Management of pregnancy - VA/DoD Clinical Practice Guidelines ...
Management of pregnancy - VA/DoD Clinical Practice Guidelines ...
Management of pregnancy - VA/DoD Clinical Practice Guidelines ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>VA</strong>/<strong>DoD</strong> <strong>Clinical</strong> <strong>Practice</strong> Guideline<br />
For Pregnancy <strong>Management</strong><br />
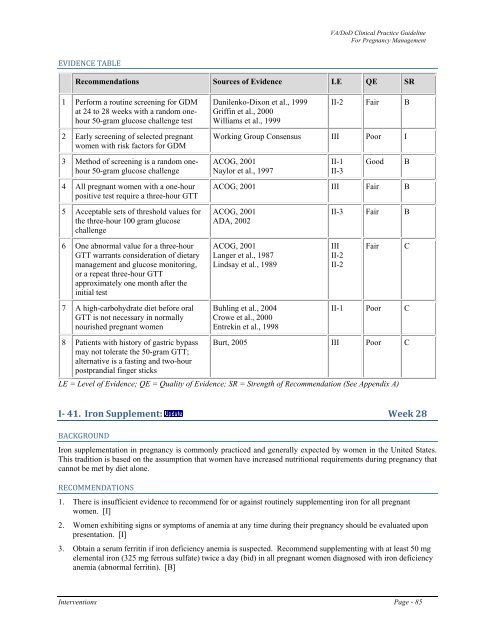
EVIDENCE TABLE<br />
Recommendations Sources <strong>of</strong> Evidence LE QE SR<br />
1 Perform a routine screening for GDM<br />
at 24 to 28 weeks with a random onehour<br />
50-gram glucose challenge test<br />
Danilenko-Dixon et al., 1999<br />
Griffin et al., 2000<br />
Williams et al., 1999<br />
II-2 Fair B<br />
2 Early screening <strong>of</strong> selected pregnant<br />
women with risk factors for GDM<br />
Working Group Consensus III Poor I<br />
3 Method <strong>of</strong> screening is a random onehour<br />
50-gram glucose challenge<br />
ACOG, 2001<br />
Naylor et al., 1997<br />
II-1<br />
II-3<br />
Good<br />
B<br />
4 All pregnant women with a one-hour<br />
positive test require a three-hour GTT<br />
ACOG, 2001 III Fair B<br />
5 Acceptable sets <strong>of</strong> threshold values for<br />
the three-hour 100 gram glucose<br />
challenge<br />
ACOG, 2001<br />
ADA, 2002<br />
II-3 Fair B<br />
6 One abnormal value for a three-hour<br />
GTT warrants consideration <strong>of</strong> dietary<br />
management and glucose monitoring,<br />
or a repeat three-hour GTT<br />
approximately one month after the<br />
initial test<br />
ACOG, 2001<br />
Langer et al., 1987<br />
Lindsay et al., 1989<br />
III<br />
II-2<br />
II-2<br />
Fair<br />
C<br />
7 A high-carbohydrate diet before oral<br />
GTT is not necessary in normally<br />
nourished pregnant women<br />
Buhling et al., 2004<br />
Crowe et al., 2000<br />
Entrekin et al., 1998<br />
II-1 Poor C<br />
8 Patients with history <strong>of</strong> gastric bypass Burt, 2005 III Poor C<br />
may not tolerate the 50-gram GTT;<br />
alternative is a fasting and two-hour<br />
postprandial finger sticks<br />
LE = Level <strong>of</strong> Evidence; QE = Quality <strong>of</strong> Evidence; SR = Strength <strong>of</strong> Recommendation (See Appendix A)<br />
I 41. Iron Supplement: Week 28<br />
BACKGROUND<br />
Iron supplementation in <strong>pregnancy</strong> is commonly practiced and generally expected by women in the United States.<br />
This tradition is based on the assumption that women have increased nutritional requirements during <strong>pregnancy</strong> that<br />
cannot be met by diet alone.<br />
RECOMMENDATIONS<br />
1. There is insufficient evidence to recommend for or against routinely supplementing iron for all pregnant<br />
women. [I]<br />
2. Women exhibiting signs or symptoms <strong>of</strong> anemia at any time during their <strong>pregnancy</strong> should be evaluated upon<br />
presentation. [I]<br />
3. Obtain a serum ferritin if iron deficiency anemia is suspected. Recommend supplementing with at least 50 mg<br />
elemental iron (325 mg ferrous sulfate) twice a day (bid) in all pregnant women diagnosed with iron deficiency<br />
anemia (abnormal ferritin). [B]<br />
Interventions Page - 85