2013 Employee Benefits Guidebook - Administration Home
2013 Employee Benefits Guidebook - Administration Home
2013 Employee Benefits Guidebook - Administration Home
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
EMPLOYEE BENEFITS<br />
Open Enrollment<br />
GUIDEBOOK<br />
A comprehensive guide to your<br />
EMPLOYEE BENEFITS<br />
for the<br />
<strong>2013</strong><br />
Plan Year<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
EL PASO COUNTY’S<br />
EMPLOYEE BENEFITS GUIDEBOOK<br />
PLAN YEAR <strong>2013</strong><br />
PREFACE<br />
Your <strong>Benefits</strong> <strong>Guidebook</strong> is intended to provide information you need to assist with your<br />
employee benefit selections:<br />
<br />
<br />
<br />
<br />
<br />
The types of questions you can ask yourself to help you decide which plan(s) are best for<br />
you and your family;<br />
What benefits are available for the <strong>2013</strong> plan year;<br />
What administrative steps you must take to enroll;<br />
How to access your benefits;<br />
Where you can go to get more information or assistance regarding any of the plans<br />
offered by El Paso County.<br />
To take full advantage of the benefits, please take the time to fully consider each of the available<br />
benefit plan options explained in the guidebook.<br />
We have included a benefits telephone directory on the following page for your convenience<br />
when you have benefit questions. Please feel free to contact any of the vendors directly for any<br />
plan-related questions you may have now and throughout the year.<br />
If you have a general question regarding any of the benefit plans, please do not hesitate to call<br />
the EL Paso County EBMS Benefit Division at 719-520-7420, Monday-Friday, 8:00 a.m. to 5:00<br />
p.m.<br />
OPEN ENROLLMENT<br />
Please remember that open enrollment is the only time of the year that you may elect to make<br />
changes to benefit plans without having a Qualifying Life Event.<br />
ABOUT THE BENEFITS GUIDEBOOK<br />
This <strong>Guidebook</strong> is intended to provide a general overview of all the insurance benefit plans,<br />
including eligibility, cost, contact information and how to use your benefits. Should there be an<br />
inconsistency with any communications regarding these plans the actual Master Plan Documents<br />
will govern. Any information contained herein may be subject to change.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
PHONE DIRECTORY<br />
Employment, <strong>Benefits</strong>, and Medical Services Department<br />
<strong>Employee</strong> <strong>Benefits</strong> Division .......................................................................... 719 520-7420<br />
E-Mail ..................................................................................................ebms@elpasoco.com<br />
Workers Compensation Division.................................................................... 719 520-7486<br />
HIPAA Compliance........................................................................................ 719 520-7402<br />
Finance/Payroll Office<br />
Rhonda Wagoner ............................................................................................ 719 520-6427<br />
Debra Morrow................................................................................................. 719 520-7404<br />
Payroll Fax...................................................................................................... 719 520-6469<br />
Medical Plans<br />
Use the Member Service Number and Website below for Questions, Claims, ID Cards, and Pre-<br />
Authorizations<br />
<strong>Employee</strong> <strong>Benefits</strong> Management Services (EBMS) Member Services.......1-866-887-4115<br />
EBMS mi<strong>Benefits</strong> Website Address............................................................www.ebms.com<br />
Care Link Pre-Notification and Priority Maternity Care .............................1-866-894-1505<br />
Cofinity Medical Network Customer Service Number and Website<br />
Find a Provider.................................... www.cofinity.net/EPCDirectory/Index.aspx<br />
Cofinity Medical Provider Network Customer Service...................1-800-831-1166<br />
El Paso County <strong>Employee</strong> Health Centers<br />
Regional Development Center (RDC) Health Center..................................... 719 520-7080<br />
Customer Service Center (CSC) ..................................................................... 719 520-7600<br />
Prescription <strong>Benefits</strong><br />
Catamaran Rx Customer Service.................................................................1-800-207-2568<br />
Website .................................................................................................mycatamaranrx.com<br />
Mail Service Prescription Refills..............................1-800-RX-REFILL (1-800-797-3345)<br />
BriovaRx Specialty ........................................................................................1-800-850-9122<br />
Dental Plans<br />
Guardian Dental Member Services..............................................................1-800-541-7846<br />
Guardian Dental Web site...................................................... www.GuardianAnytime.com<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
Vision Plan<br />
EyeMed Vision Care Customer Service ......................................................1-866-723-0596<br />
EyeMed Vision Care Website................................................. www.eyemedvisioncare.com<br />
Flexible Spending Accounts<br />
PayFlex Customer Service: .........................................................................1-800-284-4885<br />
PayFlex Claim Fax Number: ...................................................................... 1-800-450-0016<br />
PayFlex Website .................................................................................. www.healthhub.com<br />
Reach Your Peak Health Management Program<br />
Reach Your Peak Program Questions email:..................... RYPsimplywell@elpasoco.com<br />
Program Website................................................................................ www.simplywell.com<br />
Website Technical Questions.......................................................................1-877-991-9355<br />
Wellness Reimbursement Account (WRA) Website........................... www.healthhub.com<br />
Wellness Reimbursement Account (WRA) Customer Service…………...1-800-284-4885<br />
<strong>Employee</strong> Assistance Program (EAP)<br />
ComPsych ...................................................................................................1-800-272-7255<br />
Website ..................................................www.guidanceresources.com Web ID COM589<br />
Life and Disability Insurance<br />
UNUM Life Insurance .……………………………………………………1-800-421-0344<br />
Plan Highlights & Forms ........http://w3.unum.com/enroll/ElPasoCounty/enrollment.aspx<br />
Short Term Disability (policy #907374) - to file a claim...................... 888 673-9940<br />
STD Fax ................................................................................................ 800 447-2498<br />
General Questions Contact the <strong>Employee</strong> <strong>Benefits</strong> Office .................. 719 520-7420<br />
El Paso County Retirement Plan<br />
Retirement Benefit Information...................................................................... 719 520-7490<br />
Internet Address...............................................................................www.epcretirement.org<br />
Deferred Compensation (457 Plan)<br />
Great West Retirement Services ..................................................................1-800-947-4409<br />
Key-Talk ......................................................................................................1-800-701-8255<br />
Web Site....................................................................................................... www.gwrs.com<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
IMPORTANT INFORMATION<br />
SUMMARY OF BENEFITS AND COVERAGE (SBC) AND SUMMARY PLAN<br />
DOCUMENTS (SPD): For a copy of the Summary of <strong>Benefits</strong> and Coverage and also the<br />
Summary Plan Documents contact the <strong>Employee</strong>, <strong>Benefits</strong> and Medical Services Department<br />
(EBMS) <strong>Benefits</strong> Division at (719) 520-7402, or go to www.elpasoco.com under the EBMS<br />
<strong>Benefits</strong> Division. This information is also available on Depot, the El Paso County Intranet site.<br />
ENROLLMENT AND EFFECTIVE DATE OF COVERAGE FOR MEDICAL, DENTAL,<br />
VISION AND LIFE INSURANCE BENEFITS: Eligible employees must complete the<br />
enrollment process (even if waiving coverage) through <strong>Employee</strong> Self Service (ESS) or by<br />
completing a Benefit Enrollment Form. <strong>Employee</strong>s enrolling for coverage agree to pay the<br />
required contributions. Dependents of an eligible employee may not be enrolled in the Medical,<br />
Dental and Vision plans unless the employee is also enrolled for coverage under the Plan.<br />
If both spouses are employees of El Paso County and both are eligible for benefits, you should<br />
carefully review the contribution rates and select the option that provides the best coverage for<br />
you and your family at the lowest total cost. If both parents of an eligible dependent child are<br />
enrolled as a subscriber, only one parent may enroll the child as a dependent.<br />
ELIGIBLE DEPENDENTS: Eligible dependents include your lawful spouse and children who<br />
are less than 26 years old. Dependent children are also covered if age 26 or more years old and<br />
primarily supported by you and incapable of self-sustaining employment by reason of mental or<br />
physical handicap. You may be required to provide proof of the child’s dependent status to the<br />
health care provider or to the EBMS <strong>Benefits</strong> Division.<br />
You must provide the social security number (SSN) for dependents enrolled on our medical plan.<br />
Federal law requires group health plans and claim administrators to provide reports to the<br />
Centers for Medicare & Medicaid Services (CMS). We understand that you may have concerns<br />
with sharing your SSN. However, federal law requires that we collect this information so that<br />
accurate reports can be provided to CMS. This information will be shared only for reporting<br />
directly to CMS. The medical administrator sends the reports to CMS using a secure data<br />
transmission method to ensure the privacy and security of your information.<br />
Documentation for any covered dependents is also a requirement. If an employee enrolls a<br />
spouse, a copy of the marriage certificate must be provided. If enrolling children, copies of birth<br />
certificates must also be provided. These persons are excluded as Dependents: other<br />
individuals living in the covered <strong>Employee</strong>'s home, but who are not eligible as defined in the<br />
Summary Plan Document (SPD); the divorced former Spouse of the <strong>Employee</strong>; foster children;<br />
or any person who is covered under the Plan as an <strong>Employee</strong>. See the SPD for additional<br />
information on eligible classes of dependents.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
ENROLLMENT: Enrollment must be completed within 31 days of your full-time hire date. If<br />
you do not enroll within this 31 day period, you will not be eligible to enroll until the next open<br />
enrollment period, unless you have a Qualifying Life Event.<br />
Full-time employees are required to have medical coverage. Therefore, if you waive medical<br />
coverage offered by El Paso County, you must provide proof of other medical coverage.<br />
If you do not submit your enrollment for medical coverage within the first 31 days, or<br />
waive coverage and fail to provide proof of other medical insurance coverage, EBMS has<br />
the right to enroll you in the lowest medical plan option offered and you will be required to<br />
pay past due premiums. If you do not submit your enrollment for dental coverage, you will not<br />
be eligible for enrollment in a dental plan until the next dental plan Open Enrollment period.<br />
WHEN COVERAGE IS EFFECTIVE: If you are hired full-time starting from the 1 st through<br />
the 15 th of the month, coverage for you and any of your enrolled dependents is effective on the<br />
first day of the next month. If you are hired full-time starting the 16 th through the last day of the<br />
month, coverage for you and any of your enrolled dependents is effective on the first day of the<br />
second following month. (Example 1: First day of full-time employment is January 15 th ,<br />
coverage is effective February 1 st . Example 2: First day of full-time employment is January<br />
16 th , coverage is effective March 1 st .)<br />
In no event will health services be rendered or delivered before the effective date of coverage.<br />
WHEN COVERAGE ENDS: Coverage ends on the last day of the month that you separate<br />
employment, are no longer a full-time employee, the last day premiums are paid through, or<br />
when you no longer meet the eligibility requirements.<br />
ANNUAL OPEN ENROLLMENT: Every year each eligible employee is given an opportunity<br />
to change his or her benefit elections for the upcoming benefit plan year. Benefit elections made<br />
during the open enrollment period take effect January 1 st of the following calendar year. Changes<br />
to open enrollment elections will only be accepted if received by EBMS in writing by the last<br />
business day in December. After this date, changes can only be made during the plan year if you<br />
have a Qualifying Life Event (please see the Making Changes on the following page).<br />
BENEFIT PLAN YEAR: El Paso County’s “Plan Year” begins January 1 st and ends December<br />
31 st .<br />
CALENDAR YEAR DEDUCTIBLE: El Paso County’s “Calendar Year Deductible” begins<br />
January 1 st and ends December 31 st .<br />
PROVIDER AND FACILITY CONTRACTS: Although most physicians or providers and<br />
facilities that contract with our insurance plans remain with those network(s) year after year, you<br />
should always contact the plan vendor to verify that they are still participating in the plan<br />
network(s) and to verify if they are accepting new patients to ensure coverage.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
EMPLOYEE CONTRIBUTIONS AND POP: The employee medical, dental, vision and life<br />
insurance benefit contributions (see the monthly contribution schedule in this guidebook) are<br />
deducted the first and second pay period of each month through payroll deduction. (These<br />
deductions will not be taken when there is a third pay period in the month.) El Paso County<br />
health plans are Premium Only Plans (POP) allowing deductions to be taken on a pre-tax basis.<br />
With pre-tax deductions, you will not pay federal, state or social security taxes on these monies,<br />
but you may not claim your medical or dental premiums as a deduction on your Federal Income<br />
Tax Return. Because your taxable income will be smaller under the pre-tax method, your tax<br />
withholding will be less and your take home pay may be higher. A lower social security<br />
reportable income may lower your potential income from social security upon retirement.<br />
Unless you submit a written request for your contributions to be taken on after tax basis,<br />
contributions for health and/or dental premiums will automatically be deducted on a pre-tax<br />
basis.<br />
BENEFITS MAY BE TERMINATED FOR NON-PAYMENT OF BENEFIT PREMIUMS.<br />
ARRANGEMENT MUST BE MADE IN ADVANCE WITH THE EBMS BENEFITS<br />
DIVISION IF BENEFIT CONTRIBUTIONS ARE NOT DEDUCTED THROUGH<br />
PAYROLL (SUCH AS WHEN AN EMPLOYEE IS OFF WORK DUE TO WORKERS<br />
COMPENSATION, FMLA OR OTHER UNPAID LEAVE OF ABSENCE.) YOU WILL<br />
BE GIVEN 30 DAYS NOTICE EXCEPT IN CASES OF FRAUD OR INTENTIONAL<br />
MISREPRESENTATION.<br />
MAKING CHANGES – QUALIFYING LIFE EVENTS: If you have a qualifying life event as<br />
defined by the IRS you MUST submit a Benefit Change form directly to the EBMS <strong>Benefits</strong><br />
Division within 31 days of the life event effective date.<br />
The following is a list of Qualifying Life Events and the required documentation:<br />
Qualifying Life Event Required Documentation:<br />
• Marriage: Marriage Certificate<br />
• Dissolution of Marriage/Common Law: Divorce Decree<br />
• Divorce: Divorce Decree<br />
• Legal Separation: Court Decree<br />
• Annulment: Court Decree<br />
• Birth/Adoption/Custody of Dependent: Birth Certificate/Final Court Decree<br />
• Death of a Dependent: Death Certificate<br />
• Loss/Gain of Spousal Medical/Dental Coverage: Letter from Spouses Former Employer<br />
or Insurance Company<br />
• Ineligible Dependent: Proof of Age<br />
• Medicare Eligibility: Proof of Medicare Eligibility<br />
• Medicaid Eligibility for your Dependents: Proof of Medicaid Eligibility<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
Contact the EBMS <strong>Benefits</strong> Division with any questions regarding documentation.<br />
IF YOU DO NOT SUBMIT THE BENEFIT CHANGE FORM WITHIN THE 31-DAY<br />
PERIOD, YOU WILL NOT BE ALLOWED TO MAKE A CHANGE UNTIL THE NEXT<br />
OPEN ENROLLMENT PERIOD OR YOUR NEXT QUALIFYING LIFE EVENT. El<br />
Paso County can require you to provide documentation of your qualifying life event<br />
whenever you request changes.<br />
Failure to remove a dependent within 31 days of when the dependent is no longer eligible<br />
(i.e. divorce) will result in additional premiums due based on the COBRA rates and may be<br />
deducted through payroll.<br />
QUALIFYING LIFE EVENT EFFECTIVE DATE: Your new benefit elections made as a result<br />
of a Qualifying Life Event will take effect on the first day of the month coincident with or<br />
following the effective date of the Qualifying Life Event. Any benefit election changes must be<br />
consistent with the Qualifying Life Event.<br />
Changes to coverage due to a Marriage or Birth/Adoption/Custody of Dependent will take effect<br />
on the day of the Qualifying Life Event.<br />
COBRA: In the event of a loss of coverage, you and/or your eligible dependents may be eligible<br />
to continue medical/dental/vision insurance for a period of up to 18 months, or 29 months for<br />
disabled individuals. Please contact the <strong>Employee</strong> <strong>Benefits</strong> Office for more information.<br />
REACH YOUR PEAK HEALTH MANAGEMENT PROGRAM: Reach Your Peak (RYP) is a<br />
wellness program designed to assist you by promoting and maintaining your good health. If you<br />
(and your spouse, if applicable) are enrolled in the County medical plan, you can participate in<br />
this program. Please call 719 520-6960 with any questions and for information on the<br />
enrollment period.<br />
WORKERS COMPENSATION: For employees who are injured on the job or develop<br />
occupational illnesses, this insurance pays for all reasonable and necessary medical expenses<br />
and, if necessary, partial wage replacement during periods of temporary disability. It may also<br />
provide permanent disability entitlements for those who qualify.<br />
For any personal health (non-work related) problems, please seek the advise of your family<br />
physician. Worker’s Compensation does not cover expenses for non-work related accidents,<br />
injuries or illnesses (for example, a private automobile accident). Your health insurance<br />
coverage would apply.<br />
IF INJURED ON THE JOB, WRITTEN NOTICE MUST BE GIVEN TO YOUR EMPLOYER<br />
WITHIN FOUR (4) WORKING DAYS OF THE ACCIDENT PURSUANT TO SECTION 8-<br />
43-102-1 C.R.S.<br />
For questions regarding workers compensation, call the EBMS Workers Compensation Division<br />
at 719 520-7488.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
MEDICAL, VISION AND DENTAL PLAN PREMIUMS<br />
EMPLOYEE MONTHLY CONTRIBUTIONS<br />
January 1 st , <strong>2013</strong><br />
<strong>2013</strong> <strong>Employee</strong> <strong>Benefits</strong><br />
<strong>Employee</strong><br />
Only<br />
<strong>Employee</strong> +<br />
Spouse<br />
<strong>Employee</strong> +<br />
Children<br />
<strong>Employee</strong> +<br />
Family<br />
El Paso County<br />
Medical/EBMS<br />
Cofinity EPO<br />
Network Plan<br />
Guardian PPO<br />
Dental Low<br />
Guardian PPO<br />
Dental High<br />
$73.84 $265.36 $246.10 $328.50<br />
$14.98 $25.16 $38.93 $56.91<br />
$38.90 $65.36 $101.15 $147.83<br />
EyeMed Vision Plan $5.72 $10.87 $11.44 $16.82<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
MEDICAL PLANS<br />
EBMS MEDICAL BENEFITS<br />
EL PASO COUNTY MEDICAL EPO PLAN:<br />
In <strong>2013</strong> you will have one medical plan option – the El Paso County Medical EPO Plan<br />
administered by <strong>Employee</strong> Benefit Management Services (EBMS).* With this plan you have<br />
access to the County <strong>Employee</strong> Health Centers and a customized El Paso County Cofinity<br />
Network.<br />
The custom Cofinity Network uses only Penrose Hospital and Penrose affiliated providers and<br />
facilities to serve the Colorado Springs service area. Any non-emergent, medical services must<br />
be provided through a provider or facility contracted with Cofinity for this custom network. If<br />
you have procedures performed at a Memorial facility (now University of Colorado Health) or<br />
other non-contracted facilities (other than true emergencies and/or certain medical procedures<br />
not available through Penrose that have been pre-approved by the CareLink Care Management<br />
team), it will not be covered. You may find out if a provider is in the custom El Paso County<br />
Cofinity Network by calling Cofinity Provider Network Customer Service by logging on to their<br />
website at www.cofinity.net/EPCDirectory/Index.aspx.<br />
This plan has a $2,000 individual deductible ($6,000 Family Maximum) that applies to some<br />
services such as inpatient hospital services, surgery, and ambulance.<br />
See the EBMS Summary of <strong>Benefits</strong> on the following pages for additional information on<br />
deductibles, co-pays and co-insurance.<br />
*Please note that our medical plan administrator has the same acronym but is NOT the same as<br />
the El Paso County Employment, <strong>Benefits</strong> & Medical Services (EBMS) Department.<br />
GENERAL INFORMATION: Once you make your elections you may not change or cancel<br />
your benefits or change enrolled dependents until the next open enrollment period, unless you<br />
have a Qualifying Life Event.<br />
GRANDFATHERED HEALTH PLAN:<br />
El Paso County believes this Medical Health Plan is a “grandfathered health plan” under the<br />
Patient Protection and Affordable Care Act (the Affordable Care Act). As permitted by the<br />
Affordable Care Act, a grandfathered health plan can preserve certain basic health coverage that<br />
was already in effect when that law was enacted. Being a grandfathered health plan means that<br />
your Plan may not include certain consumer protections of the Affordable Care Act that apply to<br />
other plans, for example, the requirement for the provision of preventive health services without<br />
any cost sharing. However, grandfathered health plans must comply with certain other consumer<br />
protections in the Affordable Care Act, for example, the elimination of lifetime limits on<br />
benefits.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
Questions regarding which protections apply and which protections do not apply to a<br />
grandfathered health plan and what might cause a plan to change from grandfathered health plan<br />
status can be directed to the plan administrator at EPC EBMS <strong>Benefits</strong> Department (719) 520-<br />
7420. You may also contact the U.S. Department of Health and Human Services at<br />
www.healthreform.gov.<br />
Medical Plan Summaries:<br />
Two medical plan summaries are listed on the following pages. 1.) The Standard Medical EPO<br />
<strong>Benefits</strong> Schedule reflects benefits for employees who did not meet the Reach Your Peak (RYP)<br />
Wellness 2012-<strong>2013</strong> requirements for Phase 1 by the established deadline. 2.) The Reach Your<br />
Peak (RYP) Medical EPO <strong>Benefits</strong> Schedule reflects benefits for employees who are considered<br />
Reach Your Peak Wellness Program Participants. The RYP benefits are effective the first of the<br />
calendar year following complete enrollment in the RYP program. Please refer to the<br />
appropriate schedule of benefits. Your medical ID card will reflect the plan in which you are<br />
enrolled.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
STANDARD MEDICAL EPO BENEFITS SUMMARY<br />
PARTICIPATING<br />
PROVIDERS<br />
CALENDAR YEAR<br />
ANNUAL LIMIT $2,000 ,000<br />
NON-PARTICIPATING<br />
PROVIDERS<br />
DEDUCTIBLE, PER CALENDAR YEAR<br />
Per Covered Person $2,000 Not Covered<br />
Per Family Unit $6,000 Not Covered<br />
MAXIMUM OUT-OF-POCKET AMOUNT, PER CALENDAR YEAR<br />
Per Covered Person $8,000 Not Covered<br />
Per Family Unit $16,000 Not Covered<br />
The Plan will pay the designated percentage of Covered Charges until out-of-pocket amounts are reached, at<br />
which time the Plan will pay 100% of the remainder of Covered Charges for the rest of the Calendar Year unless<br />
stated otherwise.<br />
The following charges do not apply toward the out-of-pocket maximum and are never paid at 100%.<br />
<br />
Copayments<br />
COVERED CHARGES<br />
Hospital Services<br />
Inpatient Room and Board 75% after deductible and $500<br />
copayment per admission<br />
semiprivate room rate<br />
Intensive Care Unit 75% after deductible and $500<br />
copayment per admission<br />
Not Covered<br />
Not Covered<br />
Outpatient Facility Services<br />
Hospital's ICU Charge<br />
75% after $250 copayment per<br />
visit<br />
No deductible applies<br />
Not Covered<br />
Outpatient Physician services<br />
75%, no deductible or<br />
copayment applies<br />
Note: The copayment will apply as long as services billed include one or more of the facility room charges:<br />
Operating room, recovery room, procedures room, treatment room, and observation room.<br />
Skilled Nursing Facility, Rehabilitation 75% after deductible the<br />
Not Covered<br />
Hospital and<br />
Sub-Acute Facilities<br />
facility's semiprivate room rate<br />
Emergency Room Services<br />
100% after $200 copayment per visit;<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
(including ER Physician services)<br />
Medical Non-Emergency Care<br />
Note: The ER copayment will be waived<br />
if admitted to the Hospital directly from<br />
the ER.<br />
Urgent Care Services<br />
100% after $100 copayment per<br />
visit;<br />
No deductible applies<br />
No deductible applies<br />
Not Covered<br />
Not Covered<br />
Note: The Urgent Care copayment will be waived if admitted to the Hospital directly from Urgent Care.<br />
Physician Services<br />
Inpatient Services 75% after deductible Not Covered<br />
El Paso County <strong>Employee</strong> Health Center<br />
(“Clinic”) Office Visit<br />
Primary Care Physician (PCP)<br />
Office Visit<br />
100% after $10 copayment per<br />
visit<br />
No deductible applies<br />
100% after $50 copayment per<br />
visit<br />
Not Covered<br />
Not Covered<br />
No deductible applies<br />
Note: A Primary Care Physician (PCP) is defined as a general practitioner, family practitioner, general internist<br />
(internist whose practice is 70% general medicine), Nurse Practitioner, Physician’s Assistant, or pediatrician.<br />
An OB/GYN will be considered a specialist.<br />
Specialist office visits<br />
Surgery performed in the office (including<br />
any medical supplies and injections<br />
rendered during the surgery)<br />
100% after $75 copayment per<br />
visit<br />
No deductible applies<br />
100% after $10 Clinic, $50 PCP<br />
or<br />
$75 Specialist copayment per<br />
visit<br />
Not Covered<br />
Not Covered<br />
No deductible applies<br />
Injections (other than allergy or<br />
100%<br />
chemotherapy)<br />
No deductible or copayment<br />
will apply<br />
Allergy serum and injections 100%<br />
No deductible or copayment<br />
will apply<br />
Preventive Care<br />
Routine Well Care<br />
(ages birth through adult)<br />
100% after $10 Clinic copay or<br />
$40 copayment for all other<br />
providers<br />
No deductible applies<br />
Not Covered<br />
Not Covered<br />
Not Covered<br />
Includes: Routine office visits, routine physical examination, mammogram, gynecological exam, Pap smear,<br />
PSA, routine lab and x-rays, routine colonoscopy, flexible sigmoidoscopy, and immunizations.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
Ambulance Service<br />
75% after deductible<br />
Note: Pre-authorization with the Claims Administrator will be required for non-emergent transport.<br />
Advanced Radiological Imaging (i.e.,<br />
MRIs, MRAs, CAT Scans, PET Scans and<br />
Nuclear Medicine)<br />
75%<br />
No deductible or copayment<br />
will apply<br />
Not Covered<br />
Diagnostic X-ray & Lab Testing 100%<br />
No deductible applies<br />
Not Covered<br />
Durable Medical Equipment 100%<br />
Not Covered<br />
No deductible or copayment<br />
will apply<br />
<strong>Home</strong> Health Care 75% after deductible Not Covered<br />
<strong>Home</strong> Infusion Therapy 75% after deductible Not Covered<br />
Hospice Care<br />
75% after deductible<br />
Not Covered<br />
Note: A pre-authorization is required prior to services being rendered. Please see the Covered Charges section fo<br />
Bereavement Counseling<br />
75% after deductible<br />
Not Covered<br />
Mental Disorders and Substance Abuse Treatment<br />
Inpatient Services Payable as any other Illness Not Covered<br />
Outpatient Visits<br />
100% after $10 copayment<br />
Not Covered<br />
No deductible applies<br />
Morbid Obesity Benefit Payable as any other Illness Not Covered<br />
more information regarding this benefit.<br />
Nutritional Evaluation<br />
Outpatient Short-Term Rehabilitation<br />
Therapy and Chiropractic Services<br />
Payable as any other Illness<br />
3 visits per Calendar Year<br />
maximum<br />
100% after $20 copay per visit<br />
No deductible applies<br />
Not Covered<br />
Not Covered<br />
Includes: Cardiac Rehab, Physical Therapy, Speech Therapy, Occupational Therapy, Pulmonary Rehab,<br />
Cognitive Therapy and Chiropractic services.<br />
Multiple services provided on the same day constitute one visit, but a separate copayment will apply to the<br />
services provided by each Physician.<br />
Orthotics 75% after deductible Not Covered<br />
Note: See Covered Charges section for details.<br />
Prosthetics 100%<br />
Not Covered<br />
No deductible or copayment<br />
will apply<br />
Pregnancy *<br />
Initial visit<br />
(to confirm Pregnancy)<br />
100% after $75 Specialist office<br />
visit copayment<br />
Not Covered<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
All subsequent prenatal visits, postnatal<br />
visits, and Physician’s delivery charges<br />
(i.e., global maternity fee)<br />
Physician’s office visits in addition to the<br />
global maternity fee (when performed by<br />
an OB/GYN or specialist)<br />
Delivery – Facility charges<br />
(Inpatient Hospital, Birthing Center)<br />
Organ Transplants<br />
Transportation Benefit Maximum<br />
(Available only when using a COE<br />
facility)<br />
75% after deductible<br />
100% after $75 office visit<br />
copayment<br />
No deductible applies<br />
Payable per Inpatient<br />
Hospitalization benefit<br />
Payable as any other illness<br />
$10,000 Lifetime Maximum<br />
Not Covered<br />
Not Covered<br />
Not Covered<br />
Not Covered<br />
Note: See the Covered Charges section for more information regarding this benefit.<br />
Wigs<br />
75% after deductible<br />
$1,000 Lifetime Maximum<br />
Note: Limited to the initial purchase of a wig when deemed Medically Necesssary due to temporary or permanen<br />
hair loss. See the Covered Charges section for more information regarding this benefit.<br />
All Other Eligible Charges 75% after deductible Not Covered<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
REACH YOUR PEAK MEDICAL EPO BENEFITS SCHEDULE<br />
PARTICIPATING<br />
PROVIDERS<br />
CALENDAR YEAR<br />
ANNUAL LIMIT $2, 000,000<br />
NON-PARTICIPATING<br />
PROVIDERS<br />
DEDUCTIBLE, PER CALENDAR YEAR<br />
Per Covered Person $2,000 Not Covered<br />
Per Family Unit $6,000 Not Covered<br />
MAXIMUM OUT-OF-POCKET AMOUNT, PER CALENDAR YEAR<br />
Per Covered Person $8,000 Not Covered<br />
Per Family Unit $16,000 Not Covered<br />
The Plan will pay the designated percentage of Covered Charges until out-of-pocket amounts are reached, at whi<br />
time the Plan will pay 100% of the remainder of Covered Charges for the rest of the Calendar Year unless stated<br />
otherwise.<br />
The following charges do not apply toward the out-of-pocket maximum and are never paid at 100%.<br />
<br />
Copayments<br />
Upon a completed referral by the Clinic, recommended testing service and procedures rendered to determine or<br />
establish a diagnosis will be payable at 100% and will not be subject to either deductible or copayment. Once a<br />
diagnosis has been established, additional recommended medical treatments / services will be payable per norma<br />
REACH YOUR PEAK BENEFITS– REFERRAL REQUIREMENT<br />
Plan provisions.<br />
COVERED CHARGES<br />
Hospital Services<br />
Inpatient Room and Board 75% after deductible and $500<br />
copayment per admission<br />
Not Covered<br />
the semiprivate room rate<br />
Intensive Care Unit 75% after deductible and $500<br />
copayment per admission<br />
Not Covered<br />
Outpatient Facility Services<br />
Outpatient Physician services<br />
Hospital's ICU Charge<br />
75% after $250 copayment per<br />
visit<br />
No deductible applies<br />
75%, no deductible or copayment<br />
applies<br />
Not Covered<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
Note: The copayment will apply as long as services billed include one or more of the facility room charges:<br />
Operating room, recovery room, procedures room, treatment room, and observation room.<br />
Skilled Nursing Facility, Rehabilitation<br />
Hospital and<br />
Sub-Acute Facilities<br />
75% after deductible the facility's<br />
semiprivate room rate<br />
Not Covered<br />
Emergency Room Services<br />
(including ER Physician services)<br />
100% after $200 copayment per visit;<br />
No deductible applies<br />
Medical Non-Emergency Care<br />
Not Covered<br />
Note: The ER copayment will be waived if admitted to the Hospital directly from the ER.<br />
Urgent Care Services<br />
100% after $100 copayment per<br />
Not Covered<br />
visit;<br />
No deductible applies<br />
Note: The Urgent Care copayment will be waived if admitted to the Hospital directly from Urgent Care.<br />
Physician Services<br />
Inpatient Services 75% after deductible Not Covered<br />
El Paso County <strong>Employee</strong> Health Center 100% after $10 copayment per<br />
Not Covered<br />
(Clinic) Office Visit<br />
visit<br />
Primary Care Physician (PCP)<br />
Office Visit<br />
No deductible applies<br />
100% after $50 copayment per<br />
visit<br />
No deductible applies<br />
Not Covered<br />
Note: A Primary Care Physician (PCP) is defined as a general practitioner, family practitioner, general internist<br />
(internist whose practice is 70% general medicine), Nurse Practitioner, Physician’s Assistant, or pediatrician.<br />
An OB/GYN will be considered a specialist.<br />
Specialist office visits<br />
Surgery performed in the office (including<br />
any medical supplies and injections<br />
rendered during the surgery)<br />
100% after $75 copayment per<br />
visit<br />
No deductible applies<br />
100% after $10 Clinic, $50 PCP<br />
or<br />
$75 Specialist copayment per visit<br />
Not Covered<br />
Not Covered<br />
No deductible applies<br />
Injections (other than allergy or<br />
100%<br />
chemotherapy)<br />
No deductible or copayment will<br />
apply<br />
Allergy serum and injections 100%<br />
No deductible or copayment will<br />
apply<br />
Preventive Care*<br />
Routine Well Care<br />
(ages birth through adult)<br />
100%<br />
No deductible or copayment<br />
applies<br />
Not Covered<br />
Not Covered<br />
Not Covered<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
Includes: Routine office visits, routine physical examination, mammogram, gynecological exam, Pap smear, PSA<br />
eight additional services that will be covered without cost-sharing requirements, please refer to SPD for full deta<br />
routine lab and x-rays, routine colonoscopy, flexible sigmoidoscopy, and immunizations.<br />
*Note: Due to the Affordable Care Act, Women’s preventive health care services has been expanded to include<br />
Ambulance Service<br />
75% after deductible<br />
Note: Pre-authorization with the Claims Administrator will be required for non-emergent transport.<br />
Advanced Radiological Imaging (i.e.,<br />
MRIs, MRAs, CAT Scans, PET Scans and<br />
Nuclear Medicine)<br />
75%<br />
No deductible or copayment will<br />
apply<br />
Not Covered<br />
Note: A pre-authorization is required prior to services being rendered. Please see the Covered Charges section fo<br />
Diagnostic X-ray & Lab Testing 100%<br />
Not Covered<br />
No deductible applies<br />
Durable Medical Equipment 100%<br />
Not Covered<br />
No deductible or copayment will<br />
apply<br />
<strong>Home</strong> Health Care 75% after deductible Not Covered<br />
<strong>Home</strong> Infusion Therapy 75% after deductible Not Covered<br />
Hospice Care 75% after deductible Not Covered<br />
Mental Disorders and Substance Abuse Treatment<br />
Inpatient Services Payable as any other Illness Not Covered<br />
Outpatient Visits<br />
100% after $10 copayment<br />
Not Covered<br />
No deductible applies<br />
Morbid Obesity Benefit Payable as any other Illness Not Covered<br />
more information regarding this benefit.<br />
Nutritional Evaluation<br />
Payable as any other Illness<br />
3 visits per Calendar Year<br />
maximum<br />
Not Covered<br />
Outpatient Short-Term Rehabilitation<br />
Therapy and Chiropractic Services<br />
100% after $20 copay per visit<br />
No deductible applies<br />
Not Covered<br />
Includes: Cardiac Rehab, Physical Therapy, Speech Therapy, Occupational Therapy, Pulmonary Rehab, Cogniti<br />
Therapy and Chiropractic services.<br />
Multiple services provided on the same day constitute one visit, but a separate copayment will apply to the servic<br />
provided by each Physician.<br />
Orthotics 75% after deductible Not Covered<br />
Note: See Covered Charges section for details.<br />
Prosthetics 100%<br />
No deductible or copayment will<br />
apply<br />
Not Covered<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
Pregnancy *<br />
Initial visit<br />
(to confirm Pregnancy)<br />
100% after $75 Specialist office<br />
visit copayment<br />
Not Covered<br />
All subsequent prenatal visits, postnatal<br />
visits, and Physician’s delivery charges (i.e.,<br />
global maternity fee)<br />
Physician’s office visits in addition to the<br />
global maternity fee (when performed by an<br />
OB/GYN or specialist)<br />
75% after deductible<br />
100% after $75 office visit<br />
copayment<br />
No deductible applies<br />
Not Covered<br />
Not Covered<br />
Delivery – Facility charges<br />
(Inpatient Hospital, Birthing Center)<br />
Payable per Inpatient<br />
Hospitalization benefit<br />
Not Covered<br />
* Note: If a Clinic referral is received either to confirm a Pregnancy or after the initial diagnosis has been<br />
made and the Covered Person also enrolls in the CareLink Priority Maternity Care program during the<br />
first trimester of the Pregnancy, the Covered Person will not be subject to the inpatient hospital copay,<br />
inpatient hospital deductible or inpatient Physician deductible for the delivery charges or other pregnancy<br />
related treatment (billed with a primary diagnosis of “Pregnancy”). ER copay will also be waived if the vi<br />
is Pregnancy related (billed with a primary diagnosis of “Pregnancy”)<br />
Organ Transplants<br />
Payable as any other Illness<br />
Not Covered<br />
Transportation Benefit Maximum<br />
(Available only when using a COE facility)<br />
$10,000 Lifetime Maximum<br />
Note: See the Covered Charges section for more information regarding this benefit.<br />
Wigs<br />
75% after deductible<br />
$1,000 Lifetime Maximum<br />
Note: Limited to the initial purchase of a wig when deemed Medically Necesssary due to temporary or permanen<br />
hair loss. See the Covered Charges section for more information regarding this benefit.<br />
All Other Eligible Charges 75% after deductible Not Covered<br />
This <strong>Guidebook</strong> is only a summary of benefits and is not a binding contract. Summary Plan Documents, Certificates of<br />
Coverage, and the El Paso County Policies and Procedures Manual describes benefits in great detail and are available<br />
through ESS or by contacting the <strong>Employee</strong> <strong>Benefits</strong> office. Should there be differences between this summary and the plan<br />
documents, contracts or policies, the plan documents, contract, and/or policies will govern.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
<strong>Employee</strong>/Retiree Health Centers<br />
<strong>Employee</strong>s, retirees, spouses and children enrolled in the County’s medical plan can receive high<br />
quality health care services through the El Paso County <strong>Employee</strong> Health Centers (Clinics), operated<br />
by Take Care Health Systems..<br />
El Paso County <strong>Employee</strong> Health Centers compliment your medical insurance benefits, providing<br />
you with comprehensive, affordable, convenient and excellent health care. Two Board Certified<br />
Family Physicians and a Board Certified Nurse Practitioner provide service at both El Paso County<br />
<strong>Employee</strong> Health Centers. This program works in collaboration with both providers and your<br />
medical insurance benefits to ensure that you receive the very best in health care. The Health<br />
Centers offer acute care as well as a variety of preventive health and wellness educational services.<br />
When appropriate, the Health Centers can also make referrals to Specialists. The Health Center<br />
Physicians and Nurse Practitioners can also write prescriptions.<br />
Health Center copays are only $10.00 for both nurse practitioner and PCP visits! Other medical<br />
services, such as immunizations and vaccinations, may carry an additional cost.<br />
Ensuring your privacy and maintaining confidentiality is assured — strict adherence to HIPAA<br />
guidelines ensures all personal medical information obtained by the Health Centers and pharmacies<br />
is protected and kept completely confidential.<br />
Following are just a few examples of the many services offered:<br />
Health Center Services include:<br />
Comprehensive Individual/Family Primary Care<br />
Urgent and Acute Care (flu, fever, viral<br />
infections, nausea, cuts, sprains/strains)<br />
Preventive Health (annual adult and children<br />
physicals)<br />
Disease Management<br />
Stress Management Counseling<br />
Smoking Cessation Counseling<br />
Wellness Education / Support<br />
Referrals to specialists<br />
Vaccinations, Injections & Laboratory Services<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated October <strong>2013</strong>
Wellness Exams<br />
The County <strong>Employee</strong> Health Centers offer physicals for employees, dependents and retirees and<br />
their enrolled dependents. The cost of a physical is $10.00.<br />
Adults – Well Woman Physicals: Well woman physicals are also offered in the Health Centers.<br />
The physical includes a pap smear, breast exam and consultation on specific concerns or questions.<br />
Prenatal care is not offered at the Health Centers.<br />
Adolescents – Physicals: School and sports physicals are offered. The physicals include a<br />
comprehensive examination, risk appraisal, vision screen and appropriate vaccinations. Health and<br />
wellness advice will also be provided. Please bring record of immunizations and required school<br />
forms.<br />
<strong>2013</strong> RYP Program Participants who are enrolled on the County Medical Plan will receive<br />
100% preventive coverage and will not be responsible for copayments.<br />
Regional Development Center (RDC) Health Center<br />
2880 International Circle, Lower Level<br />
Colorado Springs, CO 80910<br />
(719) 520-7080<br />
Monday-Friday 8 am to 5 pm<br />
Citizens Service Center (CSC) Health Center<br />
1675 W. Garden of the Gods Road, Suite 1053<br />
Colorado Springs, CO 809-7<br />
(719) 520-7600<br />
Monday-Friday 8 am to 5 pm<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated October <strong>2013</strong>
El Paso County Health Centers<br />
Disease Management Program<br />
Disease management is an approach to healthcare that can help a patient learn how to manage a<br />
chronic disease. It is the concept of integrating care, minimizing the effects of a disease or chronic<br />
condition, and ultimately improving the lives of those being treated.<br />
Disease Management at the El Paso County <strong>Employee</strong> Health Centers is a confidential, on-site<br />
health improvement program, exclusively for El Paso County employees, retirees and dependents<br />
enrolled in the El Paso County medical plan. You will have the opportunity to work one-on-one<br />
with the Health Centers’ medical teams in lowering your health risks(s) such as type 2 diabetes,<br />
coronary heart disease, high blood pressure, heart failure, asthma, emphysema and lower back pain.<br />
The Disease Management Program at El Paso County <strong>Employee</strong> Health Centers is designed to help<br />
you and your doctor work together in managing your chronic health condition – whether you have<br />
been diagnosed by your own primary care physician, or you see a physician at one of the El Paso<br />
County <strong>Employee</strong> Health Centers.<br />
This program is 100% private, voluntary, and confidential. The services are provided by TakeCare<br />
Health Systems, the manager of our on-site El Paso County <strong>Employee</strong> Heath Centers. You can be<br />
assured that El Paso County will never have access to any individual health information from this<br />
program.<br />
For more information contact either the Health Centers at 520-7080 or 520-7600.<br />
©2008 Walgreens Health Initiatives, Inc., a wholly owned subsidiary of Walgreen Co. All rights reserved. <strong>2013</strong> <strong>Employee</strong> <strong>Benefits</strong> <strong>Guidebook</strong><br />
Updated January <strong>2013</strong>
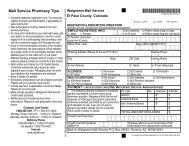
Walgreens Health Initiatives now Catamaran<br />
Walgreens Health Initiatives (WHI) now Catamaran, administers the Prescription Drug Program<br />
for El Paso County. El Paso County <strong>Employee</strong>s may fill their prescription through any<br />
Walgreens retail store for a 30 and/or 90-day supply. You can also obtain a 90-day supply of<br />
maintenance medications through the Walgreens Mail Service (Tempe, AZ facility).<br />
Filling Prescriptions at a Retail Pharmacy<br />
Filling through Catamaran will provide you with convenient access to a nationwide network of<br />
more than 6,500 retail Walgreens pharmacies. You can obtain a complete listing of pharmacies<br />
in your network by accessing the WHI website at www.walgreenshealth.com. Go to the<br />
pharmacy locator link, enter your six-digit RxGrp number of 112359 (found on your ID card),<br />
and enter your zip code or city and state.<br />
Filling Prescriptions at the Mail Service Pharmacy<br />
Through the Mail Service benefit, you can take advantage of convenient delivery of your<br />
covered maintenance medications to your home or other specified address. Maintenance<br />
medications are defined as medications that are used for chronic, long-term conditions such as<br />
high blood pressure, high cholesterol, etc. Specialty pharmacy medications are not considered to<br />
be maintenance medications.<br />
In order to use the Walgreens Mail Service pharmacy you will need to:<br />
Fill out a new Walgreens mail registration form, which was provided to you in your<br />
Catamaran Prescription packets. You can fill out one registration for your entire family<br />
even though you may not be filling a prescription for all members in your family.<br />
Obtain new prescription(s) from your doctor, and mail the originals along with your<br />
completed registration form, and copayment. The address to mail your order is provided<br />
on the Walgreens mail registration form.<br />
Please allow 14 days to process and mail your prescription(s).<br />
Catamaran Clinical Programs<br />
Specialty Pharmacy (injectable and oral medications)<br />
Catamaran Specialty Pharmacy provides convenient, dependable access to medications for<br />
people living with complex health conditions. Our programs and services focus on injectables,<br />
oral medications, and medication therapies involving strict compliance requirements; special<br />
storage, handling, and delivery; complex administration methods; and<br />
education/monitoring/ongoing support. Drugs that fall under this program can only be dispensed<br />
at a Walgreens retail pharmacy or via a home delivery method through the Walgreens Mail<br />
Service pharmacy. These drugs will be limited to a 30-day supply regardless if dispensed at a<br />
retail pharmacy or at a mail service pharmacy. Specialty Pharmacy copayments will apply at<br />
retail/mail.<br />
Drugs include the following, but are not limited to: Cystic Fibrosis medications, Enzyme<br />
replacement medications, Viral Hepatitis medications, Multiple Sclerosis medications, Growth<br />
©2008 Walgreens Health Initiatives, Inc., a wholly owned subsidiary of Walgreen Co. All rights reserved. <strong>2013</strong> <strong>Employee</strong> <strong>Benefits</strong> <strong>Guidebook</strong><br />
Updated January <strong>2013</strong>
Hormones, and all other biotech medications. Please call toll free at 1-888-782-8443 to preenroll<br />
in the Specialty Pharmacy program.<br />
Clinical Prior Authorization (CPA)<br />
Certain prescriptions may require “clinical prior authorization” or approval from Catamaran<br />
before they will be covered by your plan. The categories/medications that require clinical prior<br />
authorization may include, but are not limited to:<br />
Acne Topical (i.e. Retin-A, Avita, Differin) exceeding age 24<br />
Actiq<br />
ADHD/Narcolepsy (i.e. Dexedrine, Ritalin, Cylert) exceeding age 19<br />
Anabolic Steroids (oral, topical, injectable)<br />
Antiemetics (oral, i.e. Kytril, Zofran) are limited to a 7 day supply per 25 days. CPA if<br />
quantity limit is exceeded.<br />
Botulin Toxins (i.e. Botox, Myobloc)<br />
Butorphanol exceeding 2 bottles(5 ml)/25 days<br />
Byetta<br />
Crinone 8%<br />
Duragesic exceeding a quantity of 15/25 days<br />
Fentora<br />
Impotency (i.e. Viagra, Caverject, Levitra, Cyalis) CPA with max quantity of 8, if<br />
approved.<br />
Insomnia (i.e. Ambien, Restoril, Sonata) exceeding quantity of 90/144 days<br />
Lamisil/Sporanox/Penlac<br />
Oxycontin<br />
To request prior authorization for your prescription, the pharmacy, the physician or you may<br />
call the Prior Authorization Department toll free at 1-877-665-6609. Please have available the<br />
name of your medication, physician’s name, phone (and fax number, if available), your ID<br />
number, and your Rx Group number of 112359.<br />
Quantity Limits:<br />
Certain categories/medications may have quantity limits. These categories/medications may include,<br />
but are not limited to:<br />
<br />
<br />
<br />
<br />
<br />
<br />
Sleep Aids<br />
Pain Management<br />
Anti-Nausea<br />
Anti-psychotics<br />
Anti-depressants<br />
Migraine<br />
Your Cost: Retail, Mail-Order and Specialty Pharmacy<br />
When covered prescriptions are filled under this program, you will share a portion of the cost; the plan<br />
pays for the remainder. Your prescription drug program provides you with three-tier options. These<br />
formulary medications have received FDA approval as safe and effective. The Catamaran Preferred<br />
©2008 Walgreens Health Initiatives, Inc., a wholly owned subsidiary of Walgreen Co. All rights reserved. <strong>2013</strong> <strong>Employee</strong> <strong>Benefits</strong> <strong>Guidebook</strong><br />
Updated January <strong>2013</strong>
Medication List (PML)/formulary is available on the website at www.walgreenshealth.com. The online<br />
guide is updated regularly every calendar quarter or more often if needed to reflect important<br />
changes. Please note that although a drug is on a formulary, it does not necessarily mean that it is a<br />
covered drug under your plan. Refer to your Summary Plan Description for a list of<br />
coverages/exclusions.<br />
Walgreens Concierge Prescription Delivery to El Paso County Health<br />
Centers<br />
Walgreens is pleased to provide Concierge prescription delivery service to El Paso County RDC &<br />
CSC Health Centers effective January 2, <strong>2013</strong>! With this new service offering, if you receive a<br />
prescription from a Take Care Health medical provider at the El Paso County CSC or RDC Health<br />
Center and would like to pickup your prescription at the CSC or RDC Health Center, you can take<br />
advantage of the Concierge Delivery Service. Below are a few highlights of this new service:<br />
Service Options: Concierge delivery service to the CSC Health Center is provided by Walgreens<br />
located at 4315 Centennial Blvd. (PH: 719-264-1400). Concierge delivery service to RDC Health<br />
Center will be provided by Walgreens located at 303 South Circle Dr.<br />
(Phone number: 719-444-8569).<br />
Sign-up for Express Pay: In order for Walgreens to deliver your prescription to the El Paso County<br />
Health Center (RDC or CSC), you must sign-up for Express Pay which allows payment for delivered<br />
prescriptions. There are two easy ways to enroll in Express Pay:<br />
1) visit any Walgreens store and put a credit or debit card on file<br />
OR<br />
2) register for Express Pay online at: http://www.walgreens.com/pharmacy/expresspay-info<br />
Request Concierge Service: Once you have signed up for Express Pay, you can request Concierge<br />
Prescription Delivery service by making a verbal request to your El Paso County Health Center<br />
medical provider for each El Paso County Health Center medical provider prescription (new or refill)<br />
that you would like to pick-up at the onsite health center. Please note if you have a refill prescription<br />
setup at another Walgreens (different from Service Options listed above), then you will need to contact<br />
Walgreens and request that the originating refill prescription be transferred to the designated<br />
Walgreens Pharmacy servicing El Paso County RDC or CSC Health Center.<br />
Same Day Delivery: Prescriptions submitted by El Paso County Health Center medical providers<br />
Mon-Fri by 12:00 pm to Walgreens will be eligible for same day pickup at the RDC or CSC Health<br />
Center between 2:30 pm-4:00 pm. Please note some exceptions may apply.<br />
Next Day Delivery: Prescriptions submitted by El Paso County Health Center medical providers Mon-<br />
Fri after 12:00 pm to Walgreens will be eligible for next day pickup at the RDC or CSC Health Center<br />
between 2:30 pm - 4:00 pm. Please note some exceptions may apply.<br />
Returns: Please note that any prescriptions not picked up by 4:00 pm each Friday will be returned to<br />
the Walgreens Pharmacy that delivered the prescription.<br />
©2008 Walgreens Health Initiatives, Inc., a wholly owned subsidiary of Walgreen Co. All rights reserved. <strong>2013</strong> <strong>Employee</strong> <strong>Benefits</strong> <strong>Guidebook</strong><br />
Updated January <strong>2013</strong>
Your costs for the program are as follows:<br />
Pharmacy<br />
Walgreens<br />
Retail<br />
Pharmacy<br />
Drug Type/Copay Tier<br />
Member Copay<br />
Up to a 30 Day 84-90 Day<br />
Supply<br />
Supply*<br />
Generic $6.00 $15.00<br />
Preferred Brand $24.00 $60.00<br />
Non-Preferred Brand $42.00 $105.00<br />
Preferred Brand - Specialty Medication** $100.00<br />
Non-Preferred Brand - Specialty Medication** $200.00<br />
Up to a 90 Day<br />
Supply<br />
Walgreens<br />
Mail Order<br />
Pharmacy<br />
Generic $15.00<br />
Preferred Brand $60.00<br />
Non-Preferred Brand $105.00<br />
Preferred Brand - Specialty Medication** $100.00<br />
Non-Preferred Brand - Specialty Medication** $200.00<br />
*Your prescription must be written for at least an 84-day supply in order to obtain at the retail pharmacy.<br />
**Covered Specialty Pharmacy medications are limited to a 30-day supply. For Specialty Pharmacy medications, a Patient<br />
Max-Out-of-Pocket (MOOP) of $2,500.00 applies per individual, per calendar year. Once the MOOP is met, the member's<br />
copayment is zero for the remainder of the calendar year.<br />
Note: Eligible RYP members who have been compliant with their diabetes, hypertension, and/or<br />
cardiovascular disease medications will receive waived copays for the fourth quarter of the calendar<br />
year. This program begins in <strong>2013</strong>.<br />
It is standard pharmacy practice (and in some states, it is even required by law) to substitute generic<br />
equivalents for brand-name drugs whenever possible. When you use the mail service or a<br />
participating retail pharmacy, you may receive generic substitutes whenever available and allowable.<br />
If you select a brand name drug when a generic equivalent is available, you will be responsible for<br />
the difference in the cost of the brand and generic drug, plus your applicable<br />
Copayment.
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong><br />
EYEMED<br />
VISION PLAN<br />
Basic Services Network Non-Network<br />
Exams with Dilation as Necessary $10 copay $35<br />
Exam Options:<br />
Standard Contact Lens Fit and Follow-Up Up to $55 N/A<br />
Premium Contact Lens Fit and Follow-Up 10% off Retail Price N/A<br />
Materials No copay N/A<br />
Frequency of Services<br />
Exams<br />
every 12 months<br />
Lenses<br />
every 12 months<br />
Frames<br />
every 24 months<br />
Contact Lenses<br />
every 12 months<br />
Lenses Network Non-Network<br />
Standard Plastic Lenses:<br />
Single Vision $25 copay $40<br />
Bifocals $25 copay $60<br />
Trifocals $25 copay $60<br />
Lenticular $25 copay $80<br />
Standard Progressive Lens* $90 $60<br />
Premium Progressive Lens* $90<br />
$60<br />
80% of charge less $120 allowance<br />
Lens Options:<br />
UV Treatment $15 N/A<br />
Tint (Solid and Gradient) $15 N/A<br />
Standard Plastic Scratch Coating $0 $5<br />
Standard Polycarbonate – Adults $40 N/A<br />
Standard Polycarbonate – Kids under 19 $40 N/A<br />
Standard Anti-Reflective Coating $45 N/A<br />
Polarized 20% off Retail Price N/A<br />
Other Add-Ons 20% off Retail Price N/A<br />
Contact Lenses (in lieu of lenses & frames)<br />
Medically Necessary<br />
Conventional<br />
Disposable<br />
Standard Frames<br />
No copay<br />
$130 allowance<br />
No copay; $130 allowance<br />
15% off balance over $130<br />
No copay; $130 allowance<br />
Plus balance over $130<br />
No copay; $130 allowance<br />
20% off balance over $130<br />
Additional <strong>Benefits</strong><br />
Fundus Photography Up to $39 N/A<br />
Lasik or PRK from U.S. Laser Network 15% off Retail Price or 5% off promotional<br />
Additional Pair of Glasses<br />
price<br />
40% discount off complete pair eyeglass<br />
purchases & 15% discount off conventional<br />
contact lenses once the funded benefit has been<br />
$200<br />
$105<br />
$105<br />
$45<br />
N/A<br />
N/A
* Standard/Premium Progressive lenses not covered - fund as a Bifocal Lens<br />
used<br />
Additional Discounts:<br />
Members also receive 15% off retail price or 5% off promotional price for Lasik or PRK from the US Laser<br />
Network, owned and operated by LCA Vision.<br />
After initial purchase, replacement contact lenses may be obtained via the Internet at substantial savings<br />
and mailed directly to the member. Details are available at www.eyemedvisioncare.com.<br />
The contact lens benefit allowance is not applicable to this service.<br />
Benefit Allowances provide no remaining balance for future use within the same Benefit Frequency.<br />
Certain brand name Vision Materials in which the manufacturer imposes a no-discount practice.<br />
Additional Purchases and Out-of-Pocket Discount <strong>Benefits</strong> are not provided for services or materials arising<br />
from: Orthoptic or vision training, subnormal vision aids and any associated supplemental testing; Aniseikonic<br />
lenses; Medical and/or surgical treatment of the eye, eyes or supporting structures; Any eye or Vision<br />
Examination, or any corrective eyewear required by a Policyholder as a condition of employment; safety<br />
eyewear; Services provided as a result of any Workers’ Compensation law, or similar legislation, or required by<br />
any governmental agency or program whether federal, state or subdivisions thereof; Plano (non-prescription)<br />
lenses and/or contact lenses; Non-prescription sunglasses; Two pair of glasses in lieu of bifocals; Services or<br />
materials provided by any other group benefit plan providing vision care; Certain brand name Vision Materials in<br />
which the manufacturer imposes a no-discount policy; or Services rendered after the date an Insured Person<br />
ceases to be covered under the Policy, except when Vision Materials ordered before coverage ended are<br />
delivered, and the services rendered to the Insured Person are within 30 days from the date of such order. Lost or<br />
broken lenses, frames, glasses, or contact lenses will not be replaced except in the next Benefit Frequency when<br />
Vision Materials would next become available.<br />
<strong>Benefits</strong> may not be combined with any discount, promotional offering, or other group benefit plans.<br />
Standard/Premium Progressive Lens not covered - fund as a Bifocal Lens. Standard Progressive Lens covered -<br />
fund Premium Progressive as a Standard. Member will receive a 20% discount on remaining balance at<br />
Participating Providers beyond plan coverage; the discount does not apply to EyeMed's Providers' professional<br />
services or disposable contact lenses. Members also receive a 40% discount off complete pair eyeglass purchases<br />
and a 15% discount off conventional contact lenses once the funded benefit has been used.<br />
Underwritten by Combined Insurance Company of America, 5050 Broadway, Chicago, IL 60640, except in New<br />
York. CICA Form # VN P63007 0801. This is a snapshot of your benefits. The Certificate of Insurance is on file<br />
with your employer.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
Guardian<br />
DENTAL PLANS<br />
El Paso County offers two options with Guardian Dental: Low Option PPO and a High Option PPO. A<br />
comparison of the two plans is shown on the following page.<br />
On the Low and High Guardian Dental options, dental procedures are covered either through a Guardian<br />
Dental Guard Preferred Network PPO dental provider or through any licensed dentist. A listing of Network<br />
providers can be found through the Guardian website at www.GuardianAnytime.com, clock on the “Find a<br />
Provider” in the right hand corner of the page. Next click the box “Find a Dentist”. When prompted for the<br />
Dental Plan, select “PPO”, and for the Dental Network choose ‘DentalGuard Preferred” Network.<br />
Guardian Dental<br />
Comparison of <strong>2013</strong> Plans<br />
DENTAL SERVICES LOW OPTION HIGH OPTION<br />
In<br />
Network<br />
Out of<br />
Network<br />
In<br />
Network<br />
Out of<br />
Network<br />
Teeth Cleaning – 2 per calendar year 100% 80% 100% 100%<br />
Oral Evaluations (Diagnostic) 100% 80% 100% 100%<br />
X Rays (Diagnostic) 100% 80% 100% 100%<br />
Lab and Other Diagnostic Tests 100% 80% 100% 100%<br />
Prophylaxis (Preventive) 100% 80% 100% 100%<br />
Fluoride Treatment (Preventive) for children<br />
100% 80% 100% 100%<br />
under age 19<br />
Fillings (Amalgam & Anterior Composites) 80% 60% 90% 70%<br />
Crowns: Stainless Steel 80% 60% 90% 70%<br />
Simple Extractions 80% 60% 90% 70%<br />
Oral Surgery (simple extractions) 80% 60% 90% 70%<br />
Endodontic Services – Root Canal Therapy 50% 30% 90% 70%<br />
Periodontal Services 50% 30% 90% 70%<br />
Inlays/Onlays/Bridges 50% 30% 60% 30%<br />
Dentures and other Removable Prosthetics 50% 30% 60% 30%<br />
Fixed Prosthetics 50% 30% 60% 30%<br />
Crowns: Resin, Metal 50% 30% 60% 30%<br />
Implants 50% 30% 60% 30%<br />
Orthodontia N/A N/A 50% 50%<br />
Orthodontia Eligibility N/A Adults and Children<br />
Deductible Per Person $50/$150 $50/$150 $25/$75 $50/$150<br />
Deductible applies to Preventive & Diagnostic No No No No<br />
Ortho Lifetime Maximum N/A N/A $1500<br />
Calendar Maximum includes In and Out of<br />
$1,000 $1,000 $1,500 $1,500<br />
Network<br />
Waiting Period applies No No<br />
Out of Network Basis MAC UCR 90th<br />
This <strong>Guidebook</strong> is only a summary of benefits and is not a binding contract. Summary Plan Documents, Certificates of Coverage, and the El Paso County<br />
Policies and Procedures Manual describes benefits in great detail and are available through ESS or by contacting the <strong>Employee</strong> <strong>Benefits</strong> office. Should<br />
there be differences between this summary and the plan documents, contracts or policies, the plan documents, contract, and/or policies will govern<br />
Dental Rate Proposal<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
Maximum Rollover Feature:<br />
With Maximum Rollover, Guardian will roll over a portion of your unused annual maximum into your<br />
personal Maximum Rollover Account (MRA). The MRA can be used in further years, if you reach the<br />
plan’s annual maximum.<br />
Even better, if you use the services of Preferred Providers exclusively during the benefit year, Guardian will<br />
increase the amount credited to your MRA.<br />
To qualify, you must submit a claim for covered services for which a benefit payment is issued, in excess of<br />
any deductible or co-pay, and you must not exceed the paid claims threshold during the benefit year.<br />
You and your insured dependents maintain separate MRAs based on your own claim activity. Each MRA<br />
may not exceed the MRA limit.<br />
You will receive an annual MRA statement detailing your account and those of your dependents.<br />
High Plan:<br />
Low Plan:<br />
PLAN ANNUAL<br />
MAXIMUM **<br />
THRESHOLD<br />
MAXIMUM<br />
ROLLOVER AMOUNT<br />
IN-NETWORK ONLY<br />
MAXIMUM<br />
ROLLOVER AMOUNT<br />
MAXIMUM<br />
ROLLOVER<br />
ACCOUNT LIMIT<br />
$1500 $700 $350 $500 $1250<br />
PLAN ANNUAL<br />
MAXIMUM **<br />
THRESHOLD<br />
MAXIMUM<br />
ROLLOVER AMOUNT<br />
IN-NETWORK ONLY<br />
MAXIMUM<br />
ROLLOVER AMOUNT<br />
MAXIMUM<br />
ROLLOVER<br />
ACCOUNT LIMIT<br />
$1000 $500 $250 $350 $1000<br />
This <strong>Guidebook</strong> is only a summary of benefits and is not a binding contract. Summary Plan Documents, Certificates of Coverage, and the El Paso County<br />
Policies and Procedures Manual describes benefits in great detail and are available through ESS or by contacting the <strong>Employee</strong> <strong>Benefits</strong> office. Should<br />
there be differences between this summary and the plan documents, contracts or policies, the plan documents, contract, and/or policies will govern<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
What is an FSA?<br />
FLEXIBLE SPENDING ACCOUNTS (FSA)<br />
An FSA is a Flexible Spending Account that allows you to set aside money for eligible expenses on a pre-tax<br />
basis. There are two types of Flexible Spending Accounts available - a healthcare account and a dependent day<br />
care account.<br />
What you need to know about FSAs<br />
• You may only determine your contribution in an FSA during open enrollment or when you first become<br />
eligible.<br />
• You do not need to be covered by your employer’s health plan to participate in an FSA.<br />
• Expenses must be for services received, not for services to be provided in the future.<br />
• Once you establish your plan year contribution, you may only change it if you experience a Qualifying Life<br />
Event.<br />
• Any claims that were incurred during the plan year must be submitted for reimbursement by the end of your<br />
run out period (60 days). The run out date is 60 days after the end of your plan year or February 28, 2014.<br />
• Any amount left in your healthcare and/or dependent day care FSA at the end of the plan year will be<br />
forfeited.<br />
An FSA is a smart way to save!<br />
Annual<br />
Salary<br />
Healthcare contribution<br />
Dependent day<br />
care contribution<br />
Savings<br />
$20,000 $1,500 $0 $405<br />
$40,000 $1,750 $4,000 $1,553<br />
$60,000 $2,000 $4,500 $1,755<br />
Getting started is as easy as 1-2-3!<br />
1. Estimate the amount you will spend on out-of-pocket healthcare expenses and/or dependent day care<br />
expenses during the plan year.<br />
• Review expenses from prior plan year.<br />
• Use our planning tools available at HealthHub.com<br />
2. Decide how much you wish to set aside in your healthcare FSA and/or dependent day care FSA.<br />
• Divide your annual contribution by 26 pay periods in your plan year to determine the amount that<br />
will be deducted from you paycheck each pay period.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
3. As you incur eligible healthcare and dependent day care expenses throughout the year, you can<br />
access your funds by:<br />
• Using your PayFlex Card OR<br />
• Submitting a claim for reimbursement<br />
Quick Tip: View a listing of eligible expenses Login to HealthHub.com > My HealthHub Resources ><br />
Planning Tools<br />
My HealthHub Resources: Education & Planning Tools<br />
• Savings calculator to help you estimate your healthcare & dependent day care expenses<br />
• Digital library designed to help you understand FSAs<br />
• Educational materials & forms to better assist you with your spending account(s)<br />
Quick Tip: Find out how much you can save Login to HealthHub.com > My HealthHub Resources ><br />
Planning Tools<br />
Healthcare Flexible Spending Account:<br />
What you should know:<br />
Reimburses you for out-of-pocket medical, dental, prescription or vision services, such as deductibles, copays,<br />
and coinsurance. The maximum annual amount reimbursed may not exceed $2,500.<br />
Allows you to set aside money for eligible expenses on a pre-tax basis for you, your spouse and/or<br />
dependents.<br />
You do not pay Federal income or Social Security taxes on this money.<br />
Your entire contribution is available at the beginning of the plan year.<br />
View a detailed listing of eligible expenses at HealthHub.com<br />
OTC Items<br />
Since January 1, 2011, certain OTC medicines and drugs are considered ineligible unless you have a written<br />
prescription from your doctor. You cannot get reimbursed for OTC drugs or medicine unless you have a<br />
prescription. In addition, healthcare cards (e.g., PayFlex Card ) cannot be used to pay for OTC drugs and<br />
medicines.<br />
Dependent Day Care Flexible Spending Account:<br />
What you should know:<br />
Reimburses you for expenses such as day care, before and after school programs, nursery school or<br />
preschool, summer day camp and even adult day care.<br />
For day care expenses of a child under age 13 OR for the care of a dependent who is physically or mentally<br />
incapable of taking care of themselves.<br />
You and your spouse, if married must be actively working, seeking employment, or full-time student, in<br />
order to get reimbursed.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
You can only be reimbursed up to the amount that is available in your account.<br />
View a detailed listing of eligible expenses at HealthHub.com<br />
The annual expense reimbursement may not exceed:<br />
o the lesser of your earned income;<br />
o if married, your spouse’s earned income;<br />
o $5,000 ($2,500 if married, filing separate income tax returns)<br />
Eligible expenses:<br />
• Licensed day care provider<br />
• In-home provider as long as the care provider is not your child under age 19, or someone you claim as a<br />
tax dependent<br />
• Summer camps (not overnight)<br />
• Tuition through preschool<br />
• Before and after school care (under age 13)<br />
Ineligible expenses:<br />
• Tuition expenses for kindergarten and beyond<br />
• Overnight camps<br />
• Child care expenses for a child 13 or older (unless disabled)<br />
• Child care expenses for night-time babysitting<br />
• Child care expenses while you are on an extended leave of absence<br />
• Care provided by an older dependent or sibling<br />
Questions?<br />
Contact PayFlex Customer Service at 800.284.4885, 7am-7pm, Monday – Friday and Saturday 9am-2pm CT.<br />
Quick Tip: Enroll in direct deposit Login to HealthHub.com > Financial Center > Enroll in Direct Deposit<br />
Reimbursement Methods<br />
Online: www.HealthHub.com<br />
Fax: 402.231.4310<br />
Mail: PayFlex Systems USA, Inc.<br />
PO Box 3039 Omaha, NE<br />
68103-3039<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
LIFE INSURANCE PLANS<br />
BASIC LIFE/ACCIDENTAL DEATH AND DISMEMBERMENT PLAN BENEFIT<br />
EMPLOYEE: LIFE BENEFIT: $40,000 AD&D BENEFIT: $40,000<br />
SPOUSE: LIFE BENEFIT: $2,000 AD&D BENEFIT: $0<br />
CHILD: LIFE BENEFIT: $1,000 first 6 months/$2,000 thereafter until age 26<br />
TERM LIFE: This coverage is Term Life Insurance. The Life Insurance benefit is payable to<br />
the designated beneficiary upon the death of the insured. Coverage is provided for the time<br />
period that you are eligible and premium is paid. There is no cash value associated with this<br />
product.<br />
AD&D: Accidental Death and Dismemberment Insurance provides specified benefits for a<br />
covered accidental bodily injury that directly causes dismemberment (i.e. the loss of a hand, foot,<br />
or eye). In the event that death occurs to an employee from a covered accident, both the Life and<br />
the AD&D benefit would be payable.<br />
ELIGIBILITY: All full-time active employees working 40 or more hours per week in an eligible<br />
class are eligible for coverage on the policy effective date. A delayed effective date will apply if<br />
the employee is not actively at work on the date the insurance would otherwise take effect.<br />
GUARANTEE ISSUE: For timely entrants enrolled within 30 days of becoming eligible, up to<br />
$40,000 in coverage is available without any evidence of insurability requirement.<br />
LIVING BENEFIT: A living benefit (also called an Accelerated Death Benefit) is available to<br />
employees who have satisfied the Active Work Rule. When such employees are diagnosed as<br />
terminally ill (having 12 months or less to live), they may withdraw up to 75% of their life<br />
insurance coverage to a maximum of $30,000. The death benefit will be reduced by the amount<br />
taken as a Living Benefit, plus interest.<br />
PORTABILITY: If you terminate your employment or if you become ineligible for this<br />
coverage, you have the option to convert all or part of the amount of Life Insurance in force on<br />
the date of termination at the group rates. Conversion election must be made within 30 days of<br />
your date of termination.<br />
BENEFIT REDUCTION: Life and AD&D benefits will terminate at retirement. Prior to this,<br />
reduce to: 65% at age 70 and at age 75 benefits reduce further to 50% of the original amount.<br />
This is only a summary of coverage and is not a binding contract. A certificate of coverage will<br />
be made available to you that will describe the benefits in greater detail. Should there be<br />
differences between this summary and the contract, the contract will govern.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
VOLUNTARY TERM LIFE INSURANCE<br />
Voluntary Term Life insurance is an optional benefit. Coverage is available in $10,000<br />
units starting at $10,000 up to the lesser of seven (7) times your salary rounded to the next<br />
highest $10,000 or $500,000 for employees and up to the lesser of 100% of the employee’s<br />
elected amount or $250,000 for spouses. You may also elect a flat $10,000 of coverage for<br />
dependent child(ren).<br />
You must elect coverage in order to elect coverage for your spouse or dependent child(ren).<br />
If you choose to elect AD&D coverage, the amount of coverage will be the same as your life<br />
insurance.<br />
Up to $200,000 of coverage is guaranteed for you the employee and up to $30,000 for your<br />
spouse as long as you, your spouse or dependent children meet eligibility requirements and<br />
enroll within the first 30 days from your eligibility date. This means no medical questions are<br />
asked in order to sign up for coverage up to these limits.<br />
Any coverage applied for above the guaranteed coverage amounts requires an Evidence of<br />
Insurability form to be completed along with the Enrollment Form. These forms can be found at<br />
http://w3.unum.com/enroll/ElPasoCounty/enrollment.aspx.<br />
If you do not elect the minimum coverage when first eligible, you will only be eligible again at<br />
the next Open Enrollment period and Evidence of Insurability will be required to obtain this<br />
coverage.<br />
Additional medical information may be required depending on the amount applied for, or in<br />
response to the information disclosed on the application.<br />
During the <strong>2013</strong> open enrollment period, if you already have the minimum amount of life<br />
insurance ($10,000) for yourself and your dependents, you can purchase additional insurance up<br />
to the Guaranteed Issue (GI) amount, as long as you remain actively at work.<br />
Please see rates on the following page.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
AD&D Coverage Rates<br />
<strong>Employee</strong>, Spouse & Child<br />
AD&D<br />
Semi-Monthly Rate<br />
$.100 per $10,000<br />
Term Life<br />
Coverage Rates<br />
Rates shown are your semi-monthly deduction:<br />
A tobacco user is defined as anyone who currently uses or has used a<br />
tobacco product within the last 12 months.<br />
<strong>Employee</strong> and Spouse Life Semi-Monthly<br />
Step Rates per $10,000<br />
Child Life<br />
Semi-Monthly Rate<br />
Age Non-Tobacco Tobacco<br />
15-24 0.220 0.310 $1.00 per $10,000<br />
25-29 0.220 0.310<br />
30-34 0.265 0.395<br />
35-39 0.310 0.530<br />
40-44 0.570 1.275<br />
45-49 0.925 2.155<br />
50-54 1.585 3.390<br />
55-59 2.465 5.700<br />
60-64 3.870 8.850<br />
65-69 6.700 15.95<br />
70-74 12.50 28.50<br />
75+ 12.50 28.50<br />
Insurance Age: Your rate is based on your insurance age. To calculate your insurance age,<br />
subtract your year of birth from the year your coverage becomes effective.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
DISABILITY BENEFITS<br />
SHORT TERM DISABILITY (STD) - Unum Policy #907374<br />
WEEKLY BENEFIT: If you are Totally Disabled beyond the elimination period due to a<br />
covered injury or sickness, you may be eligible to receive a weekly benefit of 60% of your basic<br />
weekly income to a maximum benefit of $1,000. This benefit may be reduced by income or<br />
benefits from certain other income sources listed in your plan document.<br />
DEFINITION OF TOTAL DISABILITY: Total Disability is defined as the inability to perform<br />
the material and substantial duties of the employees’ regular occupation due to injury or illness<br />
as certified by a health care provider and approved by the Disability Management Company.<br />
ELIGIBILITY DATE: An employee becomes eligible for coverage provided by the Policy on<br />
the later of the Policy’s effective date or the date the Insured <strong>Employee</strong> satisfies the Waiting<br />
Period specified in the Policy Effective Date.<br />
POLICY EFFECTIVE DATE: <strong>Employee</strong>s are eligible for coverage on the first of the month<br />
following the first day of full-time employment or concurrent with their date of hire if hired on<br />
the first day of the month. If you are hired full-time starting from the 1 st through the 15 th of the<br />
month, coverage is effective the first day of the next month. If you are hired full-time starting<br />
the 16 th through the last day of the month, coverage is effective on the first day of the second<br />
following month. (Example 1: First day of full-time employment is January 15 th , coverage is<br />
effective February 1 st . Example 2: First day of full-time employment is January 16 th , coverage<br />
is effective March 1 st .)<br />
ELIMINATION PERIOD: <strong>Benefits</strong> begin following 14 continuous days of Disability or<br />
following exhaustion of available sick and vacation benefits, whichever is later.<br />
HOW TO REPORT A DISABILITY CLAIM:<br />
1. Advise your supervisor or manager as soon as possible, preferably on or before your first<br />
absence.<br />
2. Call the UNUM hotline at 888-673-9940 as soon as possible, or you can access the form<br />
on the following website: http://w3.unum.com/enroll/ElPasoCounty/enrollment.aspx<br />
NOTIFICATION OF CLAIM DECISION: The insurance company will notify both the<br />
employee and the <strong>Benefits</strong> Administrator of their claim decision. Claims can take a few weeks<br />
or even longer to be processed so employees are encouraged to submit their paperwork as soon<br />
as possible. STD checks are available in the <strong>Employee</strong> <strong>Benefits</strong> and Medical Services <strong>Benefits</strong><br />
Division office after 9:00 a.m. on paydays.<br />
SUMMARY PLAN DESCRIPTION (SPD): The SPD information may be obtained by<br />
contacting the <strong>Employee</strong> <strong>Benefits</strong> Division at 719-520-7420.<br />
WHO PAYS FOR DISABILITY COVERAGE: <strong>Employee</strong>s are required to contribute $5.00 per<br />
pay period for their Short Term Disability coverage.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
LONG TERM DISABILITY (LTD) – Unum Policy # 907338<br />
MONTHLY BENEFIT: If you are Totally Disabled beyond the elimination period due to a<br />
covered injury or sickness, you will be eligible to receive a weekly benefit of 60% of predisability<br />
earnings (when combined with other income sources) up to a maximum monthly<br />
benefit of $6,500. This benefit may be reduced by income or benefits from certain other income<br />
sources listed in your certificate.<br />
ELIMINATION PERIOD: You need to satisfy a 180-day elimination period before benefits<br />
would begin. This elimination period can be satisfied with days of Partial Disability, Total<br />
Disability or a combination of both. The elimination period may be met by days of disability<br />
built up over an accumulation period of 360 days, so there is no penalty for briefly attempting to<br />
return to work during this elimination period.<br />
ELIGIBILITY: All full-time active employees working 40 or more hours per week are eligible<br />
for coverage on the policy effective date. A delayed effective date will apply if the employee is<br />
not actively at work on the date the insurance would otherwise take effect.<br />
DEFINITION OF TOTAL DISABILITY: Total Disability is defined as the inability to perform<br />
each of the main duties of your own occupation, due to injury and illness. Your “own”<br />
occupation is covered for 24 months. Following this, the definition of disability becomes the<br />
inability to perform any occupation for which you are reasonably fitted, based on your<br />
experience, education or training.<br />
BENEFIT DURATION: <strong>Benefits</strong> may continue to be paid until you reach age 65/SSNRA, as<br />
long as you meet the definition of disability. Please note that certain conditions may be limited<br />
benefit durations. Review your employee certificate of coverage for clarification.<br />
PRE-EXISTING CONDITION: <strong>Benefits</strong> will not be paid for any disability for which you<br />
received medical treatment, care or consultation, including diagnostic measures or took<br />
prescribed drugs or medications during the three months preceding your effective date under this<br />
policy, until you are covered under this policy (or a prior policy) for 12 consecutive months<br />
before disability begins.<br />
SUMMARY PLAN DESCRIPTION (SPD): The Long Term Disability SPD information may<br />
be obtained by contacting the <strong>Employee</strong> <strong>Benefits</strong> office at 719-520-7420.<br />
WHO PAYS FOR DISABILITY COVERAGE: El Paso County pays the full cost for Long Term<br />
Disability premium costs.<br />
For more information, please contact the EBMS <strong>Benefits</strong> Division.<br />
This is only a summary of coverage and is not a binding contract. Certificates of Coverage, which describes<br />
benefits in great detail, are available through ESS or by contacting the EBMS <strong>Benefits</strong> Division. Should there<br />
be differences between this summary and the plan contract, the contract will govern.<br />
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong><br />
EL PASO COUNTY RETIREMENT PLAN<br />
The El Paso County Retirement Plan is a Defined Benefit Plan as stated under section 401(a) of<br />
the IRS Code. Participation is mandatory.<br />
CONTRIBUTION LEVEL: Beginning January 1, <strong>2013</strong>, the contribution amount is 8% of your<br />
pre-tax salary. The County also contributes 8% each pay period. By having the contributions<br />
withheld on a pre-tax basis, the amount of your taxable income is lowered. No additional<br />
contributions can be made to this Plan.<br />
VESTING: If hired after January 1, <strong>2013</strong>, the vesting period under this Plan is 8 years. If hired<br />
prior to January 1, <strong>2013</strong> the vesting period is 5 years. This means after you have been employed<br />
5 or 8 years, depending on your hire date and once you reach the age requirements, you would be<br />
eligible for a lifetime retirement benefit.<br />
RETIREMENT ELIGIBILITY: Normal retirement age is 62. You can retire under the Rule<br />
of 75 with a full benefit. The Rule of 75 = your age and service total the number 75 (i.e. age 50<br />
with 25 years). No minimum age. Early retirement is age 55 at a reduced rate of 3% for each<br />
year you are under 62. All benefits are lifetime benefits.<br />
BENEFIT CALCULATION: The benefit is calculated using your FAMP Final Average<br />
Monthly Salary (highest 36 months out of last 10 years) x Service x the benefit multiplier.<br />
Pre-2010 employment-<br />
The formula for calculating your monthly benefit is:<br />
(FAMP x Service x 2.22%) + (FAMP x Service x 2.00%)<br />
Post-2010 employment-<br />
The formula for calculating your monthly benefit is:<br />
FAMP x Service x 2.00%<br />
SEPARATION BENEFITS – NOT VESTED: If hired after <strong>2013</strong> and you leave employment<br />
with less than 8 years of service, you are required to remove your contributions from the Plan. If<br />
hired prior to <strong>2013</strong> and you leave employment with less than 5 years of service, you are required<br />
to remove your contributions from the Plan. You are paid your contributions plus interest. The<br />
County’s portion is forfeited.<br />
Since the money was withheld on a pre-tax basis, unless the money is rolled over into an IRA or<br />
another retirement plan, 20% Federal Income Tax is withheld from the distribution. In addition,<br />
at the time you file your taxes for the year in which you received the distribution; there is a 10%<br />
early distribution penalty if you are under age 59½ . If you roll it over, taxes are deferred and<br />
there is no tax penalty.<br />
SEPARATION BENEFITS – VESTED: If hired after <strong>2013</strong> and you leave employment with 8<br />
years or more of service, you have the option of taking the money out of the Plan with the same
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong><br />
provisions stated above. If hired before <strong>2013</strong> and you leave employment with 5 years or more of<br />
service, you have the option of taking the money out of the Plan with the same provisions stated<br />
above.<br />
You may choose to leave your money in the Plan until you are eligible to begin a monthly<br />
benefit anytime between age 55 and 61 at a reduced benefit (3% for each year under age 62), or<br />
at age 62 with no reduction. No further contributions can be made. Your contributions<br />
accumulate interest. The current interest rate is 3%.<br />
You may withdraw the money at anytime which then forfeits any future benefits and the taxes<br />
and penalties apply. Again, you only get back your contributions plus interest. The County’s<br />
portion is forfeited.<br />
DEATH BENEFITS: If you die while you are actively employed by the County and are not<br />
vested, your beneficiary will receive your contributions and interest.<br />
If you die, were vested and under age 55, your beneficiary could take two times your account<br />
balance or they could leave the money in the Plan until you would have been 55. They would<br />
then receive a lifetime benefit equal to 60% of the benefit you had accrued. If you were already<br />
55 and vested, they could begin that 60% benefit immediately. If you were already 62, it would<br />
be treated as a 100% J & S benefit and benefits would begin immediately.<br />
IF YOU LEAVE AND RETURN: If you leave employment and return to work full-time<br />
within 48 months and had removed your contributions from the Plan, you have the option of repaying<br />
your contributions, plus interest, for the period of time you were gone. You would get<br />
credit for your prior service. You have one year from the date you are re-hired to re-pay the<br />
Plan. If you were vested and left your money in the Plan, you would pick up where you left off<br />
and would be credited with the prior service at retirement.<br />
PURCHASE OF SERVICE: Hired post-<strong>2013</strong> and after 8 years or hired pre-<strong>2013</strong> and after 5<br />
years you can purchase service from a previous employer. The cost is based upon an actuarial<br />
equivalent of your final average salary at the time of purchase. You would be purchasing service<br />
from a previous employer that you participated in a retirement plan with but are not entitled to a<br />
retirement benefit from. It has to be full-time employment. Verification from your previous<br />
employer is needed stating your dates of full-time employment and non-vested status.<br />
MEDICAL BENEFITS: To be eligible for continuation of medical coverage the employee<br />
must be enrolled on the county’s medical plan at the time of retirement. Retiree Eligibility<br />
Definitions: Normal Retirement – Age 62 Years and who have a minimum of eight (8) years, if<br />
hired after <strong>2013</strong>, or five (5) years, if hired prior to <strong>2013</strong>, of creditable service as an employee of<br />
El Paso County are eligible for continuation of health insurance medical benefits, if enrolled at<br />
the time of retirement.<br />
Early Retirement – Retirees who were fifty-five (55) years of age or older when he/she left the<br />
continuous service of El Paso County and who have a minimum of eight (8) years, if hired after<br />
<strong>2013</strong>, or five (5) years, if hired prior to <strong>2013</strong>, of creditable service as an employee of El Paso<br />
County are eligible for continuation of health insurance medical benefits, if enrolled at the time
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong><br />
of retirement. Elected officials who were fifty-five (55) years of age or older when he/she left<br />
the service of El Paso County and who have a minimum of eight (8) years, if elected after <strong>2013</strong>,<br />
or five (5) years, if elected prior to <strong>2013</strong>, of creditable service with El Paso County are eligible<br />
for continuation of the County’s self-funded medical benefits, if enrolled at the time of<br />
separation. This eligibility clause is effective for all employees retiring after January 1, 2003.<br />
Special Early Retirement – Rule of 75 Years. Age + creditable (continuous) years of service<br />
must equal 75 years. (No minimum age requirement)<br />
Eligibility: Retirees and eligible dependents (spouses and/or children) of retirees may continue<br />
medical coverage on the County’s self-funded medical plans if the retiree is currently enrolled<br />
and elects such coverage at the time of retirement. (Retirement is not a qualifying life event.)<br />
Spouses and dependent children can continue coverage under the medical plans if they meet the<br />
eligibility requirements outlined in Chapter IX of the El Paso County <strong>Employee</strong> Policies and<br />
Procedures manual.<br />
Spouses may continue to receive coverage under their own identity after the retiree has become<br />
entitled to Medicare, reached age sixty-five (65) or death. The spouse is eligible to remain on<br />
the EPO medical plan until age sixty-five (65) or Medicare entitlement, whichever may occur<br />
first, at which time they may choose to enroll in the 65+ PPO Plan.<br />
Dependent children of a retiree that is no longer eligible for the medical plans will be allowed to<br />
continue coverage as a dependent on the EPO Medical Plan until the retiree’s spouse reaches the<br />
age of sixty-five (65) or Medicare entitlement, provided the dependent child meets the eligibility<br />
requirements. Once the retiree’s spouse reaches the age of sixty-five (65) or Medicare<br />
entitlement, the dependent child is no longer eligible for the EPO Medical Plan.<br />
If the retiree has coverage for eligible dependent children and no spouse coverage and the retiree<br />
becomes entitled to Medicare, reaches age sixty-five (65), or dies, the dependent child is eligible<br />
to remain on the EPO Medical Plan until they no longer meet the definition of an Eligible<br />
Dependent.<br />
When enrolled retirees and spouses of retirees become Medicare eligible, they are no longer<br />
eligible for the EPO plan but can enroll at that time in the PPO 65 + Plan, provided the member<br />
is also enrolled in Medicare Part A and Part B. The PPO 65+ Plan will be the covered<br />
individual’s secondary insurance and pay after Medicare pays in accordance with plan<br />
provisions. Please contact the <strong>Employee</strong> <strong>Benefits</strong> office for more information at 719-520-7420.<br />
(The PPO 65+ Plan will only be offered if the County meets all eligibility requirements as<br />
defined by the Plan Provider. If the eligibility requirements are not met, the benefit will not be<br />
offered until such eligibility is guaranteed and will begin on January 1st of the following year.)<br />
For the retiree and dependents of the retiree to be eligible for continuation of health benefits,<br />
the retiring employee and dependents must be currently enrolled and elect to continue the<br />
coverage at the time of retirement. If the retiring employee does not elect continuation of the
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong><br />
benefit at the time of retirement, the benefit is forfeited for the retiree and dependents of the<br />
retiree.<br />
If the retiring employee is married to another El Paso County employee, the retiring employee<br />
may elect to be covered under the active married employee.<br />
Contribution Schedule: The cost for continuation of health benefits for retirees and dependents<br />
of retirees will be subject to the premium rate for the benefit plan(s) elected; however, the county<br />
may provide a medical plan retirement subsidy depending upon the number of years of creditable<br />
service the retiree had at the time of retirement. If the premium rate of the medical plan selected<br />
is less than the provided subsidy, no subsidy reimbursement to the retiree will occur. If the<br />
premium rate of the medical plan selected is more than the provided subsidy, the balance due<br />
will be deducted from the retiree’s benefit payment<br />
If the premium rate of the medical or dental plan exceeds the retiree benefit payment, the retiree<br />
is responsible to make payment for the health benefits directly to the Retirement Plan office by<br />
the 1 st day of each month. Non-Payment of Health Premiums: In the event of late or nonpayment<br />
of health premiums, coverage will be terminated retroactively to the last day coverage<br />
was paid in full. You will be given 30 days notice except in cases of fraud or intentional<br />
misrepresentation. Health benefits will not be reinstated if payment has not been received in<br />
full by the end of the 30-day grace period.<br />
The Health Plan Trust Board will determine the subsidy amount. The retiree subsidy rate may be<br />
re-evaluated and may be adjusted each year with increases to the retiree subsidy, which will be<br />
based on contributions for active employees.<br />
RETIREE DENTAL AND VISION PLAN<br />
Retirees who meet the eligibility requirements of the medical plan are also eligible for<br />
continuation of dental and vision coverage if enrolled at the time of retirement. The rate for<br />
dental and vision coverage will be based on the actual cost of plans.<br />
BOARD OF RETIREMENT: The Board of Retirement consists of seven members. Two are<br />
elected by the participants. Two are appointed by the BOCC. One is the County Treasurer who is<br />
mandated by State Statute to be on the Board and two associate members, employees appointed<br />
by the second and third largest employers.<br />
The Board makes all decisions pertaining to the Plan (COLAS, benefit factor, investment<br />
managers, etc.)<br />
WEB SITE ADDRESS- www.epcretirement.org:<br />
A Web Site has been established to provide more current and detailed information. Information<br />
provided:<br />
Benefit Calculator (Calculate your own benefit)<br />
Investment Performance<br />
Financial Statements<br />
Actuarial Report
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong><br />
DISCLAIMER<br />
Other Retirement Planning Tools<br />
El Paso County Retirement Plan Document<br />
Minutes of Meetings<br />
This summary information is intended to provide general information about the El Paso<br />
County Retirement Plan. The El Paso County Retirement Plan Document is the governing<br />
authority.
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong><br />
NOTICE OF PRIVACY PRACTICES<br />
GROUP MEDICAL PLAN<br />
(El Paso County Medical Group Plan)<br />
GROUP DENTAL PLAN<br />
(Guardian Dental Group Plan)<br />
FLEXIBLE SPENDING ACCOUNT (FSA) (PayFlex)<br />
THIS NOTICE DESCRIBES HOW HEALTH INFORMATION ABOUT YOU MAY BE<br />
USED AND DISCLOSED AND HOW YOU CAN GET ACCESS TO THIS<br />
INFORMATION. PLEASE REVIEW IT CAREFULLY.<br />
El Paso County provides many types of services, such as employee benefits, various health, welfare, and wellness<br />
activities as well as an assortment of social services. We must collect information about you in order to provide<br />
these services.<br />
At El Paso County, we respect your privacy and will protect your health information responsibly and professionally.<br />
Both Federal and State law require that we maintain the privacy of your health information.<br />
This Notice of Privacy Practices is being provided to you as a requirement of the Health Insurance Portability and<br />
Accountability Act (HIPAA) and describes how we may collect, use, and disclose your health information. It also<br />
describes your rights concerning your health information. El Paso County is required to abide by the terms of the<br />
Notice that’s currently in effect.<br />
As you read this Notice, you’ll see an important term: “Protected Health Information” or PHI. PHI is<br />
individually identifiable health information, including health and demographic information created, transmitted<br />
and/or received by us that can reasonably be used to identify you regardless of form (oral, written, or electronic).<br />
Some examples of PHI might be age, gender, and address information. PHI also includes information relating to<br />
your past, present, and future physical or mental health or condition, the provision of health care and/or health care<br />
related services, and payment for that care.<br />
To the extent practical or feasible, any PHI created, transmitted, received and/or otherwise used by us shall,<br />
regardless of form (oral, written, or electronic), be de-identified in order to protect individual privacy.
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong><br />
DESIGNATED PRIVACY OFFICER<br />
In compliance with HIPAA regulatory requirements, El Paso County has designated a “Privacy Officer” who is<br />
responsible for overseeing privacy
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong>
<strong>2013</strong> <strong>Employee</strong> Benefit <strong>Guidebook</strong><br />
Updated August <strong>2013</strong><br />
4 th Revision: January 1, <strong>2013</strong> (removed reference to Cigna and United Health Care Dental, changed Medical Plan<br />
Account number)<br />
5 th Distribution (sent by EBMS October 2012 to fulfill every three year requirement)<br />
5th Revision: September 1 st , 2012 (removed onsite pharmacy information and updated applicable program and cost<br />
information for <strong>2013</strong>. Not a material change to the document.)