Physician-assisted dying for children is conceivable for most Dutch pediatricians, irrespective of the patient’s age or competence to decide
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Physician</strong>-<strong>ass<strong>is</strong>ted</strong> <strong>dying</strong> <strong>f<strong>or</strong></strong> <strong>children</strong><br />
Bolt et al.<br />
analys<strong>is</strong>. Th<strong>is</strong> approach was chosen so that compar<strong>is</strong>ons<br />
could be made between different <strong>age</strong> groups and between<br />
requests by a patient and a parent <strong>or</strong> parents, both<br />
separately and in combination. F<strong>or</strong> instance, <strong>the</strong> two<br />
categ<strong>or</strong>ies had per<strong>f<strong>or</strong></strong>med PAD on <strong>the</strong> request <strong>of</strong> a patient<br />
<strong>age</strong>d one <strong>to</strong> 11 and had per<strong>f<strong>or</strong></strong>med PAD on <strong>the</strong> request <strong>of</strong><br />
<strong>the</strong> parents <strong>of</strong> a patient <strong>age</strong>d one <strong>to</strong> 11 were combined as<br />
had per<strong>f<strong>or</strong></strong>med PAD on request <strong>f<strong>or</strong></strong> a patient <strong>age</strong>d one <strong>to</strong> 11.<br />
Combined categ<strong>or</strong>ies are indicated in <strong>the</strong> tables.<br />
The first two interviews were d<strong>is</strong>cussed by three auth<strong>or</strong>s<br />
(EF, EB and RP) and some adaptations were made <strong>to</strong> <strong>the</strong><br />
<strong>to</strong>pic l<strong>is</strong>t. The Qualitative Analys<strong>is</strong> Guide <strong>of</strong> Leuven method<br />
was used <strong>f<strong>or</strong></strong> <strong>the</strong> analys<strong>is</strong> (19). First, two auth<strong>or</strong>s (EF and<br />
EB) read <strong>the</strong> interviews and made narrative interview<br />
rep<strong>or</strong>ts. These were compared and d<strong>is</strong>cussed and a conceptual<br />
summary was made <strong>of</strong> each interview. In <strong>the</strong> second<br />
phase, <strong>the</strong> conceptual interview summaries were compared<br />
by <strong>the</strong> same two auth<strong>or</strong>s and used as <strong>the</strong> bas<strong>is</strong> <strong>f<strong>or</strong></strong> <strong>the</strong> coding<br />
tree. The codes were structured around <strong>the</strong> research<br />
questions. One <strong>of</strong> <strong>the</strong> auth<strong>or</strong>s (EB) reread and coded <strong>the</strong><br />
interviews. There was a high level <strong>of</strong> consensus among <strong>the</strong><br />
interviewees, and no new codes emerged after five<br />
interviews. The data were analysed manually.<br />
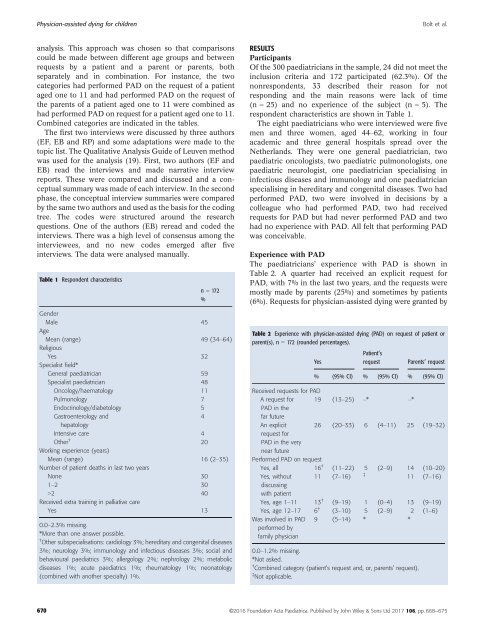
Table 1 Respondent character<strong>is</strong>tics<br />
n = 172<br />
%<br />
Gender<br />
Male 45<br />
Age<br />
Mean (range) 49 (34–64)<br />
Religious<br />
Yes 32<br />
Special<strong>is</strong>t field*<br />
General paediatrician 59<br />
Special<strong>is</strong>t paediatrician 48<br />
Oncology/haema<strong>to</strong>logy 11<br />
Pulmonology 7<br />
Endocrinology/diabe<strong>to</strong>logy 5<br />
Gastroenterology and<br />
4<br />
hepa<strong>to</strong>logy<br />
Intensive care 4<br />
O<strong>the</strong>r † 20<br />
W<strong>or</strong>king experience (years)<br />
Mean (range) 16 (2–35)<br />
Number <strong>of</strong> patient deaths in last two years<br />
None 30<br />
1–2 30<br />
>2 40<br />
Received extra training in palliative care<br />
Yes 13<br />
0.0–2.3% m<strong>is</strong>sing.<br />
*M<strong>or</strong>e than one answer possible.<br />
† O<strong>the</strong>r subspecial<strong>is</strong>ations: cardiology 3%; hereditary and congenital d<strong>is</strong>eases<br />
3%; neurology 3%; immunology and infectious d<strong>is</strong>eases 3%; social and<br />
behavioural paediatrics 3%; allergology 2%; nephrology 2%; metabolic<br />
d<strong>is</strong>eases 1%; acute paediatrics 1%; rheuma<strong>to</strong>logy 1%; neona<strong>to</strong>logy<br />
(combined with ano<strong>the</strong>r specialty) 1%.<br />
RESULTS<br />
Participants<br />
Of <strong>the</strong> 300 paediatricians in <strong>the</strong> sample, 24 did not meet <strong>the</strong><br />
inclusion criteria and 172 participated (62.3%). Of <strong>the</strong><br />
nonrespondents, 33 described <strong>the</strong>ir reason <strong>f<strong>or</strong></strong> not<br />
responding and <strong>the</strong> main reasons were lack <strong>of</strong> time<br />
(n = 25) and no experience <strong>of</strong> <strong>the</strong> subject (n = 5). The<br />
respondent character<strong>is</strong>tics are shown in Table 1.<br />
The eight paediatricians who were interviewed were five<br />
men and three women, <strong>age</strong>d 44–62, w<strong>or</strong>king in four<br />
academic and three general hospitals spread over <strong>the</strong><br />
Ne<strong>the</strong>rlands. They were one general paediatrician, two<br />
paediatric oncolog<strong>is</strong>ts, two paediatric pulmonolog<strong>is</strong>ts, one<br />
paediatric neurolog<strong>is</strong>t, one paediatrician special<strong>is</strong>ing in<br />
infectious d<strong>is</strong>eases and immunology and one paediatrician<br />
special<strong>is</strong>ing in hereditary and congenital d<strong>is</strong>eases. Two had<br />
per<strong>f<strong>or</strong></strong>med PAD, two were involved in dec<strong>is</strong>ions by a<br />
colleague who had per<strong>f<strong>or</strong></strong>med PAD, two had received<br />
requests <strong>f<strong>or</strong></strong> PAD but had never per<strong>f<strong>or</strong></strong>med PAD and two<br />
had no experience with PAD. All felt that per<strong>f<strong>or</strong></strong>ming PAD<br />
was <strong>conceivable</strong>.<br />
Experience with PAD<br />
The paediatricians’ experience with PAD <strong>is</strong> shown in<br />
Table 2. A quarter had received an explicit request <strong>f<strong>or</strong></strong><br />
PAD, with 7% in <strong>the</strong> last two years, and <strong>the</strong> requests were<br />
<strong>most</strong>ly made by parents (25%) and sometimes by patients<br />
(6%). Requests <strong>f<strong>or</strong></strong> physician-<strong>ass<strong>is</strong>ted</strong> <strong>dying</strong> were granted by<br />
Table 2 Experience with physician-<strong>ass<strong>is</strong>ted</strong> <strong>dying</strong> (PAD) on request <strong>of</strong> patient <strong>or</strong><br />
parent(s), n = 172 (rounded percent<strong>age</strong>s).<br />
Yes<br />
Patient’s<br />
request<br />
Parents’ request<br />
% (95% CI) % (95% CI) % (95% CI)<br />
Received requests <strong>f<strong>or</strong></strong> PAD<br />
A request <strong>f<strong>or</strong></strong> 19 (13–25) –* –*<br />
PAD in <strong>the</strong><br />
far future<br />
An explicit 26 (20–33) 6 (4–11) 25 (19–32)<br />
request <strong>f<strong>or</strong></strong><br />
PAD in <strong>the</strong> very<br />
near future<br />
Per<strong>f<strong>or</strong></strong>med PAD on request<br />
Yes, all 16 † (11–22) 5 (2–9) 14 (10–20)<br />
Yes, without 11 (7–16)<br />
‡<br />
11 (7–16)<br />
d<strong>is</strong>cussing<br />
with patient<br />
Yes, <strong>age</strong> 1–11 13 † (9–19) 1 (0–4) 13 (9–19)<br />
Yes, <strong>age</strong> 12–17 6 † (3–10) 5 (2–9) 2 (1–6)<br />
Was involved in PAD<br />
per<strong>f<strong>or</strong></strong>med by<br />
family physician<br />
9 (5–14) * *<br />
0.0–1.2% m<strong>is</strong>sing.<br />
*Not asked.<br />
† Combined categ<strong>or</strong>y (<strong>patient’s</strong> request and, <strong>or</strong>, parents’ request).<br />
‡ Not applicable.<br />
670 ©2016 Foundation Acta Pædiatrica. Publ<strong>is</strong>hed by John Wiley & Sons Ltd 2017 106, pp. 668–675