Methods Applying AHRQ Quality Indicators to Healthcare ... - HCUP
Methods Applying AHRQ Quality Indicators to Healthcare ... - HCUP
Methods Applying AHRQ Quality Indicators to Healthcare ... - HCUP
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
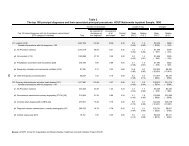
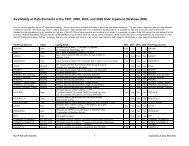
"clinical grouper" makes it easier <strong>to</strong> quickly understand patterns of diagnoses andprocedures. The target CCS for CHF was 108; the target CCS for asthma was128; the target CCS for asthma/COPD was 127 or 128; the target for pneumoniawas 122; and the target for AMI was 100.Discharged alive.Not a combined transfer record.For the CHF analysis, there was a fourth criterion that excluded records with hearttransplant procedures (any ICD-9-CM procedure code in the range 37.51-37.54).All discharges with non-missing patient discharge status were retained for the selectedpatients. A patient was allowed <strong>to</strong> have multiple index admissions, if they occurred morethan 30 days apart.5. Readmissions: This analysis considered readmissions within 30 days of an indexadmission (defined above). The 30-day window was defined from the end of the firstevent (discharge date) <strong>to</strong> the beginning of the second event (admission date). Thereadmission could occur at any hospital and was not limited <strong>to</strong> the hospital of the indexadmission. Readmissions may be discharged in January <strong>to</strong> December 2008, include apatient discharge status of “died”, and be combined transfer records. Three types ofreadmissions were evaluated for inclusion in the NHQR:Readmissions based on same principal diagnosis: If within 30 days of anindex admission, there was a discharge record for the same person with thesame principal diagnosis CCS, using the CCS categories noted above.Readmissions based on same diagnosis: If within 30 days of an indexadmission, there was a discharge record for the same person with the same CCSas a principal or secondary diagnosis. This type of readmission uses the sameCCS categories identified above.Readmissions for any diagnosis: If within 30 days of an index admission, therewas a discharge record for the same person, regardless of the principal orsecondary diagnosis.For the analysis we looked at both readmission rates and cost using the following methodology:Readmission Rates. Readmission rates were calculated as the percentage of index eventswith at least one readmission by reporting category: age (18-64, 65+), gender,race/ethnicity, and income quartile.Costs. The <strong>HCUP</strong> databases include information on <strong>to</strong>tal hospital charges. Using <strong>HCUP</strong>hospital-level cost-<strong>to</strong>-charge ratios based on hospital accounting reports from the Centersfor Medicare and Medicaid Services, 10 <strong>to</strong>tal charges are converted <strong>to</strong> costs. Costs will tend<strong>to</strong> reflect the actual costs of production, while charges represent what the hospital billed forthe stay. Hospital charges reflect the amount the hospital charged for the entire hospitalstay and does not include professional (physician) fees. The <strong>to</strong>tal and average cost was10 <strong>HCUP</strong> Cost-<strong>to</strong>-Charge Ratio Files (CCR). <strong>Healthcare</strong> Cost and Utilization Project (<strong>HCUP</strong>). August2011. U.S. Agency for <strong>Healthcare</strong> Research and <strong>Quality</strong>, Rockville, MD. www.hcupus.ahrq.gov/db/state/cost<strong>to</strong>charge.jsp.<strong>Methods</strong> for <strong>HCUP</strong> Data in 2011 NHQR and NHDR F-2December 9, 2011