General Practice BILLING GUIDE - British Columbia Medical ...
General Practice BILLING GUIDE - British Columbia Medical ...
General Practice BILLING GUIDE - British Columbia Medical ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
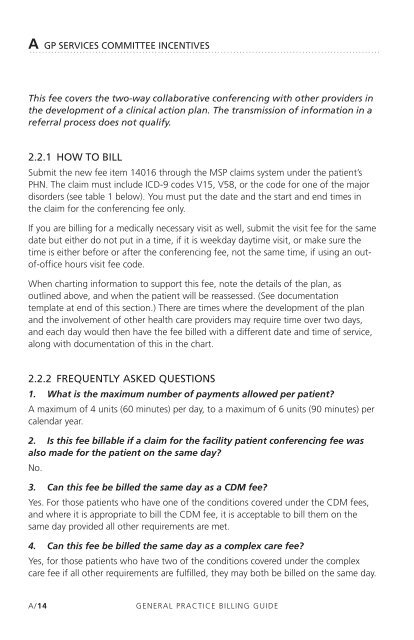
A GP SERVICES COMMITTEE INCENTIVES<br />
This fee covers the two-way collaborative conferencing with other providers in<br />
the development of a clinical action plan. The transmission of information in a<br />
referral process does not qualify.<br />
2.2.1 hOW TO BIll<br />
Submit the new fee item 14016 through the MSP claims system under the patient’s<br />
PHN. The claim must include ICD-9 codes V15, V58, or the code for one of the major<br />
disorders (see table 1 below). You must put the date and the start and end times in<br />
the claim for the conferencing fee only.<br />
If you are billing for a medically necessary visit as well, submit the visit fee for the same<br />
date but either do not put in a time, if it is weekday daytime visit, or make sure the<br />
time is either before or after the conferencing fee, not the same time, if using an outof-office<br />
hours visit fee code.<br />
When charting information to support this fee, note the details of the plan, as<br />
outlined above, and when the patient will be reassessed. (See documentation<br />
template at end of this section.) There are times where the development of the plan<br />
and the involvement of other health care providers may require time over two days,<br />
and each day would then have the fee billed with a different date and time of service,<br />
along with documentation of this in the chart.<br />
2.2.2 FREqUENTly ASKED qUESTIONS<br />
1. What is the maximum number of payments allowed per patient?<br />
A maximum of 4 units (60 minutes) per day, to a maximum of 6 units (90 minutes) per<br />
calendar year.<br />
2. Is this fee billable if a claim for the facility patient conferencing fee was<br />
also made for the patient on the same day?<br />
No.<br />
3. Can this fee be billed the same day as a CDM fee?<br />
Yes. For those patients who have one of the conditions covered under the CDM fees,<br />
and where it is appropriate to bill the CDM fee, it is acceptable to bill them on the<br />
same day provided all other requirements are met.<br />
4. Can this fee be billed the same day as a complex care fee?<br />
Yes, for those patients who have two of the conditions covered under the complex<br />
care fee if all other requirements are fulfilled, they may both be billed on the same day.<br />
A/14<br />
GENERAL PRACTICE <strong>BILLING</strong> <strong>GUIDE</strong>