Management of pregnancy - VA/DoD Clinical Practice Guidelines ...
Management of pregnancy - VA/DoD Clinical Practice Guidelines ...
Management of pregnancy - VA/DoD Clinical Practice Guidelines ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>VA</strong>/<strong>DoD</strong> <strong>Clinical</strong> <strong>Practice</strong> Guideline<br />
For Pregnancy <strong>Management</strong><br />
et al., 1982). A decrease in fetal movement may indicate fetal jeopardy and should immediately prompt the<br />
pregnant woman to seek further evaluation <strong>of</strong> fetal well-being.<br />
RECOMMENDATIONS<br />
1. Recommend instructing all pregnant women about the importance <strong>of</strong> assessing fetal movement on a daily basis<br />
beginning in the third trimester. [B]<br />
2. Recommend instructing all pregnant women as to the course <strong>of</strong> action they should take if they do not perceive<br />
the minimum fetal movement counts within the time frame specific to their healthcare facility.<br />
DISCUSSION<br />
Fetal movement counting is by far the oldest and simplest <strong>of</strong> all fetal assessment techniques. In Moore and<br />
Piacquadio’s (1989) study <strong>of</strong> 2,519 pregnant women, the fetal mortality rate was 8.7/1,000 among women who had<br />
no instruction in formal daily fetal movement assessment, and fell to 2.1/1,000 when women: 1) kept a record <strong>of</strong><br />
how long it took to feel 10 fetal movements, and 2) took prompt action to seek further evaluation <strong>of</strong> fetal well-being<br />
when they did not perceive 10 movements within a two-hour time frame. In contrast, Grant and Hepburn (1984) did<br />
not observe significant differences in unexplained fetal death between counting and non-counting groups <strong>of</strong> women,<br />
but did note that there seemed to be a time period <strong>of</strong> decreased fetal movement prior to actual fetal death. Most data<br />
suggest an improvement in perinatal outcomes with the early identification <strong>of</strong> decreased fetal activity (Moore &<br />
Piacquadio, 1989; Neldam, 1980; Pearson & Weaver, 1976; Sad<strong>of</strong>sky & Yaffe, 1973).<br />
Many methods <strong>of</strong> counting fetal movements have been proposed. Most research supports the idea that compliance<br />
among low-risk pregnant women is highest when the monitoring method is minimally time-consuming and<br />
relatively simple (Davis, 1987). The number <strong>of</strong> fetal movements perceived is arbitrary, though some studies suggest<br />
that the perceived lack <strong>of</strong> fetal movement for two hours or more requires further evaluation (Connors et al., 1988;<br />
Moore & Piacquadio, 1989; Wilailak et al., 1992).<br />
Most authorities agree that once a decrease in fetal movement is reported, further and prompt investigation is<br />
warranted, usually via external fetal monitoring. It is imperative then, that women are given relevant information to<br />
assist them in recognizing warning signs <strong>of</strong> potential fetal compromise.<br />
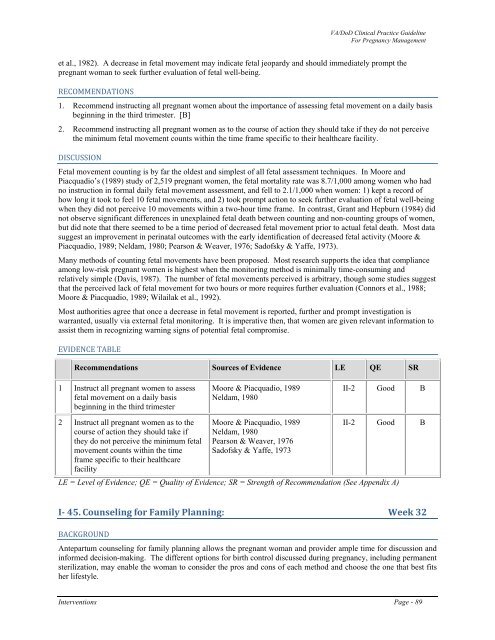
EVIDENCE TABLE<br />
Recommendations Sources <strong>of</strong> Evidence LE QE SR<br />
1 Instruct all pregnant women to assess<br />
fetal movement on a daily basis<br />
beginning in the third trimester<br />
Moore & Piacquadio, 1989<br />
Neldam, 1980<br />
II-2 Good B<br />
2 Instruct all pregnant women as to the<br />
course <strong>of</strong> action they should take if<br />
they do not perceive the minimum fetal<br />
movement counts within the time<br />
frame specific to their healthcare<br />
facility<br />
Moore & Piacquadio, 1989<br />
Neldam, 1980<br />
Pearson & Weaver, 1976<br />
Sad<strong>of</strong>sky & Yaffe, 1973<br />
II-2 Good B<br />
LE = Level <strong>of</strong> Evidence; QE = Quality <strong>of</strong> Evidence; SR = Strength <strong>of</strong> Recommendation (See Appendix A)<br />
I 45. Counseling for Family Planning: Week 32<br />
BACKGROUND<br />
Antepartum counseling for family planning allows the pregnant woman and provider ample time for discussion and<br />
informed decision-making. The different options for birth control discussed during <strong>pregnancy</strong>, including permanent<br />
sterilization, may enable the woman to consider the pros and cons <strong>of</strong> each method and choose the one that best fits<br />
her lifestyle.<br />
Interventions Page - 89