />
Nottingham, United Kingdom<br />
Februrary 19-22<br />
COMPREHENSIVE REVIEW OF<br />
MUSCULOSKELETAL MRI<br />
Lake Buena Vista, FL, United States<br />
March 2-5<br />
2011 Abdominal Radiology Course<br />
Carlsbad, CA, United States<br />
March 3-7<br />
European Congress <strong>of</strong> Radiology<br />
Meeting ECR 2011<br />
Vienna, Austria<br />
March 6-9<br />
<strong>World</strong> Congress Thoracic Imaging - IV<br />
Bonita Springs, FL, United States<br />
WJR|www.wjgnet.com<br />
March 14-18<br />
9th Annual NYU Radiology Alpine<br />
Imaging Symposium at Beaver<br />
Creek<br />
Beaver Creek, CO, United States<br />
March 20-25<br />
Abdominal Radiology Course 2011<br />
Carlsbad, CA, United States<br />
March 26-31<br />
2011 SIR Annual Meeting<br />
Chicago, IL, United States<br />
March 28-April 1<br />
University <strong>of</strong> Utah Neuroradiology<br />
2nd Intensive Interactive Brain &<br />
Spine Imaging Conference<br />
Salt Lake City, UT, United States<br />
April 3-8<br />
1st Annual Ottawa Radiology<br />
Resident Review<br />
Ottawa, Canada<br />
April 3-8<br />
43rd International Diagnostic Course<br />
Davos on Diagnostic Imaging and<br />
Interventional Techniques<br />
Davos, Switzerland<br />
April 6-9<br />
Image-Based Neurodiagnosis:<br />
Intensive Clinical and Radiologic<br />
Review, CAQ Preparation<br />
Cincinnati, OH, United States<br />
April 28-May 1<br />
74th Annual Scientific Meeting<br />
<strong>of</strong> the Canadian Association <strong>of</strong><br />
Radiologists CAR<br />
Montreal, Canada<br />
May 5-8<br />
EMBL Conference-Sixth<br />
International Congress on Electron<br />
Tomography<br />
Heidelberg, Germany<br />
May 10-13<br />
27th Iranian Congress <strong>of</strong> Radiology<br />
Tehran, Iran<br />
May 14-21<br />
Radiology in Marrakech<br />
Marrakech, Morocco<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Radiology<br />
May 21-24<br />
European Society <strong>of</strong> Gastrointestinal<br />
and Abdominal Radiology 2011<br />
Annual Meeting<br />
Venice, Italy<br />
May 23-25<br />
Sports Medicine Imaging State <strong>of</strong><br />
the Art: A Collaborative Course for<br />
Radiologists and Sports Medicine<br />
Specialists<br />
New York, NY, United States<br />
May 24-26<br />
Russian Congress <strong>of</strong> Radiology<br />
Moscow, Russia<br />
May 28-31<br />
International Congress <strong>of</strong> Pediatric<br />
Radiology (IPR)<br />
London, United Kingdom<br />
June 4-8<br />
58th Annual Meeting <strong>of</strong> the Society<br />
<strong>of</strong> Nuclear Medicine<br />
San Antonio, TX, United States<br />
June 6-8<br />
UKRC 2011 - UK Radiological<br />
Congress<br />
Manchester, United Kingdom<br />
June 8-11<br />
CIRA 2011 - Canadian Internventinal<br />
Radiology Association Meeting<br />
Montreal, QC, Canada<br />
June 9-10<br />
8th ESGAR Liver Imaging Workshop<br />
Dublin, Ireland<br />
June 17-19<br />
ASCI 2011 - 5th Congress <strong>of</strong> Asian<br />
Society <strong>of</strong> Cardiovascular Imaging<br />
Hong Kong, China<br />
June 22-25<br />
CARS 2011 - Computer Assisted<br />
Radiology and Surgery - 25th<br />
International Congress and<br />
Exhibition<br />
Berlin, Germany<br />
June 27-July 1<br />
NYU Summer Radiology<br />
Symposium at The Sagamore<br />
Lake George, NY, United States<br />
July 18-22<br />
Clinical Case-Based Radiology<br />
Update in Iceland<br />
Reykjavik, Iceland<br />
August 1-5<br />
NYU Clinical Imaging Symposium<br />
in Santa Fe<br />
Santa Fe, NM, United States<br />
<strong>World</strong> J Radiol 2011 March 28; 3(3): I<br />
ISSN 1949-8470 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
September 22-25<br />
European Society <strong>of</strong> Neuroradiology<br />
(ESNR) XXXV Congress and 19th<br />
Advanced Course<br />
Antwerp, Belgium<br />
October 12-14<br />
International Conference Vipimage<br />
2011 - Computational Vision and<br />
Medical Image Processing<br />
Algarve, Portugal<br />
October 15-16<br />
Essentials <strong>of</strong> Emergency and Trauma<br />
Radiology<br />
Ottawa, Canada<br />
October 23-29<br />
2011 IEEE NSS - 2011 IEEE Nuclear<br />
Science Symposium and Medical<br />
Imaging Conference<br />
Valencia, Spain<br />
October 25-28<br />
NYU Radiology in Scottsdale - Fall<br />
Radiology Symposium in Scottsdale<br />
Scottsdale, AZ, United States<br />
October 28-30<br />
Fourth National Congress <strong>of</strong><br />
Pr<strong>of</strong>essionals <strong>of</strong> Radiological<br />
Techniques<br />
Florianópolis, Brazil<br />
October 28-30<br />
Multi-Modality Gynecological &<br />
Obstetric Imaging<br />
Ottawa, Canada<br />
November 3-4<br />
9th ESGAR Liver Imaging Workshop<br />
Taormina, Italy<br />
November 15-19<br />
EANM 2011 - Annual Congress <strong>of</strong><br />
the European Association <strong>of</strong> Nuclear<br />
Medicine<br />
Birmingham, United Kingdom<br />
November 22-29<br />
NSS/MIC - Nuclear Science<br />
Symposium and Medical Imaging<br />
Conference 2011<br />
Valencia, Spain<br />
November 26-28<br />
8th Asia Oceaninan Congress <strong>of</strong><br />
Neuro-Radiology<br />
Bangkok, Thailand<br />
I March 28, 2011|Volume 3|Issue 3|
W J R<br />
Online Submissions: http://www.wjgnet.com/1949-8470<strong>of</strong>fice<br />
wjr@wjgnet.com<br />
www.wjgnet.com<br />
Instructions to authors<br />
GENERAL INFORMATION<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Radiology (<strong>World</strong> J Radiol, WJR, online ISSN<br />
1949-8470, DOI: 10.4329), is a monthly, open-access (OA), peerreviewed<br />
journal supported by an editorial board <strong>of</strong> 319 experts in<br />
Radiology from 40 countries.<br />
The biggest advantage <strong>of</strong> the OA model is that it provides free,<br />
full-text articles in PDF and other formats for experts and the public<br />
without registration, which eliminates the obstacle that traditional<br />
journals possess and usually delays the speed <strong>of</strong> the propagation<br />
and communication <strong>of</strong> scientific research results. The open access<br />
model has been proven to be a true approach that may achieve the<br />
ultimate goal <strong>of</strong> the journals, i.e. the maximization <strong>of</strong> the value to<br />
the readers, authors and society.<br />
Maximization <strong>of</strong> personal benefits<br />
The role <strong>of</strong> academic journals is to exhibit the scientific levels <strong>of</strong><br />
a country, a university, a center, a department, and even a scientist,<br />
and build an important bridge for communication between scientists<br />
and the public. As we all know, the significance <strong>of</strong> the publication<br />
<strong>of</strong> scientific articles lies not only in disseminating and communicating<br />
innovative scientific achievements and academic views,<br />
as well as promoting the application <strong>of</strong> scientific achievements, but<br />
also in formally recognizing the “priority” and “copyright” <strong>of</strong> innovative<br />
achievements published, as well as evaluating research performance<br />
and academic levels. So, to realize these desired attributes<br />
<strong>of</strong> WJR and create a well-recognized journal, the following four<br />
types <strong>of</strong> personal benefits should be maximized. The maximization<br />
<strong>of</strong> personal benefits refers to the pursuit <strong>of</strong> the maximum personal<br />
benefits in a well-considered optimal manner without violation <strong>of</strong><br />
the laws, ethical rules and the benefits <strong>of</strong> others. (1) Maximization<br />
<strong>of</strong> the benefits <strong>of</strong> editorial board members: The primary task <strong>of</strong><br />
editorial board members is to give a peer review <strong>of</strong> an unpublished<br />
scientific article via online <strong>of</strong>fice system to evaluate its innovativeness,<br />
scientific and practical values and determine whether it should<br />
be published or not. During peer review, editorial board members<br />
can also obtain cutting-edge information in that field at first hand.<br />
As leaders in their field, they have priority to be invited to write<br />
articles and publish commentary articles. We will put peer reviewers’<br />
names and affiliations along with the article they reviewed in<br />
the journal to acknowledge their contribution; (2) Maximization <strong>of</strong><br />
the benefits <strong>of</strong> authors: Since WJR is an open-access journal, readers<br />
around the world can immediately download and read, free <strong>of</strong><br />
charge, high-quality, peer-reviewed articles from WJR <strong>of</strong>ficial website,<br />
thereby realizing the goals and significance <strong>of</strong> the communication<br />
between authors and peers as well as public reading; (3) Maximization<br />
<strong>of</strong> the benefits <strong>of</strong> readers: Readers can read or use, free <strong>of</strong><br />
charge, high-quality peer-reviewed articles without any limits, and<br />
cite the arguments, viewpoints, concepts, theories, methods, results,<br />
conclusion or facts and data <strong>of</strong> pertinent literature so as to validate<br />
the innovativeness, scientific and practical values <strong>of</strong> their own<br />
research achievements, thus ensuring that their articles have novel<br />
arguments or viewpoints, solid evidence and correct conclusion;<br />
and (4) Maximization <strong>of</strong> the benefits <strong>of</strong> employees: It is an iron law<br />
that a first-class journal is unable to exist without first-class editors,<br />
and only first-class editors can create a first-class academic journal.<br />
We insist on strengthening our team cultivation and construction so<br />
that every employee, in an open, fair and transparent environment,<br />
could contribute their wisdom to edit and publish high-quality articles,<br />
thereby realizing the maximization <strong>of</strong> the personal benefits<br />
WJR|www.wjgnet.com<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Radiology<br />
<strong>World</strong> J Radiol 2011 March 28; 3(3): I-V<br />
ISSN 1949-8470 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
<strong>of</strong> editorial board members, authors and readers, and yielding the<br />
greatest social and economic benefits.<br />
Aims and scope<br />
The major task <strong>of</strong> WJR is to rapidly report the most recent improvement<br />
in the research <strong>of</strong> medical imaging and radiation therapy by the<br />
radiologists. WJR accepts papers on the following aspects related to<br />
radiology: Abdominal radiology, women health radiology, cardiovascular<br />
radiology, chest radiology, genitourinary radiology, neuroradiology,<br />
head and neck radiology, interventional radiology, musculoskeletal<br />
radiology, molecular imaging, pediatric radiology, experimental<br />
radiology, radiological technology, nuclear medicine, PACS and<br />
radiology informatics, and ultrasound. We also encourage papers that<br />
cover all other areas <strong>of</strong> radiology as well as basic research.<br />
Columns<br />
The columns in the issues <strong>of</strong> WJR will include: (1) Editorial: To introduce<br />
and comment on major advances and developments in the<br />
field; (2) Frontier: To review representative achievements, comment<br />
on the state <strong>of</strong> current research, and propose directions for future<br />
research; (3) Topic Highlight: This column consists <strong>of</strong> three formats,<br />
including (A) 10 invited review articles on a hot topic, (B) a commentary<br />
on common issues <strong>of</strong> this hot topic, and (C) a commentary<br />
on the 10 individual articles; (4) Observation: To update the development<br />
<strong>of</strong> old and new questions, highlight unsolved problems, and<br />
provide strategies on how to solve the questions; (5) Guidelines for<br />
Basic Research: To provide guidelines for basic research; (6) Guidelines<br />
for Clinical Practice: To provide guidelines for clinical diagnosis<br />
and treatment; (7) Review: To review systemically progress and<br />
unresolved problems in the field, comment on the state <strong>of</strong> current<br />
research, and make suggestions for future work; (8) Original Articles:<br />
To report innovative and original findings in radiology; (9) Brief<br />
Articles: To briefly report the novel and innovative findings in radiology;<br />
(10) Case Report: To report a rare or typical case; (11) Letters to<br />
the Editor: To discuss and make reply to the contributions published<br />
in WJR, or to introduce and comment on a controversial issue <strong>of</strong><br />
general interest; (12) Book Reviews: To introduce and comment on<br />
quality monographs <strong>of</strong> radiology; and (13) Guidelines: To introduce<br />
consensuses and guidelines reached by international and national<br />
academic authorities worldwide on the research in radiology.<br />
Name <strong>of</strong> journal<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Radiology<br />
Serial publication number<br />
ISSN 1949-8470 (online)<br />
Indexed and Abstracted in<br />
PubMed Central, PubMed.<br />
Published by<br />
PubMed Central, PubMed, Digital Object Identifer, and Directory<br />
<strong>of</strong> Open Access <strong>Journal</strong>s.<br />
SPECIAL STATEMENT<br />
All articles published in this journal represent the viewpoints <strong>of</strong> the<br />
authors except where indicated otherwise.<br />
Biostatistical editing<br />
Statisital review is performed after peer review. We invite an expert<br />
in Biomedical Statistics from to evaluate the statistical method used<br />
I March 28, 2011|Volume 3|Issue 3|
Instructions to authors<br />
in the paper, including t-test (group or paired comparisons), chisquared<br />
test, Ridit, probit, logit, regression (linear, curvilinear, or<br />
stepwise), correlation, analysis <strong>of</strong> variance, analysis <strong>of</strong> covariance,<br />
etc. The reviewing points include: (1) Statistical methods should<br />
be described when they are used to verify the results; (2) Whether<br />
the statistical techniques are suitable or correct; (3) Only homogeneous<br />
data can be averaged. Standard deviations are preferred to<br />
standard errors. Give the number <strong>of</strong> observations and subjects (n).<br />
Losses in observations, such as drop-outs from the study should be<br />
reported; (4) Values such as ED50, LD50, IC50 should have their<br />
95% confidence limits calculated and compared by weighted probit<br />
analysis (Bliss and Finney); and (5) The word ‘significantly’ should<br />
be replaced by its synonyms (if it indicates extent) or the P value (if<br />
it indicates statistical significance).<br />
Conflict-<strong>of</strong>-interest statement<br />
In the interests <strong>of</strong> transparency and to help reviewers assess any potential<br />
bias, WJR requires authors <strong>of</strong> all papers to declare any competing<br />
commercial, personal, political, intellectual, or religious interests<br />
in relation to the submitted work. Referees are also asked to indicate<br />
any potential conflict they might have reviewing a particular<br />
paper. Before submitting, authors are suggested to read “Uniform<br />
Requirements for Manuscripts Submitted to Biomedical <strong>Journal</strong>s:<br />
Ethical Considerations in the Conduct and Reporting <strong>of</strong> Research:<br />
Conflicts <strong>of</strong> Interest” from International Committee <strong>of</strong> Medical<br />
<strong>Journal</strong> Editors (ICMJE), which is available at: http://www.icmje.<br />
org/ethical_4conflicts.html.<br />
Sample wording: [Name <strong>of</strong> individual] has received fees for serving<br />
as a speaker, a consultant and an advisory board member for [names<br />
<strong>of</strong> organizations], and has received research funding from [names <strong>of</strong><br />
organization]. [Name <strong>of</strong> individual] is an employee <strong>of</strong> [name <strong>of</strong> organization].<br />
[Name <strong>of</strong> individual] owns stocks and shares in [name <strong>of</strong><br />
organization]. [Name <strong>of</strong> individual] owns patent [patent identification<br />
and brief description].<br />
Statement <strong>of</strong> informed consent<br />
Manuscripts should contain a statement to the effect that all human<br />
studies have been reviewed by the appropriate ethics committee<br />
or it should be stated clearly in the text that all persons gave their<br />
informed consent prior to their inclusion in the study. Details that<br />
might disclose the identity <strong>of</strong> the subjects under study should be<br />
omitted. Authors should also draw attention to the Code <strong>of</strong> Ethics<br />
<strong>of</strong> the <strong>World</strong> Medical Association (Declaration <strong>of</strong> Helsinki, 1964,<br />
as revised in 2004).<br />
Statement <strong>of</strong> human and animal rights<br />
When reporting the results from experiments, authors should follow<br />
the highest standards and the trial should conform to Good Clinical<br />
Practice (for example, US Food and Drug Administration Good<br />
Clinical Practice in FDA-Regulated Clinical Trials; UK Medicines<br />
Research Council Guidelines for Good Clinical Practice in Clinical<br />
Trials) and/or the <strong>World</strong> Medical Association Declaration <strong>of</strong> Helsinki.<br />
Generally, we suggest authors follow the lead investigator’s national<br />
standard. If doubt exists whether the research was conducted<br />
in accordance with the above standards, the authors must explain the<br />
rationale for their approach and demonstrate that the institutional<br />
review body explicitly approved the doubtful aspects <strong>of</strong> the study.<br />
Before submitting, authors should make their study approved by<br />
the relevant research ethics committee or institutional review board.<br />
If human participants were involved, manuscripts must be accompanied<br />
by a statement that the experiments were undertaken with the<br />
understanding and appropriate informed consent <strong>of</strong> each. Any personal<br />
item or information will not be published without explicit consents<br />
from the involved patients. If experimental animals were used,<br />
the materials and methods (experimental procedures) section must<br />
clearly indicate that appropriate measures were taken to minimize<br />
pain or discomfort, and details <strong>of</strong> animal care should be provided.<br />
SUBMISSION OF MANUSCRIPTS<br />
Manuscripts should be typed in 1.5 line spacing and 12 pt. Book<br />
WJR|www.wjgnet.com<br />
Antiqua with ample margins. Number all pages consecutively, and<br />
start each <strong>of</strong> the following sections on a new page: Title Page, Abstract,<br />
Introduction, Materials and Methods, Results, Discussion,<br />
Acknowledgements, References, Tables, Figures, and Figure Legends.<br />
Neither the editors nor the publisher are responsible for the<br />
opinions expressed by contributors. Manuscripts formally accepted<br />
for publication become the permanent property <strong>of</strong> Baishideng<br />
Publishing Group Co., Limited, and may not be reproduced by any<br />
means, in whole or in part, without the written permission <strong>of</strong> both<br />
the authors and the publisher. We reserve the right to copy-edit and<br />
put onto our website accepted manuscripts. Authors should follow<br />
the relevant guidelines for the care and use <strong>of</strong> laboratory animals<br />
<strong>of</strong> their institution or national animal welfare committee. For the<br />
sake <strong>of</strong> transparency in regard to the performance and reporting <strong>of</strong><br />
clinical trials, we endorse the policy <strong>of</strong> the ICMJE to refuse to publish<br />
papers on clinical trial results if the trial was not recorded in a<br />
publicly-accessible registry at its outset. The only register now available,<br />
to our knowledge, is http://www.clinicaltrials.gov sponsored<br />
by the United States National Library <strong>of</strong> Medicine and we encourage<br />
all potential contributors to register with it. However, in the case<br />
that other registers become available you will be duly notified. A<br />
letter <strong>of</strong> recommendation from each author’s organization should<br />
be provided with the contributed article to ensure the privacy and<br />
secrecy <strong>of</strong> research is protected.<br />
Authors should retain one copy <strong>of</strong> the text, tables, photographs<br />
and illustrations because rejected manuscripts will not be returned<br />
to the author(s) and the editors will not be responsible for loss or<br />
damage to photographs and illustrations sustained during mailing.<br />
Online submissions<br />
Manuscripts should be submitted through the Online Submission<br />
System at: http://www.wjgnet.com/1949-8470<strong>of</strong>fice. Authors are<br />
highly recommended to consult the ONLINE INSTRUCTIONS<br />
TO AUTHORS (http://www.wjgnet.com/1949-8470/g_info_<br />
20100316162358.htm) before attempting to submit online. For<br />
assistance, authors encountering problems with the Online Submission<br />
System may send an email describing the problem to wjr@<br />
wjgnet.com, or by telephone: +86-10-85381892. If you submit your<br />
manuscript online, do not make a postal contribution. Repeated<br />
online submission for the same manuscript is strictly prohibited.<br />
MANUSCRIPT PREPARATION<br />
All contributions should be written in English. All articles must be<br />
submitted using word-processing s<strong>of</strong>tware. All submissions must be<br />
typed in 1.5 line spacing and 12 pt. Book Antiqua with ample margins.<br />
Style should conform to our house format. Required information<br />
for each <strong>of</strong> the manuscript sections is as follows:<br />
Title page<br />
Title: Title should be less than 12 words.<br />
Running title: A short running title <strong>of</strong> less than 6 words should be<br />
provided.<br />
Authorship: Authorship credit should be in accordance with the<br />
standard proposed by International Committee <strong>of</strong> Medical <strong>Journal</strong><br />
Editors, based on (1) substantial contributions to conception and<br />
design, acquisition <strong>of</strong> data, or analysis and interpretation <strong>of</strong> data; (2)<br />
drafting the article or revising it critically for important intellectual<br />
content; and (3) final approval <strong>of</strong> the version to be published. Authors<br />
should meet conditions 1, 2, and 3.<br />
Institution: Author names should be given first, then the complete<br />
name <strong>of</strong> institution, city, province and postcode. For example, Xu-<br />
Chen Zhang, Li-Xin Mei, Department <strong>of</strong> Pathology, Chengde<br />
Medical College, Chengde 067000, Hebei Province, China. One author<br />
may be represented from two institutions, for example, George<br />
Sgourakis, Department <strong>of</strong> General, Visceral, and Transplantation<br />
Surgery, Essen 45122, Germany; George Sgourakis, 2nd Surgical<br />
II March 28, 2011|Volume 3|Issue 3|
Department, Korgialenio-Benakio Red Cross Hospital, Athens<br />
15451, Greece<br />
Author contributions: The format <strong>of</strong> this section should be:<br />
Author contributions: Wang CL and Liang L contributed equally<br />
to this work; Wang CL, Liang L, Fu JF, Zou CC, Hong F and Wu<br />
XM designed the research; Wang CL, Zou CC, Hong F and Wu<br />
XM performed the research; Xue JZ and Lu JR contributed new<br />
reagents/analytic tools; Wang CL, Liang L and Fu JF analyzed the<br />
data; and Wang CL, Liang L and Fu JF wrote the paper.<br />
Supportive foundations: The complete name and number <strong>of</strong> supportive<br />
foundations should be provided, e.g., Supported by National<br />
Natural Science Foundation <strong>of</strong> China, No. 30224801<br />
Correspondence to: Only one corresponding address should be<br />
provided. Author names should be given first, then author title, affiliation,<br />
the complete name <strong>of</strong> institution, city, postcode, province,<br />
country, and email. All the letters in the email should be in lower<br />
case. A space interval should be inserted between country name and<br />
email address. For example, Montgomery Bissell, MD, Pr<strong>of</strong>essor <strong>of</strong><br />
Medicine, Chief, Liver Center, <strong>Gastroenterology</strong> Division, University<br />
<strong>of</strong> California, Box 0538, San Francisco, CA 94143, United States.<br />
montgomery.bissell@ucsf.edu<br />
Telephone and fax: Telephone and fax should consist <strong>of</strong> +, country<br />
number, district number and telephone or fax number, e.g., Telephone:<br />
+86-10-85381892 Fax: +86-10-85381893<br />
Peer reviewers: All articles received are subject to peer review.<br />
Normally, three experts are invited for each article. Decision for<br />
acceptance is made only when at least two experts recommend<br />
an article for publication. Reviewers for accepted manuscripts are<br />
acknowledged in each manuscript, and reviewers <strong>of</strong> articles which<br />
were not accepted will be acknowledged at the end <strong>of</strong> each issue.<br />
To ensure the quality <strong>of</strong> the articles published in WJR, reviewers <strong>of</strong><br />
accepted manuscripts will be announced by publishing the name,<br />
title/position and institution <strong>of</strong> the reviewer in the footnote accompanying<br />
the printed article. For example, reviewers: Pr<strong>of</strong>essor<br />
Jing-Yuan Fang, Shanghai Institute <strong>of</strong> Digestive Disease, Shanghai,<br />
Affiliated Renji Hospital, Medical Faculty, Shanghai Jiaotong University,<br />
Shanghai, China; Pr<strong>of</strong>essor Xin-Wei Han, Department <strong>of</strong><br />
Radiology, The First Affiliated Hospital, Zhengzhou University,<br />
Zhengzhou, Henan Province, China; and Pr<strong>of</strong>essor Anren Kuang,<br />
Department <strong>of</strong> Nuclear Medicine, Huaxi Hospital, Sichuan University,<br />
Chengdu, Sichuan Province, China.<br />
Abstract<br />
There are unstructured abstracts (no more than 256 words) and<br />
structured abstracts (no more than 480). The specific requirements<br />
for structured abstracts are as follows:<br />
An informative, structured abstracts <strong>of</strong> no more than 480<br />
words should accompany each manuscript. Abstracts for original<br />
contributions should be structured into the following sections. AIM<br />
(no more than 20 words): Only the purpose should be included.<br />
Please write the aim as the form <strong>of</strong> “To investigate/study/…;<br />
MATERIALS AND METHODS (no more than 140 words);<br />
RESULTS (no more than 294 words): You should present P values<br />
where appropriate and must provide relevant data to illustrate<br />
how they were obtained, e.g. 6.92 ± 3.86 vs 3.61 ± 1.67, P < 0.001;<br />
CONCLUSION (no more than 26 words).<br />
Key words<br />
Please list 5-10 key words, selected mainly from Index Medicus, which<br />
reflect the content <strong>of</strong> the study.<br />
Text<br />
For articles <strong>of</strong> these sections, original articles and brief articles, the<br />
main text should be structured into the following sections: INTRO-<br />
WJR|www.wjgnet.com<br />
Instructions to authors<br />
DUCTION, MATERIALS AND METHODS, RESULTS and<br />
DISCUSSION, and should include appropriate Figures and Tables.<br />
Data should be presented in the main text or in Figures and Tables,<br />
but not in both. The main text format <strong>of</strong> these sections, editorial,<br />
topic highlight, case report, letters to the editors, can be found at:<br />
http://www.wjgnet.com/1949-8470/g_info_20100313183720.htm.<br />
Illustrations<br />
Figures should be numbered as 1, 2, 3, etc., and mentioned clearly<br />
in the main text. Provide a brief title for each figure on a separate<br />
page. Detailed legends should not be provided under the<br />
figures. This part should be added into the text where the figures<br />
are applicable. Figures should be either Photoshop or Illustrator<br />
files (in tiff, eps, jpeg formats) at high-resolution. Examples<br />
can be found at: http://www.wjgnet.com/1007-9327/13/4520.<br />
pdf; http://www.wjgnet.com/1007-9327/13/4554.pdf; http://<br />
www.wjgnet.com/1007-9327/13/4891.pdf; http://www.<br />
wjgnet.com/1007-9327/13/4986.pdf; http://www.wjgnet.<br />
com/1007-9327/13/4498.pdf. Keeping all elements compiled is<br />
necessary in line-art image. Scale bars should be used rather than<br />
magnification factors, with the length <strong>of</strong> the bar defined in the legend<br />
rather than on the bar itself. File names should identify the figure<br />
and panel. Avoid layering type directly over shaded or textured<br />
areas. Please use uniform legends for the same subjects. For example:<br />
Figure 1 Pathological changes in atrophic gastritis after treatment.<br />
A: ...; B: ...; C: ...; D: ...; E: ...; F: ...; G: …etc. It is our principle<br />
to publish high resolution-figures for the printed and E-versions.<br />
Tables<br />
Three-line tables should be numbered 1, 2, 3, etc., and mentioned<br />
clearly in the main text. Provide a brief title for each table. Detailed<br />
legends should not be included under tables, but rather added into<br />
the text where applicable. The information should complement,<br />
but not duplicate the text. Use one horizontal line under the title, a<br />
second under column heads, and a third below the Table, above any<br />
footnotes. Vertical and italic lines should be omitted.<br />
Notes in tables and illustrations<br />
Data that are not statistically significant should not be noted. a P <<br />
0.05, b P < 0.01 should be noted (P > 0.05 should not be noted). If<br />
there are other series <strong>of</strong> P values, c P < 0.05 and d P < 0.01 are used.<br />
A third series <strong>of</strong> P values can be expressed as e P < 0.05 and f P < 0.01.<br />
Other notes in tables or under illustrations should be expressed as<br />
1 F, 2 F, 3 F; or sometimes as other symbols with a superscript (Arabic<br />
numerals) in the upper left corner. In a multi-curve illustration, each<br />
curve should be labeled with ●, ○, ■, □, ▲, △, etc., in a certain sequence.<br />
Acknowledgments<br />
Brief acknowledgments <strong>of</strong> persons who have made genuine contributions<br />
to the manuscript and who endorse the data and conclusions<br />
should be included. Authors are responsible for obtaining<br />
written permission to use any copyrighted text and/or illustrations.<br />
REFERENCES<br />
Coding system<br />
The author should number the references in Arabic numerals according<br />
to the citation order in the text. Put reference numbers in<br />
square brackets in superscript at the end <strong>of</strong> citation content or after<br />
the cited author’s name. For citation content which is part <strong>of</strong> the<br />
narration, the coding number and square brackets should be typeset<br />
normally. For example, “Crohn’s disease (CD) is associated with<br />
increased intestinal permeability [1,2] ”. If references are cited directly<br />
in the text, they should be put together within the text, for example,<br />
“From references [19,22-24] , we know that...”<br />
When the authors write the references, please ensure that the<br />
order in text is the same as in the references section, and also ensure<br />
the spelling accuracy <strong>of</strong> the first author’s name. Do not list the same<br />
citation twice.<br />
III March 28, 2011|Volume 3|Issue 3|
Instructions to authors<br />
PMID and DOI<br />
Pleased provide PubMed citation numbers to the reference list, e.g.<br />
PMID and DOI, which can be found at http://www.ncbi.nlm.nih.<br />
gov/sites/entrez?db=pubmed and http://www.crossref.org/SimpleTextQuery/,<br />
respectively. The numbers will be used in E-version<br />
<strong>of</strong> this journal.<br />
Style for journal references<br />
Authors: the name <strong>of</strong> the first author should be typed in bold-faced<br />
letters. The family name <strong>of</strong> all authors should be typed with the initial<br />
letter capitalized, followed by their abbreviated first and middle<br />
initials. (For example, Lian-Sheng Ma is abbreviated as Ma LS, Bo-<br />
Rong Pan as Pan BR). The title <strong>of</strong> the cited article and italicized<br />
journal title (journal title should be in its abbreviated form as shown<br />
in PubMed), publication date, volume number (in black), start page,<br />
and end page [PMID: 11819634 DOI: 10.3748/wjg.13.5396].<br />
Style for book references<br />
Authors: the name <strong>of</strong> the first author should be typed in bold-faced<br />
letters. The surname <strong>of</strong> all authors should be typed with the initial<br />
letter capitalized, followed by their abbreviated middle and first<br />
initials. (For example, Lian-Sheng Ma is abbreviated as Ma LS, Bo-<br />
Rong Pan as Pan BR) Book title. Publication number. Publication<br />
place: Publication press, Year: start page and end page.<br />
Format<br />
<strong>Journal</strong>s<br />
English journal article (list all authors and include the PMID where applicable)<br />
1 Jung EM, Clevert DA, Schreyer AG, Schmitt S, Rennert J,<br />
Kubale R, Feuerbach S, Jung F. Evaluation <strong>of</strong> quantitative contrast<br />
harmonic imaging to assess malignancy <strong>of</strong> liver tumors:<br />
A prospective controlled two-center study. <strong>World</strong> J Gastroenterol<br />
2007; 13: 6356-6364 [PMID: 18081224 DOI: 10.3748/wjg.13.<br />
6356]<br />
Chinese journal article (list all authors and include the PMID where applicable)<br />
2 Lin GZ, Wang XZ, Wang P, Lin J, Yang FD. Immunologic<br />
effect <strong>of</strong> Jianpi Yishen decoction in treatment <strong>of</strong> Pixu-diarrhoea.<br />
Shijie Huaren Xiaohua Zazhi 1999; 7: 285-287<br />
In press<br />
3 Tian D, Araki H, Stahl E, Bergelson J, Kreitman M. Signature<br />
<strong>of</strong> balancing selection in Arabidopsis. Proc Natl Acad Sci USA<br />
2006; In press<br />
Organization as author<br />
4 Diabetes Prevention Program Research Group. Hypertension,<br />
insulin, and proinsulin in participants with impaired glucose<br />
tolerance. Hypertension 2002; 40: 679-686 [PMID: 12411462<br />
PMCID:2516377 DOI:10.1161/01.HYP.0000035706.28494.<br />
09]<br />
Both personal authors and an organization as author<br />
5 Vallancien G, Emberton M, Harving N, van Moorselaar RJ;<br />
Alf-One Study Group. Sexual dysfunction in 1, 274 European<br />
men suffering from lower urinary tract symptoms. J Urol<br />
2003; 169: 2257-2261 [PMID: 12771764 DOI:10.1097/01.ju.<br />
0000067940.76090.73]<br />
No author given<br />
6 21st century heart solution may have a sting in the tail. BMJ<br />
2002; 325: 184 [PMID: 12142303 DOI:10.1136/bmj.325.<br />
7357.184]<br />
Volume with supplement<br />
7 Geraud G, Spierings EL, Keywood C. Tolerability and safety<br />
<strong>of</strong> frovatriptan with short- and long-term use for treatment<br />
<strong>of</strong> migraine and in comparison with sumatriptan. Headache<br />
2002; 42 Suppl 2: S93-99 [PMID: 12028325 DOI:10.1046/<br />
j.1526-4610.42.s2.7.x]<br />
Issue with no volume<br />
8 Banit DM, Kaufer H, Hartford JM. Intraoperative frozen<br />
section analysis in revision total joint arthroplasty. Clin Orthop<br />
Relat Res 2002; (401): 230-238 [PMID: 12151900 DOI:10.10<br />
97/00003086-200208000-00026]<br />
WJR|www.wjgnet.com<br />
No volume or issue<br />
9 Outreach: Bringing HIV-positive individuals into care. HRSA<br />
Careaction 2002; 1-6 [PMID: 12154804]<br />
Books<br />
Personal author(s)<br />
10 Sherlock S, Dooley J. Diseases <strong>of</strong> the liver and billiary system.<br />
9th ed. Oxford: Blackwell Sci Pub, 1993: 258-296<br />
Chapter in a book (list all authors)<br />
11 Lam SK. Academic investigator’s perspectives <strong>of</strong> medical<br />
treatment for peptic ulcer. In: Swabb EA, Azabo S. Ulcer<br />
disease: investigation and basis for therapy. New York: Marcel<br />
Dekker, 1991: 431-450<br />
Author(s) and editor(s)<br />
12 Breedlove GK, Schorfheide AM. Adolescent pregnancy.<br />
2nd ed. Wieczorek RR, editor. White Plains (NY): March <strong>of</strong><br />
Dimes Education Services, 2001: 20-34<br />
Conference proceedings<br />
13 Harnden P, J<strong>of</strong>fe JK, Jones WG, editors. Germ cell tumours V.<br />
Proceedings <strong>of</strong> the 5th Germ cell tumours Conference; 2001<br />
Sep 13-15; Leeds, UK. New York: Springer, 2002: 30-56<br />
Conference paper<br />
14 Christensen S, Oppacher F. An analysis <strong>of</strong> Koza's computational<br />
effort statistic for genetic programming. In: Foster JA,<br />
Lutton E, Miller J, Ryan C, Tettamanzi AG, editors. Genetic<br />
programming. EuroGP 2002: Proceedings <strong>of</strong> the 5th European<br />
Conference on Genetic Programming; 2002 Apr 3-5;<br />
Kinsdale, Ireland. Berlin: Springer, 2002: 182-191<br />
Electronic journal (list all authors)<br />
15 Morse SS. Factors in the emergence <strong>of</strong> infectious diseases.<br />
Emerg Infect Dis serial online, 1995-01-03, cited 1996-06-05;<br />
1(1): 24 screens. Available from: URL: http://www.cdc.gov/<br />
ncidod/eid/index.htm<br />
Patent (list all authors)<br />
16 Pagedas AC, inventor; Ancel Surgical R&D Inc., assignee.<br />
Flexible endoscopic grasping and cutting device and positioning<br />
tool assembly. United States patent US 20020103498. 2002 Aug<br />
1<br />
Statistical data<br />
Write as mean ± SD or mean ± SE.<br />
Statistical expression<br />
Express t test as t (in italics), F test as F (in italics), chi square test as<br />
χ 2 (in Greek), related coefficient as r (in italics), degree <strong>of</strong> freedom<br />
as υ (in Greek), sample number as n (in italics), and probability as P (in<br />
italics).<br />
Units<br />
Use SI units. For example: body mass, m (B) = 78 kg; blood pressure,<br />
p (B) = 16.2/12.3 kPa; incubation time, t (incubation) = 96 h,<br />
blood glucose concentration, c (glucose) 6.4 ± 2.1 mmol/L; blood<br />
CEA mass concentration, p (CEA) = 8.6 24.5 mg/L; CO 2 volume<br />
fraction, 50 mL/L CO 2, not 5% CO 2; likewise for 40 g/L formaldehyde,<br />
not 10% formalin; and mass fraction, 8 ng/g, etc. Arabic<br />
numerals such as 23, 243, 641 should be read 23 243 641.<br />
The format for how to accurately write common units and<br />
quantums can be found at: http://www.wjgnet.com/1949-8470/<br />
g_info_20100313185816.htm.<br />
Abbreviations<br />
Standard abbreviations should be defined in the abstract and on<br />
first mention in the text. In general, terms should not be abbreviated<br />
unless they are used repeatedly and the abbreviation is helpful<br />
to the reader. Permissible abbreviations are listed in Units, Symbols<br />
and Abbreviations: A Guide for Biological and Medical Editors and<br />
Authors (Ed. Baron DN, 1988) published by The Royal Society <strong>of</strong><br />
Medicine, London. Certain commonly used abbreviations, such as<br />
DNA, RNA, HIV, LD50, PCR, HBV, ECG, WBC, RBC, CT, ESR,<br />
CSF, IgG, ELISA, PBS, ATP, EDTA, mAb, can be used directly<br />
without further explanation.<br />
IV March 28, 2011|Volume 3|Issue 3|
Italics<br />
Quantities: t time or temperature, c concentration, A area, l length,<br />
m mass, V volume.<br />
Genotypes: gyrA, arg 1, c myc, c fos, etc.<br />
Restriction enzymes: EcoRI, HindI, BamHI, Kbo I, Kpn I, etc.<br />
Biology: H. pylori, E coli, etc.<br />
Examples for paper writing<br />
Editorial: http://www.wjgnet.com/1949-8470/g_info_20100313<br />
182341.htm<br />
Frontier: http://www.wjgnet.com/1949-8470/g_info_2010031318<br />
2448.htm<br />
Topic highlight: http://www.wjgnet.com/1949-8470/g_info_201003<br />
13182639.htm<br />
Observation: http://www.wjgnet.com/1949-8470/g_info_20100313<br />
182834.htm<br />
Guidelines for basic research: http://www.wjgnet.com/1949-8470/<br />
g_info_20100313183057.htm<br />
Guidelines for clinical practice: http://www.wjgnet.com/1949-<br />
8470/g_info_20100313183238.htm<br />
Review: http://www.wjgnet.com/1949-8470/g_info_20100313<br />
183433.htm<br />
Original articles: http://www.wjgnet.com/1949-8470/g_info_2010<br />
0313183720.htm<br />
Brief articles: http://www.wjgnet.com/1949-8470/g_info_201003<br />
13184005.htm<br />
Case report: http://www.wjgnet.com/1949-8470/g_info_20100313<br />
184149.htm<br />
Letters to the editor: http://www.wjgnet.com/1949-8470/g_info_20<br />
100313184410.htm<br />
Book reviews: http://www.wjgnet.com/1949-8470/g_info_201003<br />
13184803.htm<br />
Guidelines: http://www.wjgnet.com/1949-8470/g_info_20100313<br />
185047.htm<br />
SUBMISSION OF THE REVISED MANUSCRIPTS<br />
AFTER ACCEPTED<br />
Please revise your article according to the revision policies <strong>of</strong> WJR.<br />
The revised version including manuscript and high-resolution image<br />
figures (if any) should be re-submitted or uploaded online. The<br />
author should send copyright transfer letter, and responses to the<br />
reviewers and science news to us via email.<br />
Editorial Office<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Radiology<br />
Editorial Department: Room 903, Building D,<br />
WJR|www.wjgnet.com<br />
Instructions to authors<br />
Ocean International Center, No. 62 Dongsihuan Zhonglu,<br />
Chaoyang District, Beijing 100025, China<br />
E-mail: wjr@wjgnet.com<br />
http://www.wjgnet.com<br />
Telephone: +86-10-85381892<br />
Fax: +86-10-85381893<br />
Language evaluation<br />
The language <strong>of</strong> a manuscript will be graded before it is sent for<br />
revision. (1) Grade A: priority publishing; (2) Grade B: minor language<br />
polishing; (3) Grade C: a great deal <strong>of</strong> language polishing<br />
needed; and (4) Grade D: rejected. Revised articles should reach<br />
Grade A or B.<br />
Copyright assignment form<br />
Please download a Copyright assignment form from http://www.<br />
wjgnet.com/1949-8470/g_info_20100313185522.htm.<br />
Responses to reviewers<br />
Please revise your article according to the comments/suggestions<br />
provided by the reviewers. The format for responses to the reviewers’<br />
comments can be found at: http://www.wjgnet.com/1949-8470/<br />
g_info_20100313185358.htm.<br />
Pro<strong>of</strong> <strong>of</strong> financial support<br />
For paper supported by a foundation, authors should provide a<br />
copy <strong>of</strong> the document and serial number <strong>of</strong> the foundation.<br />
Links to documents related to the manuscript<br />
WJR will be initiating a platform to promote dynamic interactions between<br />
the editors, peer reviewers, readers and authors. After a manuscript<br />
is published online, links to the PDF version <strong>of</strong> the submitted<br />
manuscript, the peer-reviewers’ report and the revised manuscript will<br />
be put on-line. Readers can make comments on the peer reviewer’s<br />
report, authors’ responses to peer reviewers, and the revised manuscript.<br />
We hope that authors will benefit from this feedback and be<br />
able to revise the manuscript accordingly in a timely manner.<br />
Science news releases<br />
Authors <strong>of</strong> accepted manuscripts are suggested to write a science<br />
news item to promote their articles. The news will be released rapidly<br />
at EurekAlert/AAAS (http://www.eurekalert.org). The title for<br />
news items should be less than 90 characters; the summary should<br />
be less than 75 words; and main body less than 500 words. Science<br />
news items should be lawful, ethical, and strictly based on your<br />
original content with an attractive title and interesting pictures.<br />
Publication fee<br />
WJR is an international, peer-reviewed, Open-Access, online journal.<br />
Articles published by this journal are distributed under the<br />
terms <strong>of</strong> the Creative Commons Attribution Non-commercial<br />
License, which permits use, distribution, and reproduction in any<br />
medium, provided the original work is properly cited, the use is<br />
non commercial and is otherwise in compliance with the license.<br />
Authors <strong>of</strong> accepted articles must pay a publication fee. The related<br />
standards are as follows. Publication fee: 1300 USD per article;<br />
Reprints fee: 350 USD per 100 reprints, including postage cost.<br />
Editorial, topic highlights, book reviews and letters to the editor<br />
are published free <strong>of</strong> charge.<br />
V March 28, 2011|Volume 3|Issue 3|