Chapter 80
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Patient Positioning and<br />
Precautions During<br />
Anesthesia and Surgery<br />
<strong>80</strong><br />
CHAPTER<br />
Ahmed Mohamed Shalabi<br />
INTRODUCTION<br />
Proper patient positioning is an important but often overlooked<br />
part of the surgical plan. It not only allows optimal surgical<br />
exposure and reduces surgeon fatigue but also ensures the patient’s<br />
comfort and protection from injury. Physiologic changes that<br />
occur as a result of positioning have their origins primarily in<br />
gravitational effects.<br />
GENERAL GUIDELINES AND<br />
PRECAUTIONS FOR POSITIONING<br />
Frequently, a small child is happy to sit up and play but has no<br />
intention of lying down on the operating table. In such cases, it is<br />
much better to proceed with induction with the child sitting up<br />
near the upper edge of the operating table and his or her back<br />
supported by the anesthesiologist’s chest or arms or resting on her<br />
or her lap. This should not be considered a mandatory approach<br />
for induction of anesthesia, but rather, one method out of many<br />
that reduces stress and anxiety for the child. Of course, the choice<br />
depends on the medical condition, the type of premedication used,<br />
and the surgical situation. For instance, preoxygenation is more<br />
effective in 25 degrees head-up position than in supine position in<br />
severely obese patients and/or patients with poor pulmonary<br />
reserves. 1 The following considerations must be observed before<br />
beginning the anesthesia: (1) ensure that the operating room table<br />
is working properly; (2) ask the surgical personnel about the<br />
position of the patient for surgery; (3) ensure that help will be<br />
available for positioning and communicate clearly the different<br />
steps to achieve position before the patient is moved to avoid<br />
personnel injuries; (4) prepare all needed material and equipment<br />
for positioning (e.g., padding, rolls, blankets, tape); (5) move the<br />
patient slowly while protecting the airway, intravenous lines,<br />
drains, monitoring cables, and other equipment; and (6) once the<br />
patient is positioned, recheck everything, particularly to ensure<br />
proper lung ventilation and avoid pressure points and neuro -<br />
vascular compressions. The anesthesiologist is responsible at all<br />
times for the airway equipment and the handling of the head of the<br />
patient. In this position, she or he can better guide the positioning<br />
of the patient and ensure safety during this precarious maneuver.<br />
Many anesthesiologists prefer disconnecting the monitor cables<br />
and intravenous and arterial lines just before positioning in order<br />
to prevent accidental removal or kinking. It helps, while recon -<br />
necting the monitoring cables and vascular lines, to ensure proper<br />
functioning, prevent pressure points, and provide proper padding<br />
to protect the patient against potential injury. 2 However, to mini -<br />
mize the time while the patient is not monitored, it is recom -<br />
mended to remove the pulse oximeter just before positioning and<br />
replace it immediately after positioning. Proper lung ventilation<br />
should be confirmed immediately by capnography and chest<br />
auscultation. The team should be prepared to return the patient to<br />
the supine position immediately if, for unknown reason, the<br />
patient’s safety cannot be ensured in this new position. General<br />
review of the items that should be checked and verified during a<br />
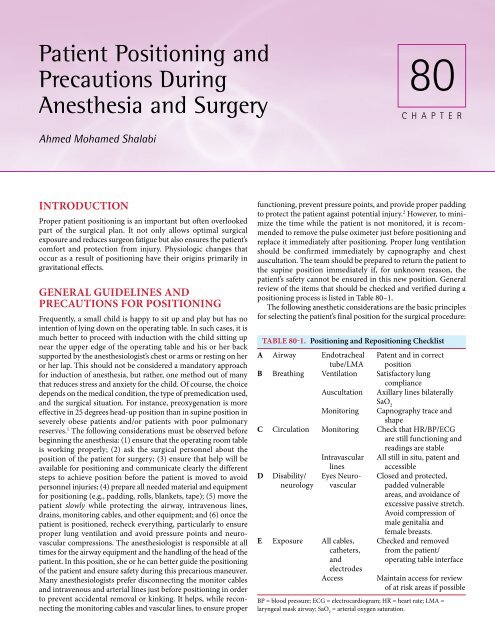
positioning process is listed in Table <strong>80</strong>–1.<br />
The following anesthetic considerations are the basic principles<br />
for selecting the patient’s final position for the surgical procedure:<br />
A<br />
B<br />
C<br />
D<br />
E<br />
TABLE <strong>80</strong>-1. Positioning and Repositioning Checklist<br />
Airway<br />
Breathing<br />
Circulation<br />
Disability/<br />
neurology<br />
Exposure<br />
Endotracheal<br />
tube/LMA<br />
Ventilation<br />
Auscultation<br />
Monitoring<br />
Monitoring<br />
Intravascular<br />
lines<br />
Eyes Neurovascular<br />
All cables,<br />
catheters,<br />
and<br />
electrodes<br />
Access<br />
Patent and in correct<br />
position<br />
Satisfactory lung<br />
compliance<br />
Axillary lines bilaterally<br />
SaO 2<br />
Capnography trace and<br />
shape<br />
Check that HR/BP/ECG<br />
are still functioning and<br />
readings are stable<br />
All still in situ, patent and<br />
accessible<br />
Closed and protected,<br />
padded vulnerable<br />
areas, and avoidance of<br />
excessive passive stretch.<br />
Avoid compression of<br />
male genitalia and<br />
female breasts.<br />
Checked and removed<br />
from the patient/<br />
operating table interface<br />
Maintain access for review<br />
of at risk areas if possible<br />
BP = blood pressure; ECG = electrocardiogram; HR = heart rate; LMA =<br />
laryngeal mask airway; SaO 2<br />
= arterial oxygen saturation.
1342 PART 4 ■ Special Monitoring and Resuscitation Techniques<br />
(1) Does the position allow proper surgical exposure? (2) Does<br />
the position allow access to the airway at all time, to vascular<br />
access, and monitors? (3) Does the position stretch muscles or<br />
hyperextend joints unacceptably? (4) Does the position increase<br />
the risk of pressure points on the skin or neurovascular structures?<br />
(5) Is ventilation and/or circulation compromised? (6) Does the<br />
position respect the patient’s physiologic condition? and (7) Does<br />
the position affect the proposed anesthetic technique and increase<br />
the risk of complications related to the suggested position.<br />
For instance, the position chosen for the administration of<br />
spinal anesthesia should ensure that the head of the patient is<br />
neither up nor down to prevent sudden hemodynamic complica -<br />
tions if the head is down, allowing for the local anesthetic to move<br />
upward; or an insufficient block level if the head is up, allowing<br />
the local anesthetic to move downward by gravity.<br />
Figure <strong>80</strong>-2. The “lawnchair” position. The advantage of the<br />
position lies in the comfort of the awake or sedated patient<br />
because the weight of the body is more evenly distributed, and<br />
in addition, it permits less strain at the hips and knee joints.<br />
SUPINE POSITION<br />
General Considerations<br />
The supine position is the most commonly used surgical position.<br />
It is well tolerated and causes no important effect on the phy -<br />
siologic systems in normal adults and children. It is normally used<br />
in most circumstances at the beginning of anesthesia to the secure<br />
the airway, ensure proper lung ventilation, and place vascular<br />
access and monitoring equipment. However, because the head of<br />
an infant and a small child is large in comparison with the trunk,<br />
it is highly recommended to use a head ring (the shape of a donut)<br />
and a roll under the shoulders to maintain the head in position<br />
for induction and airway management. Furthermore, the use of<br />
this roll under the shoulders will limit the neck flexion and<br />
improve airway patency.<br />
Variation of Supine Positions<br />
With the traditional supine position, the patient lies on his or her<br />
back and the head is supported on a pillow. The arms are placed<br />
by the side of the body or rest on outstretched armboards. The<br />
weight of the patient rests on the occiput, back and scapula,<br />
sacrum, dorsal legs, and heels (Figure <strong>80</strong>–1). There is a loss of the<br />
normal lumbar lordosis that may lead to postoperative backache<br />
and is usually associated to the duration of the surgery. With the<br />
contoured supine/lawnchair position, the hips and knees are slightly<br />
flexed into an anatomically neutral joint position using soft rolls<br />
underneath the knees, reproducing the position assumed when<br />
one is resting in a reclining chair. This is a more natural position,<br />
especially during prolonged surgical procedures. With a pillow<br />
beneath the shoulders and the head slightly elevated above the<br />
level of the atrium, a reduction of cerebral venous pressure is<br />
ensured. This posture should be considered over the traditional<br />
supine position for the older and larger child (Figure <strong>80</strong>–2). Care<br />
should be taken to ensure that the venous return from the lower<br />
limbs is not jeopardized by external compression. The frogleg<br />
supine position is achieved by simultaneous flexion of the knees<br />
and hips while the hips are externally rotated, bringing the heels<br />
together in the midline. The thighs are externally rotated at the<br />
hips. Pillows are placed beneath the knees and on the lateral sides<br />
of the thighs and lower legs (Figure <strong>80</strong>–3). This posture allows<br />
procedures to be performed on the medial thigh, genitalia, and<br />
perineum. The supine hanging leg position is used during opera -<br />
tions involving the knee joint with the patient moved to the end of<br />
the operating table, allowing the knee to overhang the edge of the<br />
table.<br />
Physiologic Effects of the Supine Position<br />
The normal hydrostatic effect of gravity on venous return is insi -<br />
gnificant in the supine position. As a result, the change of posture<br />
from an erect to a supine position results in an initial increase in<br />
venous return with a subsequent increase in pulmo nary perfusion<br />
and an increase in cardiac output and arterial pressure. This effect<br />
is not sustained because compensating mechanisms (via arterial<br />
baroreceptors in the walls of the aorta and the carotid arteries) are<br />
initiated, resulting in the reduction of heart rate, stroke volume,<br />
peripheral resistance, and mean arterial pressure (MAP). Regional<br />
Figure <strong>80</strong>-1. Supine position.<br />
Figure <strong>80</strong>-3. The “frogleg” supine position allows excellent surgical<br />
exposure to the perineum and groin. Excessive strain or<br />
stretch at the hip joints is minimized by supporting the lateral<br />
aspects of the legs.
CHAPTER <strong>80</strong> ■ Patient Positioning and Precautions During Anesthesia and Surgery 1343<br />
pulmonary circulation is mainly distributed within the lung below<br />
the right atrium. Preferential perfusion to the dependent lung<br />
areas remain unchanged in awake and anesthetized patients. There<br />
is a reversal of the dependence ventilation in the conscious patient<br />
to that of the increased ven tilation to the nondependent portions<br />
of the lungs in anesthetized patients, resulting in an increased in<br />
the ventilation-perfusion (V˙/Q˙) mismatch and, consequently,<br />
hypoxemia.<br />
The effect of gravity accounts for the majority of the physiolo -<br />
gic changes in the supine position with alterations in respiratory<br />
mechanics, ventilation, and perfusion. In the upright posture, the<br />
position of the diaphragm is determined by the balance of forces<br />
between the cephalad pull by the lungs’ elastic recoil forces and<br />
the caudad pull by the weight of the abdominal contents. The<br />
diaphragm is displaced cephalad owing to the combined forces of<br />
the lungs’ elastic recoil and the hydrostatic forces of the abdominal<br />
contents. During quiet breathing in the awake subject or spon -<br />
taneous respiration in an anesthetized patient, there is only a<br />
minor cephalad shift of the diaphragm dome. However, anes -<br />
thetized and paralyzed patients show greater cephalad shift, with<br />
the dorsal part of the diaphragm most significantly displaced. 3<br />
Studies in the pediatric population demonstrated similar<br />
respiratory alterations with postural changes. In healthy children,<br />
the functional residual capacity (FRC) in the supine position is<br />
lower than sitting FRC by 25 to 30%. 4 Hypoxemia may occur if<br />
the FRC is less than the closing volume and small airway closure<br />
occurs during exhalation. Some small airways will in fact be closed<br />
throughout the respiratory cycle, leading to a reduction in lung<br />
compliance. The closing volume is much higher in neonates and<br />
infants because of the decrease in elastic tissues present in the<br />
lungs. Consequently, in infants, the small terminal alveoli at the<br />
dependent portions of the lungs would be closed by atelectasis at<br />
the end of each breath. Healthy infants can overcome this<br />
tendency by constant activity and crying. As in adults, induction<br />
of anesthesia is associated with a significant reduction in the FRC.<br />
Computed tomography (CT) revealed that atelectasis occurs on<br />
induction of anesthesia in pediatric patients. 5 Anesthesia with<br />
spontaneous breathing increased the volume of atelectasis mea -<br />
sured whereas anesthesia with mechanical ventilation significantly<br />
decreased the volume of atelectasis present at end-expiration. In<br />
anesthetized-paralyzed healthy adults, the amount of atelectasis<br />
formation in dependent lung regions could be as much as 16<br />
to 20% of the normal aerated lung tissue as seen on spiral CT.<br />
The distribution of atelectasis is nonhomogeneous, with the<br />
amount of atelectasis greatest near the diaphragm and less at<br />
the apex of the lungs. This suggests that relaxation and cranial<br />
shift of the diaphragm that compresses the dependent portion of<br />
the lungs could be responsible for the formation of these atelectatic<br />
regions. 6<br />
Atelectasis is an important cause of impaired gas exchange<br />
during general anesthesia because it causes pulmonary shunting<br />
and regions with low V˙/Q˙ ratios. The pulmonary shunt increases<br />
up to 12% and is located in dependent lung regions corresponding<br />
to the atelectatic areas. Atelectasis development occupied 0.6 to<br />
7% of the intrathoracic area. Increasing tidal volumes will abolish<br />
the reduction in FRC and minimize the degree of atelectasis. Reexpansion<br />
of the atelectatic regions by the application of positive<br />
end-expiratory pressure (PEEP) has also been shown to be effec -<br />
tive in reversing atelectasis and improving arterial oxygenation. 7<br />
The institution of muscle paralysis and intermittent positivepres<br />
sure ventilation results in preferential ventilation to the non -<br />
depen dent portions of the lungs. However, the anesthetic agent may<br />
play an important role in the changes in lung volumes. For instance,<br />
the FRC did not change during induction of anesthesia with<br />
ketamine in children who were spontaneously breathing. 8 Similar to<br />
adults, total respiratory compliance is decreased after induction of<br />
anesthesia in supine infants breathing spontaneously. This can be<br />
prevented by increasing tidal volume in the paralyzed children to<br />
match tidal volumes of these infants during the sedated state. 9,10<br />
Complications of the Supine Position<br />
Several skin surfaces are placed at risk for injury from direct<br />
pressure (Figure <strong>80</strong>–4). Decreased skin blood flow may favor<br />
blistering and skin necrosis. In small infants and children, the<br />
scalp is at risk during prolonged anesthesia in the supine position.<br />
Most often, the occipital area bears the full weight of the head,<br />
creating the potential for pressure-induced ischemia and hair loss.<br />
Alopecia (circular bald spot) may appear only days or weeks after<br />
the procedure. Even the adequate padding may not prevent this<br />
injury during very long procedures. Lifting the head and massag -<br />
ing the scalp briefly or turning the head at reasonable intervals<br />
seem appropriate to prevent this problem. Supraorbital nerve<br />
compression from the anesthetic ventilation circuit or tracheal<br />
tube or from pressure from the facemask or strap placement may<br />
lead to permanent supraorbital paresthesia. Coexisting medical<br />
problems (e.g., diabetes mellitus, uremia, hypothyroidism, polycythemia<br />
vera, hypothermia) may also contribute to nerve injury.<br />
The potential causes of nerve injury include:<br />
●<br />
●<br />
●<br />
●<br />
Section (e.g., type of surgery [sternotomy]).<br />
Compression (e.g., prolonged tourniquet [>2 h]).<br />
Traction (e.g., prolonged position (>4 h lithotomy]).<br />
Ischemia (e.g., congenital anomalies [cervical rib and thoracic<br />
outlet syndrome]).<br />
Figure <strong>80</strong>-4. Area at risk for pressure<br />
point injuries in the supine<br />
position. A: Scalp over the occiput.<br />
B: Condylar groove. C: Skin over<br />
the sacrum. D: Area over the<br />
Achilles tendon and foot.<br />
1 2 3 4
1344 PART 4 ■ Special Monitoring and Resuscitation Techniques<br />
●<br />
●<br />
Neurovascular compromise:<br />
• Compression or stretching of intraneural vasa nervorum—<br />
neural ischemia.<br />
• Nerve has a long or superficial course between two points of<br />
fixation.<br />
• Stretching and compression combined—worst.<br />
• Tissue edema from intravenous fluid may contribute to neurovascular<br />
compression.<br />
Equipment malfunction is another cause of problems, especially<br />
tourniquets, blood pressure cuffs, infusion pumps or armboards.<br />
The brachial plexus is at risk from pressure-induced ischemia<br />
and stretch injury, and it is the second most common nerve injury<br />
reported under anesthesia. The most common mode of brachial<br />
plexus injury is through excessive stretching of the nerves. Stretchinduced<br />
neuropathy of the brachial plexus remains a frequently<br />
preventable complication. The arms of the patient are frequently<br />
abducted and externally rotated for ease of access to the monitors<br />
and intravenous access. With the arm held in constant abduction,<br />
flexion of the neck to the contralateral side puts the brachial plexus<br />
under tension with the head of the humerus being a pivot point for<br />
the stretch. Neurapraxia may result. Modification of the supine<br />
position with the arm suspended above the head may also result<br />
in stretch injury to the brachial plexus when extreme abduction or<br />
anterior flexion of the arm is performed and especially if com -<br />
bined with contralateral neck rotation. The anesthesiologist should<br />
always be vigilant to guard against extremes of movement during<br />
the course of the surgical procedure to minimize the risk of peri -<br />
operative neuropathy. In adult patients, brachial plexus formed<br />
the second most common site of anesthesia-related nerve injury in<br />
the American Society of Anesthesiologists (ASA) Closed Claims<br />
Database (20% of 4183 claims). 11 The diagnosis is established on<br />
the basis of pain, numbness, and decreased movement noted<br />
immediately postoperatively to 48 hours postsurgery. Brachial<br />
plexus injury may present in the first postoperative day with pain<br />
in the neck and upper arm accompanied by sensory anesthesia<br />
and motor function loss. Commonly, only the upper roots (C5–7,<br />
Erb’s palsy) with upper arm and forearm are involved. Rarely, the<br />
lower roots (C8–T1) with predominantly hand involvement or the<br />
whole plexus may be damaged. Full recovery is expected if incom -<br />
plete lesions are present, although regeneration may take 3 to 6<br />
months. If there is no evidence of activity, stretch injuries may<br />
have a poor prognosis because not only are the axons injured but<br />
also the tubular conduits, which permit regeneration, are affected.<br />
In 2000, the ASA published a practice advisory for the prevention<br />
of perioperative peripheral neuropathies. 12 This advisory made<br />
several recommendations that may decrease the incidence of<br />
neuropathies and are listed in Table <strong>80</strong>–2.<br />
Ulnar nerve injury accounts for nearly one third of all nerve<br />
injuries associated with anesthesia and is the most common<br />
anesthesia-related neuropathy. Traction injury occurs with exten -<br />
sion and lateral displacement of the neck, with resultant increased<br />
TABLE <strong>80</strong>-2. Summary of Task Force Consensus by the American Society of Anesthesiologists<br />
Preoperative Assessment<br />
● When judged appropriate, it is helpful to ascertain that patients can comfortably tolerate the anticipated operative position.<br />
Upper Extremity Positioning<br />
● Arm abduction should be limited to 90 degrees in supine patients; patients who are positioned prone may comfortably tolerate<br />
arm abduction > 90 degrees.<br />
● Arms should be positioned to decrease pressure on the postcondylar groove of the humerus (ulnar groove). When arms are<br />
tucked at the side, a neutral forearm position is recommended. When arms are abducted on armboards, either supination or a<br />
neutral forearm position is acceptable.<br />
● Prolonged pressure on the radial nerve in the spiral groove of the humerus should be avoided.<br />
● Extension of the elbow beyond a comfortable range may stretch the median nerve.<br />
Lower Extremity Positioning<br />
● Lithotomy positions that stretch the hamstring muscle group beyond a comfortable range may stretch the sciatic nerve.<br />
● Prolonged pressure on the peroneal nerve at the fibular head should be avoided.<br />
● Neither extension nor flexion of the hip increases the risk of femoral neuropathy.<br />
Protective Padding<br />
● Padded armboards may decrease the risk of upper extremity neuropathy.<br />
● The use of chest rolls in laterally positioned patients may decrease the risk of upper extremity neuropathies.<br />
● Padding at the elbow and at the fibular head may decrease the risk of upper and lower extremity neuropathies, respectively.<br />
Equipment<br />
● Properly functioning automated blood pressure cuffs on the upper arms do not affect the risk of upper extremity neuropathies.<br />
● Shoulder braces in steep head-down positions may increase the risk of brachial plexus neuropathies.<br />
Postoperative Assessment<br />
● A simple postoperative assessment of extremity nerve function may lead to early recognition of peripheral neuropathies.<br />
Documentation<br />
● Charting specific positioning actions during the care of patients may result in improvements of care by (1) helping practitioners<br />
focus attention on relevant aspects of patient positioning and (2) providing information that continuous improvement processes<br />
can use to lead to refinements in patient care.
CHAPTER <strong>80</strong> ■ Patient Positioning and Precautions During Anesthesia and Surgery 1345<br />
traction on the contralateral brachial plexus, or when the arm is<br />
abducted more than 90 degrees with posterior displacement that<br />
will increase tension of the ipsilateral ulnar nerve. At the elbow, the<br />
ulnar nerve runs superficially behind the medial epicondyle of the<br />
humerus (condylar groove); at this location, direct prolonged<br />
compression or indirect compression during elbow flexion due to<br />
stretch of the cubital tunnel retinaculum between the medial<br />
epicondyle and the olecranon process can render the nerve<br />
ischemic with resultant neurapraxia. Positioning the arm and wrist<br />
dorsally and in extension to secure an indwelling arterial catheter<br />
may also lead to compression of the nerve at the wrist. Injury to<br />
the ulnar is disabling, because the small muscles of the hands will<br />
be paralyzed. Vigilance is mandatory to keep the elbow well<br />
padded and the position of the arm noted at all times during the<br />
surgical procedure. Unfortunately, treatment of established lesions<br />
has yielded mixed results. 13<br />
Median nerve injury results from extreme wrist dorsiflexion or<br />
from extravasations in the antecubital fossa. Very tight blood<br />
pressure cuffs and upper limb tourniquets can cause radial nerve<br />
injury.<br />
Lower limb neuropathies are more common in the lithotomy<br />
position than in neutral supine positions. In the supine patient,<br />
injury to the sciatic nerve is uncommon; however, it could result<br />
from a direct stretch or compression secondary to strangulation of<br />
its blood supply. This complication can lead to a compartment<br />
syndrome. Positioning of the buttock over an edge of the operating<br />
table or on beanbags placed to elevate and stabilize the leg during<br />
arthroscopy can result in compression injury to the sciatic nerve.<br />
The common peroneal nerve, a branch of the sciatic nerve, can be<br />
damage by direct pressure around the neck of the fibula. The<br />
common peroneal nerve is more frequently affected than the<br />
sciatic. All muscles below the knee are paralyzed and the patient<br />
will present with a footdrop. There is also loss of sensation below<br />
the knee except for the area distributed medially supplied by the<br />
saphenous nerve. Femoral neuropathy can result from improper<br />
placement of abdominal wall retractors, which causes direct com -<br />
pression of the iliopsoas muscle resulting in direct compression<br />
of the nerve, or from occluding the external iliac vessels or pene -<br />
trating vessels, causing ischemic injury to the nerve.<br />
Management of postoperative neuropathy can be carried on as<br />
follows:<br />
1. If a sensory disorder is present usually in the form of numbness<br />
and/or tingling, reassure the patient because it usually resolves<br />
during the first 5 postoperative days. If it persists for longer<br />
than 5 days, consult a neurologist.<br />
2. If a motor disorder is present, consult a neurologist imme -<br />
diately. Usually, neurophysiologic studies are done as electro -<br />
myography and nerve conduction studies.<br />
Improper handling and positioning of the head and neck in<br />
certain patients such as those with Down syndrome, achondro -<br />
plasia, Morquio-Brailsford syndrome, or cervical instability may<br />
predispose to cervical cord complications. The range of movement<br />
for flexion, extension, and lateral flexion should be determined<br />
before anesthesia, and the limits of motion, especially flexion and<br />
extension, avoided. Extremes of position (rotation, lateral flexion)<br />
and improper care during patient movement also place the<br />
cervical spine at risk. When transferring the anesthetized patient,<br />
it is important that the head move as one unit with the trunk,<br />
because “whiplash” injury may occur if the trunk moves faster<br />
than the head and neck. Hyperextension of the knee may result in<br />
ligament stretch and pain over the posterior joint capsule. Com -<br />
partment syndrome of the lower limbs is a very rare complication<br />
in a patient lying in the supine position. This may occur, however,<br />
when the calves are resting on a hard cushion used to maintain<br />
knee flexion during a lengthy procedure, leading to rhabdomyoly -<br />
sis and myoglobinuria. 14<br />
HEAD-UP TILT POSITIONS/REVERSE<br />
TRENDELENBURG POSITION<br />
Physiology of the Head-Up Tilt/Reverse<br />
Trendelenburg Position<br />
Changes in respiratory system mechanics are relatively small in<br />
healthy awake subjects owing to adaptability of total chest wall<br />
mechanics. A change of posture from the supine to a 30-degree<br />
head-up tilt results in a negligible decrease in the chest wall and<br />
lung elastances and improved compliance 15,16 but increases the<br />
FRC by nearly 20%. In a healthy anesthetized adult, the head-up<br />
tilt results in a significant reduction of cardiac output and MAP of<br />
up to 40% compared with the supine position. The heart rate and<br />
peripheral vascular resistance are slightly increased because filling<br />
pressures are reduced significantly. Echocardiographic indices of<br />
preload, as measured by left ventricular end-diastolic area, are also<br />
decreased, changing in the same direction as the pressure indices. 17<br />
This is associated with a decrease in intrathoracic and pulmonary<br />
blood volume by 14% and 17%, respectively. The decrease is<br />
probably due to a shift of blood volume toward extrathoracic<br />
compartments, especially the dependent lower limbs. The creation<br />
of a pneumoperitoneum during laparoscopic surgery on the upper<br />
abdominal viscera results in a reduction of 13% in cardiac output<br />
in anesthetized-paralyzed patients placed in a 20-degree reverse<br />
Trendelenburg position. 18 The effects of carbon dioxide (CO 2<br />
)<br />
pneumoperitoneum are a reduction in cardiac index of 3% and<br />
stroke volume of 10% and an increase in both heart rate and MAP<br />
of 7% and 16%, respectively. Head-up tilt of 20 degrees further<br />
decreased cardiac output by 11% and stroke volume by 22%<br />
whereas heart rate increased by 14% and MAP by 19%. 19 The<br />
mechanisms that result in these hemodynamic changes are com -<br />
plex and include direct mechanical effects, neurohumoral<br />
responses, and absorbed CO 2<br />
.<br />
The respiratory effects are well documented. The total com -<br />
pliance of the lungs may be reduced up to 48% due to the cephalad<br />
shift of the diaphragm caused by the insufflated gas. 20 This is<br />
without significantly altering the intrapulmonary distribution of<br />
ventilation and perfusion. 21 Although the reverse Trendelenburg<br />
position increases FRC and, presumably, compliance, oxygenation<br />
does not necessarily improve. 22 This is probably because of the<br />
reduction in cardiac output, which occurs in the head-up tilt,<br />
negating the beneficial effects of position on the distribution of<br />
ventilation. There are limited data regarding the effects of reverse<br />
Trendelenburg position in the pediatric population. One report<br />
on 25 children aged 1 to 14 years undergoing laparoscopic fundo -<br />
plication showed that 3 patients developed hypotension or<br />
bradycardia occurring before peritoneal insufflation. 23 Transient<br />
hypotension was probably related to hypovolemia. One bronchial<br />
intubation episode developed as a result of the positional change<br />
and the creation of the pneumoperitoneum.
1346 PART 4 ■ Special Monitoring and Resuscitation Techniques<br />
central nervous system pathology and essentially useless for vas -<br />
cular volume resuscitation.<br />
Physiology of the Trendelenburg Position<br />
Figure <strong>80</strong>-5. Reverse Trendelenburg position.<br />
Complications of the Head-Elevated Positions<br />
The complications associated with the head-elevated prone posi -<br />
tion or the head-elevated supine position are similar to that known<br />
to the traditional prone and supine positioning (Figure <strong>80</strong>–5).<br />
Beside the complications that might arise as a result from the<br />
physiologic changes with repositioning, ophthalmic complications<br />
from compression of the eye from a headrest is feared in the headelevated<br />
prone position. Proper strap placement at the edge of the<br />
buttocks must be used to prevent the patient from sliding down<br />
the tilted table. The strap should be positioned between the<br />
femoral head and the iliac crest to avoid compression of the<br />
vascular bundle crossing the hip joint and causing ischemic necro -<br />
sis of the femoral head, or the strap may be applied 2 inches distal<br />
to the knee. Because the head is elevated above the level of the<br />
heart, the risk of air embolism is present, although it is signifi -<br />
cantly less than that observed in the classic sitting position. Appr -<br />
opriate monitoring should be instituted. Cerebral perfusion and<br />
blood flow may decrease.<br />
TRENDELENBURG POSITION<br />
General Considerations<br />
The steep 45-degree head-down tilt surgical posture was<br />
popularized in the 1870s by Friedrich. Trendelenburg as a means<br />
of improving access to pelvic pathology as the abdominal contents<br />
shifted cephalad with gravity. The eponym “Trendelenburg” now<br />
encompasses any degree of head-down tilt, regardless of whether<br />
the patient is lying supine, lateral, or prone (Figure <strong>80</strong>–6). All<br />
head-down tilt positions are now recognized, however, as poten -<br />
tially harmful in the presence of cardiac, pulmonary, ocular, and<br />
Figure <strong>80</strong>-6. Trendelenburg position.<br />
Walter Cannon advocated the value of the Trendelenburg position<br />
in the management of cardiovascular shock during the early 1900s.<br />
The belief was that any head-down tilt increased venous return<br />
and improved cerebral blood flow. But placing the adult patient<br />
in a mild 15-degree Trendelenburg position resulted only a 1.8%<br />
displacement of the total volume centrally; this small amount is<br />
unlikely to have an important clinical effect. 24 Subsequent studies<br />
also questioned the validity of this posture in the management of<br />
shock when patients who were hypotensive had worsening of<br />
hemodynamic parameters and increased mortality when they<br />
were placed in the Trendelenburg position. 25 In healthy normo -<br />
tensive volunteers and patients, the head-down tilt resulted in an<br />
increase in the filling pressures of the heart, no change or a slight<br />
increase in the cardiac output, and no significant change in the<br />
arterial pressure as the carotid and aortic baroreceptors induced<br />
systemic vasodilatation and a slight decrease in pulse rate. 26 The<br />
increase in cardiac output, if any, results from the increase in<br />
stroke volume from the initial increase in venous return, but this<br />
effect is short-lived and disappeared within 10 minutes. 27 The<br />
cardiac output may increase or more commonly be reduced when<br />
hypotensive patients are placed in a head-down tilt. Significant<br />
decrease in the arterial pressure was observed when the cardiac<br />
varied from +52% to 14% in a group of hypotensive patients<br />
placed in a 10-degree Trendelenburg tilt. 24 No significant impro -<br />
vement in oxygen delivery or oxygen extraction ratio in hypoten -<br />
sive critically ill patients placed in the Trendelenburg position was<br />
observed. The mild increase in blood pressure is not associated<br />
with an improvement in blood flow or tissue oxygenation. 28 In<br />
nonanesthetized patients, no changes are found in cardiac output,<br />
MAP, systemic vascular resistance, and oxygenation when<br />
they were placed in 10- or 30-degree Trendelenburg position. 29<br />
Although most studies confirm that the Trendelenburg position in<br />
healthy anesthetized patients does not result in any sustained<br />
hemodynamic changes, peritoneal insufflation with CO 2<br />
results<br />
in a significant increase in systemic vascular resistance as well as<br />
a significant decrease in cardiac index and ejection fraction area<br />
compared with baseline. 17,26 The mild Trendelenburg position is<br />
often used during insertion of a central venous line, possibly by<br />
making the jugular veins less collapsible because of increased<br />
intravascular pressure. The diameter of the internal jugular vein<br />
(IJV) was shown to increase with the head-down tilt, but this<br />
maneuver was less effective when compared with the application<br />
of an abdominal binder or the use of a Valsalva maneuver. 30 A<br />
head-down tilt of more than 20 degrees does not increase crosssectional<br />
area of the IJV any further, whether or not hepatic<br />
compression is applied. Hepatic compression and positive inspira -<br />
tory pressure caused by a Valsalva maneuver effectively dilate the<br />
IJV, which facilitates venous cannulation in supine patients when<br />
the Trendelenburg position is not advisable or possible. 31 It was<br />
found that, in the pediatric age group, inguinal compression<br />
effectively increases the cross-sectional area of the femoral vein; its<br />
effect is also prominent in the Trendelenburg position. Valsalva<br />
maneuver is more effective in smaller children younger than 2<br />
years. Gravitational position changes alone have little effect on the<br />
size of the femoral vein in children. 32
CHAPTER <strong>80</strong> ■ Patient Positioning and Precautions During Anesthesia and Surgery 1347<br />
The most significant effect of the Trendelenburg position on<br />
the respiratory system is the mechanical interference with chest<br />
movement and the limitation of lung expansion. With the head<br />
and chest at a level lower than the abdomen, the weight of the<br />
abdominal viscera will impair diaphragmatic movement and<br />
reduce lung volumes. A 10-degree head-down tilt causes a 3%<br />
decrease in tidal volume, whereas a 20- or 30-degree Trendelen -<br />
burg position resulted in a 12% reduction. A significant increase<br />
in the physiologic deadspace is seen in patients placed in the 20-<br />
degree Trendelenburg position. The arterial–to–end-tidal CO 2<br />
(PaCO 2<br />
-PETCO 2<br />
) gradient is increased compared with that in the<br />
supine posture. 33 Changes of intrapulmonary gas and pulmonary<br />
blood distribution are probably responsible for the observed<br />
physiologic deadspace and CO 2<br />
gradient differences. A study of<br />
10 anesthetized-paralyzed children aged 1 to 15 years undergoing<br />
laparoscopic surgery found that head-down tilt induced a mean<br />
decrease of 17% in lung compliance, which was further decreased<br />
by 27% from the baseline during intra-abdominal CO 2<br />
insuffla -<br />
tion. There is a concomitant increase in the peak inspiratory<br />
pressure (PIP) by 19% and 32% during Trendelenburg position<br />
and peritoneal insufflation, respectively. The changes in the lung<br />
compliance and PIP returned to their respective baseline values<br />
after removal of CO 2<br />
from the peritoneal cavity and the patient<br />
was returned to the supine position. 34 Respiration should be<br />
controlled when the child is placed in the head-down tilt because<br />
the work of breathing during spontaneous breathing is expected to<br />
increase and the reduction in lung volumes will predispose the<br />
lungs to atelectasis. This is more evident in the smaller child. The<br />
main contributing forces associated with negative intrapleural<br />
pressure are generated by the diaphragmatic and abdominal<br />
muscles. The hydrostatic pressure exerted by the abdominal<br />
contents on the diaphragm will hinder the motion and result in a<br />
greater work of breathing. In addition, in the neonate and infant,<br />
the increased compliance of the chest wall lowers the resting lung<br />
volume, making the FRC more difficult to maintain. The closing<br />
volume is also much higher in neonates and infants than in adults<br />
because of the decrease in elastic tissues. A spontaneous breathing<br />
technique in an anesthetized infant produces shunting and<br />
hypoxemia because the reduction in lung volumes will result in<br />
tidal breaths that are less than the closing volumes and, hence,<br />
alveoli closure developed. Pediatric patients should have their lung<br />
ventilation controlled in the head-down position to ensure opti -<br />
mal oxygenation and gas exchange. Data collected in a retros -<br />
pective audit of members of the French Association of Paediatric<br />
Anaesthetists (ADARPEF) revealed a high PETCO 2<br />
in 37% of<br />
neonates and children younger than 4 months and hypoxemia in<br />
0.5% when lung insufflation pressure was limited to 15 mmHg. 35<br />
Pulmonary mechanics in infants change significantly during<br />
laparoscopic CO 2<br />
pneumoperitoneum. The magnitude of change<br />
correlates directly with intraperitoneal pressure. The majority of<br />
infants required at least one ventilatory intervention to restore<br />
baseline tidal volume and PETCO 2<br />
. 36 It is generally not recom -<br />
mended to exceed an intra-abdominal pressure of 6 to 10 mmHg<br />
in newborns and children less than 5 kg and an intra-abdominal<br />
pressure of 10 to 12 mmHg in infants heavier than 5 kg and older<br />
children. 36,37<br />
Cerebral perfusion may be affected as the central venous<br />
pressure (CVP) is increased because of the effects of gravity. The<br />
shift of cerebrospinal fluid cranially from the spinal canal further<br />
predisposes the patient to a raise in intracranial pressure. Healthy<br />
patients placed in a 30-degree Trendelenburg position do not<br />
experience any significant changes or only a slight decrease in the<br />
middle cerebral arterial flow despite a reduction in the cerebral<br />
perfusion pressure (CPP). This decrease in CPP is probably the<br />
result of a decrease in cardiac output and MAP with an increased<br />
in the CVP. As long as blood pressure was maintained, cerebral<br />
autoregulation was intact and cerebral oxygenation preserved. 38<br />
The increase in the IJV pressure that occurred with the head-down<br />
tilt was transient, lasting less than 10 minutes. 34 Although the<br />
slight reduction in cerebral perfusion and the transient cerebral<br />
venous pooling should not produce any adverse effect on the<br />
cerebral circulation in patients with normal cerebral autoregula -<br />
tion, patients with intracranial pathology may experienced intra -<br />
cranial hypertension. The changes in intracranial pressure (ICP)<br />
that resulted from a head-down tilt of 45 degrees in anesthetizedparalyzed<br />
rabbits were nearly 200% and immediate on adoption of<br />
the steep Trendelenburg position. 39 The presence of hypotension,<br />
inadvertent or deliberate, with the head-down tilt should be<br />
considered risky for any patient because the CPP may be lowered<br />
significantly below the autoregulation limits and result in cerebral<br />
ischemia. Any other process that increases intrathoracic pressure<br />
such as the use of overzealous ventilatory maneuvers (e.g., PEEP)<br />
will also increases cerebral venous pooling and can lead to cerebral<br />
edema.<br />
Complications of the Head-Down Tilt<br />
Regurgitation or vomiting and subsequent aspiration of gastric<br />
contents remains an important cause of morbidity and mortality<br />
in anesthesia. It is generally accepted that the integrity of the lower<br />
esophageal sphincter is the major protective mechanism against<br />
regurgitation. The tendency to regurgitate is opposed by the<br />
barrier pressure between the lower esophageal and the gastric<br />
pressures. The effects of a 15- and 30-degree head-down tilt of<br />
healthy patients under general anesthesia have been shown to<br />
increase both gastric and lower esophageal pressures so that<br />
barrier pressure did not change significantly. The use of the<br />
Trendelenburg position does not predispose to gastroesophageal<br />
regurgitation. 40 However, patients with a history of gastroeso -<br />
phageal reflux may be at higher risk for regurgitation when they<br />
are placed in the Trendelenburg position. Animal studies showed<br />
that pigs with low esophageal sphincter pressure before induction<br />
of anesthesia regurgitated when placed in the head-down tilt with<br />
a pneumoperitoneum of 15 mmHg. 41<br />
Brachial plexus injuries (0.16% incidence rate) have been<br />
reported with the use of shoulder braces when the patient’s arm<br />
was extended at 90 degree. 42 Stretching or compression of the<br />
retroclavicular neurovascular bundle is believed to be responsible<br />
for the neurologic deficits. The recommendations of the depart -<br />
ment of anesthesiology of the University of California San Diego<br />
to avoid anesthesia-related neuropathies from the Trendelenburg<br />
position are (1) steep Trendelenburg position should be avoided<br />
whenever possible, (2) shoulder restraints, when necessary, should<br />
be placed over the acromioclavicular joints bilaterally, (3) abduction<br />
of the upper extremities should be less than 90 degrees from<br />
the body, (4) the patient’s head position should remain neutral,<br />
and (5) when the arms are abducted, the shoulder restraints<br />
should be removed on the ipsilateral side. 43<br />
Leg supports used during head-down tilt plus lithotomy<br />
posture should be adequately padded to prevent pressure on the<br />
common peroneal nerve. Once the position is finalized, the<br />
position of the tracheal tube should be reconfirmed to avoid
1348 PART 4 ■ Special Monitoring and Resuscitation Techniques<br />
bronchial intubation because of the cephalad shift of the<br />
mediastinum and the upward displacement of the lungs and the<br />
carina. The risk of malposition of the tracheal tube in the pediatric<br />
patient is higher than in adults because the distance between the<br />
vocal cords and the carina is shorter. Even simple neck flexion and<br />
extension is known to result in a significant shift of the tracheal<br />
tube that could lead to bronchial intubation or inadvertent<br />
extubation. Increased CVP, intraocular pressure (IOP), and ICPs<br />
may be precipitated by steep Trendelenburg position. Clinical<br />
swelling of the face, eyelids and conjunctivae, and tongue has been<br />
observed, along with a plethoric color of venous stasis in the head<br />
and neck. Lingual and buccal nerve neuropathy can occur. In<br />
patients with substantial swelling, it may be prudent to delay<br />
removal of the endotracheal tube until that situation has improved<br />
to avoid the risks of upper airway edema. 44 There are no data<br />
demonstrating a higher incidence of unexpected neurologic events<br />
in patients placed in the steep Trendelenburg position for long<br />
operations, but there is one case report of a patient who had a<br />
cerebral hemorrhage during such a procedure and emerged with<br />
a significant neurologic deficit. 45<br />
LATERAL DECUBITUS POSITION<br />
General Considerations<br />
The lateral decubitus position is inherently unstable and support<br />
must be available to maintain the patient in this posture. As the<br />
torso is tilted slightly laterally, usually a pad is placed under the<br />
shoulder so that the head and neck can be turned without tension.<br />
Such turning of the shoulder area alone may place torque on the<br />
lower back. It may be useful to place a pad under the hip so that it<br />
can follow the tilt of the shoulder and prevent the torque on the<br />
spine. Extreme lateral neck flexion has been reported to cause<br />
transient Horner’s syndrome. 46 Stability of the patient can be<br />
maintained by the use of straps, belts, or strips of adhesive tapes.<br />
Depending on the clinical circumstances, two straps are recom -<br />
mended with the upper applied just caudad to the axilla, taking<br />
care to avoid compression of the brachial neurovascular bundle,<br />
and the lower strap placed across the hip just below the iliac crests.<br />
They must be placed in such a manner that respiratory movements<br />
of the chest are not restricted and the abdomen moves freely to<br />
minimize respiratory compromise. Maintenance of the head and<br />
neck in a neutral position relative to the torso with pillows and<br />
support is also vital to avoid stretch injuries to the brachial plexus.<br />
The downside arm is usually tucked beneath the pillow that<br />
supports the head. An axillary roll placed just caudad to the axilla<br />
minimizes compression of the dependent neurovascular struc -<br />
tures. This minimizes the risk of brachial plexus injury due to<br />
compression of the nerves between the humeral head and the<br />
thoracic cage. There is a possibility of direct compression of the<br />
brachial plexus by an axilla roll when it is placed in the axilla, and<br />
care should be taken to ensure that the roll is placed beneath the<br />
upper chest. Other methods that have been used with success<br />
include the beanbag “Vacu-Pac.” This is a moldable support filled<br />
with thousands of tiny plastic beads. Once the patient adopts the<br />
necessary operative position, a negative pressure (e.g., vacuum) is<br />
used to remove all air within the Vacu-Pac through a valve. This<br />
process forces the beads tightly and molds the bag firmly around<br />
the contours of the patient, providing a support similar to a plaster<br />
cast. This device offers considerable advantages over the straps<br />
and padded rests in the pediatric patients. It has the added<br />
advantage of a more even distribution of the body weight and<br />
reduces the risk of pressure injuries.<br />
Once the lateral decubitus position has been established, the<br />
operating table is flexed at the level of or just cephalad to the iliac<br />
crest to establish the kidney position. Care must be taken not to<br />
raise the kidney rest (i.e., point of flexion of the table) within either<br />
the flank or the lower ribs of the patient (Figure <strong>80</strong>–7). When<br />
placed correctly, little interference to the dependent lung and<br />
diaphragm is present and obstruction of the inferior vena cava is<br />
avoided. Because the legs will be in a dependent manner once the<br />
position is attained, elastic compressive stockings should be<br />
applied to minimize venous pooling. In the smaller child or infant,<br />
an appropriate-sized roll may be placed at the flexion point (Figure<br />
<strong>80</strong>–8). A modification of the lateral decubitus position is com -<br />
monly referred to as the left lateral or semiprone position. It is<br />
similar to the Sims position described by J. M. Sims in 1857. It may<br />
be used during gynecologic procedures and is commonly<br />
employed as a posture of recovery after anesthesia. The upside leg<br />
in the semiprone position is flexed at the knee and hip while the<br />
downside leg is kept extended. The body is allowed to rotate<br />
forward with gravity. The downside arm may be kept beneath the<br />
pillow supporting the head to facilitate breathing by extending the<br />
airway.<br />
Figure <strong>80</strong>-7. The kidney position<br />
with the kidney resting beneath the<br />
down-side iliac crest to minimize interference<br />
of the downside diaphragmatic<br />
motion. The kidney rest, a<br />
transverse elevating bar of the table,<br />
is raised to increase the separation of<br />
the iliac crest from the lateral costal<br />
margin.
CHAPTER <strong>80</strong> ■ Patient Positioning and Precautions During Anesthesia and Surgery 1349<br />
A<br />
Figure <strong>80</strong>-8. A: Lateral decubitus in an infant with an axillary roll. B: Lateral decubitus in an infant with an axillary rolls.<br />
B<br />
Physiology of the Lateral Decubitus Position<br />
It was demonstrated that the upper airway of sedated, sponta -<br />
neously breathing children widens significantly in the lateral<br />
position compared with the supine position. This widening occur -<br />
red at all noncartilaginous areas of the upper airway and was most<br />
pronounced in the region at and below the tip of the epiglottis.<br />
The empirical findings confirm the widespread clinical experience<br />
that sedated children experience less upper airway obstruction in<br />
the lateral position than in the supine position. 47 A retrospective<br />
study of the hemodynamic and respiratory effect of pediatric<br />
urologic laparoscopic surgery 48 and another prospective study of<br />
the hemodynamic and respiratory effects of pediatric urologic<br />
retroperitoneal laparoscopic surgery 49 described the significant<br />
cardiopulmonary changes in children that were associated and<br />
occurred in relation to the CO2 insufflation in both retroperito -<br />
neal and transperitoneal approaches. The lateral position is well<br />
tolerated by most patients with minimal effects on the body. Few<br />
studies described the hemodynamic effects of postural changes<br />
from the supine to the lateral position. Changes will be more<br />
evident in exaggerated lateral positions with the kidney rest<br />
positions in which venous pooling in the dependent limbs is more<br />
significant. Venous return may also be reduced owing to kinking<br />
of the inferior vena cava. The proximity of the inferior vena cava<br />
to the right flank may allow compression by the kidney rest. It may<br />
result in a greater decrease in blood pressure than the left lateral<br />
position. Echocardiographic studies documented increases in<br />
right ventricular end-diastolic diameters in the left dependent<br />
position and shortened diameters in the right dependent position.<br />
The better preload and cardiac function in the left decubitus<br />
position is supported by the significantly increased in atrial<br />
natriuretic peptide levels compared with the supine. The right<br />
ventricular end-diastolic volume decreased by almost 10% in the<br />
right decubitus position and was associated with decreased atrial<br />
natriuretic peptide levels even though cardiac indices were<br />
unchanged.<br />
Like all other postures, postural-related mechanical restriction<br />
of chest movement limits lung expansion and results in reduction<br />
of lung volumes. In healthy conscious subjects, the vital capacity<br />
in the lateral position is decreased by 10% when compared with<br />
the sitting position. A greater reduction is seen with the use of the<br />
kidney position in which the truncal flexion can produce up to<br />
15% reduction in vital capacity. The reduction is due to the<br />
restriction of the thoracic cage movements and impairment of the<br />
ipsilateral hemidiaphragmatic motion. The tidal volume can be<br />
reduced up to 14%. In conscious adult subjects, a decrease of<br />
almost 16% in the FRC was observed when the subjects were<br />
placed in the lateral position from the sitting posture. This reduc -<br />
tion is almost of the same magnitude as in the prone position but<br />
is less than the decrease in FRC in the supine position (28%).<br />
Radiographic studies showed that the dependent lung is subjected<br />
to the compressive effects of the cranial shift of the lower<br />
hemidiaphragm whereas the nondependent diaphragm may not<br />
move cephalad at all. The smaller reduction in FRC may be due to<br />
the change in position of only one diaphragm (dependent lung). 3<br />
Similar changes were seen in the pediatric population. The FRC in<br />
supine anesthetized mechanically ventilated children was about<br />
60% of predicted awake value and increased by 19% when the<br />
child was turned to the right lateral decubitus posture. 50 In a group<br />
of anesthetized adult patients receiving mechanical ventilation in<br />
the lateral position, 34% of ventilation was distributed to the<br />
dependent and 66% to the nondependent lung. 51 The dynamic<br />
lung compliance and deadspace are lower and lung resistance is<br />
higher in the dependent versus the nondependent lung. Total lung<br />
dynamic compliance is, however, reduced, and the reduction<br />
occurred whether respiration was controlled or spontaneous. 52<br />
The decrease is progressive and probably due to the formation of<br />
atelectasis in the dependent lung and overdistention of the<br />
nondependent lung. Unlike in adults, ventilation is preferentially<br />
distributed to the uppermost lung in the lateral position in infants<br />
and young children—a reversal of the adult pattern. 53 The pattern<br />
of regional ventilation in children was examined using krypton-<br />
81m radionuclide ventilation lung scans in the supine, right, and<br />
left decubitus postures in 43 children aged 2 to 10 years. 54 The<br />
mean fractional ventilation to the right lung was 46% in the supine<br />
position, and this fell to 36% when dependent and rose to 56% in<br />
the nondependent position. Redistribution of ventilation away<br />
from the dependent toward the uppermost lung was seen in all<br />
children. In children aged 10 to 18 years, the mean fractional<br />
ventilation to the right lung was 57% (supine), 48% (dependent),<br />
and 63% (nondependent). These changes could be due to the<br />
difference in pleural pressure, which is closer to atmospheric
1350 PART 4 ■ Special Monitoring and Resuscitation Techniques<br />
pressure in the infant, predisposing to closure of peripheral air -<br />
ways in the dependent regions of the lungs, because such ven -<br />
tilation is distributed toward the nondependent lung. In addition,<br />
there is likely to be less difference in contractility between depen -<br />
dent and nondependent hemidiaphragms in the young because<br />
the abdomen is narrower. Hence, because the abdominal-related<br />
preload is similar, there is less discrepancy in the fractional<br />
ventilation between the lungs.<br />
Complications Associated With the<br />
Lateral Decubitus Position<br />
Care must be taken to ensure that the down ear is positioned<br />
properly to avoid prolonged compression and pressure necrosis.<br />
The downside eye is at risk of compression and retinal artery<br />
thrombosis if positioned against an improperly placed headrest.<br />
Proper soft padding and great attention should be used to prevent<br />
this injury to the downside eye, ear, and facial nerve. The skin<br />
overlying the bony prominences of the lower limbs, especially<br />
on the downside leg, is at risk from pressure necrosis during<br />
pro longed positioning. Adequate padding should be provided<br />
underneath the patient and between the legs. The head and neck<br />
should be adequately elevated on a support in the neutral position<br />
to avoid stress and strain of the muscles that may result in<br />
postoperative neckache. Significant displacement of the tracheal<br />
tube caused by flexion and extension of the neck was shown using<br />
fiberoptic bronchoscopy in children between the ages of 16 and<br />
19 months. The tip of the tube moved a mean distance of 0.9 cm<br />
toward the carina with neck flexion and 1.7 cm toward the vocal<br />
cords with extension. Bronchial intubation and accidental extuba -<br />
tion could occur after significant changes of the head position in<br />
small children. 55 The same effect was observed with a nasally<br />
placed tracheal tube. 56 Unlike most surgical positions in which<br />
stretch injuries account for the majority of damage to the brachial<br />
plexus, compression is the principal cause of positional nerve<br />
injuries in the lateral position. This may occur when the lower<br />
shoulder and arm lie under the chest and compress the axilla in the<br />
lateral position without the use of an axilla roll. Conversely, an<br />
improperly placed roll may compress the axilla. A cervical rib may<br />
also predispose the brachial plexus to compression injury.<br />
Excessive stretching may lead to brachial plexus injury of the<br />
upside arm when there is excessive lateral flexion of the neck. This<br />
occurs more often because of postural instability secondary to<br />
surgical manipulations during the procedure.<br />
The suprascapular nerve may be stretched circumduction of<br />
the arm across the chest when the laterally placed patient is shifted<br />
to the semisupine position. This same injury to the nerve of lower<br />
arm occurs when the laterally placed patient shifts to the<br />
semiprone position and traps the arm beneath the chest. The long<br />
thoracic nerve may be injured when the head and neck of the<br />
patient are laterally flexed from the upper shoulder. The common<br />
peroneal nerve is one of the most frequent nerve injuries in<br />
patients placed in the lateral position. Compression of the nerve at<br />
the tip of the fibula happens when the patient is positioned with<br />
inadequate padding between the side of the leg and the operating<br />
table. The lower sciatic nerve may be compressed between the<br />
operating table and the ischiopubic ramus, whereas the upper<br />
sciatic nerve may be compressed by the retaining straps placed<br />
across the hips.<br />
When switching from two-lung to one-lung ventilation (OLV)<br />
during surgical thoracotomy, shunt fraction increases, oxygena -<br />
tion is impaired, and hypoxemia may occur. Hypoxemia during<br />
OLV may be predicted from measurements of lung function,<br />
distribution of perfusion between the lungs, whether the right or<br />
the left lung is ventilated, and whether the operation will be<br />
performed in the supine or the lateral decubitus position. Hypo -<br />
xemia during OLV may be prevented by applying a ventila tion<br />
strategy that limits alveolar collapse while minimally affecting<br />
perfusion of the dependent lung. The choice of anesthesia does<br />
not influence oxygenation during clinical OLV. Hypoxemia during<br />
OLV may be treated symptomatically by increasing inspired<br />
fraction of inspired oxygen, changing ventilation parameters, or<br />
using continuous positive airway pressure in the nonventilated<br />
lung. Hypoxemia during OLV may be treated causally by correct -<br />
ing the position of the double-lumen tube, clearing the main<br />
bronchi of the ventilated lung from secretions, and improving the<br />
ventilation strategy. 57 The lateral decubitus position has been<br />
reported to be associated with myonecrosis and sciatic nerve palsy<br />
but not compartment syndrome. 58<br />
PRONE POSITION<br />
General Considerations and Variations<br />
There are a number of variations of the prone position (Figure<br />
<strong>80</strong>–9). They include the horizontal prone, the head-elevated prone<br />
(Concorde position), the sea lion prone, the thoracic prone, the<br />
prone jack-knife, and the seated prone. The common element is a<br />
facedown patient with supports placed beneath the shoulders and<br />
the iliac crests, allowing freedom of abdominal movement and<br />
chest expansion. Since the 1950s, various methods of supporting<br />
the patient in the prone position have been described to reduce<br />
compression of the abdomen and enhanced respiratory function<br />
and cardiovascular stability. A great number of frames have been<br />
designed and an assortment of supportive devices and equipment<br />
has been used for protection of the head and relief of ventral<br />
abdominal pressure. The head is usually placed in a headrest or<br />
turned on the side while resting on a pillow. A padded foam or<br />
jelly donut shape can be used to protect the ear and the eye.<br />
Most often in pediatric anesthesia, surgical sheets rolled tightly<br />
to form a wrinkle-free cylinder is a simple and inexpensive<br />
Figure <strong>80</strong>-9. Patient in the prone position shows the placement<br />
of rolls underneath the pelvis and the chest that allow proper<br />
abdominal expansion during mechanical ventilation. The head<br />
is turned on the side and leveled to maintain the cervical spine<br />
in line with the back. The eye and nose are padded to prevent<br />
injury, and the airway equipment is visible at all time and easily<br />
accessible. The feet are protected using a roll underneath the<br />
ankles.
CHAPTER <strong>80</strong> ■ Patient Positioning and Precautions During Anesthesia and Surgery 1351<br />
90 degrees and the weight is borne on knees, and the pelvis is<br />
supported under iliac crests and pillows under chest. The arms are<br />
abducted above head and the head is turned to the side. The tight<br />
paraspinal muscles in the Georgia prone position can limit the<br />
lateral access to the spine. The Buie position is similar to the<br />
Georgia prone, but involves a head-down tilt and is useful for<br />
anorectal surgery. A hypobaric spinal block is possible. The Ray<br />
frame assumes a similar position but with more even weight<br />
distribution on the knees and the arms adducted across the chest.<br />
The seated prone position is also known to the knee-chest position.<br />
It has the advantage that the weight is borne on the ischeal tubero -<br />
sities and not the knees. 59<br />
Figure <strong>80</strong>-10. The Wilson frame for spine surgery. Note the<br />
position of the pelvic and chest bolsters allowing complete<br />
clearance of the abdomen and proper mechanical ventilation.<br />
It is very important to ensure that all pressure points are wellpadded<br />
(see elbow).<br />
method of providing support for the torso, lifting the abdomen<br />
free from the surface of the operating table, and stabilizing the<br />
patient. For larger patients and/or specific surgical procedures, the<br />
Wilson, Relton-Hall, and Andrew frames can be used. The Wilson<br />
frame consists of parallel convex padded arches that allow a<br />
variable degree of adjustable curvature and is used to minimize<br />
the patient’s lumbar lordosis during spinal operations (Figure<br />
<strong>80</strong>–10). This frame supports both the iliac crests and the chest but<br />
is more suitable for adults or larger children undergoing lumbar or<br />
thoracic spinal procedures. The main advantages of this frame are<br />
that the abdomen and lower chest are unrestricted and that good<br />
surgical access to the intervertebral space may be achieved by<br />
adjusting the width and height of the frame. The Relton-Hall<br />
frame consists of four pedestals that could be adjusted to the<br />
dimensions of the patient. The padded pedestals support the<br />
patient just below the axilla on the anterolateral chest wall and at<br />
the anterior iliac spines (Figure <strong>80</strong>–11). Although the chest and<br />
abdomen move freely, the whole weight of the torso is supported<br />
only at these four points and may result in the development of<br />
pressure sores, especially if the pedestals are inadequately padded.<br />
Finally, the Andrew frame is a kneeling system in which the weight<br />
of the patient is maintained on a chest support and on the knees.<br />
In this widely used version, longitudinal padded rolls support the<br />
torso with the chest resting on a chest pad. The hips are flexed at<br />
right angles and the knees rest on a kneeling pad. A gluteal pad<br />
helps to retain the flexion posture.<br />
Other variations include the Georgia position, in which<br />
the patient is kneeling on a shelf, her or his hips are flexed at<br />
Preanesthetic Evaluation<br />
If the prone position is required, a history of neck injury, cervical<br />
arthritis, or previous operations on the cervical spine should be<br />
documented and the range of movement of the head and neck<br />
assessed. Certain pediatric syndromes (e.g., Down and Morquio-<br />
Brailsford syndromes) are associated with cervical spine ano -<br />
malies, and such patients are at risk of cervical spinal cord injury.<br />
Stability of the cervical spine should be assessed and deficits<br />
documented in the preoperative assessment. The presence of a<br />
cervical rib should be excluded, because this will predispose to<br />
brachial plexus injury if the arms are to be abducted during<br />
surgery. The presence of obesity should be noted, because chest<br />
size may impose a shifting base, preventing a stable posture, and<br />
may also cause abdominal compression, so alternative frame<br />
devices that minimize abdominal pressure may be used or a<br />
variation of the prone position be employed. All limb movement<br />
should be tested. The elbows, arms, and legs must be able to flex<br />
and the arms must be lifted above the head without resulting in<br />
any injury.<br />
Physiology of the Prone Position<br />
Under normal circumstances in the awake state, diaphragmatic<br />
excursion increases intra-abdominal pressure while decreasing<br />
intrathoracic pressure. This pressure gradient facilitates venous<br />
return to the heart. Limitation of the diaphragmatic motion or<br />
institution of intermittent positive-pressure ventilation hinders<br />
venous return and, consequently, affects the cardiac output. Dimi -<br />
nished venous return may also occur with compression of the<br />
inferior vena cava and femoral veins by improperly placed sup -<br />
ports or via the effects of gravity. When they are compressed or<br />
the abdominal expansion is limited, the blood flow from the distal<br />
part of the body will be diverted into the perivertebral venous<br />
Figure <strong>80</strong>-11. The Relton-Hall frame is<br />
an adjustable four-pedestal bolsters that<br />
allow control of the degree of lumbar<br />
lordosis by the varying the position of<br />
the pedestals.
1352 PART 4 ■ Special Monitoring and Resuscitation Techniques<br />
plexuses (i.e., Batson’s veins). These are valveless and represent a<br />
very low pressure system. This may result in engorgement of the<br />
vertebral venous plexus during spinal surgery, contributing to<br />
increased blood loss. The correlation between the types of prone<br />
support and the inferior vena caval pressure was discussed. 60 A<br />
significant reduction of almost 50% in the mean inferior vena<br />
caval pressure was seen when the patient was positioned on a<br />
Relton-Hall frame compared with the prone position on a<br />
conventional pad. The association between an elevated CVP and<br />
an increased intraoperative blood loss was studied; however, the<br />
authors did not find any evidence to support the hypothesis that<br />
CVP is useful in determining the ideal prone position in patients<br />
undergoing lumbar laminectomy. 61 Patients undergoing halothane<br />
anesthesia and muscle paralysis positioned in a flat prone position<br />
did not show any significant changes in hemodynamic variables.<br />
However, the elevation of the frame led to a significant reduction<br />
in cardiac output (20%) and stroke volume with increases in<br />
peripheral vascular resistance. The decrease in cardiac output is<br />
believed to be secondary to the reduced venous return. 62 A study<br />
on the cardiovascular effects of four other different prone<br />
positions (patient on pillows, evacuatable mattress, Relton-Hall<br />
props, knee-chest/seated prone) found that the use of pillows (one<br />
underneath the thorax and another under the pelvis) resulted in<br />
less impairment than when the volunteers were prone in either the<br />
knee-chest position or in the Relton-Hall frame. 63 It has been<br />
suggested that the decrease in cardiac index could be attributed<br />
to increased intrathoracic pressures causing a decrease in arterial<br />
filling, leading to an increase in sympathetic activity via the baro -<br />
ceptor reflex. Consistent with this theory is the work that demon -<br />
strated decreased stroke volume accompanied by an increased<br />
sympathetic activity (increased heart rate, total peripheral vascular<br />
resistance, and plasma noradrenaline) in prone patients. Another<br />
study has suggested that, in addition to reduced venous return,<br />
left ventricular compliance may also decrease secondary to in -<br />
creased intrathoracic pressure that could contribute to the<br />
observed decrease in cardiac output. 64<br />
Recent investigations suggest that the anesthetic technique<br />
could affect hemodynamic variables in the prone position. 64-65 One<br />
study compared total intravenous anesthesia (TIVA) with<br />
inhalation anesthesia by measuring MAP and heart rate in patients<br />
undergoing spinal surgery. A greater decrease in arterial pressure<br />
in the TIVA group was observed. 64 The other study comparing<br />
inhalation anesthesia to TIVA for the maintenance of anesthesia<br />
used noninvasive cardiac output measures with the patients supine<br />
and then prone on a Montreal mattress. The authors found a<br />
decrease in cardiac index and increase in systemic vascular resis -<br />
tance on turning the patient prone. 65 The changes were greater<br />
during TIVA (decrease in cardiac index of 25.9%) than during<br />
inhalation anesthesia (12.9%). However, a contributor to these<br />
observations could be a change in propofol pharmacokinetics in<br />
the prone position. Measured propofol concentrations have been<br />
observed to increase during target-controlled infusions when<br />
patients are transferred from supine to prone, probably as a result<br />
of the decrease in cardiac output. 65<br />
Interference with rib cage and diaphragmatic movements may<br />
account for the reduction in vital capacity and tidal volume when<br />
patients are placed prone. Compared with the sitting position, the<br />
FRC in the prone position is reduced by 10%. Similar to the awake<br />
state, the reduction of the FRC in anesthetized-paralyzed patients<br />
in the prone position is of a smaller magnitude than that seen in<br />
the supine position. 66 Pulmonary airway resistance increased and<br />
compliance decreased in awake subjects when they were changed<br />
from sitting to the prone position. 67 Although pulmonary shunting<br />
was unchanged in anesthetized patients placed in the prone<br />
position compared with baseline awake values, 68 an increased<br />
gradient in the PaCO 2<br />
-PETCO 2<br />
gradient was observed. 69 A number<br />
of studies have shown that prone positioning improves arterial<br />
oxygenation. This improvement in oxygenation is well docu -<br />
mented in both adult and pediatric patients with acute respiratory<br />
diseases 70–72 as well as in patients receiving general anesthesia in<br />
the prone position. Several mechanisms have been proposed to<br />
explain this phenomenon and include an increase in lung volume<br />
(such as FRC) and an improvement in V˙/Q˙ matching. The latter<br />
can result from redistribution of perfusion to better-ventilated<br />
alveoli units or redistribution of ventilation to better-perfused<br />
capillaries. An increase in regional lung ventilation by recruitment<br />
of previously collapsed lung units with unchanged perfusion may<br />
also led to the improved oxygenation. An improvement in the V˙/Q˙<br />
relationship with increases in ventilation, and a nongravitational<br />
distribution of perfusion to the nondependent lung regions in the<br />
prone position may also explain the improvement in oxygena -<br />
tion. 73,74 The latter is postulated to be related to regional differences<br />
in pulmonary vascular resistance (PVR) and not due solely to<br />
gravity. There is some evidence that PVR is intrinsically lower in<br />
the dorsal lung regions such that a more uniform distribution of<br />
blood is expected in the prone position. 75 Data on pulmonary<br />
mechanics in the pediatric patients placed in the prone position<br />
during anesthesia are still lacking. Using the inert gas argon<br />
rebreathing method adapted for neonates to measure FRC, no<br />
difference in FRC was observed in nonanesthetized babies studied<br />
in either the prone, the supine, or the right decubitus position. 76<br />
The effects of prone position in pulmonary mechanics in spon -<br />
taneously breathing healthy preterm infants aged almost 32 weeks’<br />
gestational age were studied and showed that respiratory rate, tidal<br />
volume, minute ventilation, pulmonary resistance, or dynamic<br />
compliance was similar between supine and prone positions. 77<br />
Position-dependent cerebral ischemia may result from flow<br />
impairment in the large neck vessels (carotid and vertebral<br />
arteries) on marked movements of head and neck. In infants,<br />
extreme extension or rotation of the head, which may occur in the<br />
prone-sleeping position, can occlude one or both vertebral arteries<br />
and may be an important risk factor in some cases of sudden<br />
unexpected infant deaths. Rotation of the head is not uncommon<br />
when positioning the patient in the prone position and may<br />
predispose the brainstem to ischemia if the vertebral arteries are<br />
occluded. The risk of position-dependent cerebral hypoxemia was<br />
greatest with rotation of the neck and dorsal flexion of the head.<br />
No vertebral artery compression was demonstrated in the necks<br />
held in the neutral position. 78 The lag in available blood flow from<br />
small communicating and asymmetrical vertebral arteries may<br />
predispose the infant brainstem to ischemia if one or both ver -<br />
tebral arteries are occluded by head rotation or extension. 79 A<br />
patient with unrecognized carotid stenosis who suffered a fatal<br />
stroke after spine surgery positioned prone with the head rotated<br />
has been reported. <strong>80</strong> Occlusion of the vertebral arteries has been<br />
reported in at least four cases. In one, an underlying asymptomatic<br />
stenosis of the distal right vertebral artery led to hypoperfusion in<br />
those areas of the brain supplied after rotation or extension of the<br />
neck. 81 The patient developed a lateral medullary syndrome im -<br />
mediately after surgery but, with anticoagulation and rehabili -<br />
tation, made a good recovery. The other three case reports<br />
in volved patients with apparently normal vascular anatomy.
CHAPTER <strong>80</strong> ■ Patient Positioning and Precautions During Anesthesia and Surgery 1353<br />
Complications of Prone Positioning<br />
Many injuries can occur when the patient is turned into the prone<br />
position. A survey of the process of transferring patients to and<br />
from the operating table showed that all anesthesiologists ques -<br />
tioned had no relevant training with regards to the transfer of<br />
patients. It was also reported that most transfers were undertaken<br />
by two staff alone. Injuries resulting from manual handling are<br />
common and operating theater staff should receive appropriate<br />
training. 82 The airway must be secured before positioning.<br />
Unintentional tracheal extubation while a patient is turned from<br />
supine to prone is a true risk. Monitoring cables as well as infusion<br />
lines should be placed so they do not become entangled upon<br />
turning the patient. Usually, disconnection is most convenient and<br />
may help to avoid severe complications. Intravascular access such<br />
as invasive arterial and central venous lines should be handled<br />
with great precaution before and during turning to prevent<br />
accidental dislodgment. The arms of the patients should be placed<br />
alongside the body during positioning, left in this position or<br />
abducted for the final positioning. The majority of skin contacts,<br />
the knees, iliac crests, elbows, can be at risk for pressure necrosis<br />
if the patient is left in this posture for long periods. A pillow or<br />
soft padding may be placed under these areas. Special attention to<br />
female breasts and particularly the nipples is necessary to prevent<br />
compressive necrosis and pain in the postoperative period. The<br />
eyes should be firmly taped after instillation of saline or an oph -<br />
thalmic lubricant to prevent corneal abrasions. Corneal abrasion<br />
presents immediately after emergence from anesthesia with severe<br />
pain in the eye. Conjunctival and periorbital injuries are frequent<br />
complications of the dependent eye. Other ophthalmic injuries are<br />
fortunately rare. They may be evident immediately after the<br />
surgery or occur several days after. 83 Retinal ischemia leading to<br />
blindness cannot be underestimated and is a potential complica -<br />
tion. The most common reported cause of postoperative visual<br />
loss is ischemic optic neuropathy (ION). 84 It is usually associated<br />
with hypotension and anemia. Fat or air embolism is a potential<br />
etiologic factor. In the older population, arteriosclerotic risk<br />
factors such as hypertension, diabetes, and smoking are important<br />
risk factors. 85 The perfusion pressure of the optic nerve head is<br />
determined by the difference between the perfusion pressure of<br />
the posterior ciliary artery and the IOP. Factors that decrease the<br />
posterior ciliary arterial pressure such as prolonged systemic<br />
hypotension or an increase in the IOP will decrease perfusion<br />
pressure and increase the risk of ION. A prolonged prone position<br />
with the head in a dependent, down-tilt position can be associated<br />
with a decrease in venous return leading to an elevation in local<br />
capillary bed stasis. As a result of increased CVP or venous<br />
obstruction, the IOP is raised with a corresponding decrease in<br />
choroidal blood flow, which leads to ION. 86 An appropriate<br />
headrest may minimize the risk of ocular complications. The<br />
weight of the head should be supported by the bony parts of the<br />
face and ear (i.e., forehead and zygomatic arches). Special attention<br />
should be provided to the position of the eyes and the nose of the<br />
patient. They should be positioned within the concavity of the<br />
frame or bolster. The head should be in the neutral position as<br />
much as possible to avoid rotation of the neck and potential<br />
vascular compression. Most important, whatever head and face<br />
support is chosen, repeated and careful inspection of the patient’s<br />
face should be done throughout the operative period to avoid this<br />
serious complication. Weight-bearing directly onto the face or<br />
forehead can hyperextend the neck and cause myofascial pain in<br />
the postoperative period. Macroglossia is a rare and unusual<br />
complication that has been described after posterior fossa surgery<br />
in the prone position. 87 It is probably the result of vascular<br />
congestion due to extreme flexion of the neck. Nerve injuries in<br />
pediatric patients represent 1% of all pediatric claims. 88 Peripheral<br />
nerve injury account for 16% of all claims in anesthesia. 11 Entrain -<br />
ment of air into the cranial cavity is common after neurosurgical<br />
procedures and occurs in all operative positions. There is a single<br />
case report of quadriplegia as a result of pneumorrhachis (air<br />
entrainment into the spinal canal) after posterior fossa explora -<br />
tion. 89 This was assumed to have resulted from a head-down<br />
position, allowing entrapped air in the posterior fossa to pass<br />
through the foramen magnum. Supportive treatment led to com -<br />
plete resolution of the symptoms. Excessive neck flexion in a<br />
patient undergoing an 8.5-h operation in the prone position with<br />
the neck flexed and the chin approximately one finger-breadth<br />
from the sternum resulted in complete and permanent C5–6<br />
sensory and motor deficit level after operation. This was presumed<br />
to result from overstretching of the cervical cord in a narrow spinal<br />
canal and a bulging C5–6 disk, with consequent ischemia. 90<br />
Although rare, space-occupying lesions within the spinal canal<br />
or cranial cavity can become symptomatic as a result of prone<br />
positioning, including spinal arachnoid cysts, 91 spinal metastases,<br />
and frontal lobe tumors. In each case, the mechanism involved was<br />
uncertain but the temporal relationship to the prone position<br />
strongly implicates it. Altered cerebrospinal flow dynamics and<br />
epidural venous engorgement could have been responsible. A<br />
patient with neurofibromatosis has also been described in whom an<br />
undiagnosed pedunculated neurofibroma in the posterior fossa fell<br />
anteriorly when prone, compressing the medulla and pons and<br />
leading to a bradycardia and fatal neurogenic pulmonary edema. 92,93<br />
Other less frequent complications include direct pressure<br />
necrosis of the skin in areas of iliac crest, chin, eyelids, nose, malar<br />
region, and tongue. 59 Contact dermatitis of the face from a head<br />
prone position and from the electrodes of a bispectral index on<br />
the forehead has also been reported. 94,95 Tracheal compression<br />
have been reported in a few cases due to reduced anteroposterior<br />
diameter of the chest and compression of the trachea between the<br />
sternum and the spine. This occurred in patients with thoracic<br />
scoliosis and was exacerbated by connective tissue defect of the<br />
trachea because of either Marfan syndrome or tracheomalacia. 96,97<br />
Submandibular gland swelling is also a reported complication<br />
most probably due to stretch of the salivary duct or venous stasis. 98<br />
Anterior shoulder dislocation when the arms are abducted at 90<br />
degrees at the shoulder in prone position has also been reported. 99<br />
The chest is usually large enough and strong to allow the<br />
patient’s weight to rest on it; however, in the presence of chest wall<br />
congenital deformities or after cardiothoracic surgery, reduction of<br />
the anteroposterior diameter of the chest can occur, leading to loss<br />
of the cardiac output probably due to compression of the heart<br />
and major vessels. 100 This can even be more pronounced in pectus<br />
excavatum. Two cases reported severe hypotension in prone posi -<br />
tion due to compression of the right ventricle against an abnormal<br />
sternum. 101,102 Another case report documented the compression<br />
of a Rastelli conduit in a patient with Fallot’s tetralogy during<br />
surgical manipulation of the spine. 103<br />
Abdominal organ compression may lead to hepatic ischemia,<br />
infarction, progressive metabolic acidosis, and elevated liver enzy -<br />
mes. 102,104 Pancreatitis is a known complication of spine sur gery<br />
related to systemic factors such as blood loss, hypotension, drug<br />
effect, or the use of CellSavers, as well as to prone posi tioning. 105
1354 PART 4 ■ Special Monitoring and Resuscitation Techniques<br />
Limb compartmental syndrome and rhabdomyolysis were<br />
reported in the knee-chest position and other variations of the<br />
prone position involving flexion of the knees and hip joints,<br />
ranging from biochemical muscle damage evidenced by elevated<br />
plasma creatine phosphokinase to myoglobinemia and myoglo -<br />
binuria up to acute renal failure. Some patients required fascioto -<br />
mies. Care should be taken to avoid obstruction to blood flow in<br />
the lower limbs, which may lead to these ischemic complications. 59<br />
Venous gas embolism may occur owing to abdominal compres -<br />
sion of the inferior vena cava rendering a negative pressure<br />
gradient between the right atrium and the veins in the operative<br />
site. There is a variability in the sensitivity of the different detec -<br />
tion methods, and there is no formal evidence to support the<br />
insertion of a multiorificed central venous catheter as a means of<br />
aspiration of air emboli. 106,107 Fat embolism has also been reported<br />
during spinal surgeries.<br />
Prone Positioning and Resuscitation<br />
There are several reports for the management of cardiac arrest in<br />
the prone positioning. Conventional teaching has been that, in the<br />
event of the occurrence of life-threatening effects, the patient<br />
should be turned to the supine position; this has the advantages in<br />
terms of accessibility of the airway and pericordium and familia -<br />
rity. This necessitates the routine presence of a stretcher and the<br />
operating room table, so that the patient can be returned supine in<br />
case of problems during positioning. However, this may not be the<br />
case in some situations when there are bulky surgical instruments<br />
protruding from the back of the patient. Several techniques have<br />
been described in these situations. Chest compressions have been<br />
delivered successfully with the hands on the central upper back,<br />
between the scapulae. In some patients, it has been found neces -<br />
sary to provide counterpressure between the chest and the<br />
operating table to effectively compress the thoracic cage. Both onehanded<br />
and two-handed maneuvers have been described, as have<br />
a variety of hand positions to avoid open operative sites. 108 In one<br />
patient with an unstable spine, internal cardiac massage was<br />
undertaken via a left thoracotomy incision. 109 A “postcordial<br />
thump” delivered between the shoulder blades to treat pulseless<br />
ventricular tachycardia has also been described. 110 Defibrillation<br />
has been successfully undertaken using the anteroposterior paddle<br />
position 111 or paddle orientation on left and right sides of the<br />
back. 112 However, the use of posterior paddle positions may not<br />
deliver energy to sufficient myocardium, owing to anterior dis -<br />
placement of the heart in the prone position and also increased<br />
transthoracic impedance with positive-pressure ventilation. 113 The<br />
authors recommend the use of biphasic shocks and anterior<br />
paddle or pad positioning. It has also been recommended that selfadhesive<br />
pads be placed before prone positioning of the high-risk<br />
patient. 109 Rarely, the prone position may even benefit the patient<br />
needing resuscitation in which mediastinal masses compress the<br />
trachea or obstruct cardiac filling in the supine position. 114<br />
LITHOTOMY POSITION<br />
General Considerations<br />
Lithotomy, for extraction of a bladder stone, was a common pro -<br />
cedure in the 16th century. This was performed with the patient<br />
sitting upright, legs abducted and flexed at the knees and res -<br />
trained by attendants. This seated posture is known as the “litho -<br />
A<br />
B<br />
Figure <strong>80</strong>-12. A: Lithotomy position in a child using stirrups.<br />
B: Lithotomy position in a child using a “ring circle” mounted<br />
frame.<br />
tomy” position. In more recent times, however, the lithotomy<br />
position describes a patient in a supine position with the legs<br />
elevated and the knees flexed and held in position by supports<br />
(Figure <strong>80</strong>–12). Several types of lithotomy positions are in use,<br />
and they differ mainly in the degree of leg elevation, the amount<br />
of abduction of the thighs, and the use of a head-down tilt. For<br />
the traditional lithotomy position, considerations in the pediatric<br />
population are similar to those of adult patients. The foot section<br />
of the operating table is usually removed and the leg holders are<br />
securely fixed to both sides of the table. As the patient is moved<br />
toward the end of the table to adopt the lithotomy position after<br />
induction of anesthesia, an adequate length of anesthetic breathing<br />
circuit and monitoring cables should be available. The hips of the<br />
patient should be positioned adjacent to the lithotomy supports<br />
and the legs abducted, knees flexed, and elevated to the degree<br />
appropriate for the surgical procedure. The arms of the patients<br />
should be flexed across the chest, or more commonly in the larger<br />
patient, supported by lateral armboards by the side of the operat -<br />
ing table. A sacral support with a wedge of a roll may be used to<br />
improve exposure of the perineum.<br />
In the pediatric patient, the final position will be determined<br />
by the type of leg support available. The availability of appr -<br />
opriately sized leg holders usually decides how the legs are being<br />
held up. Regardless of the type used, the legs must rest in a neutral<br />
position without strain or pressure on any joint. For the very young<br />
child, none of the conventional leg holders may be suitable and<br />
im provised supports such as sheet rolls may be used to hold the<br />
legs up. For the bigger child, a variety of leg holders for the<br />
lithotomy position is available. Each is connected to the pole that<br />
has been clamped to the side of the table. The legs are either held<br />
up by the ankles (“candy cane” pole, foot boot) or supported at the
CHAPTER <strong>80</strong> ■ Patient Positioning and Precautions During Anesthesia and Surgery 1355<br />
popliteal fossa (“knee crutch”) or at the calf (“calf support”). The<br />
stirrups must be positioned according to the height, weight, and<br />
age of the patient and the estimate of knee-to-ankle and thigh<br />
lengths. One must note that the use of a leg support that leads to<br />
compression of the calves may predispose the patient to the<br />
development of compartment syndrome, especially if the patient<br />
is retained in the lithotomy position for a prolonged period.<br />
Although no particular type (skids, stirrups, boots) is exempted<br />
from the development of this complication, the use of stirrups is<br />
recommended because the support pressure is concentrated at the<br />
heel. Circumferential bindings to secure the legs in place or<br />
wrappings to prevent venous blood pooling are potentially harmful<br />
and are never recommended.<br />
Physiology of the Lithotomy Position<br />
Elevation of the legs increases venous return to the heart and<br />
activates baroreceptors to accommodate the volume shift via<br />
vasodilatation. There is a transient increase in the filling pressures<br />
of the heart, cardiac output, and cerebral arterial flow. Normal<br />
cardiovascular compensatory mechanisms tend to return the<br />
hemodynamic parameters to normal levels rapidly in healthy<br />
patients. The lithotomy position is known to decrease lower limb<br />
blood flow. There is a significant reduction in lower leg perfusion<br />
from 103 mmHg to 21 mmHg after 25 minutes in the lithotomy<br />
position. It is associated with a reduction in medial gastrocnemius<br />
muscle oxygen saturation from 68% to 58%. 115 The low lithotomy<br />
position resulted in a reduction of about 16% in lower leg systolic<br />
pressures, whereas an exaggerated lithotomy positions was<br />
associated with a decrease of almost 40% in lower leg pressures<br />
when compared with the supine data. When a 15-degree headdown<br />
tilt is added, the decrease in lower leg pressures was more<br />
significant. 116 MAPs of this level have been associated with the<br />
development of compartment syndromes, especially in patients<br />
who are in the lithotomy positions for 5 hours or more. In<br />
addition, these changes would be exacerbated in patients with<br />
peripheral vessel diseases flow, provoked ischemia in the lower<br />
limbs, and predisposed to lower extremity venous thrombosis.<br />
The lithotomy position limits respiratory movements by<br />
compression of abdominal viscera. It reduces the vital capacity of<br />
normal conscious patients by 18% as a result of the marked<br />
restriction of abdominal movement. The FRC and tidal volume are,<br />
however, minimally affected in the awake patient. However, it is<br />
suggested that raising the legs appeared to have little impact on<br />
respiratory elastance and resistances. 15 During spontaneous res -<br />
piration in anesthetized patients placed in the lithotomy position,<br />
a 3% reduction in tidal volume was seen and a 10-degree headdown<br />
tilt led to a 14% decrease. 50 Patients placed in the flexed headdown<br />
position, compared with the supine position, developed a<br />
significant decrease in arterial oxygen tension (14%) and a signi -<br />
ficant increase in CO 2<br />
tension (23%) and shunt fraction (78%). 117<br />
Complications Associated With<br />
the Lithotomy Position<br />
Although several complications have been reported, including<br />
finger burn, low back pain (14%) postoperatively, 118 and rhabdo -<br />
myolysis and elevated creatine kinase due to compression of calf<br />
muscles and ischemia, 119 none of these is known to have happened<br />
in children. Compartmental syndrome, a rare but life-threatening<br />
complication, particularly with head-down tilt (Lloyd Davies<br />
position) was reported after a lengthy procedure in the pediatric<br />
age group due to hypoperfusion and external compression by leg<br />
supports. 120,121 By placing the child in the lithotomy position only<br />
when access to the lower abdomen and perineum is required,<br />
these injuries may be avoided. For a lengthy procedure, using a leg<br />
support that places pressure on the popliteal fossa or the calf<br />
should be avoided. Systemic hypotension should be avoided and<br />
the risk posed by vasoconstrictive agents that decrease peripheral<br />
blood flow should be kept in mind. If needed, a clinical diagnosis<br />
can be obtained by venogram and magnetic resonance imaging<br />
(MRI). The venogram will demonstrate an external compression<br />
of the popliteal vein and the MRI an extensive muscle edema.<br />
Fasciotomies are necessary to relieve the compartment syndrome,<br />
whereas adequate rehydration and alkalinization of urine are<br />
cornerstones for the management of acute renal failure.<br />
Persistent neuropathies have been reported with an incidence<br />
of 1 per 3608 anesthetic instillations in a general surgical popula -<br />
tion. 122 Thin patients with a body mass index of less than 20,<br />
diabetes mellitus, and peripheral vascular disease in smokers<br />
predispose the patients to the development of lower limb neuropa -<br />
thies. Prolonged procedures (>4 h) are a definite association. Each<br />
hour in a lithotomy position increases the risk of motor neuro -<br />
pathy 100-fold. 122 This finding suggested that alternatives should<br />
be sought when a prolonged surgery in the lithotomy is planned.<br />
Forty percent of isolated sciatic neuropathies are associated with<br />
operation using the lithotomy position. Unlike compartment<br />
syndrome in which a prolonged duration in the lithotomy position<br />
is a significant risk factor, sciatic nerve injuries may occur even<br />
after short procedures. 123 The mechanisms for the development of<br />
neurapraxia include ischemic changes from a compartment<br />
syndrome or a direct compression of the nerve. 120 The sciatic nerve<br />
may be subjected to excessive stretching forces. The common<br />
peroneal nerve and its distal branches are the most common major<br />
motor nerve in the lower extremities to be affected by the litho -<br />
tomy position. 122 The common peroneal nerve may be compressed<br />
against the upright pole of stirrups as it passes around the head of<br />
the fibula when the legs are placed inside the poles. It is important<br />
also to remember that external pressure exerted by the surgical<br />
assistant leaning against the knees could contribute to this<br />
problem. The saphenous nerve may be compressed against the<br />
stirrups poles as it courses superficially near the medial malleolus<br />
when the legs are placed outside the poles. Femoral neuropathy<br />
have been reported and is thought to result from the extreme<br />
abduction of the thighs with external rotation at the hip causing<br />
ischemia of the femoral nerve as it is kinked beneath the tough<br />
inguinal ligament.<br />
To prevent lower back injury, the lower limbs should be moved<br />
simultaneously and symmetrically. The lower back should be<br />
supported to maintain the normal lumbar lordosis. Hip disloca -<br />
tion may follow slippage or disconnection of lithotomy poles.<br />
Lowering of the legs at the end of the surgery may be followed by<br />
hypotension secondary to hypovolemia. Accidental entrapment<br />
of the digits when lowering or raising the end of the operating<br />
table can cause crush injury, amputation, or skin breakdown. 121<br />
SITTING POSITION<br />
General Considerations<br />
The use of the sitting position has decreased over the years.<br />
A postal survey of the use of the sitting position in general
1356 PART 4 ■ Special Monitoring and Resuscitation Techniques<br />
neuro surgical practice in Britain was conducted in 1991. Com -<br />
pared with the data from 1981, the number of neurosurgical<br />
centers using the sitting position for posterior fossa surgery and<br />
posterior cervical spine surgery decreased more than 50%. 124 The<br />
surgical position is said to offer surgical advantages such as better<br />
surgical exposure; less tissue traction; less bleeding; less cranial<br />
nerve damage; more complete resection of the lesion; ready access<br />
to the airway, chest, and extremities; and presence of monitoring<br />
methods for early detection of venous air embolism (VAE).<br />
Neurosurgical practice in Germany, however, retained the sitting<br />
position as the preferred position for posterior fossa and cranio -<br />
spinal surgery, although the prone position is an alternative for<br />
use during posterior cervical surgery. Alternative positions like<br />
the lateral or the “park-bench” positions are rarely used. 125 The low<br />
sitting position offers main advantages over the sitting position by<br />
reducing venous pooling in the dependent areas as well as a<br />
reduced risk of VAE. The torso is usually placed in the midline of<br />
the operating table and the back section of the table is elevated.<br />
The hips and knees are flexed to provide some stability. The<br />
operating table is adjusted until the lower limbs are at the level of<br />
the heart. Pads are placed beneath the knees, as in the sitting<br />
position, to relieve ligamentous stress. The head-elevated prone<br />
position is mainly used during proce dures on the posterior cranial<br />
fossa or the cervical spine. Venous congestion at the operative site<br />
is minimal with gravity drainage. The arms of the patient are<br />
usually placed alongside the torso. Because the operative site is<br />
above the level of the heart, air embolism is a significant risk and<br />
appropriate monitoring should be instituted.<br />
There are several relative contraindications to the sitting position<br />
such as ventriculoatrial shunt in place and open, cerebral<br />
ischemia upright awake, left atrial pressure more than right atrial<br />
pressure, platypnea-orthodeoxia, and preoperative demonstration<br />
of patent foramen ovale or right-to-left shunt. If a shunt tube is in<br />
place from the cerebral ventricular system to the right atrium, air<br />
may enter the end of the shunt as cerebrospinal fluid drains out<br />
and may be pulled into the heart. The noncollapsible tubing acts<br />
as a noncollapsible vein and allows air to pass unimpeded into the<br />
heart. This is not a potential problem with a ventriculoperitoneal<br />
shunt, because the air would have no venous access. We recom -<br />
mend that a patient with a ventriculoatrial shunt in place have the<br />
shunt tied off before undergoing an intracranial procedure in the<br />
sitting position. Some patients experience cerebral ischemia<br />
whenever they assume the upright position. Their cardiovascular<br />
and cerebrovascular systems may both be implicated in this situa -<br />
tion. These patients may present for an extracranial-intracranial<br />
bypass for the posterior cerebral circulation; some surgeons<br />
believe that the sitting position gives the best exposure for this<br />
procedure. We cannot be sure that cerebral circulation will be<br />
maintained in the sitting position, because we must not only place<br />
the patient upright but also provide an anesthetic. It seems a<br />
reasonable balance of risks and benefits to place such a patient in<br />
the horizontal position. There has been suggested that, if the left<br />
atrial pressure, as measured by pulmonary artery occlusion<br />
pressure, is less than the right atrial pressure in the sitting position,<br />
the patient should be placed horizontally because of an increased<br />
risk of paradoxical embolism. 126 This is based on two important<br />
assumptions: (1) the left atrial pressure will be greater than the<br />
right atrial pressure in the horizontal position and (2) the atrial<br />
pressure gradient and its direction constitute a prognostic<br />
indicator of whether VAE will become paradoxical air embolism<br />
(PAE). Some work suggests that these assumptions may not be<br />
applicable. In a pig model with an iatrogenic atrial septal defect,<br />
the atrial pressure gradient before air embolism was unrelated to<br />
the occurrence of PAE. 127 We believe that decisions regarding the<br />
use of the sitting position based on estimates of preoperative atrial<br />
pressure gradients are not well founded. Some patients demon -<br />
strate a potential right-to-left shunt before surgery. Platypnea/<br />
orthodeoxia is an unusual cardiovascular illness in which the atrial<br />
gradients apparently reverse when the upright position is assum -<br />
ed. 128 Patients with this condition are well oxygenated in the supine<br />
position but become easily desaturated in the upright position<br />
because of unsaturated blood passing from right to left at the atrial<br />
level. Other patients demonstrate a patent foramen ovale before<br />
surgery during a cardiac work-up, and still others may have a<br />
known right-to-left shunt. These patients might be at greater risk<br />
for PAE should VAE occur; therefore, it seems prudent to give<br />
these findings appropriate consideration before using the sitting<br />
position for such patients.<br />
Physiology of the Sitting Position<br />
Of all the surgical positions commonly used, the effects of gravity<br />
on the cardiovascular system are most evident in the sitting posi -<br />
tion. The magnitude of the hemodynamic changes will be depen -<br />
dent upon the type of sitting position adopted and influenced by<br />
the anesthetic agents employed. The gravitational effects will have<br />
the most significant impact in the full sitting position with a<br />
straight back and legs dependent; this posture is, fortunately, rarely<br />
used nowadays. Modifications in which the legs and thighs are<br />
flexed and the feet are at the level of the heart will have less signi -<br />
ficant hemodynamic effects. Different anesthetics with their dif -<br />
ferent pharmacologic effects may affect the hemodynamics<br />
differently. The incidence of hypotension in anesthetized patients<br />
in the sitting position varies from 5% to more than 30%. The<br />
incidence and extent of hypotension in the sitting position are<br />
influenced by the technique of patient positioning, the use of<br />
equipment such as elastic stocking wrapping or antigravity suits to<br />
minimize the effects of gravity on hemodynamics, the physical<br />
status of the patients studied, and the anesthetic techniques. 129 A<br />
significant decrease in the right atrial pressure from a mean of 3.4<br />
to 0.68 mmHg was observed in 60 anesthetized-paralyzed patients<br />
aged 2 to 13 years scheduled for neurosurgical procedures in the<br />
sitting position. Of these, 25% of patients had a subatmospheric<br />
right atrial pressure, although MAP was only slightly decreased. 129<br />
These results are consistent with the decrease in venous return to<br />
the heart and diminished filling of pulmonary vessels. These<br />
effects were expected to be more exaggerated in hypovolemic<br />
patients.<br />
With the patient breathing spontaneously, the sitting position<br />
caused the least physiologic changes in the respiratory system<br />
among all the positions described. Because the weight of the<br />
abdominal contents is not acting against the diaphragm in the<br />
sitting position, it offers the least restriction to movement of<br />
the diaphragmatic or chest wall and the least impairment of FRC.<br />
Lung volumes are preserved with increases in the FRC and closing<br />
volume from supine values. 130 The average lung compliance was<br />
greatest in patients in the sitting position, less in the lateral, and the<br />
least in the supine positions. The total respiratory resistance is 40<br />
to 50% less in the sitting position compared with supine values.<br />
Because of the effects of gravity on the pulmonary circulation, the<br />
upper lung fields are less well perfused. There is closure of alveolar<br />
and extra-alveolar vessels in the upper part of the lung in the
CHAPTER <strong>80</strong> ■ Patient Positioning and Precautions During Anesthesia and Surgery 1357<br />
patients placed in the sitting position. The use of intermittent<br />
positive-pressure ventilation may further reduce blood flow to<br />
these areas. There is an increase in the nonuniformity of intra -<br />
pulmonary gas distribution in patients who are anesthetized and<br />
mechanically ventilated compared with awake values in the sitting<br />
position, 131 and this may lead to V˙/Q˙ mismatch. Volatile agents<br />
abolish the hypoxic pulmonary vasoconstriction responses and<br />
exacerbate the mismatch. The reduction in cardiac output in the<br />
upright posture also led to the significant decrease in arterial<br />
oxygenation. 132 These pulmonary effects is children are similar to<br />
those in adults. The effects of body positions on pulmonary<br />
mechanics were examined in 30 former preterm infants. 133 These<br />
infants were sedated and kept breathing spontaneously. Changing<br />
from a supine position to semisitting position at 45 degrees<br />
decreased total pulmonary resistance and augmented the specific<br />
and dynamic lung compliances and increased FRC.<br />
The neck and cerebral vessels above the level of the heart are<br />
subjected to reductions in intra-arterial and venous pressures in<br />
the sitting position because of gravitational forces. The subatmos -<br />
pheric pressure within the neck veins predisposes the patient to<br />
the risk of VAE. The relationship of superior sagittal sinus pressure<br />
(SSP) to head position during jugular venous compression and<br />
PEEP on SSP was examined in 15 children. 134 Progressive head<br />
elevation significantly decreased mean SSP, and in 5 patients, SSP<br />
was less than 0 mmHg at 90 degrees torso elevation. The applica -<br />
tion of 10 cmH 2<br />
O PEEP was ineffective in raising the SSP, whereas<br />
bilateral internal jugular compression always caused a significant<br />
increase in SSP. These observations suggest that children are at<br />
great risk for VAE when undergoing neurosurgical procedures in<br />
the sitting position because intracranial venous pressure is often<br />
subatmospheric when the head is elevated.<br />
A head-up position may have beneficial effects on ICP via<br />
changes in MAP, airway pressure, CVP, and cerebrospinal fluid<br />
displacement. A paradoxical increase of cerebrovascular tone and<br />
ICP may occur, however, when the head-up position is associated<br />
with a decrease in MAP through autoregulation mechanisms. This<br />
is mainly because of the compensatory increase in systemic<br />
vascular resistance in response to the reduction in systemic arterial<br />
pressure. When mechanical ventilation with PEEP is used in<br />
patients without intracranial hypertension, intracranial perfusion<br />
is unchanged. However, in patients with increased ICP, the<br />
combination of head flexion with application of PEEP may result<br />
in a dangerous increase in ICP, even when the patients were in the<br />
sitting position. 135<br />
Complications of the Sitting Position<br />
Hypotension is the most common complication of the sitting<br />
position. Measures to minimize hypotension include slow staged<br />
positioning over 10 to 20 minutes and adequate fluid loading. The<br />
use of compressive elastic bandages or stockings to wrap the lower<br />
limbs before elevating the patient may partially reduce the amount<br />
of blood pooled in the dependent structures. Treatment with<br />
vasopressors may be required in severe cases. Vital sign changes<br />
resulting from brain manipulation may also occur. Positioning the<br />
patient from supine to sitting is a common cause of tracheal tube<br />
malplacement in the pediatric patient because the distance be -<br />
tween the vocal cords and the carina is shorter than in the adult. 55<br />
It is not uncommon for the head to be flexed excessively in the<br />
sitting position to optimize surgical exposure; compression or<br />
kinking of the tracheal tube may result. A reinforced tube is<br />
recommended and there should be at least one fingerbreadth<br />
distance between the chin and the chest. The insertion of the<br />
transesophageal echocardiography or Doppler probe may lead to<br />
misplacement or compression of the tracheal tube. The major phy -<br />
siologic concern for patients in the sitting position is air entrain -<br />
ment when the surgical site is above the level of the heart, which<br />
may result in VAE (see <strong>Chapter</strong> 57).<br />
Peripheral nerve injuries reported with the sitting position are<br />
likely to be due to faulty positioning or prolonged surgery. Com -<br />
mon peroneal nerve injury is fortunately rare (incidence < 1%).<br />
However, sciatic nerve injury is more frequent as a result of<br />
compression or stretching. Other nerves injuries such as brachial<br />
plexus 136 and recurrent laryngeal nerve palsies have also been<br />
reported. 137 The latter was attributed to the large probes placed in<br />
conjunction with neck flexion and tracheal intubation. Quadri -<br />
plegia is rare and the result of prolonged stretching and compres -<br />
sion of the cervical cord from excessive head flexion, 138 PAE into<br />
the arterial system, and occlusion of the vertebral artery due to<br />
excessive neck flexion. Young patients exhibiting extraordinary<br />
growth spurts may demonstrate a higher risk for this complica -<br />
tion. Nitta and colleagues described a 7-year-old boy who develop -<br />
ed acute cervical spinal cord infarction after an operation in the<br />
sitting position. 138 It was assumed that head flexion and the<br />
presence of the abnormal skeletal growth spurt resulting from an<br />
excessive secretion of human chorionic gonadotropin from a<br />
tumor was a possible predisposing factor for this complication. 139<br />
Somatosensory evoked potential monitoring has been proposed<br />
as an indicator of the adequacy of regional spinal cord perfusion<br />
in cases requiring sitting position during surgery.<br />
Macroglossia may result in either inadequate positioning of the<br />
head or excessive oral cavity manipulation. Extreme flexion of the<br />
head with the chin resting on the chest and the prolonged use of<br />
an oral airway may promote obstruction of venous and lymphatic<br />
drainage of the tongue after procedures performed in the sitting<br />
position. Postoperative macroglossia may lead to airway obstruc -<br />
tion. It is recommended that any oral airway should not be left in<br />
the oral cavity and a bite block used instead.<br />
Deep venous thrombosis is frequent during prolonged surgery,<br />
especially if associated with intraoperative hypotension. In larger<br />
patients, the use of sequential pneumatic compression devices<br />
should be used to minimize this risk.<br />
Blindness is an unusual complication that may result from<br />
direct compression of the eye. Pediatric patients, especially new -<br />
borns and infants, are at higher risk because the horseshoe<br />
headrest is often used and most often inappropriately sized for the<br />
zygomatic arches. Blindness may also result from an episode of air<br />
embolism involving the occipital cortex. 140<br />
PROLONGED BEDREST AND<br />
PATIENT TRANSPORT<br />
Prolonged bedrest may be responsible for most of the physiologic<br />
changes occurring with postural changes. A contraction of the<br />
plasma and blood volume (10–16%) as well as altered vasomotor<br />
responses have been observed after 2 to 6 weeks with 6-degree mild<br />
head-down bedrest. The latter is probably due to the inhi bition of<br />
the synthesis and release of norepinephrine. These changes lead to<br />
orthostatic intolerance with a decrease in blood pressure when<br />
these subjects are seated upright. 141 A down-regula tion of the<br />
cardiovascular oxygen transport system is seen after prolonged<br />
bedrest. Stroke volume, cardiac output, and hemoglo bin level are
1358 PART 4 ■ Special Monitoring and Resuscitation Techniques<br />
lowered after an enforced period of inactivity. This is accompanied<br />
by a decreased in oxygen delivery up to 40% at rest whereas oxygen<br />
consumption is reduced by almost 16%. 142 A similar reduction of<br />
13% in maximal oxygen consumption was reported in children<br />
aged 7 to 11 years after 9 weeks of bedrest for various illnesses. 143<br />
Prolonged bedrest produces profound changes in muscle and bone,<br />
particularly of the lower limbs. Dramatic change in muscle mass<br />
occurs within 4 to 6 weeks of bedrest, which is associated with<br />
a reduction in muscle strength of 40%. Even in young students,<br />
10 days of bedrest led to decreases in muscle strength and mass.<br />
Isometric muscle strength was de creased in both nonantigravity<br />
and antigravity muscles, although the rate of changes did not<br />
correlate with the corresponding changes in muscle mass. A<br />
reduction in neuromuscular function probably contributed to the<br />
decreases in maximum voluntary strength, 144 whereas a decrease<br />
in muscle protein synthesis accounts for the decrease in both whole<br />
body and skeletal muscle mass. 145 Ideally, patients should be<br />
transferred in their bed from their ward to the operating theater. In<br />
patients who have been confined to bed for a prolonged period,<br />
the physiologic derange ments may provoke dizziness and nausea,<br />
possibly hypotension. All patients should be reviewed thoroughly<br />
before anesthesia induction because the potential complications<br />
that may arise from the transport-related instability are certainly<br />
preventable. Transfer of the patient onto the operating table should<br />
be done as gently as possible. Careful planning must be achieved<br />
before positioning.<br />
POSITIONING IN PARTICULAR CASES<br />
Experienced personnel should tailor the required and special<br />
consideration during positioning to each patient depending on<br />
the patient’s own medical condition, physical deformity, and<br />
surgical needs, avoiding anticipated complications that could<br />
happen such as compression injuries, hemodynamic effects, or<br />
respiratory problems. For example, placing neurologic patients<br />
with contracture deformities in the supine position is sometimes<br />
difficult or impossible. Care has to be taken not to overstretch the<br />
extremities in these situations, and the most appropriate position<br />
exposing the surgical field can be achieved by cooperation with<br />
surgeons and other personnel, to reach the optimum for the<br />
patient’s condition. For instance, patients suffering from osteo -<br />
genesis imperfecta, a group of connective tissue disorders, are<br />
characterized by very fragile bones that can fracture easily during<br />
positioning for surgery. Patients affected with severe scoliosis can<br />
render positioning difficult. Patients presenting with Down<br />
syndrome are another case in which special consideration must<br />
be taken during positioning. Occipitoatlantoaxial instability must<br />
be kept in mind to avoid subluxation or fracture of the cricoid<br />
apophysis, especially in prone position. Care should be taken to<br />
avoid forced extension and flexion by in-line stabilization by a<br />
skilled helper.<br />
CONCLUSION<br />
The reduction of potential morbidity associated with positioning<br />
of patients in the operating room begins with a well-conducted<br />
preoperative evaluation. Risk factors should be assessed while<br />
evaluating the range of movement, especially the joints most<br />
involved for the patient’s position during surgery. Obvious defor -<br />
mity should be assessed and the neurologic function documented.<br />
Adequate protection should be conferred to these during the<br />
operative procedure. Communication with surgical colleagues is<br />
of prime importance to determine the position ex pected for<br />
surgery; operating room personnel should be informed of the<br />
intention; and all proper equipment needed to achieve safe<br />
positioning of the patient should be readily available. Transfer of<br />
patients to the operating rooms should be a stress-free experience<br />
for all involved, and coordination between the transport and the<br />
operating staff should be discussed before beginning anesthesia. It<br />
is essential that all equipment be serviced regularly and rechecked<br />
before every use. Knowledgeable staff acquainted with the phy -<br />
siologic demands of specific positions should ideally be present<br />
during the positioning of the patient. Accurate intraoperative<br />
documentation is imperative once the patient has been positioned.<br />
Immediately after positioning, airway equipment, ventilation, and<br />
hemodynamic stability should be checked, and confirmation that<br />
everything is in order should be obtained confirmed before any -<br />
thing else is done to the patient. All monitoring devices, intra -<br />
vascular lines, and proper padding to avoid pressure point<br />
complications must be provided. Special attention to the face, eyes,<br />
neck, and neurovascular structures must be checked before the<br />
patient is covered with the surgical blankets. As much as correct<br />
positioning can effectively aid surgery, improper positioning<br />
should never be accepted because the consequences potentially<br />
resulting from any oversight can lead to permanent injuries and<br />
dramatic outcome for the patient, the family, and the professionals<br />
involved in his or her care.<br />
REFERENCES<br />
1. Dixon BJ, Carden JR, Jennifer R, et al. Preoxygenation is more effective in<br />
the 25-degrees head up position than in the supine position in severely<br />
obese patients: a randomized controlled study. Anesthesiology. 2005;102:<br />
1110–1115.<br />
2. Knight JW, Mahajan RP. Patient positioning in anaesthesia. Continuing<br />
Education in Anaesthesia. Crit Care Pain. 2004;4:160–163.<br />
3. Reber A, Nylund U, Hedenstierna G. Position and shape of the dia -<br />
phragm: implications for atelectasis formation. Anaesthesia. 1998;53:<br />
1054–1061.<br />
4. Taussig LM, Harris TR, Lebowitz MD. Lung function in infants and<br />
young children: functional residual capacity, tidal volume, and respiratory<br />
rats. Am Rev Respir Dis. 1977;116:233–239.<br />
5. Damgaard PK, Qvist T. Pediatric pulmonary CT-scanning. Anaesthesiainduced<br />
changes. Pediatr Radiol. 19<strong>80</strong>;9:145–148.<br />
6. Reber A, Engberg G, Sporre B, et al. Volumetric analysis of aeration in<br />
the lungs during general anaesthesia. Br J Anaesth. 1996;76:760–766.<br />
7. Tusman G, Böhm SH, Vazquez de Anda GF, et al. “Alveolar recruitment<br />
strategy” improves arterial oxygenation during general anaesthesia. Br J<br />
Anaesth. 1999;82: 8–13.<br />
8. Shulman D, Beardsmore CS, Aronson HB, et al. The effect of ketamine on<br />
the functional residual capacity in young children. Anesthesiology. 1985;<br />
62:551–556.<br />
9. Fletcher ME, Stack C, Ewart M, et al. Respiratory compliance during<br />
sedation, anesthesia, and paralysis in infants and young children. J Appl<br />
Physiol. 1991;70:1977–1982.<br />
10. Fletcher ME, Ewert M, Stack C, et al. Influence of tidal volume on<br />
respiratory compliance in anesthetized infants and young children. J Appl<br />
Physiol. 1990;68:1127–1133.<br />
11. Cheney FW, Domino KB, Caplan RA, et al. Nerve injury associated with<br />
anesthesia: a closed claims analysis. Anesthesiology. 1999;90:1062–1069.<br />
12. American Society of Anesthesiologists. Practice advisory for prevention<br />
of perioperative peripheral neuropathies: a report by the American<br />
Society of Anesthesiologists Task Force on Prevention of Perioperative<br />
Peripheral Neuropathies. Anesthesiology. 2000;92:1168–1182.<br />
13. Perreault L, Drolet P, Farny J. Ulnar nerve palsy at the elbow after general<br />
anaesthesia. Can J Anaesth. 1992;39:499–503.
CHAPTER <strong>80</strong> ■ Patient Positioning and Precautions During Anesthesia and Surgery 1359<br />
14. Choufane S, Lemogne M, Jacob L. Unexpected rhabdomyolysis with<br />
myoglobinuria in a patient in the supine position. Eur J Anaesthesiol.<br />
1998;15:493–496.<br />
15. Barnas GM, Green MD, Mackenzie CF, et al. Effect of posture on lung<br />
and regional chest wall mechanics. Anesthesiology. 1993;78:251–259.<br />
16. Fahy BG, Barnas GM, Nagle SE, et al. Effects of Trendelenburg and<br />
reverse Trendelenburg postures on lung and chest wall mechanics. J Clin<br />
Anesth. 1996;8:236–244.<br />
17. Gannedahl P, Odeberg S, Brodin LA, et al. Effects of posture and<br />
pneumoperitoneum during anaesthesia on the indices of left ventricular<br />
filling. Acta Anaesthesiol Scand. 1996;40:160–166.<br />
18. Hachenberg T, Ebel C, Czorny M, et al. Intrathoracic and pulmonary<br />
blood volume during CO 2<br />
-pneumoperitoneum in humans. Acta<br />
Anaesthesiol Scand. 1998;42:794–798.<br />
19. Dorsay DA, Greene FL, Baysinger CL. Hemodynamic changes during<br />
laparoscopic cholecystectomy monitored with transesophageal<br />
echocardiography. Surg Endosc. 1995;9:128–133.<br />
20. Viale JP, Annat G, Bertrand O, et al. Continuous measurement of pulmo -<br />
nary gas exchange during general anaesthesia in man. Acta Anaesthesiol<br />
Scand. 1988;32:691–697.<br />
21. Critchley LA, Critchley JA, Gin T. Haemodynamic changes in patients<br />
undergoing laparoscopic cholecystectomy: measurement by transthoracic<br />
electrical bioimpedance. Br J Anaesth. 1993;70:681–683.<br />
22. Rose DK, Cohen MM, Soutter DI. Laparoscopic cholecystectomy: the<br />
anaesthetist’s point of view. Can J Anaesth. 1992;39:<strong>80</strong>9–815.<br />
23. Mattioli G, Montobbio G, Pini Prato A, et al. Anesthesiologic aspects of<br />
laparoscopic fundoplication for gastroesophageal reflux in children with<br />
chronic respiratory and gastroenterological symptoms. Surg Endosc.<br />
2003;17:559–566.<br />
24. Ko MT, Chuang KC, Su CY. Multiple analyses of factors related to<br />
intraoperative blood loss and the role of reverse Trendelenburg position<br />
in endoscopic sinus surgery. Laryngoscope. 2008;118:1687–1691.<br />
25. Taylor J, Weil MH. Failure of the Trendelenburg position to improve<br />
circulation during clinical shock. Surg Gynecol Obstet. 1967;124:1005–<br />
1010.<br />
26. Russo A, Marana E, Viviani D, et al. Diastolic function: the influence of<br />
pneumoperitoneum and Trendelenburg positioning during laparoscopic<br />
hysterectomy. Eur J Anaesthesiol. 2009;26:923–927.<br />
27. Terai C, Anada H, Matsushima S, et al. Effects of mild Trendelenburg on<br />
central hemodynamics and internal jugular vein velocity, cross-sectional<br />
area, and flow. Am J Emerg Med. 1995;13:255–258.<br />
28. Sing RF, O’Hara D, Sawyer MA, et al. Trendelenburg position and oxygen<br />
transport in hypovolemic adults. Ann Emerg Med. 1994;23:564–567.<br />
29. Ostrow CL, Hupp E, Topjian D. The effect of Trendelenburg and modified<br />
Trendelenburg positions on cardiac output, blood pressure, and oxygena -<br />
tion: a preliminary study. Am J Crit Care. 1994;3:382–386.<br />
30. Armstrong PJ, Sutherland R, Scott DH. The effect of position and<br />
different manoeuvres on internal jugular vein diameter size. Acta<br />
Anaesthesiol Scand. 1994;38:229–231.<br />
31. Tartiere D, Seguin P, Juhel C, et al. Estimation of the diameter and crosssectional<br />
area of the internal jugular veins in adult patients. Crit Care.<br />
2009;13:R197.<br />
32. Jin TK, Chun SP, Hyun JK, et al. The effect of inguinal compression,<br />
Valsalva maneuver, and reverse Trendelenburg position on the crosssectional<br />
area of the femoral vein in children. Anesth Analg. 2009;108:<br />
1493–1496.<br />
33. Casati A, Salvo I, Torri G, et al. Arterial to end-tidal carbon dioxide<br />
gradient and physiological dead space monitoring during general<br />
anaesthesia: effects of patients’ position. Minerva Anestesiol. 1997;63:177–<br />
182.<br />
34. Manner T, Aantaa R, Alanen M. Lung compliance during laparoscopic<br />
surgery in paediatric patients. Paediatr Anaesth. 1998;8:25–29.<br />
35. Sfez M. Laparoscopic surgery in paediatrics: the point of view of the<br />
anesthetist. Cah Anesthesiol. 1993;41:237–244.<br />
36. Bannister C, Brosius K, Wulkan M. The effect of insufflations pressure<br />
on pulmonary mechanics in infants during laparoscopic surgical<br />
procedures. Paediatr Anaesth. 2003;13:785–789.<br />
37. Baroncini S, Gentili A, Pigna A, et al. Anaesthesia for laparoscopic surgery<br />
in paediatrics. Minerva Anestesiol. 2002;68:406–413.<br />
38. Kirkinen P, Hirvonen E, Kauko M, et al. Intracranial blood flow during<br />
laparoscopic hysterectomy. Acta Obstet Gynecol Scand. 1995;74:71–74.<br />
39. Doi M, Kawai Y. Mechanisms of increased intracranial pressure in rabbits<br />
exposed to head-down tilt. Jpn J Physiol. 1998;48:63–69.<br />
40. Heijke SA, Smith G, Key A. The effect of the Trendelenburg position on<br />
lower oesophageal sphincter tone. Anaesthesia. 1991;46:185–187.<br />
41. Tournadre JP, Chassard D, Berrada KR, et al. Effect of pneumoperitoneum<br />
and Trendelenburg position on gastro-oesophageal reflux and lower<br />
oesophageal sphincter pressure. Br J Anaesth. 1996;76:130–132.<br />
42. Romanowski L, Reich H, McGlynn F, et al. Brachial plexus neuropathies<br />
after advanced laparoscopic surgery. Fertil Steril. 1993;60:729–732.<br />
43. Goskowicz R. Use of shoulder restraints during arm abduction and steep<br />
Trendelenburg’s position. Anesthesiology. 1995;83:1377–1378.<br />
44. Winter R, Munro M. Lingual and buccal nerve neuropathy in a patient in<br />
the prone position: a case report. Anesthesiology. 1989;71:452–454.<br />
45. Oliver SB, Cucchiara RF, Warner MA. Unexpected focal neurologic deficit<br />
on emergence from anesthesia: a report of three cases. Anesthesiology.<br />
1987;67:823–826.<br />
46. Jaffe TB, McLeskey CH. Position-induced Horner’s syndrome. Anes -<br />
thesiology. 1982;56:49–50.<br />
47. Litman R, Wake N, Chan L, et al. Effect of lateral positioning on upper<br />
airway size and morphology in sedated children. Anesthesiology. 2005;103:<br />
484–488.<br />
48. Halachmi S, El-Ghoneimi A, Bissonnette B, et al. Hemodynamic and<br />
respiratory effect of pediatric urological laparoscopic surgery: a<br />
retrospective study. J Urol. 2003;170:1651–1654.<br />
49. Lorenzo AJ, Karsli C, Halachmi S, et al. Hemodynamic and respiratory<br />
effects of pediatric urological retroperitoneal laparoscopic surgery: a<br />
prospective study. J Urol. 2006;175:1461–1465.<br />
50. Larsson A, Jonmarker C, Jogi P, et al. Ventilatory consequences of the lateral<br />
position and thoracotomy in children. Can J Anaesth. 1997;34:141–145.<br />
51. Hedenstierna G, Baehrendtz S, Klingstedt C, et al. Ventilation and<br />
perfusion of each lung during differential ventilation with selective PEEP.<br />
Anesthesiology. 1984;61:369–376.<br />
52. Tanskanen P, Kytta J, Randell T. The effect of patient positioning on<br />
dynamic lung compliance. Acta Anaesthesiol Scand. 1997;41:602–606.<br />
53. Heaf DP, Helms P, Gordon I, et al. Postural effects on gas exchange in<br />
infants. N Engl J Med. 1983;308:1505–1508.<br />
54. Davies H, Helms P, Gordon I. Effect of posture on regional ventilation in<br />
children. Pediatr Pulmonol. 1992;12:227–232.<br />
55. Sugiyama K, Yokoyama K. Displacement of the endotracheal tube caused<br />
by change of head position in pediatric anesthesia: evaluation by<br />
fiberoptic bronchoscopy. Anesth Analg. 1996;82:251–253.<br />
56. Hartrey R, Kestin IG. Movement of oral and nasal tracheal tubes as a re -<br />
sult of changes in head and neck position. Anaesthesia. 1995;50:682–687.<br />
57. Karzai W, Schwarzkopf K. Hypoxaemia during one-lung ventilation:<br />
pre diction, prevention and treatment. Anesthesiology. 2009;110:1402–<br />
1411.<br />
58. Mathes DD, Assimos DG, Donofrio PD. Rhabdomyolysis and myonecro -<br />
sis in a patient in the lateral decubitus position. Anesthesiology. 1996;84:<br />
727–729.<br />
59. Edgcombe H, Carter K, Tarrow S. Anaesthesia in the prone position. Br<br />
J Anaesth. 2008;100:165–183.<br />
60. Lee TC, Yang LC, Chen HJ. Effect of patient position and hypotensive<br />
anesthesia on inferior vena caval pressure. Spine. 1998;23:941–945.<br />
61. McNulty SE, Weiss J, Azad SS, et al. The effect of the prone position on<br />
venous pressure and blood loss during lumbar laminectomy. J Clin Anesth.<br />
1992;4:220–225.<br />
62. Dharmavaram S, Jellish WS, Nockels RP, et al. Effect of prone positioning<br />
systems on hemodynamic and cardiac function during lumbar spine<br />
surgery: an echocardiographic study. Spine. 2006 20;31:1388–1393.<br />
63. Wadsworth R, Anderton JM, Vohra A. The effect of four different surgical<br />
prone positions on cardiovascular parameters in healthy volunteers.<br />
Anaesthesia. 1996;51:819–822.<br />
64. Pump B, Talleruphuus U, Christensen NJ, et al. Effects of supine, prone,<br />
and lateral positions on cardiovascular and renal variables in humans.<br />
Am J Physiol Regul Integr Comp Physiol. 2002;283:174–1<strong>80</strong>.<br />
65. Sudheer PS, Logan SW, Ateleanu B, et al. Haemodynamic effects of the<br />
prone position, a comparison of propofol total intravenous and inhalation<br />
anaesthesia. Anaesthesia. 2006;61:138–141.<br />
66. Pelosi P, Croci M, Calappi E, et al. The prone positioning during general<br />
anesthesia minimally affects respiratory mechanics while improving<br />
functional residual capacity and increasing oxygen tension. Anesth Analg.<br />
1995;<strong>80</strong>:955–960.<br />
67. Lorino AM, Atlan G, Lorino H, et al. Influence of posture on mechanical<br />
parameters derived from respiratory impedance. Eur Respir J. 1992;5:<br />
1118–1122.
1360 PART 4 ■ Special Monitoring and Resuscitation Techniques<br />
68. Stone JG, Khambatta HJ. Pulmonary shunts in the prone position.<br />
Anaesthesia. 1978;33:512–517.<br />
69. Wahba RW, Tessler MJ, Kardash KJ. Carbon dioxide tensions during<br />
anesthesia in the prone position. Anesth Analg. 1998;86:668–669.<br />
70. Jolliet P, Bulpa P, Chevrolet JC. Effects of the prone position on gas<br />
exchange and hemodynamics in severe acute respiratory distress<br />
syndrome. Crit Care Med. 1998;26:1977–1985.<br />
71. Martin RJ, Herrell N, Rubin D, et al. Effect of supine and prone positions<br />
on arterial oxygen tension in the preterm infant. Pediatrics. 1979;63:<br />
528–531.<br />
72. Trottier SJ. Prone position in acute respiratory distress syndrome: turning<br />
over an old idea. Crit Care Med. 1998;26:1934–1935.<br />
73. Pelosi P, Croci M, Calappi E, et al. Prone positioning improves pulmonary<br />
function in obese patients during general anesthesia. Anesth Analg.<br />
1996;83:578–583.<br />
74. Glenny RW, Bernard S, Robertson HT, et al. Gravity is an important but<br />
secondary determinant of regional pulmonary blood flow in upright<br />
primates. J Appl Physiol. 1999;86:623–632.<br />
75. Richter T, Bergmann R, Pietzsch J, et al. Effect of posture on regional<br />
pulmonary blood flow in rats as measured by PET. J Appl Physiol.<br />
2010;108:422–429.<br />
76. Aiton NR, Fox GF, Alexander J, et al. The influence of sleeping position<br />
on functional residual capacity and effective pulmonary blood flow in<br />
healthy neonates. Pediatr Pulmonol. 1996;22:342–347.<br />
77. Fox RE, Viscardi RM, Taciak VL, et al. Effect of position on pulmonary<br />
mechanics in healthy preterm newborn infants. J Perinatol. 1993;13:205–<br />
211.<br />
78. Pamphlett R, Raisanen J, Kum JS. Vertebral artery compression resulting<br />
from head movement: a possible cause of the sudden infant death<br />
syndrome. Pediatrics. 1999;103:460–468.<br />
79. Pamphlett R, Murray N. Vulnerability of the infant brain stem to<br />
ischemia: a possible cause of sudden infant death syndrome. J Child<br />
Neurol. 1996;11:181–184.<br />
<strong>80</strong>. Wang L-C, Liou J-T, Liu F-C, et al. Fatal ischemia stroke in a patient with<br />
an asymptomatic carotid artery occlusion after lumbar spine surgery—a<br />
case report. Acta Anaesthesiol Taiwan. 2004;42:179–182.<br />
81. Chu Y-C, Tsai S-K, Chan K-H, et al. Lateral medullary syndrome after<br />
prone position for general surgery. Anesth Analg. 2002;95:1451–1453.<br />
82. Luntley JB, Ross J, Pearce FJ. Lifting and handling of patients by<br />
anaesthetists. Anaesthesia. 1995;50:729–732.<br />
83. Lee LA, Newman NJ, Wagner TA, et al. Postoperative ischemic optic<br />
neuropathy. Spine. 2010;20:S105–S116.<br />
84. Williams EL, Hart WJ, Tempelhoff R. Postoperative ischemic optic<br />
neuropathy. Anesth Analg. 1995;<strong>80</strong>:1018–1029.<br />
85. Myers MA, Hamilton SR, Bogosian AJ, et al. Visual loss as a complication<br />
of spine surgery. A review of 37 cases. Spine. 1997;22:1325–1329.<br />
86. Sinha A, Agarwal A, Gaur A, et al. Oropharyngeal swelling and macro -<br />
glossia after cervical spine surgery in the prone position. J Neurosurg<br />
Anesthesiol. 2001;13:237–239.<br />
87. Morray JP, Geiduschek JM, Caplan RA, et al. A comparison of pediatric<br />
and adult anesthesia closed malpractice claims. Anesthesiology. 1993;<br />
78:461–467.<br />
88. Svendsen LB, Flink P, Wojdemann M, et al. Muscle oxygen saturation<br />
during surgery in the lithotomy position. Clin Physiol. 1997;17:433–438.<br />
89. Prabhakar H, Bithal PK, Ghosh I, et al. Pneumorrhachis presenting as<br />
quadriplegia following surgery in the prone position. Br J Anaesth. 2006;<br />
97:901–903.<br />
90. Rau C-S, Liang C-L, Lui C-C, et al. Quadriplegia in a patient who under -<br />
went posterior fossa surgery in the prone position. Case report. J<br />
Neurosurg. 2002;96:101–103.<br />
91. Valls PL, Naul LG, Kanter SL. Paraplegia after a routine lumbar lami -<br />
nectomy: report of a rare complication and successful management.<br />
Neurosurgery. 1990;27:638–640.<br />
92. Van Aken H, Scherer R, Lawin P. A rare intraoperative complication in a<br />
child with Von Recklinghausen’s neurofibromatosis. Anaesthesia. 1992;<br />
37:827–829.<br />
93. Gercek A, Konya D, Babayev R, et al. Delayed recovery from general<br />
anesthesia from intracranial tumor. Anesth Analg. 2007;104:235–236.<br />
94. Jericho BG, Skaria GP. Contact dermatitis after the use of the Prone<br />
Positioner. Anesth Analg. 2003;97:1706–1708.<br />
95. Pousman RM, Eilers WA 3rd, Johns B, et al. Irritant contact dermatitis<br />
after use of Bispectral Index sensor in prone position. Anesth Analg.<br />
2002;95:1337–1338.<br />
96. Rittoo DB, Morris P. Tracheal occlusion in the prone position in an<br />
intubated patient with Duchenne muscular dystrophy. Anaesthesia.<br />
1995;50:719–721.<br />
97. Kai Y, Yamaoka A, Irita K, et al. Transient tracheal obstruction during<br />
surgical correction of scoliosis in a patient with Marfan’s syndrome.<br />
Masui. 1995;44:868–873.<br />
98. Hans P, Demoitie J, Collignon L, et al. Acute bilateral submandibular<br />
swelling following surgery in prone position. Eur J Anaesthesiol. 2006;<br />
23:83–84.<br />
99. Ali AA, Breslin DS, Hardman HD, et al. Unusual presentation and<br />
complication of the prone position for spinal surgery. J Clin Anesth.<br />
2003;15:471–473.<br />
100. Yuen VMY, Chow BFM, Irwin MG. Severe hypotension and hepatic<br />
dysfunction in a patient undergoing scoliosis surgery in the prone<br />
position. Anaesth Intensive Care. 2005;33:393–399.<br />
101. Alexianu D, Skolnick ET, Pinto AC, et al, Severe hypotension in the<br />
prone position in a child with neurofibromatosis, scoliosis and pectus<br />
excavatum presenting for posterior spinal fusion. Anesth Analg. 2004;<br />
98:334–335.<br />
102. Teoh DCA, Williams DL. Adult Klippel–Feil syndrome: haemodynamic<br />
instability in the prone position and postoperative respiratory failure.<br />
Anaesth Intensive Care. 2007;35:124–127.<br />
103. Hiraga Y, Maruoka H, Yamamoto M, et al. Compression of the graft<br />
during the corrective surgery for scoliosis in a patient who has under -<br />
gone a Rastelli’s operation: a case study. Masui. 1992;41:1490–1493.<br />
104. Ziser A, Friedhoff RJ, Rose SH, et al. Prone position: visceral hypo -<br />
perfusion and rhabdomyolysis. Anesth Analg. 1996;82:412–415.<br />
105. Curtin WA, Lahoti OP, Fogarty EE, et al. Pancreatitis after alar-trans -<br />
verse fusion for spondylolisthesis. A case report. Clin Orthop. 1993;292:<br />
142–143.<br />
106. Meridy HW, Creighton RE, Humphreys RP. Complications during<br />
neurosurgery in the prone position in children. Can Anaesth Soc J. 1974;<br />
21:445–453.<br />
107. Mirski MA, Lele AV, Fitzsimmons L, et al. Vascular air emboli. Anes -<br />
thesiology. 2007;106:164–177.<br />
108. Tobias JD, Mencio GA, Atwood R, et al. Intraoperative cardiopulmonary<br />
resuscitation in the prone position. J Pediatr Surg. 1994;29:1537–1538.<br />
109. Reid JM, Appleton PJ. A case of ventricular fibrillation in the prone<br />
position during back stabilisation surgery in a boy with Duchenne’s<br />
muscular dystrophy. Anaesthesia. 1994;54:364–367.<br />
110. Moore EW, Davies MW. A slap on the back. Anaesthesia. 1999;54:308.<br />
111. Cattell E, Saravanan P, Chay S, et al. The defibrillator back paddle: use<br />
for treatment of arrhythmias during prone position ventilation.<br />
Anaesthesia. 2000;55:491–492.<br />
112. Miranda CC, Newton MC, Successful defibrillation in the prone<br />
position. Br J Anaesth. 2001;87:937–938.<br />
113. Walsh S, Bedi A, Miranda C. Successful defibrillation in the prone<br />
position. Br J Anaesth. 89:799–<strong>80</strong>0, 2002.<br />
114. Yamashita M, Chin I, Horigome H, et al. Sudden fatal cardiac arrest in<br />
a child with an unrecognized anterior mediastinal mass. Resuscitation.<br />
1990;19:175–177.<br />
115. Halliwill JR, Hewitt SA, Joyner MJ, et al. Effect of various lithotomy<br />
positions on lower-extremity blood pressure. Anesthesiology. 1998;89:<br />
1373–1376.<br />
116. Ryniak S, Brannstedt S, Blomqvist H. Effects of exaggerated lithotomy<br />
position on ventilation and hemodynamics during radical perineal<br />
prostatectomy. Scand J Urol Nephrol. 1998;32:200–203.<br />
117. Clarke AM, Stillwell S, Paterson ME, et al. Role of the surgical position<br />
in the development of postoperative low back pain. J Spinal Disord.<br />
1993;6:238–241.<br />
118. Biswas S, Gnanasekaran I, Ivatury RR, et al. Exaggerated lithotomy<br />
position-related rhabdomyolysis. Am Surg. 1997;63:361–364.<br />
119. Kubiak R, Wilcox DT, Spitz L, et al. Neurovascular morbidity from the<br />
lithotomy position. J Pediatr Surg. 1998;33:1<strong>80</strong>8–1810.<br />
120. Warner MA, Martin JT, Schroeder DR, et al. Lower-extremity motor<br />
neuropathy associated with surgery performed on patients in a lithotomy<br />
position. Anesthesiology. 1994;81:6–12.<br />
121. Malan T, McInode AK. Positioning the surgical patient. The Foundation<br />
Years. 2006;5:185–189.<br />
122. Batres F, Barclay DL. Sciatic nerve injury during gynecologic procedures<br />
using the lithotomy position. Obstet Gynecol. 1983;62(3 Suppl):92s–94s.<br />
123. Elton RJ, Howell RS. The sitting position in neurosurgical anaesthesia:<br />
a survey of British practice in 1991. Br J Anaesth. 1994;73:247–248.
CHAPTER <strong>80</strong> ■ Patient Positioning and Precautions During Anesthesia and Surgery 1361<br />
124. Schaffranietz L, Gunther L. The sitting position in neurosurgical opera -<br />
tions. Results of a survey. Anaesthesist. 1997;46:91–95.<br />
125. Meyer PG, Cuttaree H, Charron B, et al. Prevention of venous air<br />
embolism in paediatric neurosurgical procedures performed in the<br />
sitting position by combined use of MAST suit and PEEP. Br J Anaesth.<br />
1994;73:795–<strong>80</strong>0.<br />
126. Perkins-Pearson NAK, Marshall WK, Bedford RF. Atrial pressures in the<br />
seated position: implication of paradoxical air embolism. Anesthesiology.<br />
1982;57:493–497.<br />
127. Black S, Cucchiara RF, Nishimura RA. Parameters affecting occurrence<br />
of paradoxical air embolism. Anesthesiology. 1989;71:235–241.<br />
128. Seward JB, Hayes DL, Smith HC, et al. Platypnea-orthodeoxia: Clinical<br />
profile, diagnostic workup, management, and report of seven cases.<br />
Mayo Clin Proc. 1984;59:221–231.<br />
129. Don HF, Wahba WM, Craig DB. Airway closure, gas trapping, and the<br />
functional residual capacity during anesthesia. Anesthesiology. 1972;36:<br />
533–539.<br />
130. Danon J, Druz WS, Goldberg NB, et al. Function of the isolated paced<br />
diaphragm and the cervical accessory muscles in C1 quadriplegics. Am<br />
Rev Respir Dis. 1979;119:909–919.<br />
131. Smelt WL, de Lange JJ, Booij LH. Cardiorespiratory effects of the sitting<br />
position in neurosurgery. Acta Anaesthesiol Belg. 1988;3:223–231.<br />
132. Carlo WA, Beoglos A, Siner BS, et al. Neck and body position effects on<br />
pulmonary mechanics in infants. Pediatrics. 1989;84:670–674.<br />
133. Grady MS, Bedford RF, Park TS. Changes in superior sagittal sinus<br />
pressure in children with head elevation, jugular venous compression,<br />
and PEEP. J Neurosurg. 1986;65:199–202.<br />
134. Lodrini S, Montolivo M, Pluchino F, et al. Positive end-expiratory<br />
pressure in supine and sitting positions: its effects on intrathoracic and<br />
intracranial pressures. Neurosurgery. 1989;24:873–877.<br />
135. Saady A. Brachial plexus palsy after anaesthesia in the sitting position.<br />
Anaesthesia. 1981;36:194–195.<br />
136. Cucchiara RF, Nugent M, Seward JB, et al. Air embolism in upright<br />
neurosurgical patients: detection and localization by two-dimensional<br />
transesophageal echocardiography. Anesthesiology. 1984;60:353–355.<br />
137. Haisa T, Kondo T. Midcervical flexion myelopathy after posterior fossa<br />
surgery in the sitting position: case report. Neurosurgery. 1996;38:<br />
819–821.<br />
138. Nitta H, Yamashita J, Nomura M, et al. Cervical spinal cord infarction<br />
after surgery for a pineal region choriocarcinoma in the sitting position:<br />
case report. Neurosurgery. 1997;40:1082–1085.<br />
139. Delattre O, Thoreux P, Liverneaux P, et al. Spinal surgery and ophthalmic<br />
complications: a French survey with review of 17 cases. Ophthalmic<br />
complications after spinal surgery. J Spinal Disord Tech. 2007;20:<br />
302–307.<br />
140. Traon AP, Sigaudo D, Vasseur P, et al. Cardiovascular responses to<br />
orthostatic tests after a 42-day head-down bed-rest. Eur J Appl Physiol.<br />
1998;77:50–59.<br />
141. Ferretti G, Girardis M, Moia C, et al. Effects of prolonged bed rest on<br />
cardiovascular oxygen transport during submaximal exercise in humans.<br />
Eur J Appl Physiol. 1998;78:398–404.<br />
142. Rowland TW. Effect of prolonged inactivity on aerobic fitness of<br />
children. J Sports Med Phys Fitness. 1994;34:147–155.<br />
143. Suzuki Y, Murakami T, Haruna Y, et al. Effects of 10 and 20 days bed<br />
rest on leg muscle mass and strength in young subjects. Acta Physiol<br />
Scand Suppl. 1994;616:5–18.<br />
144. Ferrando AA, Lane HW, Stuart CA, et al. Prolonged bed rest decreases<br />
skeletal muscle and whole body protein synthesis. Am J Physiol.<br />
1996;270:E627–E633.