Pediatric Neuroscience Pathways Fall 2012 - Cleveland Clinic
Pediatric Neuroscience Pathways Fall 2012 - Cleveland Clinic
Pediatric Neuroscience Pathways Fall 2012 - Cleveland Clinic
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
the scope of pediatric autonomic disorders is currently not well<br />
recognized as most publications on various aspects of autonomic<br />
function tend to concentrate mainly on adult disorders. in recent<br />
years, however, investigators have begun to appreciate the value of<br />
childhood genetic autonomic disorders as models to advance the<br />
understanding of pathophysiologic mechanisms involved in autonomic<br />
dysfunction. 1 it is therefore incumbent on pediatric caregivers<br />
to be more aware of the existence of this expanding spectrum of<br />
pediatric autonomic disorders, as early recognition is essential for<br />
appropriate investigation and management of this group of pediatric<br />
patients who may otherwise suffer debilitating symptoms and signs.<br />
symptoms of autonomic dysfunction in children<br />
Because the autonomic nervous system innervates multiple organ<br />
systems, the clinical manifestations of autonomic disorders are<br />
extremely varied and include abnormalities in the cardiovascular,<br />
respiratory, gastrointestinal, ophthalmologic, neurologic, sudomotor<br />
and urologic systems.<br />
<strong>Pediatric</strong> Neurology<br />
Postural Orthostatic Tachycardia Syndrome in Children – An Emerging Entity<br />
Manikum Moodley, MD<br />
At <strong>Cleveland</strong> <strong>Clinic</strong>, children and adolescents with postural orthostatic tachycardia syndrome (POTS) may<br />
receive state-of-the-art care from specialists dedicated to diagnosis and treatment of syncope and autonomic<br />
disorders. this multidisciplinary collaboration between pediatric neurology and cardiology offers the most<br />
modern approach to this complex group of disorders.<br />
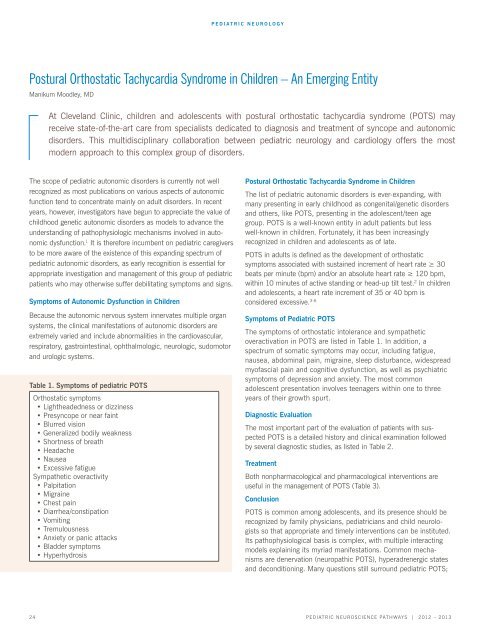
table 1. symptoms of pediatric Pots<br />
orthostatic symptoms<br />
• Lightheadedness or dizziness<br />
• Presyncope or near faint<br />
• Blurred vision<br />
• Generalized bodily weakness<br />
• Shortness of breath<br />
• Headache<br />
• Nausea<br />
• Excessive fatigue<br />
sympathetic overactivity<br />
• Palpitation<br />
• Migraine<br />
• Chest pain<br />
• Diarrhea/constipation<br />
• Vomiting<br />
• Tremulousness<br />
• Anxiety or panic attacks<br />
• Bladder symptoms<br />
• Hyperhydrosis<br />
Postural orthostatic tachycardia syndrome in children<br />
The list of pediatric autonomic disorders is ever-expanding, with<br />
many presenting in early childhood as congenital/genetic disorders<br />
and others, like POTS, presenting in the adolescent/teen age<br />
group. POTS is a well-known entity in adult patients but less<br />
well-known in children. Fortunately, it has been increasingly<br />
recognized in children and adolescents as of late.<br />
POTS in adults is defined as the development of orthostatic<br />
symptoms associated with sustained increment of heart rate ≥ 30<br />
beats per minute (bpm) and/or an absolute heart rate ≥ 120 bpm,<br />
within 10 minutes of active standing or head-up tilt test. 2 in children<br />
and adolescents, a heart rate increment of 35 or 40 bpm is<br />
considered excessive. 3-6<br />
symptoms of <strong>Pediatric</strong> Pots<br />
the symptoms of orthostatic intolerance and sympathetic<br />
overactivation in POTS are listed in Table 1. In addition, a<br />
spectrum of somatic symptoms may occur, including fatigue,<br />
nausea, abdominal pain, migraine, sleep disturbance, widespread<br />
myofascial pain and cognitive dysfunction, as well as psychiatric<br />
symptoms of depression and anxiety. the most common<br />
adolescent presentation involves teenagers within one to three<br />
years of their growth spurt.<br />
diagnostic evaluation<br />
the most important part of the evaluation of patients with suspected<br />
Pots is a detailed history and clinical examination followed<br />
by several diagnostic studies, as listed in Table 2.<br />
treatment<br />
Both nonpharmacological and pharmacological interventions are<br />
useful in the management of Pots (table 3).<br />
conclusion<br />
POTS is common among adolescents, and its presence should be<br />
recognized by family physicians, pediatricians and child neurologists<br />
so that appropriate and timely interventions can be instituted.<br />
Its pathophysiological basis is complex, with multiple interacting<br />
models explaining its myriad manifestations. common mechanisms<br />
are denervation (neuropathic POTS), hyperadrenergic states<br />
and deconditioning. Many questions still surround pediatric POTS;<br />
24 <strong>Pediatric</strong> NeuroscieNce <strong>Pathways</strong> | <strong>2012</strong> – 2013