Differential diagnosis of esophageal disease on esophagography
Differential diagnosis of esophageal disease on esophagography
Differential diagnosis of esophageal disease on esophagography
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
This review article will present<br />
a gamut or pattern approach to<br />
the <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g> <str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
<str<strong>on</strong>g>disease</str<strong>on</strong>g>s. 1,2 For most patients, analysis<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> the radiographic findings in combinati<strong>on</strong><br />
with c<strong>on</strong>siderati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> the clinical<br />
history leads to the <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g> or a<br />
graded differential <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g>. 3<br />
Dr. Rubesin is a Pr<str<strong>on</strong>g>of</str<strong>on</strong>g>essor <str<strong>on</strong>g>of</str<strong>on</strong>g> Radiology<br />
and member <str<strong>on</strong>g>of</str<strong>on</strong>g> the Gastrointestinal<br />
Radiology Secti<strong>on</strong>, and Dr. Levine<br />
is a Pr<str<strong>on</strong>g>of</str<strong>on</strong>g>essor <str<strong>on</strong>g>of</str<strong>on</strong>g> Radiology and Chief<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> the Gastrointestinal Radiology Secti<strong>on</strong><br />
at the Hospital <str<strong>on</strong>g>of</str<strong>on</strong>g> the University<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> Pennsylvania in Philadelphia, PA.<br />
October 2001<br />
<str<strong>on</strong>g>Differential</str<strong>on</strong>g> <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g><br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> <str<strong>on</strong>g>disease</str<strong>on</strong>g><br />
<strong>on</strong> <strong>esophagography</strong><br />
Stephen E. Rubesin, MD and Marc S. Levine, MD<br />
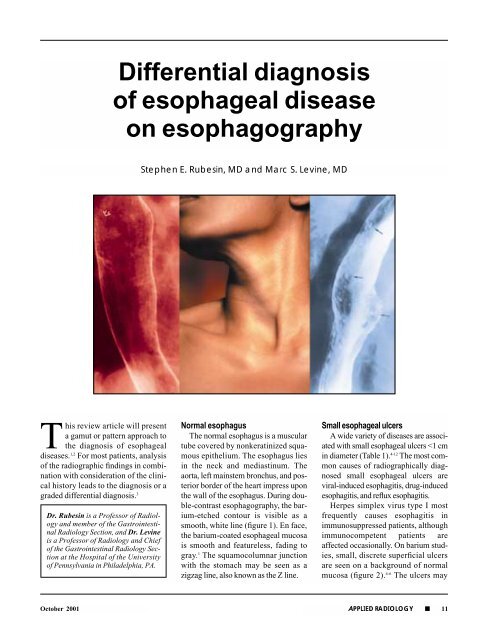
Normal esophagus<br />
The normal esophagus is a muscular<br />
tube covered by n<strong>on</strong>keratinized squamous<br />
epithelium. The esophagus lies<br />
in the neck and mediastinum. The<br />
aorta, left mainstem br<strong>on</strong>chus, and posterior<br />
border <str<strong>on</strong>g>of</str<strong>on</strong>g> the heart impress up<strong>on</strong><br />
the wall <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus. During double-c<strong>on</strong>trast<br />
<strong>esophagography</strong>, the barium-etched<br />
c<strong>on</strong>tour is visible as a<br />
smooth, white line (figure 1). En face,<br />
the barium-coated <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> mucosa<br />
is smooth and featureless, fading to<br />
gray. 1 The squamocolumnar juncti<strong>on</strong><br />
with the stomach may be seen as a<br />
zigzag line, also known as the Z line.<br />
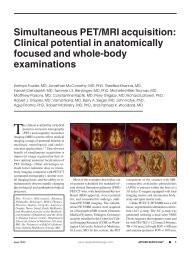
Small <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> ulcers<br />
A wide variety <str<strong>on</strong>g>of</str<strong>on</strong>g> <str<strong>on</strong>g>disease</str<strong>on</strong>g>s are associated<br />
with small <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> ulcers
FIGURE 1. Normal esophagus. The luminal<br />
c<strong>on</strong>tour is manifest as a smooth, straight<br />
white line (white arrow). The mucosal surface<br />
has a featureless, gray appearance en<br />
face (black arrow).<br />
have a round, stellate, linear, or serpentine<br />
c<strong>on</strong>figurati<strong>on</strong>. Rarely, herpes<br />
esophagitis may develop in immunocompetent<br />
patients. In this self-limited<br />
form <str<strong>on</strong>g>of</str<strong>on</strong>g> herpes esophagitis, the ulcers<br />
manifest as smaller, punctate collecti<strong>on</strong>s<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> barium. 7<br />
Drug-induced esophagitis is primarily<br />
a c<strong>on</strong>tact esophagitis caused by<br />
a variety <str<strong>on</strong>g>of</str<strong>on</strong>g> medicati<strong>on</strong>s, including<br />
tetracycline or its derivatives, quinidine,<br />
potassium chloride, n<strong>on</strong>-<br />
FIGURE 2. Small <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> ulcers in herpes<br />
esophagitis. Many small punctate collecti<strong>on</strong>s<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> barium surrounded by radiolucent halos<br />
(arrows) are seen in the midesophagus. The<br />
clinical history <str<strong>on</strong>g>of</str<strong>on</strong>g> AIDS in this patient enables<br />
the radiologist to make a <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g> viral,<br />
especially herpes, esophagitis. (Reproduced<br />
with permissi<strong>on</strong> from Levine MS, Laufer I.<br />
Esophagus. In: Levine MS, Rubesin SE,<br />
Laufer I. Double C<strong>on</strong>trast Gastrointestinal<br />
Radiology. 3rd ed. Philadelphia: WB Saunders<br />
Co.; 2000:90-126. 1 )<br />
steroidal anti-inflammatory agents,<br />
and alendr<strong>on</strong>ate sodium. If little or no<br />
water is used during ingesti<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> these<br />
medicati<strong>on</strong>s, pills may transiently<br />
lodge in the esophagus at the level <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
normal extrinsic impressi<strong>on</strong>s, includ-<br />
Table 1. Causes <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> ulcers<br />
Small <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> ulcers<br />
(1 cm in diameter)<br />
Cytomegalovirus<br />
Human immunodeficiency virus<br />
Carcinoma<br />
Drug-induced<br />
Barrett’s ulcer<br />
Sclerotherapy for varices<br />
ing the aortic arch, the left mainstem<br />
br<strong>on</strong>chus, and the left atrium. Typically,<br />
small, shallow ulcers will be<br />
clustered together in the mid-esophagus.<br />
8,9 These ulcers usually heal within<br />
7 to 10 days after cessati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g>fending medicati<strong>on</strong>.<br />
In patients with small <str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
ulcers, the clinical history provides<br />
the key to the <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g>. Patients with<br />
herpes esophagitis are usually<br />
immunosuppressed. If drug ingesti<strong>on</strong><br />
is the cause <str<strong>on</strong>g>of</str<strong>on</strong>g> the ulcer, a clinical history<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> using the <str<strong>on</strong>g>of</str<strong>on</strong>g>fending medicati<strong>on</strong><br />
can usually be elicited. Finally,<br />
patients with reflux-induced ulcers<br />
usually have a history <str<strong>on</strong>g>of</str<strong>on</strong>g> heartburn,<br />
and the ulcers are usually located in<br />
the distal esophagus near the esophagogastric<br />
juncti<strong>on</strong>. These patients also<br />
usually have other radiographic findings<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> reflux esophagitis. 2<br />
Large <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> ulcers<br />
The most comm<strong>on</strong> causes <str<strong>on</strong>g>of</str<strong>on</strong>g> large<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> ulcers, those >1 cm in<br />
diameter, are human immunodeficiency<br />
virus (HIV) and cytomegalovirus<br />
(CMV) in immunocompromised<br />
patients, primarily patients with<br />
acquired immunodeficiency syndrome<br />
(AIDS). 13-16 HIV ulcers some-<br />
12 ■ APPLIED RADIOLOGY October 2001
FIGURE 3. Large <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> ulcers due to<br />
HIV. This patient with odynophagia has<br />
large (>1 cm) ulcers (large black arrows) in<br />
the distal esophagus. Barium etches the<br />
undulating margins (arrowhead) <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
ulcers. A halo <str<strong>on</strong>g>of</str<strong>on</strong>g> edema (white arrow) surrounds<br />
the craters. This patient recently<br />
underwent seroc<strong>on</strong>versi<strong>on</strong> for HIV. Endoscopic<br />
biopsies <str<strong>on</strong>g>of</str<strong>on</strong>g> the ulcers failed to identify<br />
cytomegalovirus, so HIV esophagitis<br />
was a <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g> exclusi<strong>on</strong>.<br />
October 2001<br />
FIGURE 4. Squamous cell carcinoma. This<br />
smoker and drinker has a large ulcer (l<strong>on</strong>g<br />
arrow) surrounded by a lobulated, thickened<br />
edge (short arrows). The ulcer is<br />
deeper than a viral-induced ulcer and the<br />
edge is much thicker and more lobulated<br />
than a viral-induced ulcer. Squamous cell<br />
carcinoma was diagnosed histologically.<br />
Table 2. Mucosal nodules and plaques<br />
Cause Comment<br />
Candida Discrete plaques in immunosuppressed patient<br />
Reflux esophagitis Poorly defined nodules, associated hiatal hernia<br />
and gastro<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> reflux<br />
Glycogenic acanthosis Asymptomatic patient<br />
Superficial spreading Coalescent plaques in focal area<br />
cancer<br />
times occur near the time <str<strong>on</strong>g>of</str<strong>on</strong>g> clinical<br />
presentati<strong>on</strong> and seroc<strong>on</strong>versi<strong>on</strong>. The<br />
ulcers in CMV and HIV esophagitis<br />
(figure 3) tend to be large, flat, ovoidshaped<br />
barium collecti<strong>on</strong>s or bariumetched<br />
craters. 14,16 Endoscopic biopsy<br />
specimens are necessary to distinguish<br />
CMV or HIV ulcers, as the<br />
treatment for each <str<strong>on</strong>g>of</str<strong>on</strong>g> these infecti<strong>on</strong>s<br />
is different. Esophageal ulcerati<strong>on</strong> due<br />
to HIV is a <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g> exclusi<strong>on</strong>, so<br />
this <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g> can be made <strong>on</strong>ly when<br />
endoscopic biopsies, brushings, and<br />
cultures are negative for CMV.<br />
Other comm<strong>on</strong> causes <str<strong>on</strong>g>of</str<strong>on</strong>g> large<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> ulcers include carcinoma<br />
(figure 4), drug-induced ulcers, or<br />
Barrett’s esophagus 3,17,18 (Table 1).<br />
However, these ulcers tend to be<br />
deeper than viral-induced ulcers, and<br />
their edges are frequently thickened<br />
and lobulated. In such cases, biopsy<br />
specimens may be necessary to<br />
exclude neoplasia.<br />
Mucosal nodules and plaques<br />
Mucosal nodules and plaques are<br />
elevated lesi<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> varying size.<br />
Plaques are usually discrete, irregular<br />
or ovoid elevati<strong>on</strong>s that barely protrude<br />
above the mucosal surface. Nodules<br />
are smaller elevati<strong>on</strong>s and are<br />
more rounded than plaques. The morphology<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> the elevati<strong>on</strong>s in combinati<strong>on</strong><br />
with the clinical history allows a<br />
specific <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g> to be made in most<br />
patients (Table 2).<br />
Candida esophagitis most frequently<br />
manifests as numerous small,<br />
discrete, ovoid or linear plaque-like<br />
elevati<strong>on</strong>s aligned parallel to the l<strong>on</strong>gitudinal<br />
folds <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus (figure<br />
5). 19 In mild-to-moderate Candida<br />
esophagitis, the plaques are separated<br />
by intervening segments <str<strong>on</strong>g>of</str<strong>on</strong>g> normal<br />
mucosa. In more severe cases, the<br />
plaques may carpet the esophagus. In<br />
even more severe cases, c<strong>on</strong>fluent<br />
plaques, pseudomembranes, and barium<br />
burrowing beneath the inflammatory<br />
detritus may produce a grossly<br />
irregular appearance <str<strong>on</strong>g>of</str<strong>on</strong>g> the c<strong>on</strong>tour in<br />
APPLIED RADIOLOGY ■ 13
FIGURE 5. Candida esophagitis. This<br />
immunosuppressed patient with odynophagia<br />
has small, irregular, discrete plaque-like<br />
elevati<strong>on</strong>s (arrows) aligned parallel to the<br />
l<strong>on</strong>gitudinal folds <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus. The<br />
plaques are separated by intervening segments<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> normal mucosa.<br />
pr<str<strong>on</strong>g>of</str<strong>on</strong>g>ile and the mucosal surface en face,<br />
the so-called “shaggy esophagus.”<br />
When plaques and pseudomembranes<br />
slough, large ulcers may form, but these<br />
are almost always present <strong>on</strong> a background<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> diffuse plaque formati<strong>on</strong>.<br />
Candida albicans is the most comm<strong>on</strong><br />
cause <str<strong>on</strong>g>of</str<strong>on</strong>g> infectious esophagitis.<br />
Immunosuppressi<strong>on</strong> is the most frequent<br />
predisposing factor. Patients<br />
usually complain <str<strong>on</strong>g>of</str<strong>on</strong>g> dysphagia or<br />
odynophagia. Thrush in the oral cavity<br />
or pharynx is seen in about <strong>on</strong>ehalf<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> patients. Candida esophagitis<br />
may also develop in patients with<br />
severe <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> motility disorders,<br />
such as scleroderma, or in patients<br />
with <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> obstructi<strong>on</strong> and stasis<br />
due to achalasia or carcinoma.<br />
A B<br />
FIGURE 6. Mucosal changes in reflux esophagitis. (A) Mucosal nodularity. Well-defined<br />
radiolucent nodules carpet the mucosa <str<strong>on</strong>g>of</str<strong>on</strong>g> the distal esophagus (representative area <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
nodularity identified by arrow). (B) Granular mucosa and tiny ulcers. In a different patient, the<br />
mucosa <str<strong>on</strong>g>of</str<strong>on</strong>g> the distal esophagus is covered by innumerable, tiny, ill-defined radiolucencies<br />
(open arrows). In the more distal porti<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus, tiny ulcers are visible as punctate<br />
dots <str<strong>on</strong>g>of</str<strong>on</strong>g> barium (arrows).<br />
Small nodules and plaques <str<strong>on</strong>g>of</str<strong>on</strong>g> varying<br />
sizes may also be seen in the<br />
esophagus in patients with glycogenic<br />
acanthosis, a comm<strong>on</strong> degenerative<br />
c<strong>on</strong>diti<strong>on</strong>. 20,21 However, the plaques <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
glycogenic acanthosis are usually seen<br />
in the upper or midesophagus in a random<br />
distributi<strong>on</strong>. In this disorder,<br />
glycogen is accumulated in the cytoplasm<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> cells in the upper porti<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the squamous epithelium. Glycogenic<br />
acanthosis typically occurs in elderly<br />
individuals who have no <str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
symptoms and who do not have a history<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> immunosuppressi<strong>on</strong> or a c<strong>on</strong>diti<strong>on</strong><br />
predisposing to stasis. In c<strong>on</strong>trast,<br />
patients with Candida esophagitis are<br />
usually symptomatic, and the plaques<br />
tend to be more linear in shape and<br />
aligned l<strong>on</strong>gitudinally al<strong>on</strong>g the folds.<br />
In some patients with reflux<br />
esophagitis, tiny mucosal nodules are<br />
seen (figure 6). 2 However, these nodules<br />
are more ill-defined and less discrete<br />
than the plaques in Candida<br />
esophagitis. The nodules <str<strong>on</strong>g>of</str<strong>on</strong>g> reflux<br />
esophagitis also are more c<strong>on</strong>fluent<br />
and are located in the distal esophagus,<br />
usually in patients with gastro<str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
reflux and hiatal hernias.<br />
Reflux esophagitis is more frequently<br />
characterized by poorly defined tiny<br />
mucosal elevati<strong>on</strong>s, termed mucosal<br />
“granularity” (figure 6B). 1,2,22,23 This<br />
granularity may be associated with tiny<br />
or linear ulcers and thickened, nodular<br />
folds. These changes are also usually<br />
associated with a hiatal hernia and fluo-<br />
14 ■ APPLIED RADIOLOGY October 2001
FIGURE 7. Superficial spreading carcinoma.<br />
A l<strong>on</strong>g but focal area <str<strong>on</strong>g>of</str<strong>on</strong>g> c<strong>on</strong>fluent mucosal<br />
nodularity (arrows) is seen in the midesophagus.<br />
(Reproduced with permissi<strong>on</strong> from Low<br />
VHS, Rubesin SE. C<strong>on</strong>trast evaluati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
pharynx and esophagus. Radiol Clin North<br />
Am. 1993;31:1265-1291. 32 )<br />
roscopically detected gastro<str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
reflux. Some patients with reflux<br />
esophagitis have such severe inflammati<strong>on</strong><br />
that plaque-like pseudomembranes<br />
may eventually form. 24<br />
A focal area <str<strong>on</strong>g>of</str<strong>on</strong>g> c<strong>on</strong>fluent mucosal<br />
nodularity may be worrisome for<br />
superficial spreading carcinoma, a<br />
cancer c<strong>on</strong>fined to the mucosa and<br />
submucosa (figure 7). 25,26 However,<br />
the nodules are not as discrete as those<br />
October 2001<br />
FIGURE 8. Reticular pattern in Barrett’s esophagus. C<strong>on</strong>ed-down view <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus at<br />
the level <str<strong>on</strong>g>of</str<strong>on</strong>g> the left mainstem br<strong>on</strong>chus shows a lace-like network <str<strong>on</strong>g>of</str<strong>on</strong>g> barium-filled grooves<br />
surrounding small, polyg<strong>on</strong>al, radiolucent tufts <str<strong>on</strong>g>of</str<strong>on</strong>g> mucosa (open arrows). Distally, a striated<br />
appearance (large arrow) is seen. These changes were due to biopsy-proven Barrett’s<br />
mucosa.<br />
in Candida esophagitis, nor are they<br />
separated by normal intervening<br />
mucosa. Although most focal areas <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
mucosal irregularity will probably be<br />
caused by glycogenic acanthosis, an<br />
area <str<strong>on</strong>g>of</str<strong>on</strong>g> focal mucosal nodularity<br />
should be biopsied to exclude superficial<br />
spreading carcinoma.<br />
It is also difficult to distinguish a<br />
focal area <str<strong>on</strong>g>of</str<strong>on</strong>g> mucosal nodularity from<br />
the surface pattern termed “reticular<br />
mucosa,” which is seen in Barrett’s<br />
esophagus. 27 Barrett’s esophagus is an<br />
acquired c<strong>on</strong>diti<strong>on</strong> in which there is<br />
progressive columnar metaplasia <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the esophagus due to l<strong>on</strong>g-standing<br />
gastro<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> reflux <str<strong>on</strong>g>disease</str<strong>on</strong>g>. The<br />
reticular mucosal pattern resembles<br />
the areae gastricae <str<strong>on</strong>g>of</str<strong>on</strong>g> the stomach,<br />
with a fine, net-like web <str<strong>on</strong>g>of</str<strong>on</strong>g> bariumfilled<br />
grooves surrounding small tufts<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> mucosa (figure 8).<br />
APPLIED RADIOLOGY ■ 15
Cause<br />
Table 3. Abnormal <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> folds<br />
Comment<br />
Reflux esophagitis Other findings <str<strong>on</strong>g>of</str<strong>on</strong>g> gastro<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> reflux <str<strong>on</strong>g>disease</str<strong>on</strong>g><br />
Varices Serpentine, variable<br />
Varicoid carcinoma Rigid, fixed, irregular<br />
Lymphoma Discrete submucosal nodules<br />
FIGURE 9. Esophageal varices. A thickened,<br />
smooth, serpentine fold (l<strong>on</strong>g arrows)<br />
is seen in the esophagus at the level <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
left mainstem br<strong>on</strong>chus. Another thickened,<br />
smooth, undulating fold (short arrows) is<br />
seen in the distal esophagus.<br />
FIGURE 10. Varicoid form <str<strong>on</strong>g>of</str<strong>on</strong>g> squamous<br />
cell carcinoma. Coarsely lobulated folds<br />
expand the lumen <str<strong>on</strong>g>of</str<strong>on</strong>g> the midesophagus.<br />
No change in the size or shape <str<strong>on</strong>g>of</str<strong>on</strong>g> the folds<br />
was seen during fluoroscopy.<br />
Abnormal <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> folds<br />
The l<strong>on</strong>gitudinal folds <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus<br />
are composed <str<strong>on</strong>g>of</str<strong>on</strong>g> mucosa and<br />
submucosa and are best seen when the<br />
esophagus is underdistended. Therefore,<br />
abnormalities <str<strong>on</strong>g>of</str<strong>on</strong>g> folds reflect <str<strong>on</strong>g>disease</str<strong>on</strong>g><br />
in the mucosa and submucosa<br />
(Table 3). In patients with reflux<br />
esophagitis, thickened <str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
folds are frequently seen when the<br />
esophagus is collapsed. 1,2 These<br />
patients usually have other findings <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
reflux <str<strong>on</strong>g>disease</str<strong>on</strong>g>, including gastro<str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
reflux, a granular mucosa,<br />
and hiatal hernia. In c<strong>on</strong>trast,<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> varices are serpentine,<br />
with a smooth surface (figure 9).<br />
Varices may change in size with varying<br />
degrees <str<strong>on</strong>g>of</str<strong>on</strong>g> <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> distenti<strong>on</strong><br />
and patient positi<strong>on</strong>. If the folds are<br />
rigid, fixed, or irregular, however, the<br />
varicoid form <str<strong>on</strong>g>of</str<strong>on</strong>g> squamous cell carcinoma<br />
must be excluded (figure 10). 28<br />
Esophageal strictures<br />
The differential <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g> an<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> stricture depends <strong>on</strong> the<br />
morphology and locati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> the stricture<br />
as well as <strong>on</strong> the clinical history.<br />
Benign strictures typically manifest as<br />
smooth, tapered areas <str<strong>on</strong>g>of</str<strong>on</strong>g> c<strong>on</strong>centric<br />
narrowing (figure 11). 1 Asymmetric<br />
scarring may result in sacculati<strong>on</strong>,<br />
flattening, or other deformity <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
wall. In c<strong>on</strong>trast, malignant strictures<br />
are manifest as eccentric narrowings,<br />
thicker <strong>on</strong> the side where the tumor<br />
originated. 23 The mucosal surface is<br />
irregular, with nodules <str<strong>on</strong>g>of</str<strong>on</strong>g> varying size<br />
disrupting the surface and barium<br />
being trapped in areas <str<strong>on</strong>g>of</str<strong>on</strong>g> ulcerati<strong>on</strong>.<br />
The margins <str<strong>on</strong>g>of</str<strong>on</strong>g> malignant strictures<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g>ten appear abrupt and shelf-like (figure<br />
12). Unlike malignant lesi<strong>on</strong>s in<br />
the col<strong>on</strong>, however, malignant<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> lesi<strong>on</strong>s may have sloped<br />
or tapered margins, as the s<str<strong>on</strong>g>of</str<strong>on</strong>g>t<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> submucosa and muscularis<br />
propria provide little resistance to<br />
the l<strong>on</strong>gitudinal spread <str<strong>on</strong>g>of</str<strong>on</strong>g> tumor. In<br />
some patients, a plaque-like indentati<strong>on</strong><br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> the lumen is seen (figure 13). If<br />
16 ■ APPLIED RADIOLOGY October 2001
FIGURE 11. Reflux-induced stricture. A circumferential<br />
area <str<strong>on</strong>g>of</str<strong>on</strong>g> narrowing in the distal<br />
esophagus has a smooth, tapered c<strong>on</strong>tour<br />
(arrows) and smooth mucosa. A hiatal hernia<br />
(H) persists while the patient is in the<br />
erect positi<strong>on</strong>, indicating shortening <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
esophagus due to chr<strong>on</strong>ic scarring. (Reproduced<br />
with permissi<strong>on</strong> from Low VHS,<br />
Rubesin SE. C<strong>on</strong>trast evaluati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
pharynx and esophagus. Radiol Clin North<br />
Am. 1993;31:1265-1291. 32 )<br />
any mucosal irregularity or plaquelike<br />
flattening is identified in the<br />
regi<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> an <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> stricture,<br />
endoscopy and biopsy are required to<br />
exclude carcinoma.<br />
The most comm<strong>on</strong> causes <str<strong>on</strong>g>of</str<strong>on</strong>g> short<br />
distal <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> strictures are gastro<str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
reflux and carcinoma<br />
(Table 4; figures 11 and 14). L<strong>on</strong>g distal<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> strictures are <str<strong>on</strong>g>of</str<strong>on</strong>g>ten due<br />
to severe acid exposure related to<br />
Zollinger-Ellis<strong>on</strong> syndrome, prol<strong>on</strong>ged<br />
nasogastric intubati<strong>on</strong>, or alka-<br />
October 2001<br />
FIGURE 12. Squamous cell carcinoma. A<br />
malignant stricture is seen at the level <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
aortic arch. The c<strong>on</strong>tour is irregular (black<br />
arrows). The bulk <str<strong>on</strong>g>of</str<strong>on</strong>g> the tumor lies <strong>on</strong> the left<br />
lateral wall. The stricture has an abrupt,<br />
mass-like margin proximally (l<strong>on</strong>g white<br />
arrow). The mucosa is nodular. Smooth,<br />
tapered narrowing <str<strong>on</strong>g>of</str<strong>on</strong>g> the <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> wall<br />
(short white arrows) opposite the bulk <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
tumor indicates the beginning <str<strong>on</strong>g>of</str<strong>on</strong>g> circumferential<br />
spread <str<strong>on</strong>g>of</str<strong>on</strong>g> tumor.<br />
line reflux esophagitis (Table 4).<br />
Some patients with Crohn’s <str<strong>on</strong>g>disease</str<strong>on</strong>g><br />
may also develop l<strong>on</strong>g distal<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> strictures. A wide variety<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> c<strong>on</strong>diti<strong>on</strong>s cause mid<str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
strictures (Table 4). 29-34 The combinati<strong>on</strong><br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> the clinical history, physical<br />
examinati<strong>on</strong> findings, and radiographic<br />
appearance <str<strong>on</strong>g>of</str<strong>on</strong>g> the strictures<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g>ten enables a specific <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g>.<br />
Strictures related to reflux<br />
esophagitis are usually seen in the distal<br />
esophagus. Some reflux-induced<br />
A<br />
B<br />
FIGURE 13. Plaque-like adenocarcinoma<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> the distal esophagus. (A) Spot image <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the distal esophagus obtained with the<br />
patient in a left posterior oblique positi<strong>on</strong><br />
dem<strong>on</strong>strates a focal area <str<strong>on</strong>g>of</str<strong>on</strong>g> coarse<br />
mucosal nodularity en face (arrows) above<br />
a small hiatal hernia. (B) Spot image <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
distal esophagus obtained with patient now<br />
turned into the right posterior oblique positi<strong>on</strong>.<br />
A plaque-like lesi<strong>on</strong> (arrows) is seen in<br />
pr<str<strong>on</strong>g>of</str<strong>on</strong>g>ile <strong>on</strong> the posterolateral wall.<br />
APPLIED RADIOLOGY ■ 17
Table 4. Causes <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> strictures<br />
Short distal <str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
strictures<br />
Reflux-induced<br />
Carcinoma<br />
Crohn’s <str<strong>on</strong>g>disease</str<strong>on</strong>g><br />
Schatzki ring<br />
L<strong>on</strong>g distal <str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
strictures<br />
Nasogastric intubati<strong>on</strong><br />
Zollinger-Ellis<strong>on</strong> syndrome<br />
Alkaline reflux esophagitis<br />
Crohn’s <str<strong>on</strong>g>disease</str<strong>on</strong>g><br />
Mid<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> strictures<br />
Barrett’s esophagus<br />
Radiati<strong>on</strong> damage<br />
Caustic ingesti<strong>on</strong><br />
Primary or metastatic cancer<br />
Drug-induced stricture (especially<br />
potassium chloride)<br />
Esophageal intramural pseudodiverticulosis<br />
Benign mucous membrane pemphigoid,<br />
epidermolysis bullosa<br />
Graft versus host <str<strong>on</strong>g>disease</str<strong>on</strong>g><br />
strictures are smooth and tapered (figure<br />
11). However, other refluxinduced<br />
strictures are associated with<br />
enough asymmetric scarring to cause<br />
sacculati<strong>on</strong> in the area <str<strong>on</strong>g>of</str<strong>on</strong>g> tapering.<br />
These sacculati<strong>on</strong>s due to scarring<br />
should not be c<strong>on</strong>fused with ulcers.<br />
Other reflux-induced strictures may<br />
be associated with such severe scarring<br />
and <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> shortening that a<br />
hiatal hernia is even present in the<br />
erect positi<strong>on</strong>.<br />
In the presence <str<strong>on</strong>g>of</str<strong>on</strong>g> a hiatal hernia<br />
and gastro<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> reflux, a<br />
benign-appearing mid<str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
stricture or reticular pattern should be<br />
str<strong>on</strong>gly suggestive <str<strong>on</strong>g>of</str<strong>on</strong>g> Barrett’s<br />
esophagus. 30 Strictures associated<br />
with Barrett’s esophagus are more frequently<br />
seen in the distal esophagus,<br />
however. Patients with distal<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> strictures and reflux<br />
changes have a moderate risk <str<strong>on</strong>g>of</str<strong>on</strong>g> Bar-<br />
FIGURE 14. Short distal <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> adenocarcinoma.<br />
A short, tapered stricture<br />
(arrows) <str<strong>on</strong>g>of</str<strong>on</strong>g> the distal esophagus is eccentrically<br />
located and has a slightly irregular<br />
c<strong>on</strong>tour. Obstructi<strong>on</strong> is manifested by proximal<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> dilatati<strong>on</strong>.<br />
rett’s esophagus, between 20% and<br />
40%. 30 Patients with reflux esophagitis<br />
al<strong>on</strong>e have about a 10% risk <str<strong>on</strong>g>of</str<strong>on</strong>g> Barrett’s<br />
esophagus. 30 C<strong>on</strong>versely, a very<br />
low risk <str<strong>on</strong>g>of</str<strong>on</strong>g> Barrett’s esophagus is present<br />
if the <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> mucosa is<br />
smooth, if a stricture is not seen, and if<br />
<strong>on</strong>ly gastro<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> reflux or a<br />
hiatal hernia is present.<br />
Schatzki rings are <str<strong>on</strong>g>of</str<strong>on</strong>g> unknown etiology,<br />
possibly related to gastro<str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
reflux. They are thin (1 to<br />
3 mm in thickness), symmetric rings<br />
at the esophagogastric juncti<strong>on</strong>, frequently<br />
seen above a small hiatal hernia<br />
(figure 15). 31 Schatzki rings are<br />
best dem<strong>on</strong>strated in the pr<strong>on</strong>e positi<strong>on</strong><br />
and are sometimes detected <strong>on</strong>ly<br />
with a solid bolus. 32 Rings
FIGURE 16. Esophageal intramural pseudodiverticulosis.<br />
This patient has a l<strong>on</strong>g,<br />
tapered mid<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> stricture (large<br />
arrow). Many small flask-like outpouchings<br />
(“pseudodiverticula”) are seen lateral to the<br />
barium-filled <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> lumen (representative<br />
outpouchings identified by small arrows).<br />
pouchings are associated with a l<strong>on</strong>g<br />
cervical or upper thoracic <str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
stricture (figure 16). 33 In the more<br />
comm<strong>on</strong> form <str<strong>on</strong>g>of</str<strong>on</strong>g> <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> intramural<br />
pseudodiverticulosis, however,<br />
the outpouchings are associated with a<br />
short, distal, reflux-induced stricture. 34<br />
Primary or metastatic cancers are<br />
frequent causes <str<strong>on</strong>g>of</str<strong>on</strong>g> mid<str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
strictures. Some squamous cell carcinomas<br />
have an el<strong>on</strong>gated, circumferentially<br />
infiltrating appearance (figure<br />
12). An eccentric, annular lesi<strong>on</strong> may<br />
be seen with a coarsely lobulated c<strong>on</strong>tour<br />
and barium trapped within tumor<br />
nodules. Adenocarcinomas <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
esophagus arise in dysplastic columnar<br />
epithelium within Barrett’s<br />
October 2001<br />
FIGURE 17. Subcarinal lymph node metastases<br />
from breast carcinoma. Spot image <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the midesophagus obtained with the patient<br />
in a near lateral positi<strong>on</strong> dem<strong>on</strong>strates a<br />
smooth-surfaced mass pressing <strong>on</strong> the<br />
subcarinal esophagus.<br />
mucosa. Adenocarcinomas are found<br />
most frequently in the distal esophagus.<br />
Adenocarcinomas can have an<br />
infiltrative (figure 14), plaque-like<br />
(figure 13), ulcerative, or polypoid<br />
appearance. Unlike squamous cell<br />
carcinomas, adenocarcinomas have a<br />
marked tendency to invade the gastric<br />
cardia and fundus. Metastases to the<br />
esophagus most frequently involve<br />
the subcarinal regi<strong>on</strong> due to direct<br />
invasi<strong>on</strong> by tumor from subcarinal<br />
lymph nodes (figure 17) or from the<br />
left mainstem br<strong>on</strong>chus.<br />
Polypoid intraluminal masses<br />
A wide variety <str<strong>on</strong>g>of</str<strong>on</strong>g> polypoid masses<br />
are seen in the esophagus (Table 5). 35-41<br />
Table 5. Causes <str<strong>on</strong>g>of</str<strong>on</strong>g> polypoid<br />
intraluminal masses<br />
Benign<br />
Foreign body<br />
Inflammatory esophagogastric<br />
polyp<br />
Squamous papilloma<br />
Fibrovascular polyp<br />
Leiomyoma<br />
Malignant<br />
Squamous cell carcinoma<br />
Adenocarcinoma<br />
Spindle cell carcinoma<br />
Small cell carcinoma<br />
Primary malignant melanoma<br />
Polypoid masses are dem<strong>on</strong>strated<br />
radiographically as radiolucent filling<br />
defects in the barium pool (figure 18)<br />
or as barium-etched lines within the<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> lumen. Polypoid masses<br />
must first be distinguished from foreign<br />
bodies (figure 19). The clinical<br />
history is crucial for the <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
foreign bodies. These patients typically<br />
complain <str<strong>on</strong>g>of</str<strong>on</strong>g> abrupt-<strong>on</strong>set dysphagia<br />
or odynophagia during eating<br />
and the sensati<strong>on</strong> that food is stuck in<br />
the substernal regi<strong>on</strong>. The polypoid<br />
filling defect <str<strong>on</strong>g>of</str<strong>on</strong>g> the foreign body may<br />
be associated with an irregular meniscus<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> barium superiorly. Perforati<strong>on</strong><br />
is uncomm<strong>on</strong>, usually occurring after<br />
the impacti<strong>on</strong> has been present l<strong>on</strong>ger<br />
than 24 hours. A repeat esophagram<br />
should be performed after the foreign<br />
body has been removed to exclude an<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> stricture or motor disorder<br />
as the cause <str<strong>on</strong>g>of</str<strong>on</strong>g> the food impacti<strong>on</strong>.<br />
Squamous papillomas are the most<br />
comm<strong>on</strong> benign mucosal tumor <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
esophagus (figure 18), appearing as<br />
small, sessile, slightly lobulated<br />
polyps. The esophagus is <strong>on</strong>e organ <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the gastrointestinal tract in which true<br />
leiomyomas form. Most tumors arising<br />
in the mesenchyme are undifferentiated<br />
gastrointestinal stromal<br />
tumors <str<strong>on</strong>g>of</str<strong>on</strong>g> unknown malignant potential.<br />
Leiomyomas, however, are true<br />
APPLIED RADIOLOGY ■ 19
FIGURE 18. Squamous papilloma. A<br />
pedunculated polyp (thick arrow) is seen in<br />
the barium pool. Barium fills the interstices<br />
(thin arrow) <str<strong>on</strong>g>of</str<strong>on</strong>g> the head <str<strong>on</strong>g>of</str<strong>on</strong>g> the polyp. The<br />
pedicle (arrowhead) has a smooth surface.<br />
Pedunculated polyps are typically squamous<br />
papillomas or adenomatous polyps<br />
arising in Barrett’s mucosa. (Reproduced<br />
with permissi<strong>on</strong> from Rubesin SE. Gallery<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> double c<strong>on</strong>trast terminology. Gastro Clin<br />
North Am. 1995;24:259-288. 23 )<br />
proliferati<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> smooth muscle and<br />
are the most comm<strong>on</strong> submucosal<br />
mass in the esophagus. Granular cell<br />
tumors are another rare cause <str<strong>on</strong>g>of</str<strong>on</strong>g> submucosal<br />
masses in the esophagus. 36<br />
Polyps at the esophagogastric juncti<strong>on</strong><br />
are frequently related to chr<strong>on</strong>ic<br />
gastro<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> reflux <str<strong>on</strong>g>disease</str<strong>on</strong>g>, termed<br />
“inflammatory esophagogastric” or<br />
“sentinel” polyps. 40 These polyps are<br />
smooth-surfaced enlargements atop a<br />
thickened rugal fold at the gastric car-<br />
FIGURE 19. Kielbasa stuck in the esophagus<br />
above an <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> stricture. A triangular<br />
radiolucent filling defect with an<br />
irregular c<strong>on</strong>tour (black arrow) lies proximal<br />
to a smooth, tapered stricture (white arrow)<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> the distal esophagus. With the patient<br />
standing in an erect positi<strong>on</strong>, the presence<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> a hiatal hernia (H) indicates <str<strong>on</strong>g>esophageal</str<strong>on</strong>g><br />
shortening. This patient with l<strong>on</strong>g-standing<br />
gastro<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> reflux symptoms had<br />
been eating a sausage. The stricture was<br />
discovered at the time <str<strong>on</strong>g>of</str<strong>on</strong>g> the food impacti<strong>on</strong>.<br />
dia. If any surface irregularity is seen,<br />
however, endoscopy must be performed<br />
to exclude a malignant tumor at<br />
the cardia or in Barrett’s esophagus.<br />
Some squamous cell carcinomas<br />
have a polypoid (figure 20) rather than<br />
infiltrating appearance. 38,39 Small cell<br />
carcinomas are rare tumors that typically<br />
manifest as small, centrally<br />
ulcerated masses in the midesophagus.<br />
37 Spindle cell carcinomas are usually<br />
large, polypoid masses that<br />
FIGURE 20. Polypoid squamous cell carcinoma.<br />
A 1.5-cm lobulated lesi<strong>on</strong> (arrow)<br />
arises from the left anterolateral wall <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
midesophagus.<br />
expand the <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> lumen without<br />
causing significant obstructi<strong>on</strong>. 39<br />
Despite the relatively n<strong>on</strong>infiltrating<br />
appearance <str<strong>on</strong>g>of</str<strong>on</strong>g> spindle cell carcinomas,<br />
5-year survival rates in these<br />
patients are as dismal as in those<br />
patients with squamous cell carcinomas.<br />
Rarely, primary malignant<br />
melanoma <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus may be<br />
manifest as a bulky, polypoid intraluminal<br />
mass indistinguishable from<br />
spindle cell carcinoma. 41 AR<br />
20 ■ APPLIED RADIOLOGY October 2001
REFERENCES<br />
1. Levine MS, Laufer I. Esophagus. In: Levine<br />
MS, Rubesin SE, Laufer I. Double C<strong>on</strong>trast Gastrointestinal<br />
Radiology. 3rd ed. Philadelphia: WB<br />
Saunders Co; 2000:90-126.<br />
2. Levine MS. Radiology <str<strong>on</strong>g>of</str<strong>on</strong>g> esophagitis: A pattern<br />
approach. Radiology. 1991;179:1-7.<br />
3. Rubesin SE, Laufer I. Pictorial glossary <str<strong>on</strong>g>of</str<strong>on</strong>g> double<br />
c<strong>on</strong>trast radiology. In: Gore RM, Levine MS<br />
(eds). Textbook <str<strong>on</strong>g>of</str<strong>on</strong>g> Gastrointestinal Radiology. 2nd<br />
ed. Philadelphia: WB Saunders Co; 2000:44-66.<br />
4. Levine MS, Laufer I, Kressel HY, Friedman<br />
HM. Herpes esophagitis. AJR Am J Roentgenol.<br />
1981;136:863-866.<br />
5. Levine MS, Loevner LA, Saul SH, et al. Herpes<br />
esophagitis: Sensitivity <str<strong>on</strong>g>of</str<strong>on</strong>g> double-c<strong>on</strong>trast <strong>esophagography</strong>.<br />
AJR Am J Roentgenol. 1988;151:57-62.<br />
6. Rubesin SE, Levine MS, Laufer I. Odynophagia.<br />
In: Thomps<strong>on</strong> WM, ed. Comm<strong>on</strong> Problems in<br />
Gastrointestinal Radiology. Chicago: Year Book<br />
Medical Publishers; 1989:108-117.<br />
7. Shortsleeve MJ, Levine MS. Herpes esophagitis<br />
in otherwise healthy patients: Clinical and radiographic<br />
findings. Radiology. 1992;182:859-861.<br />
8. Creteur V, Laufer I, Kressel HY, et al. Druginduced<br />
esophagitis detected by double-c<strong>on</strong>trast<br />
radiography. Radiology. 1983;147:365-368.<br />
9. Bova JG, Dutt<strong>on</strong> NE, Goldstein HM, Hoberman<br />
LJ. Medicati<strong>on</strong>-induced esophagitis: Diagnosis by<br />
double c<strong>on</strong>trast <strong>esophagography</strong>. AJR Am J<br />
Roentgenol. 1987;148:731-732.<br />
10. Gohel V, L<strong>on</strong>g BW, Richter G. Aphthous<br />
ulcers in the esophagus with Crohn colitis. AJR<br />
Am J Roentgenol. 1981;137:872-873.<br />
11. Collazzo LA, Levine MS, Rubesin SE, Laufer I.<br />
Acute radiati<strong>on</strong> esophagitis: Radiographic findings.<br />
AJR Am J Roentgenol. 1997;169:1067-1070.<br />
12. Levine MS. Drug-induced disorders <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
esophagus. Abdom Imaging. 1999;24:3-8.<br />
13. Levine MS, Loercher G, Katzka DA, et al.<br />
Giant HIV-related ulcers in the esophagus. Radiology.<br />
1991;180:323-326.<br />
14. Sor S, Levine MS, Kowalski TE, et al. Giant<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> ulcers in HIV-positive patients: Clinical,<br />
radiographic and pathologic findings. Radiol-<br />
October 2001<br />
ogy. 1995;194:447-451.<br />
15. Levine MS, Woldenberg R, Herlinger H, Laufer<br />
I. Opportunistic esophagitis in AIDS: Radiographic<br />
<str<strong>on</strong>g>diagnosis</str<strong>on</strong>g>. Radiology. 1987;165:815-820.<br />
16. Balthazar EJ, Megibow AJ, Hulnick D, et al.<br />
Cytomegalovirus esophagitis in AIDS: Radiographic<br />
features in 16 patients. AJR Am J<br />
Roentgenol. 1987;149:919-923.<br />
17. Gloyna RE, Zornoza J, Goldstein HM: Primary<br />
ulcerative carcinoma <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus.<br />
AJR Am J Roentgenol. 1977;129:599-600.<br />
18. Levine MS, Rothstein RD, Laufer I. Giant<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> ulcer due to Clinoril. AJR Am J<br />
Roentgenol. 1991;156:955-956.<br />
19. Levine MS, Mac<strong>on</strong>es AJ, Laufer I. Candida<br />
esophagitis: Accuracy <str<strong>on</strong>g>of</str<strong>on</strong>g> radiographic <str<strong>on</strong>g>diagnosis</str<strong>on</strong>g>.<br />
Radiology. 1985;154:581-587.<br />
20. Berliner L, Redm<strong>on</strong>d P, Horowitz L, Ru<str<strong>on</strong>g>of</str<strong>on</strong>g>f M.<br />
Glycogen plaques (glycogenic acanthosis) <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
esophagus. Radiology. 1981;141:607-610.<br />
21. Glick SN, Teplick SK, Goldstein J, et al.<br />
Glycogenic acanthosis <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus. AJR<br />
Am J Roentgenol. 1982;139:683-688.<br />
22. Graziani L, Bearzi I, Romagnoli A, et al. Significance<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> diffuse granularity and nodularity <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> mucosa at double-c<strong>on</strong>trast radiography.<br />
Gastrointest Radiol. 1985;10:1-6.<br />
23. Rubesin SE. Gallery <str<strong>on</strong>g>of</str<strong>on</strong>g> double c<strong>on</strong>trast terminology.<br />
Gastro Clin North Am. 1995;24:259-288.<br />
24. Levine MS, Cajade AG, Herlinger H, Laufer I.<br />
Pseudomembranes in reflux esophagitis. Radiology.<br />
1986;159:43-45.<br />
25. Itai Y, Kogure T, Okuyama Y, Akiyama H.<br />
Superficial <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> carcinoma: Radiological<br />
findings in double-c<strong>on</strong>trast studies. Radiology.<br />
1978;126:597-601.<br />
26. Levine MS, Dill<strong>on</strong> EC, Saul SH, Laufer I. Early<br />
<str<strong>on</strong>g>esophageal</str<strong>on</strong>g> cancer. AJR Am J Roentgenol.<br />
1986;146:507-512.<br />
27. Levine MS, Kressel HY, Caroline D, et al. Barrett<br />
esophagus: Reticular pattern <str<strong>on</strong>g>of</str<strong>on</strong>g> the mucosa.<br />
Radiology. 1983;147:663-667.<br />
28. Yates CW, LeVine MA, Jensen KM. Varicoid<br />
carcinoma <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus. Radiology.<br />
1977;122:605-608.<br />
29. Levine MS, Borislow SM, Rubesin SE,<br />
O'Brien C. Proximal <str<strong>on</strong>g>esophageal</str<strong>on</strong>g> stricture caused<br />
by Motrin. Abdom Imaging. 1994;19:6-7.<br />
30. Gilchrist AM, Levine MS, Carr RF, et al. Barrett’s<br />
esophagus: Diagnosis by double-c<strong>on</strong>trast<br />
<strong>esophagography</strong>. AJR Am J Roentgenol.<br />
1988;150:97-102.<br />
31. Levine MS, Rubesin SE. Radiologic investigati<strong>on</strong><br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> dysphagia. AJR Am J Roentgenol.<br />
1990;154:1157-1163.<br />
32. Low VHS, Rubesin SE. C<strong>on</strong>trast evaluati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the pharynx and esophagus. Rad Clin North Am.<br />
1993;31:1265-1291.<br />
33. Cho SR, Sanders MM, Turner MA, et al.<br />
Esophageal intramural pseudodiverticulosis.<br />
Gastrointest Radiol. 1981;5:9-16.<br />
34. Levine MS, Moolten DN, Herlinger H, Laufer I.<br />
Esophageal intramural pseudodiverticulosis: A<br />
reevaluati<strong>on</strong>. AJR Am J Roentgenol. 1986;147:1165-<br />
1170.<br />
35. Olmsted WW, Lichtenstein JE, Hyams VJ.<br />
Polypoid epithelial malignancies <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus.<br />
AJR Am J Roentgenol. 1983;140:921-925.<br />
36. Rubesin SE, Herlinger H, Sigal H. Granular<br />
cell tumors <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus. Gastrointest Radiology.<br />
1985;10:11-15.<br />
37. Levine MS, Pant<strong>on</strong>grag-Brown L, Buck JL, et<br />
al. Small-cell carcinoma <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus: Radiographic<br />
findings. Radiology. 1996;199:703-705.<br />
38. Levine MS, Laufer I, Yamada A. Tumors <str<strong>on</strong>g>of</str<strong>on</strong>g><br />
the esophagus. In: Levine MS, Rubesin SE,<br />
Laufer I. Double C<strong>on</strong>trast Gastrointestinal Radiology.<br />
3rd ed. Philadelphia: WB Saunders Co;<br />
2000:126-148.<br />
39. Levine MS. Other malignant tumors <str<strong>on</strong>g>of</str<strong>on</strong>g> the<br />
esophagus. In: Gore RM, Levine MS (eds). Textbook<br />
<str<strong>on</strong>g>of</str<strong>on</strong>g> Gastrointestinal Radiology. 2nd ed.<br />
Philadelphia: WB Saunders Co; 2000:435-451.<br />
40. Bleshman MH, Banner MP, Johns<strong>on</strong> RC, et<br />
al. The inflammatory esophagogastric juncti<strong>on</strong><br />
polyp and fold. Radiology. 1978;128: 589-593.<br />
41. Yoo CC, Levine MS, McLarney JK, Lowry MA.<br />
Primary malignant melanoma <str<strong>on</strong>g>of</str<strong>on</strong>g> the esophagus:<br />
Radiographic findings in seven patients. Radiology.<br />
1998;209:455-459.<br />
APPLIED RADIOLOGY ■ 21