best practice guidelines: wound management in diabetic foot ulcers
best practice guidelines: wound management in diabetic foot ulcers
best practice guidelines: wound management in diabetic foot ulcers
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
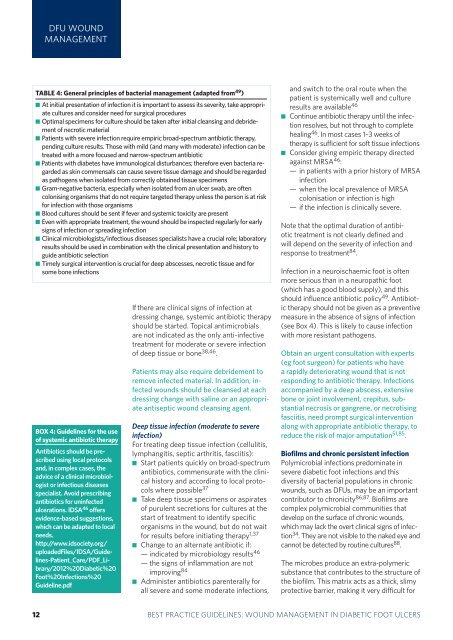
DFU WOUNDMANAGEMENTTABLE 4: General pr<strong>in</strong>ciples of bacterial <strong>management</strong> (adapted from 49 ) At <strong>in</strong>itial presentation of <strong>in</strong>fection it is important to assess its severity, take appropriatecultures and consider need for surgical procedures Optimal specimens for culture should be taken after <strong>in</strong>itial cleans<strong>in</strong>g and debridementof necrotic material Patients with severe <strong>in</strong>fection require empiric broad-spectrum antibiotic therapy,pend<strong>in</strong>g culture results. Those with mild (and many with moderate) <strong>in</strong>fection can betreated with a more focused and narrow-spectrum antibioticPatients with diabetes have immunological disturbances; therefore even bacteria regardedas sk<strong>in</strong> commensals can cause severe tissue damage and should be regardedas pathogens when isolated from correctly obta<strong>in</strong>ed tissue specimens Gram-negative bacteria, especially when isolated from an ulcer swab, are oftencolonis<strong>in</strong>g organisms that do not require targeted therapy unless the person is at riskfor <strong>in</strong>fection with those organisms Blood cultures should be sent if fever and systemic toxicity are present Even with appropriate treatment, the <strong>wound</strong> should be <strong>in</strong>spected regularly for earlysigns of <strong>in</strong>fection or spread<strong>in</strong>g <strong>in</strong>fection Cl<strong>in</strong>ical microbiologists/<strong>in</strong>fectious diseases specialists have a crucial role; laboratoryresults should be used <strong>in</strong> comb<strong>in</strong>ation with the cl<strong>in</strong>ical presentation and history toguide antibiotic selection Timely surgical <strong>in</strong>tervention is crucial for deep abscesses, necrotic tissue and forsome bone <strong>in</strong>fectionsBOX 4: Guidel<strong>in</strong>es for the useof systemic antibiotic therapyAntibiotics should be prescribedus<strong>in</strong>g local protocolsand, <strong>in</strong> complex cases, theadvice of a cl<strong>in</strong>ical microbiologistor <strong>in</strong>fectious diseasesspecialist. Avoid prescrib<strong>in</strong>gantibiotics for un<strong>in</strong>fectedulcerations. IDSA 46 offersevidence-based suggestions,which can be adapted to localneeds.http://www.idsociety.org/uploadedFiles/IDSA/Guidel<strong>in</strong>es-Patient_Care/PDF_Library/2012%20Diabetic%20Foot%20Infections%20Guidel<strong>in</strong>e.pdfIf there are cl<strong>in</strong>ical signs of <strong>in</strong>fection atdress<strong>in</strong>g change, systemic antibiotic therapyshould be started. Topical antimicrobialsare not <strong>in</strong>dicated as the only anti-<strong>in</strong>fectivetreatment for moderate or severe <strong>in</strong>fectionof deep tissue or bone 38,46 .Patients may also require debridement toremove <strong>in</strong>fected material. In addition, <strong>in</strong>fected<strong>wound</strong>s should be cleansed at eachdress<strong>in</strong>g change with sal<strong>in</strong>e or an appropriateantiseptic <strong>wound</strong> cleans<strong>in</strong>g agent.Deep tissue <strong>in</strong>fection (moderate to severe<strong>in</strong>fection)For treat<strong>in</strong>g deep tissue <strong>in</strong>fection (cellulitis,lymphangitis, septic arthritis, fasciitis): Start patients quickly on broad-spectrumantibiotics, commensurate with the cl<strong>in</strong>icalhistory and accord<strong>in</strong>g to local protocolswhere possible 37 Take deep tissue specimens or aspiratesof purulent secretions for cultures at thestart of treatment to identify specificorganisms <strong>in</strong> the <strong>wound</strong>, but do not waitfor results before <strong>in</strong>itiat<strong>in</strong>g therapy 1,37 Change to an alternate antibiotic if:— <strong>in</strong>dicated by microbiology results 46— the signs of <strong>in</strong>flammation are notimprov<strong>in</strong>g 84 Adm<strong>in</strong>ister antibiotics parenterally forall severe and some moderate <strong>in</strong>fections,and switch to the oral route when thepatient is systemically well and cultureresults are available 46 Cont<strong>in</strong>ue antibiotic therapy until the <strong>in</strong>fectionresolves, but not through to completeheal<strong>in</strong>g 46 . In most cases 1–3 weeks oftherapy is sufficient for soft tissue <strong>in</strong>fections Consider giv<strong>in</strong>g empiric therapy directedaga<strong>in</strong>st MRSA 46 :— <strong>in</strong> patients with a prior history of MRSA<strong>in</strong>fection— when the local prevalence of MRSAcolonisation or <strong>in</strong>fection is high— if the <strong>in</strong>fection is cl<strong>in</strong>ically severe.Note that the optimal duration of antibiotictreatment is not clearly def<strong>in</strong>ed andwill depend on the severity of <strong>in</strong>fection andresponse to treatment 84 .Infection <strong>in</strong> a neuroischaemic <strong>foot</strong> is oftenmore serious than <strong>in</strong> a neuropathic <strong>foot</strong>(which has a good blood supply), and thisshould <strong>in</strong>fluence antibiotic policy 49 . Antibiotictherapy should not be given as a preventivemeasure <strong>in</strong> the absence of signs of <strong>in</strong>fection(see Box 4). This is likely to cause <strong>in</strong>fectionwith more resistant pathogens.Obta<strong>in</strong> an urgent consultation with experts(eg <strong>foot</strong> surgeon) for patients who havea rapidly deteriorat<strong>in</strong>g <strong>wound</strong> that is notrespond<strong>in</strong>g to antibiotic therapy. Infectionsaccompanied by a deep abscess, extensivebone or jo<strong>in</strong>t <strong>in</strong>volvement, crepitus, substantialnecrosis or gangrene, or necrotis<strong>in</strong>gfasciitis, need prompt surgical <strong>in</strong>terventionalong with appropriate antibiotic therapy, toreduce the risk of major amputation 51,85 .Biofilms and chronic persistent <strong>in</strong>fectionPolymicrobial <strong>in</strong>fections predom<strong>in</strong>ate <strong>in</strong>severe <strong>diabetic</strong> <strong>foot</strong> <strong>in</strong>fections and thisdiversity of bacterial populations <strong>in</strong> chronic<strong>wound</strong>s, such as DFUs, may be an importantcontributor to chronicity 86,87 . Biofilms arecomplex polymicrobial communities thatdevelop on the surface of chronic <strong>wound</strong>s,which may lack the overt cl<strong>in</strong>ical signs of <strong>in</strong>fection34 . They are not visible to the naked eye andcannot be detected by rout<strong>in</strong>e cultures 88 .The microbes produce an extra-polymericsubstance that contributes to the structure ofthe biofilm. This matrix acts as a thick, slimyprotective barrier, mak<strong>in</strong>g it very difficult for312 BEST PRACTICEBEST PRACTICEGUIDELINESGUIDELINES:FOR SKINWOUNDAND WOUNDMANAGEMENTCARE ININEPIDERMOLYSISDIABETIC FOOTBULLOSAULCERS