Quantifying the material and structural determinants of bone strength
Quantifying the material and structural determinants of bone strength
Quantifying the material and structural determinants of bone strength
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
746<br />
M.L. Bouxsein, E. Seeman / Best Practice & Research Clinical Rheumatology 23 (2009) 741–753<br />
ranelate is incorporated into <strong>the</strong> mineral substance <strong>of</strong> <strong>bone</strong> [86], it is not known whe<strong>the</strong>r <strong>the</strong>se<br />
observations are true changes in <strong>bone</strong> morphology or artefacts due to altered edge-detection <strong>and</strong>/or<br />
partial volume effects.<br />
Altoge<strong>the</strong>r, HR-pQCT is promising for assessment <strong>of</strong> trabecular <strong>and</strong> cortical architecture in vivo with<br />
high precision. The disadvantages are that it requires specialised scanners, <strong>and</strong> measurements are<br />
limited to peripheral skeletal sites. Fur<strong>the</strong>rmore, motion artefacts are common, requiring re-scanning<br />
<strong>of</strong> many patients.<br />
Magnetic resonance imaging (MRI)<br />
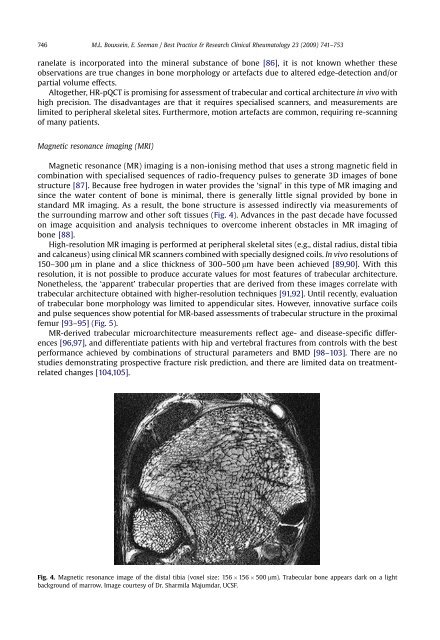
Magnetic resonance (MR) imaging is a non-ionising method that uses a strong magnetic field in<br />
combination with specialised sequences <strong>of</strong> radio-frequency pulses to generate 3D images <strong>of</strong> <strong>bone</strong><br />
structure [87]. Because free hydrogen in water provides <strong>the</strong> ‘signal’ in this type <strong>of</strong> MR imaging <strong>and</strong><br />
since <strong>the</strong> water content <strong>of</strong> <strong>bone</strong> is minimal, <strong>the</strong>re is generally little signal provided by <strong>bone</strong> in<br />
st<strong>and</strong>ard MR imaging. As a result, <strong>the</strong> <strong>bone</strong> structure is assessed indirectly via measurements <strong>of</strong><br />
<strong>the</strong> surrounding marrow <strong>and</strong> o<strong>the</strong>r s<strong>of</strong>t tissues (Fig. 4). Advances in <strong>the</strong> past decade have focussed<br />
on image acquisition <strong>and</strong> analysis techniques to overcome inherent obstacles in MR imaging <strong>of</strong><br />
<strong>bone</strong> [88].<br />
High-resolution MR imaging is performed at peripheral skeletal sites (e.g., distal radius, distal tibia<br />
<strong>and</strong> calcaneus) using clinical MR scanners combined with specially designed coils. In vivo resolutions <strong>of</strong><br />
150–300 mm in plane <strong>and</strong> a slice thickness <strong>of</strong> 300–500 mm have been achieved [89,90]. With this<br />
resolution, it is not possible to produce accurate values for most features <strong>of</strong> trabecular architecture.<br />
None<strong>the</strong>less, <strong>the</strong> ‘apparent’ trabecular properties that are derived from <strong>the</strong>se images correlate with<br />
trabecular architecture obtained with higher-resolution techniques [91,92]. Until recently, evaluation<br />
<strong>of</strong> trabecular <strong>bone</strong> morphology was limited to appendicular sites. However, innovative surface coils<br />
<strong>and</strong> pulse sequences show potential for MR-based assessments <strong>of</strong> trabecular structure in <strong>the</strong> proximal<br />
femur [93–95] (Fig. 5).<br />
MR-derived trabecular microarchitecture measurements reflect age- <strong>and</strong> disease-specific differences<br />
[96,97], <strong>and</strong> differentiate patients with hip <strong>and</strong> vertebral fractures from controls with <strong>the</strong> best<br />
performance achieved by combinations <strong>of</strong> <strong>structural</strong> parameters <strong>and</strong> BMD [98–103]. There are no<br />
studies demonstrating prospective fracture risk prediction, <strong>and</strong> <strong>the</strong>re are limited data on treatmentrelated<br />
changes [104,105].<br />
Fig. 4. Magnetic resonance image <strong>of</strong> <strong>the</strong> distal tibia (voxel size: 156 156 500 mm). Trabecular <strong>bone</strong> appears dark on a light<br />
background <strong>of</strong> marrow. Image courtesy <strong>of</strong> Dr. Sharmila Majumdar, UCSF.