Topical tacrolimus in atopic dermatitis: Effects of ... - Helda - Helsinki.fi
Topical tacrolimus in atopic dermatitis: Effects of ... - Helda - Helsinki.fi
Topical tacrolimus in atopic dermatitis: Effects of ... - Helda - Helsinki.fi
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
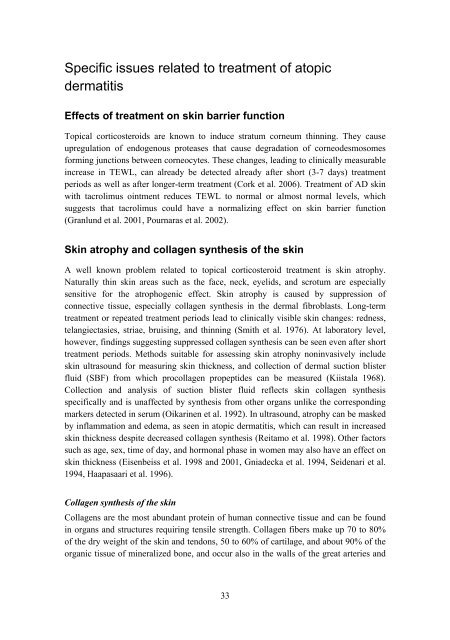
Speci<strong>fi</strong>c issues related to treatment <strong>of</strong> <strong>atopic</strong><br />
<strong>dermatitis</strong><br />
<strong>Effects</strong> <strong>of</strong> treatment on sk<strong>in</strong> barrier function<br />
<strong>Topical</strong> corticosteroids are known to <strong>in</strong>duce stratum corneum th<strong>in</strong>n<strong>in</strong>g. They cause<br />
upregulation <strong>of</strong> endogenous proteases that cause degradation <strong>of</strong> corneodesmosomes<br />
form<strong>in</strong>g junctions between corneocytes. These changes, lead<strong>in</strong>g to cl<strong>in</strong>ically measurable<br />
<strong>in</strong>crease <strong>in</strong> TEWL, can already be detected already after short (3-7 days) treatment<br />
periods as well as after longer-term treatment (Cork et al. 2006). Treatment <strong>of</strong> AD sk<strong>in</strong><br />
with <strong>tacrolimus</strong> o<strong>in</strong>tment reduces TEWL to normal or almost normal levels, which<br />
suggests that <strong>tacrolimus</strong> could have a normaliz<strong>in</strong>g effect on sk<strong>in</strong> barrier function<br />
(Granlund et al. 2001, Pournaras et al. 2002).<br />
Sk<strong>in</strong> atrophy and collagen synthesis <strong>of</strong> the sk<strong>in</strong><br />
A well known problem related to topical corticosteroid treatment is sk<strong>in</strong> atrophy.<br />
Naturally th<strong>in</strong> sk<strong>in</strong> areas such as the face, neck, eyelids, and scrotum are especially<br />
sensitive for the atrophogenic effect. Sk<strong>in</strong> atrophy is caused by suppression <strong>of</strong><br />
connective tissue, especially collagen synthesis <strong>in</strong> the dermal <strong>fi</strong>broblasts. Long-term<br />
treatment or repeated treatment periods lead to cl<strong>in</strong>ically visible sk<strong>in</strong> changes: redness,<br />
telangiectasies, striae, bruis<strong>in</strong>g, and th<strong>in</strong>n<strong>in</strong>g (Smith et al. 1976). At laboratory level,<br />
however, f<strong>in</strong>d<strong>in</strong>gs suggest<strong>in</strong>g suppressed collagen synthesis can be seen even after short<br />
treatment periods. Methods suitable for assess<strong>in</strong>g sk<strong>in</strong> atrophy non<strong>in</strong>vasively <strong>in</strong>clude<br />
sk<strong>in</strong> ultrasound for measur<strong>in</strong>g sk<strong>in</strong> thickness, and collection <strong>of</strong> dermal suction blister<br />
fluid (SBF) from which procollagen propeptides can be measured (Kiistala 1968).<br />
Collection and analysis <strong>of</strong> suction blister fluid reflects sk<strong>in</strong> collagen synthesis<br />
speci<strong>fi</strong>cally and is unaffected by synthesis from other organs unlike the correspond<strong>in</strong>g<br />
markers detected <strong>in</strong> serum (Oikar<strong>in</strong>en et al. 1992). In ultrasound, atrophy can be masked<br />
by <strong>in</strong>flammation and edema, as seen <strong>in</strong> <strong>atopic</strong> <strong>dermatitis</strong>, which can result <strong>in</strong> <strong>in</strong>creased<br />
sk<strong>in</strong> thickness despite decreased collagen synthesis (Reitamo et al. 1998). Other factors<br />
such as age, sex, time <strong>of</strong> day, and hormonal phase <strong>in</strong> women may also have an effect on<br />
sk<strong>in</strong> thickness (Eisenbeiss et al. 1998 and 2001, Gniadecka et al. 1994, Seidenari et al.<br />
1994, Haapasaari et al. 1996).<br />
Collagen synthesis <strong>of</strong> the sk<strong>in</strong><br />
Collagens are the most abundant prote<strong>in</strong> <strong>of</strong> human connective tissue and can be found<br />
<strong>in</strong> organs and structures requir<strong>in</strong>g tensile strength. Collagen <strong>fi</strong>bers make up 70 to 80%<br />
<strong>of</strong> the dry weight <strong>of</strong> the sk<strong>in</strong> and tendons, 50 to 60% <strong>of</strong> cartilage, and about 90% <strong>of</strong> the<br />
organic tissue <strong>of</strong> m<strong>in</strong>eralized bone, and occur also <strong>in</strong> the walls <strong>of</strong> the great arteries and<br />
33