Management of pregnancy - VA/DoD Clinical Practice Guidelines ...
Management of pregnancy - VA/DoD Clinical Practice Guidelines ...
Management of pregnancy - VA/DoD Clinical Practice Guidelines ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>VA</strong>/<strong>DoD</strong> <strong>Clinical</strong> <strong>Practice</strong> Guideline<br />
For Pregnancy <strong>Management</strong><br />
Visits During Weeks: 3841<br />
I 48. Consider Weekly Cervical Check/stripping (sweeping): Weeks 3841<br />
BACKGROUND<br />
Post-dates pregnancies (over 42 weeks) occur in 10 percent <strong>of</strong> uncomplicated pregnant women. Post-dates<br />
pregnancies have a higher incidence <strong>of</strong> induction <strong>of</strong> labor, operative delivery, post-partum hemorrhage and shoulder<br />
dystocia. Routine membrane stripping, in low-risk pregnant women with accurate dating criteria, has been proposed<br />
as a method <strong>of</strong> encouraging earlier delivery to prevent post-dates <strong>pregnancy</strong>.<br />
RECOMMENDATIONS<br />
1. Consider <strong>of</strong>fering routine membrane sweeping to all pregnant women every visit beginning at 38 weeks. [C]<br />
2. There is insufficient data to encourage or discourage this practice in women known to be GBS-colonized. [I]<br />
DISCUSSION<br />
Membrane sweeping lessens the incidence <strong>of</strong> post-dates pregnancies and the need for medical inductions (NNT = 8)<br />
(Boulvain et al., 2005). A well-done meta-analysis <strong>of</strong> randomized trials found no harm regarding neonatal<br />
morbidity/mortality if women undergo routine weekly “membrane stripping” beginning at 38 weeks’ gestation<br />
(Boulvain et al., 1999 & 2001, 2005). No “serious maternal morbidity/mortality,” increased cesarean-sections,<br />
instrumental delivery rates, or maternal infection was found. ACOG (2002) states that the risks <strong>of</strong> membrane<br />
stripping in women colonized with GBS “have not been investigated in well-designed prospective studies.<br />
Therefore data are insufficient to encourage or discourage this practice in women known to be GBS-colonized.”<br />
Membrane sweeping in women who are positive GBS carriers may increase susceptibility to litigation in the event<br />
<strong>of</strong> a GBS-related adverse fetal/neonatal outcome despite the fact that randomized trials found no harm regarding<br />
increased neonatal or maternal morbidity/mortality (Cohen & Goldberg, 2006).<br />
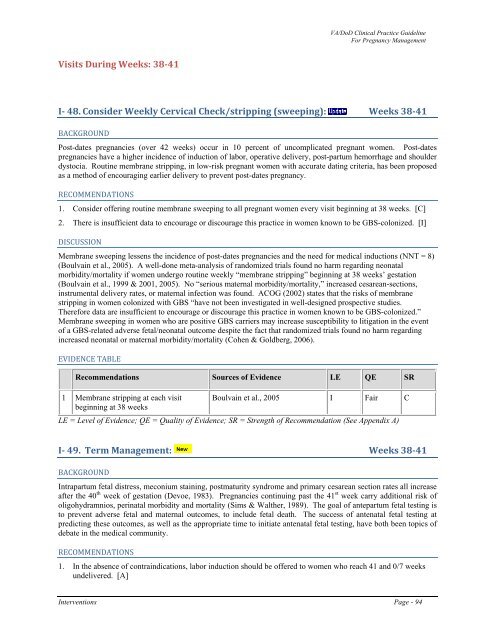
EVIDENCE TABLE<br />
Recommendations Sources <strong>of</strong> Evidence LE QE SR<br />
1 Membrane stripping at each visit Boulvain et al., 2005 I Fair C<br />
beginning at 38 weeks<br />
LE = Level <strong>of</strong> Evidence; QE = Quality <strong>of</strong> Evidence; SR = Strength <strong>of</strong> Recommendation (See Appendix A)<br />
I 49. Term <strong>Management</strong>: Weeks 3841<br />
BACKGROUND<br />
Intrapartum fetal distress, meconium staining, postmaturity syndrome and primary cesarean section rates all increase<br />
after the 40 th week <strong>of</strong> gestation (Devoe, 1983). Pregnancies continuing past the 41 st week carry additional risk <strong>of</strong><br />
oligohydramnios, perinatal morbidity and mortality (Sims & Walther, 1989). The goal <strong>of</strong> antepartum fetal testing is<br />
to prevent adverse fetal and maternal outcomes, to include fetal death. The success <strong>of</strong> antenatal fetal testing at<br />
predicting these outcomes, as well as the appropriate time to initiate antenatal fetal testing, have both been topics <strong>of</strong><br />
debate in the medical community.<br />
RECOMMENDATIONS<br />
1. In the absence <strong>of</strong> contraindications, labor induction should be <strong>of</strong>fered to women who reach 41 and 0/7 weeks<br />
undelivered. [A]<br />
Interventions Page - 94