jiafm, 2010-32(2) april-june. - forensic medicine
jiafm, 2010-32(2) april-june. - forensic medicine
jiafm, 2010-32(2) april-june. - forensic medicine
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
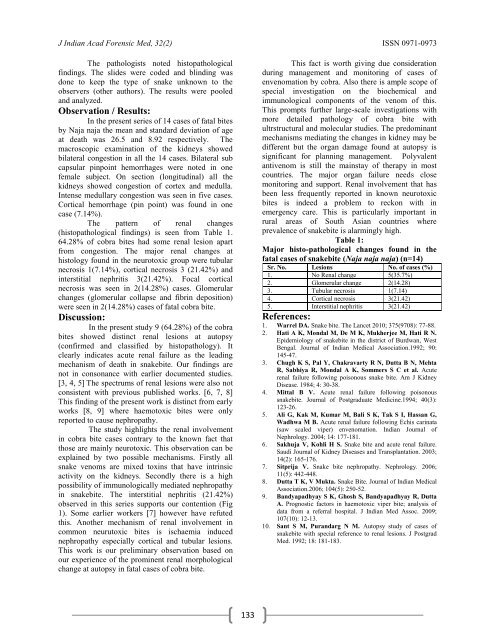
J Indian Acad Forensic Med, <strong>32</strong>(2) ISSN 0971-0973The pathologists noted histopathologicalfindings. The slides were coded and blinding wasdone to keep the type of snake unknown to theobservers (other authors). The results were pooledand analyzed.Observation / Results:In the present series of 14 cases of fatal bitesby Naja naja the mean and standard deviation of ageat death was 26.5 and 8.92 respectively. Themacroscopic examination of the kidneys showedbilateral congestion in all the 14 cases. Bilateral subcapsular pinpoint hemorrhages were noted in onefemale subject. On section (longitudinal) all thekidneys showed congestion of cortex and medulla.Intense medullary congestion was seen in five cases.Cortical hemorrhage (pin point) was found in onecase (7.14%).The pattern of renal changes(histopathological findings) is seen from Table 1.64.28% of cobra bites had some renal lesion apartfrom congestion. The major renal changes athistology found in the neurotoxic group were tubularnecrosis 1(7.14%), cortical necrosis 3 (21.42%) andinterstitial nephritis 3(21.42%). Focal corticalnecrosis was seen in 2(14.28%) cases. Glomerularchanges (glomerular collapse and fibrin deposition)were seen in 2(14.28%) cases of fatal cobra bite.Discussion:In the present study 9 (64.28%) of the cobrabites showed distinct renal lesions at autopsy(confirmed and classified by histopathology). Itclearly indicates acute renal failure as the leadingmechanism of death in snakebite. Our findings arenot in consonance with earlier documented studies.[3, 4, 5] The spectrums of renal lesions were also notconsistent with previous published works. [6, 7, 8]This finding of the present work is distinct from earlyworks [8, 9] where haemotoxic bites were onlyreported to cause nephropathy.The study highlights the renal involvementin cobra bite cases contrary to the known fact thatthose are mainly neurotoxic. This observation can beexplained by two possible mechanisms. Firstly allsnake venoms are mixed toxins that have intrinsicactivity on the kidneys. Secondly there is a highpossibility of immunologically mediated nephropathyin snakebite. The interstitial nephritis (21.42%)observed in this series supports our contention (Fig1). Some earlier workers [7] however have refutedthis. Another mechanism of renal involvement incommon neurutoxic bites is ischaemia inducednephropathy especially cortical and tubular lesions.This work is our preliminary observation based onour experience of the prominent renal morphologicalchange at autopsy in fatal cases of cobra bite.This fact is worth giving due considerationduring management and monitoring of cases ofenvenomation by cobra. Also there is ample scope ofspecial investigation on the biochemical andimmunological components of the venom of this.This prompts further large-scale investigations withmore detailed pathology of cobra bite withultrstructural and molecular studies. The predominantmechanisms mediating the changes in kidney may bedifferent but the organ damage found at autopsy issignificant for planning management. Polyvalentantivenom is still the mainstay of therapy in mostcountries. The major organ failure needs closemonitoring and support. Renal involvement that hasbeen less frequently reported in known neurotoxicbites is indeed a problem to reckon with inemergency care. This is particularly important inrural areas of South Asian countries whereprevalence of snakebite is alarmingly high.Table 1:Major histo-pathological changes found in thefatal cases of snakebite (Naja naja naja) (n=14)Sr. No. Lesions No. of cases (%)1. No Renal change 5(35.7%)2. Glomerular change 2(14.28)3. Tubular necrosis 1(7.14)4. Cortical necrosis 3(21.42)5. Interstitial nephritis 3(21.42)References:1. Warrel DA. Snake bite. The Lancet <strong>2010</strong>; 375(9708): 77-88.2. Hati A K, Mondal M, De M K, Mukherjee M, Hati R N.Epidemiology of snakebite in the district of Burdwan, WestBengal. Journal of Indian Medical Association.1992; 90:145-47.3. Chugh K S, Pal Y, Chakravarty R N, Dutta B N, MehtaR, Sabhiya R, Mondal A K, Sommers S C et al. Acuterenal failure following poisonous snake bite. Am J KidneyDisease. 1984; 4: 30-38.4. Mittal B V. Acute renal failure following poisonoussnakebite. Journal of Postgraduate Medicine.1994; 40(3):123-26.5. Ali G, Kak M, Kumar M, Bali S K, Tak S I, Hassan G,Wadhwa M B. Acute renal failure following Echis carinata(saw scaled viper) envenomation. Indian Journal ofNephrology. 2004; 14: 177-181.6. Sakhuja V, Kohli H S. Snake bite and acute renal failure.Saudi Journal of Kidney Diseases and Transplantation. 2003;14(2): 165-176.7. Sitprija V. Snake bite nephropathy. Nephrology. 2006;11(5): 442-448.8. Dutta T K, V Mukta. Snake Bite. Journal of Indian MedicalAssociation.2006; 104(5): 250-52.9. Bandyapadhyay S K, Ghosh S, Bandyapadhyay R, DuttaA. Prognostic factors in haemotoxic viper bite; analysis ofdata from a referral hospital. J Indian Med Assoc. 2009;107(10): 12-13.10. Sant S M, Purandarg N M. Autopsy study of cases ofsnakebite with special reference to renal lesions. J PostgradMed. 1992; 18: 181-183.133


![syllabus in forensic medicine for m.b.b.s. students in india [pdf]](https://img.yumpu.com/48405011/1/190x245/syllabus-in-forensic-medicine-for-mbbs-students-in-india-pdf.jpg?quality=85)



![SPOTTING IN FORENSIC MEDICINE [pdf]](https://img.yumpu.com/45856557/1/190x245/spotting-in-forensic-medicine-pdf.jpg?quality=85)

![JAFM-33-2, April-June, 2011 [PDF] - forensic medicine](https://img.yumpu.com/43461356/1/190x245/jafm-33-2-april-june-2011-pdf-forensic-medicine.jpg?quality=85)

![JIAFM-33-4, October-December, 2011 [PDF] - forensic medicine](https://img.yumpu.com/31013278/1/190x245/jiafm-33-4-october-december-2011-pdf-forensic-medicine.jpg?quality=85)