New Hampshire - June 2020
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s<br />
Year of the Nurse <strong>2020</strong><br />
Official <strong>New</strong>sletter of <strong>New</strong> <strong>Hampshire</strong> Nurses Association<br />
Quarterly publication direct mailed to approximately 1,250 Registered Nurses and LPNs and delivered<br />
electronically via email to 16,500 Registered Nurses and LPNs in <strong>New</strong> <strong>Hampshire</strong>.<br />
<strong>June</strong> <strong>2020</strong> | Vol. 44 No. 3<br />
www.NHNurses.org<br />
Florence Nightingale (1820-1910)<br />
<strong>2020</strong> STUDENT NURSE<br />
OF THE YEAR<br />
The student nurse of the year award<br />
is given to a student nurse in a prelicensure<br />
entry program who embodies<br />
the finest qualities of nursing. Unable to<br />
celebrate nursing students in the state<br />
of <strong>New</strong> <strong>Hampshire</strong> with our Annual<br />
Student Nursing Conference in the midst<br />
of the COVID-19 closure, NHNA felt it<br />
was important to recognize excellence.<br />
Graduating students were unable to<br />
celebrate traditional graduations but<br />
will soon be on the front lines caring<br />
for <strong>New</strong> <strong>Hampshire</strong> citizens and<br />
communities.<br />
The Student Nurse Award was bestowed<br />
virtually. Five deserving students were<br />
nominated and judged by the NHNA<br />
Commission on Nursing Practice based<br />
on qualities include caring, professionalism, advocacy,<br />
leadership and involvement. <strong>2020</strong> nominees were:<br />
Shadane Davis, St. Joseph School of Nursing<br />
Devon Fortier, University of <strong>New</strong> <strong>Hampshire</strong><br />
Emily Galasyn, Rivier University<br />
Laura Howard, University of <strong>New</strong> <strong>Hampshire</strong><br />
current resident or<br />
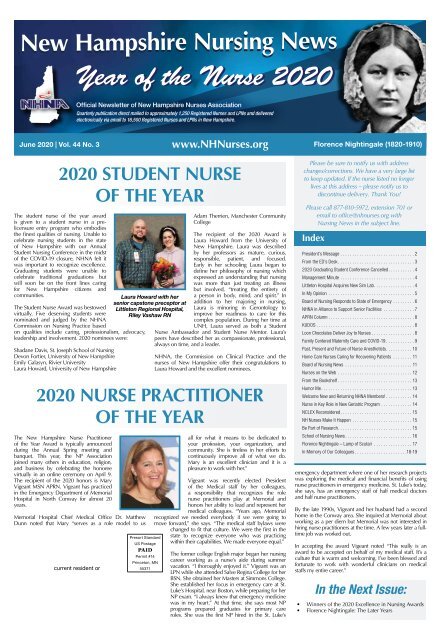
Laura Howard with her<br />
senior capstone preceptor at<br />
Littleton Regional Hospital,<br />
Riley Vashaw RN<br />
Presort Standard<br />
US Postage<br />
PAID<br />
Permit #14<br />
Princeton, MN<br />
55371<br />
Adam Therrien, Manchester Community<br />
College<br />
The recipient of the <strong>2020</strong> Award is<br />
Laura Howard from the University of<br />
<strong>New</strong> <strong>Hampshire</strong>. Laura was described<br />
by her professors as mature, curious,<br />
responsible, patient, and focused.<br />
Early in her schooling Laura began to<br />
define her philosophy of nursing which<br />
expressed an understanding that nursing<br />
was more than just treating an illness<br />
but involved, “treating the entirety of<br />
a person in body, mind, and spirit.” In<br />
addition to her majoring in nursing,<br />
Laura is minoring in Gerontology to<br />
improve her readiness to care for this<br />
complex population. During her time at<br />
UNH, Laura served as both a Student<br />
Nurse Ambassador and Student Nurse Mentor. Laura’s<br />
peers have described her as compassionate, professional,<br />
always on time, and a leader.<br />
NHNA, the Commission on Clinical Practice and the<br />
nurses of <strong>New</strong> <strong>Hampshire</strong> offer their congratulations to<br />
Laura Howard and the excellent nominees.<br />
<strong>2020</strong> NURSE PRACTITIONER<br />
OF THE YEAR<br />
The <strong>New</strong> <strong>Hampshire</strong> Nurse Practitioner<br />
of the Year Award is typically announced<br />
during the Annual Spring meeting and<br />
banquet. This year, the NP Association<br />
joined many others in education, religion,<br />
and business by celebrating the honoree<br />
virtually in an online ceremony on April 9.<br />
The recipient of the <strong>2020</strong> honors is Mary<br />
Vigeant MSN APRN. Vigeant has practiced<br />
in the Emergency Department of Memorial<br />
Hospital in North Conway for almost 20<br />
years.<br />
Memorial Hospital Chief Medical Office Dr. Matthew<br />
Dunn noted that Mary “serves as a role model to us<br />
all for what it means to be dedicated to<br />
your profession, your organization, and<br />
community. She is tireless in her efforts to<br />
continuously improve all of what we do.<br />
Mary is an excellent clinician and it is a<br />
pleasure to work with her.”<br />
Vigeant was recently elected President<br />
of the Medical staff by her colleagues,<br />
a responsibility that recognizes the role<br />
nurse practitioners play at Memorial and<br />
honors her ability to lead and represent her<br />
medical colleagues. “Years ago, Memorial<br />
recognized we needed everybody if we were going to<br />
move forward,” she says. “The medical staff bylaws were<br />
changed to fit that culture. We were the first in the<br />
state to recognize everyone who was practicing<br />
within their capabilities. We made everyone equal.”<br />
The former college English major began her nursing<br />
career working as a nurse’s aide during summer<br />
vacation. “I thoroughly enjoyed it.” Vigeant was an<br />
LPN while she attended Salve Regina College for her<br />
BSN. She obtained her Masters at Simmons College.<br />
She established her focus in emergency care at St.<br />
Luke’s Hospital, near Boston, while preparing for her<br />
NP exam. “I always knew that emergency medicine<br />
was in my heart.” At that time, she says most NP<br />
programs prepared graduates for primary care<br />
roles. She was the first NP hired in the St. Luke’s<br />
Please be sure to notify us with address<br />
changes/corrections. We have a very large list<br />
to keep updated. If the nurse listed no longer<br />
lives at this address – please notify us to<br />
discontinue delivery. Thank You!<br />
Please call 877-810-5972, extension 701 or<br />
email to office@nhnurses.org with<br />
Nursing <strong>New</strong>s in the subject line.<br />
Index<br />
President’s Message............................... 2<br />
From the ED’s Desk................................ 3<br />
<strong>2020</strong> Graduating Student Conference Cancelled........... 4<br />
Management Minute............................... 4<br />
Littleton Hospital Acquires <strong>New</strong> Sim Lab................. 4<br />
In My Opinion .................................... 5<br />
Board of Nursing Responds to State of Emergency......... 6<br />
NHNA in Alliance to Support Senior Facilities ............. 7<br />
APRN Column.................................... 8<br />
KUDOS......................................... 8<br />
Loon Chocolates Deliver Joy to Nurses.................. 8<br />
Family Centered Maternity Care and COVID-19............ 9<br />
Past, Present and Future of Nurse Anesthetists............10<br />
Home Care Nurses Caring for Recovering Patients .........11<br />
Board of Nursing <strong>New</strong>s .............................11<br />
Nurses on the Web ................................12<br />
From the Bookshelf................................13<br />
Humor Me.......................................13<br />
Welcome <strong>New</strong> and Returning NHNA Members!............14<br />
Nurse in Key Role in <strong>New</strong> Geriatric Program..............14<br />
NCLEX Reconsidered...............................15<br />
NH Nurses Make It Happen ..........................15<br />
Be Part of Research................................15<br />
School of Nursing <strong>New</strong>s.............................16<br />
Florence Nightingale – Lamp of Scutari .................17<br />
In Memory of Our Colleagues...................... 18-19<br />
emergency department where one of her research projects<br />
was exploring the medical and financial benefits of using<br />
nurse practitioners in emergency medicine. St. Luke’s today,<br />
she says, has an emergency staff of half medical doctors<br />
and half nurse practitioners.<br />
By the late 1990s, Vigeant and her husband had a second<br />
home in the Conway area. She inquired at Memorial about<br />
working as a per diem but Memorial was not interested in<br />
hiring nurse practitioners at the time. A few years later a fulltime<br />
job was worked out.<br />
In accepting the award Vigeant noted “This really is an<br />
award to be accepted on behalf of my medical staff. It’s a<br />
culture that is warm and welcoming. I’ve been blessed and<br />
fortunate to work with wonderful clinicians on medical<br />
staffs my entire career.”<br />
In the Next Issue:<br />
• Winners of the <strong>2020</strong> Excellence in Nursing Awards<br />
• Florence Nightingale: The Later Years
Page 2 • <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s <strong>June</strong>, July, August <strong>2020</strong><br />
Guidelines for Submissions to NH Nursing <strong>New</strong>s<br />
NH Nursing <strong>New</strong>s (NHNN) is the official publication<br />
of the NH Nurses’ Association (NHNA), published<br />
quarterly – and available in PDF format at our website:<br />
www.nhnurses.org. Views expressed are solely those<br />
of the guest authors or persons quoted and do not<br />
necessarily reflect NHNA views or those of the publisher,<br />
Arthur L. Davis Publishing Agency, Inc. NHNA welcomes<br />
submission of nursing and health related news items,<br />
original articles, research abstracts, and other pertinent<br />
contributions. We encourage short summaries and brief<br />
abstracts as well as lengthier reports and original works.<br />
An “article for reprint” may be considered if accompanied<br />
by written permission from the author or publisher.<br />
Authors do not need to be NHNA members.*<br />
Manuscript Format and Submission:<br />
Articles should be submitted as double spaced WORD<br />
documents (.doc format vs. .docx, please) in 12 pt. font<br />
without embedded photos. Photos should be attached<br />
separately in JPG format and include captions.<br />
Submissions should include the article’s title plus author’s<br />
name, credentials, organization / employer represented,<br />
and contact information. Authors should state any<br />
potential conflict of interest and identify any applicable<br />
Nurses, once again, are<br />
asserting their place in<br />
history. The past weeks<br />
have challenged you and<br />
yet, you have remained<br />
strong and dedicated,<br />
committed to facing the<br />
COVID-19 pandemic<br />
head-on and with sleeves<br />
rolled up. In my role as<br />
NHNA president, I’ve had<br />
the privilege of seeing the<br />
global <strong>New</strong> <strong>Hampshire</strong><br />
nursing response to the<br />
commercial affiliation. Email as<br />
attachments to office@nhnurses.<br />
org with NN Submission in the<br />
subject line.<br />
Publication Selection and<br />
Rights:<br />
Articles will be selected for<br />
publication based on the<br />
topic of interest, adherence to<br />
publication deadlines, quality<br />
of writing and peer review.<br />
*When there is space for<br />
one article and two of equal interest<br />
are under review, preference will be given to NHNA<br />
members. NHNA reserves the right to edit articles to<br />
meet style and space limitations. Publication and reprint<br />
rights are also reserved by NHNA. Feel free to call us any<br />
additional questions at 877-810-5972.<br />
Advertising:<br />
Product, program, promotional or service<br />
announcements are usually considered advertisements<br />
vs. news. To place an ad, contact: Arthur L. Davis<br />
Publishing Agency, Inc. Email sales@aldpub.com or call<br />
800-626-4081. Ad sales fund publication and mailing of<br />
NH Nursing <strong>New</strong>s and are not paid to NHNA.<br />
PRESIDENT’S MESSAGE<br />
Janice Deziel<br />
call to duty and the advocacy of patients and peers.<br />
Here is but a snapshot of what the NHNA has seen<br />
and heard about what nurses are doing throughout<br />
the state:<br />
• Working on the frontlines in Emergency<br />
Departments, ICUs, and COVID-19 dedicated<br />
units, accepting the risks to themselves and<br />
their families.<br />
Faculty Positions in Nursing<br />
School of Nursing & Health Sciences<br />
We celebrate diverse undergraduate and graduate academic<br />
programs, outstanding faculty and a strong community partnership<br />
with Dartmouth-Hitchcock Health.<br />
We are seeking multiple innovative, energetic nurse educators<br />
to teach in both the classroom and clinical setting. Applications<br />
for tenure-track and non-tenure track, full-time faculty positions<br />
beginning September 1, <strong>2020</strong> are now being requested.<br />
Qualifications:<br />
1. A doctoral degree is preferred; a Master of Science in Nursing<br />
is required.<br />
2. Demonstrate and possess a strong record of collegiate teaching.<br />
3. A philosophy of education consistent with Colby-Sawyer’s<br />
programs and mission is required.<br />
4. Expert-clinician who has a strong desire for an academic<br />
appointment focused on advancing knowledge through<br />
integrating teaching, clinical practice, scholarship and service.<br />
5. Strong interest in mentoring and advising undergraduate and<br />
graduate students.<br />
To Apply<br />
To apply, submit a current CV, letter of application, statement<br />
of teaching philosophy, sample syllabi if available, and names<br />
and telephone numbers/e-mail addresses of three references to<br />
CSCjobs@colby-sawyer.edu.<br />
• Taking care of and protecting the most<br />
vulnerable in our population: the elderly and<br />
those with special needs.<br />
• Signing up, in large numbers, for volunteer<br />
opportunities.<br />
• Coming out of retirement to contribute to the<br />
need for nursing expertise.<br />
• Thanking first responders, recognizing that<br />
healthcare truly is a team sport.<br />
• Cross-training, learning new skills to take on<br />
roles needed to address this novel pandemic.<br />
• Innovating to provide much needed supplies.<br />
• Supporting one another, keeping each other<br />
strong.<br />
Witnessing this level of dedication has been<br />
awe-inspiring and I thank you for all that you are<br />
doing. Information regarding the NHNA activities<br />
of the past several weeks is readily available on<br />
the website. There is a lot behind the scenes<br />
that the NHNA is doing to advocate for the<br />
nursing profession. Please read the Executive<br />
Director’s column for all the details, activities and<br />
accomplishments.<br />
On a national level, the ANA and Johnson &<br />
Johnson created a series of podcasts on the<br />
nursing profession for <strong>2020</strong>, the Year of the Nurse<br />
called See You Now. They have since paused their<br />
regularly scheduled programming to produce and<br />
broadcast stories from nurses serving in various<br />
roles during the pandemic. Storytelling conveys<br />
important information, concepts, and cultural mores<br />
in a way that no written word can. The stories in<br />
these podcasts will leave you feeling inspired,<br />
humbled, and proud. I encourage you to listen –<br />
they are brief yet powerful.<br />
As difficult as the past several weeks have been,<br />
never have I seen greater respect for the nursing<br />
profession. The collective power that you wield has<br />
consistently been used wisely and for the greater<br />
good of all people and our world is responding in<br />
kind, turning to you for care and guidance. When<br />
called upon during the most challenging of times,<br />
you have answered without hesitation. You are<br />
honorable people with a solid foundation of ethics<br />
and a love of mankind that serves as your moral<br />
compass.<br />
With gratitude for the privilege of being a nurse<br />
among you,<br />
Janice Deziel<br />
President, NHNA<br />
<strong>New</strong> <strong>Hampshire</strong><br />
NURSING NEWS<br />
Vol. 44 No. 3<br />
Official publication of the <strong>New</strong> <strong>Hampshire</strong> Nurses’<br />
Association (NHNA), a constituent member of the<br />
American Nurses Association. Published quarterly<br />
every December, March, <strong>June</strong>, and September. Library<br />
subscription rate is $30. ISSN 0029-6538<br />
Editorial Offices<br />
<strong>New</strong> <strong>Hampshire</strong> Nurses Association, 25 Hall St., Unit<br />
1E, Concord, NH 03301. Ph (877) 810-5972, E-mail<br />
office@NHNurses.org<br />
Editor: Susan Fetzer, RN, PhD<br />
NHNA Staff<br />
Joan Widmer, RN, Nurse Executive Director<br />
Paula MacKinnon RN, Executive Assistant/<br />
Communications Specialist<br />
Beth Dow RN, Event Coordinator<br />
NURSING NEWS is indexed in the Cumulative Nursing<br />
Index to Nursing and Allied Health Literature (CINAHL)<br />
and International Nursing Index.<br />
For advertising rates and information, please<br />
contact Arthur L. Davis Publishing Agency, Inc.,<br />
517 Washington Street, PO Box 216, Cedar Falls,<br />
Iowa 50613, (800) 626-4081, sales@aldpub.com.<br />
NHNA and the Arthur L. Davis Publishing Agency,<br />
Inc. reserve the right to reject any advertisement.<br />
Responsibility for errors in advertising is limited to<br />
corrections in the next issue or refund of price of<br />
advertisement.<br />
Acceptance of advertising does not imply<br />
endorsement or approval by the <strong>New</strong> <strong>Hampshire</strong><br />
Nurses Association of products advertised, the<br />
advertisers, or the claims made. Rejection of an<br />
advertisement does not imply a product offered for<br />
advertising is without merit, or that the manufacturer<br />
lacks integrity, or that this association disapproves<br />
of the product or its use. NHNA and the Arthur L.<br />
Davis Publishing Agency, Inc. shall not be held liable<br />
for any consequences resulting from purchase or use<br />
of an advertiser’s product. Articles appearing in this<br />
publication express the opinions of the authors; they<br />
do not necessarily reflect views of the staff, board,<br />
or membership of NHNA or those of the national or<br />
local associations.<br />
VISION STATEMENT<br />
Empower <strong>New</strong> <strong>Hampshire</strong> nurses as leaders in<br />
advancing the profession of nursing and the health of<br />
<strong>New</strong> <strong>Hampshire</strong>.<br />
MISSION STATEMENT<br />
NHNA, as a constituent member of the American<br />
Nurses Association, exists to promote the practice,<br />
development and well being of NH nurses through<br />
education, empowerment and healthcare advocacy.<br />
Adopted 10-20-2010.<br />
Do you have a news item<br />
to share with the nurses of<br />
<strong>New</strong> <strong>Hampshire</strong>?<br />
Deadline for the next issue of Nursing <strong>New</strong>s is<br />
August 1, <strong>2020</strong><br />
Send all contributions to office@nhna.org with<br />
NHNN in the Subject.
<strong>June</strong>, July, August <strong>2020</strong> <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s • Page 3<br />
FROM THE ED’S DESK<br />
The world has changed dramatically. How we work, how we<br />
learn, how we live has changed markedly over the past three<br />
months. And the work of <strong>New</strong> <strong>Hampshire</strong> Nurses Association<br />
(NHNA) has changed as well.<br />
NHNA’s single largest fund raising event of the year, the<br />
Graduating Student Conference & Career Fair, was cancelled<br />
in late March due to campus closures and social distancing<br />
directives. Meetings of the NHNA Board of Directors and the<br />
various Commissions were cancelled between mid-March and<br />
mid-April and then transitioned to teleconferencing platforms<br />
as the new norm is established.<br />
Joan Widmer<br />
The day-to-day work of the NHNA staff focuses on addressing<br />
issues and concerns related to the COVID-19 pandemic. The number of daily calls to the<br />
NHNA office and email outreaches through the Contact Us on the NHNA website has<br />
increased significantly. Nurses call with concerns regarding personal protection equipment<br />
and spreading the virus to their families; retired nurses seek ways to volunteer to help and<br />
media outlets contact NHNA with questions.<br />
During March and April you may have seen or heard NHNA representing the nurses of<br />
<strong>New</strong> <strong>Hampshire</strong>. NHNA representatives were interviewed and featured on WMUR (March<br />
24, March 25), NHPR (April 3, April 9, April 27), Valley <strong>New</strong>s (March 28), Union Leader<br />
(April 2, April 13) and the Keene Sentinel (April 4). These represent more media outreaches<br />
that I’ve encountered during my four year tenure with NHNA!<br />
NHNA has developed a series of webpages to keep <strong>New</strong> <strong>Hampshire</strong> nurses informed<br />
about the COVID-19 pandemic with vetted resources from the <strong>New</strong> <strong>Hampshire</strong><br />
Department of Health and Human Services, the Centers for Disease Control & Prevention<br />
(CDC) and the American Nurses Association (ANA). NHNA developed guidance for nurses<br />
on steps to take after their shift to minimize risks associated with transmitting COVID-19<br />
which is posted on the NHNA website.<br />
As the weeks wore on, with no signs of the abatement of the healthcare crisis, we<br />
developed a webpage of self-care resources to help nurses cope with the prolonged stress<br />
of caring for patients during this crisis and coping with the major societal changes impacting<br />
their daily lives. As nurses started to experience reduced hours, reduced pay, furloughs<br />
and/or layoffs, we developed a webpage featuring resources to help nurses cope with the<br />
financial stressors necessitated by COVID-19 healthcare crisis.<br />
NHNA created a 30-second public service announcement regarding social distancing and<br />
handwashing.<br />
“You trusted us when your baby was born. You trusted us when your loved one was<br />
sick. You trusted us when your child was at school. Please trust us now. We ask you to<br />
please stay at home. We ask you to practice social distancing and stay at least six feet<br />
apart. We ask you to please wash your hands. We ask you this to protect the vulnerable.<br />
Trust <strong>New</strong> <strong>Hampshire</strong> nurses to help us through this difficult time.”<br />
We sought and received the support of the <strong>New</strong> <strong>Hampshire</strong> Association of Nurse<br />
Anesthetists, the <strong>New</strong> <strong>Hampshire</strong> Nurse Practitioner Association, the <strong>New</strong> <strong>Hampshire</strong><br />
chapter of the American Association of Women’s Health and Neonatal Nurses, Southern<br />
<strong>New</strong> <strong>Hampshire</strong> Oncology Nurses and the <strong>New</strong> <strong>Hampshire</strong> School Nurses Association<br />
for this Public Service Announcement (PSA). The PSA aired ten times on WMUR (between<br />
April 10 and April 17). It has over 3,100 views on YouTube (https://www.youtube.com/<br />
watch?v=sAbovjqsZ7c).<br />
After receiving numerous calls from nurses seeking to volunteer, we asked DHHS if they<br />
would find a list of potential volunteers helpful. We were encouraged to proceed so we<br />
sent a survey to our members and followers list serve (about 10,000 names) and received<br />
over 600 responses in a week. This information was shared with DHHS and with 10<br />
nursing organizations around the state, as well as the Nashua Department of Public Health.<br />
When state Senator Tom Sherman reached out looking for volunteers to help with a<br />
project emanating from MIT to provide a daily check-in with <strong>New</strong> <strong>Hampshire</strong> nursing<br />
homes, we reached out to these potential volunteers again. Over 120 potential volunteers<br />
responded to this request and the Covid Alliance Senior Support Team was founded<br />
(https://covidalliance.com/sst). Past President of NHNA, Dr. Judy A. Joy, assumed the role of<br />
Statewide Volunteer Coordinator. Paula MacKinnon developed the online data collection<br />
tool and set-up a website for the project. Traci Fairbanks, Carla Smith and Susan Smith are<br />
a few of the volunteers serving as Regional Liaison Coordinators.<br />
When the Red Cross reached out seeking volunteers to help with their blood drives, we<br />
sent a follow up email to these 600 survey respondents sharing information regarding how<br />
to volunteer with the Red Cross.<br />
NHNA has responded to numerous outreaches from <strong>New</strong> <strong>Hampshire</strong>’s Congressional<br />
delegation, including Senator Jeanne Shaheen, Congresswoman Annie Kuster and<br />
Congressman Chris Pappas. We worked with Senator Shaheen’s office to understand the<br />
issues of fingerprinting to register to sit for NCLEX and how to address the closure of the<br />
state police office after the stay at home order. The National Council of State Boards of<br />
Nursing (NCSBN), which requires an FBI background check to register for NCLEX, issued a<br />
waiver for this requirement during the current healthcare crisis.<br />
We spoke with Congresswomen Kuster regarding the issue of hazard pay for frontline<br />
workers, particularly nursing staff working in long term care. Congresswoman Kuster<br />
indicated she would look into this and shortly after this discussion, Governor Sununu<br />
announced his program for a $300 weekly stipend for health care workers in Medicaid<br />
approved long term care facilities. The Congress is also considering additional legislation,<br />
the Heroes Act, to support essential, frontline workers. We have regularly touched base<br />
with Congressman Pappas’s office regarding the ongoing need for PPE.<br />
We have worked with the Board of Nursing and the Office of Professional Licensure and<br />
Occupations to address emergent needs related to the COVID-19 pandemic. We discussed<br />
issues related to streamlining re-entry into licensure for nurses with retired and lapsed<br />
licensees. We discussed the transition of senior nursing students through the licensure<br />
process, and encouraging nursing students to seek their LNA license for work in long term<br />
care facilities. Nursing students working as LNAs will help ease the dangerous staffing<br />
shortages occurring when COVID-19 infections arise in a facility, while giving the students<br />
increased experience providing patient care. We worked with a group of stakeholders to<br />
develop the Temporary Health Partner role, an unlicensed care aide to work in long term<br />
care in nursing teams with license nursing assistants (LNA), to help provide activities of<br />
daily living care.<br />
All of us at NHNA are working to support you, our members, during this challenging time.<br />
We are all in this together and together we are strong. Together we have a voice.<br />
Visit nursingALD.com today!<br />
Search job listings<br />
in all 50 states, and filter by location and credentials.<br />
Browse our online database<br />
of articles and content.<br />
Find events<br />
for nursing professionals in your area.<br />
Your always-on resource for<br />
nursing jobs, research, and events.
Page 4 • <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s <strong>June</strong>, July, August <strong>2020</strong><br />
<strong>2020</strong> GRADUATING STUDENT<br />
CONFERENCE CANCELLED<br />
Graduating Student<br />
Conference & Career Fair<br />
Co-Sponsor:<br />
Southern <strong>New</strong> <strong>Hampshire</strong> University<br />
Gold Sponsors<br />
Dartmouth-Hitchcock<br />
Encompass Health<br />
Granite State College<br />
Southern <strong>New</strong> <strong>Hampshire</strong> Health<br />
Wentworth-Douglass Hospital<br />
Silver Sponsors<br />
Cheshire Medical Center<br />
Concord Hospital<br />
North Country Health<br />
NSO<br />
River Woods<br />
VNA Health Systems of No <strong>New</strong> England<br />
Exhibitors<br />
Brattleboro Retreat<br />
Catholic Medical Center<br />
Chamberlain University<br />
Elliot Hospital<br />
Franklin VNA<br />
Genesis<br />
Littleton Regional Hospital<br />
LRGHealthcare<br />
<strong>New</strong> <strong>Hampshire</strong> Hospital<br />
<strong>New</strong> <strong>Hampshire</strong> Veterans Home<br />
Northern Light<br />
Rivier University<br />
Saint Joseph College of Maine<br />
Speare Memorial Hospital<br />
United States Army<br />
University of <strong>New</strong> <strong>Hampshire</strong><br />
University of Rhode Island<br />
University of Vermont Medical Ctr.<br />
Western Governor’s University<br />
Everyone has been touched in many ways by the<br />
COVID-19 pandemic, but the Class of <strong>2020</strong> has been<br />
particularly challenged. Both from the aspects of<br />
completing the academic requirements remotely to<br />
enable them to graduate, and from the loss of all the<br />
traditional programs that help graduating students<br />
celebrate their transition from student to a working<br />
member of society. Each year the <strong>New</strong> <strong>Hampshire</strong><br />
Nurses Association (NHNA) hosts the Graduating<br />
Student Conference and Career Fair for nursing students<br />
across the state who are in the final year of their nursing<br />
program. This year’s Conference was scheduled to be<br />
held on March 29th on the campus of Southern <strong>New</strong><br />
<strong>Hampshire</strong> University, our co-host for this wonderful<br />
event. Sadly, the event was cancelled and the planned<br />
site for this Conference was reconfigured into one of<br />
thirteen flex hospitals designed to care for patients<br />
during the anticipated surge of COVID-19 patients.<br />
<strong>New</strong> <strong>Hampshire</strong> Nurses Association fully refunded all<br />
registration fees. However, we received permission<br />
MANAGEMENT MINUTE<br />
The new normal is likely to include more virtual and<br />
fewer face-to-face meetings. With technology allowing<br />
for many participants, seeing 10 or more faces at the<br />
same time can get distracting. When your mind starts<br />
to wander, you have no idea what the last person said.<br />
Perhaps you pretend to listen while checking your inbox<br />
and answer emails. By the end of the meeting, does it<br />
seems like a waste of time?<br />
A recent article in the Harvard Review, Gershman (<strong>2020</strong>)<br />
provides five suggestions for more effective virtual<br />
meetings.<br />
1. Before the meeting, determine the purpose of the<br />
meeting and what you can contribute. If you do not<br />
have a critical role, determine what you hope to<br />
learn.<br />
2. Before you raise a new topic, reiterate what you<br />
just heard or the previous point you are addressing.<br />
from planned speakers to post their presentations and<br />
handouts on the NHNA website. We worked with the<br />
planned sponsors and exhibitors to create a Graduating<br />
Student Nurse Career Resource Guidebook. The<br />
Guidebook lists each of the sponsors and exhibitors<br />
with contact information for their human resource<br />
department and an information pitch, prepared by the<br />
organization, sharing the benefits of working at their<br />
organization. Available links to the organization’s online<br />
career resource webpages are included. The Guidebook<br />
was emailed to every registrant of the Graduating Student<br />
Conference & Career Fair and posted to the NHNA<br />
website on a specially created webpage: Graduating<br />
Student Nurse Conference.<br />
NHNA wishes to extend a thank you to all the planned<br />
sponsors and exhibitors for the Graduating Student<br />
Conference & Career Fair. We look forward to meeting<br />
the Class of 2021 in person!<br />
People are more likely<br />
to listen if they first feel<br />
they have been heard.<br />
3. Summarize frequently<br />
stated comments to<br />
guide the conversation.<br />
4. Write down wandering thoughts<br />
during the meeting allowing you to be more present<br />
and ready to listen.<br />
5. Don’t be afraid to ask a clarifying question “I<br />
apologize, I lost track of the conversation for a<br />
moment. Could someone help me understand why<br />
we are focusing on ……”<br />
Gerhman notes that the bigger the group, the less<br />
responsibility each person feels to ensure success. One<br />
of the best ways to be heard in a virtual meeting is to be<br />
an active listener.<br />
Littleton Hospital Acquires <strong>New</strong> Sim Lab<br />
Glencliff Home<br />
is accepting applications for<br />
Registered Nurses I-III<br />
Salary Range: $50,835.20 - $71,052.80<br />
Licensed Practical Nurses I-II<br />
Salary Range: $45,177.60 - $57,408.00<br />
Additional 15% Enhancement on Salary Base (Not Included)<br />
40 hours/week – All Shifts and Part-time Available<br />
Direct Care an additional $1,040.00<br />
Add additional 2nd shift diff. at $4,160.00<br />
Add additional 3rd shift diff. at $7,280.00<br />
To provide professional nursing care to residents within an<br />
assigned unit and provide and support medical care as directed<br />
by medical staff and pursuant to objectives and policies of the<br />
nursing department and Glencliff Home. Must possess and<br />
maintain a current license as a RN/LPN in NH. Salary and Position<br />
determined by years of experience and certifications.<br />
State of <strong>New</strong> <strong>Hampshire</strong> Benefit Package!<br />
Health/Dental/Vision/Prescription plan<br />
Single $22/ 2-Person $44/ Family $66 (Bi-Weekly)<br />
L. Todd Bickford, Administrator<br />
393 High Street, PO Box 76, Glencliff, NH 03238<br />
(603) 989-5203 | Louis.Bickford@dhhs.nh.gov<br />
Applications can be completed and benefits reviewed online at<br />
https://das.nh.gov/hr/index.aspx<br />
Equal Opportunity Employer<br />
The Littleton Regional Healthcare (LRH) Fundraising<br />
Committee approved the purchase of high-fidelity<br />
training manikins, and investment of $100,000 for<br />
a state of the art Simulation Lab. The funding was<br />
supported by large and small donors who had<br />
not designated their donation other than an area<br />
of greatest need. The Sim Lab will be available to<br />
new graduate nurses, nursing assistants (LNAs),<br />
medical assistants (MAs), respiratory therapists, and<br />
physicians.<br />
Full-Time Nurse Trainer Opportunity at<br />
One Sky Community Services!<br />
Office-based position at a non-profit agency in<br />
Portsmouth, NH, supporting individuals with DD, ABD/ABI,<br />
and their families. Must be an RN licensed to practice in NH<br />
and will be required to become a Nurse Trainer through the<br />
NH Bureau of Developmental Services. Job responsibilities<br />
include trainings and monitoring the quality of services<br />
and supports provided through One Sky and our service<br />
provider partners. Prior experience working with<br />
individuals with DD or ABD/ABI is ideal, but not required.<br />
Email HR@oneskyservices.org for more information.<br />
From Left to right: Calyn Brown, LNA; Crystal<br />
Kimball, LNA; Susie; Heather <strong>New</strong>field, RN, BSN,<br />
CEN, CPAN - Manager of Education and Tammy<br />
Ladd, RNC, BSN, CLC - Clinical Coordinator<br />
An adult manikin named "Susie" can be set up to mimic the<br />
various stages of pregnancy. The option will be invaluable<br />
not only to maternity staff, but to EMTs in the community.<br />
Likewise, clinical staff are able to maintain competencies<br />
necessary to care for babies born at LRH. Sim Lab staff can<br />
program "Tory," the newborn baby manikin, for any number<br />
of conditions arising in a newborn.<br />
Heather <strong>New</strong>field, RN, BSN, CEN, CPAN and Manager<br />
of Education and Staff Development states, "We are so<br />
pleased to have the Simulation Training Lab available to<br />
our staff and local emergency medical service providers. It<br />
allows LRH to provide ongoing training to clinical support<br />
staff, nurses, and physicians so we can continue to provide<br />
quality healthcare to the community."
<strong>June</strong>, July, August <strong>2020</strong> <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s • Page 5<br />
IN MY OPINION<br />
The <strong>2020</strong> Irony<br />
It is ironic. The <strong>2020</strong> outbreak<br />
of COVID-19 parallels the Year<br />
of the Nurse commemorating<br />
the 200th birthday of Florence<br />
Nightingale. Nightingale’s<br />
experience during the Crimean<br />
War has been repeated exactly<br />
200 years later. Florence<br />
felt overwhelmed by the<br />
seemingly impossible situation<br />
of having only 38 nurses to<br />
care for over 2,500 injured<br />
and sick men. Florence<br />
was frustrated with the lack<br />
Susan Fetzer<br />
and inability to obtain needed supplies. Florence felt<br />
sorrow at the inability of medical care to cure disease<br />
or prevent a death. Florence felt discouraged when<br />
necessary medications were not available and men had<br />
to undergo amputations without chloroform anesthesia.<br />
Florence had to be resourceful to create areas that were<br />
safe and clean for her patients. Florence demonstrated<br />
quiet heroism, she did not feel the need to exploit her<br />
successes. She left a legacy which we commemorate<br />
today and still learn about nursing from her writings.<br />
While the celebration of Florence Nightingale’s<br />
birthday marks the end of National Nurses Week,<br />
this year, National Nurses Month continued with<br />
the theme “Nurses Make a Difference.” Even<br />
the public service announcements on radio and<br />
television have acknowledged nurses’ contributions<br />
and the difference we are making. I have never seen<br />
as many nurses profiled on media as I have in <strong>2020</strong>.<br />
Two hundred years ago Florence used her letters to<br />
generate interest about the contributions of nurses.<br />
Today, it is technology. Even the use of technology<br />
during the past three months has provided a new<br />
normal for how individuals communicate. We<br />
would have never thought 12 months ago of having<br />
a virtual birthday party, a virtual wedding, or a<br />
virtual hospital visit. The amount of information<br />
available on the internet has exploded, from videos,<br />
interviews, opinions and scientific research. I would<br />
predict that <strong>2020</strong> will be regarded as the Year of<br />
Virtual Communication.<br />
As I do before every issue of the <strong>New</strong> <strong>Hampshire</strong><br />
Nursing <strong>New</strong>s, I virtually scan hospital, long term<br />
care, school of nursing and specialty organization<br />
websites for ‘news’ about nurses and nursing.<br />
The results are typically very disappointing. Few<br />
organizations have a section of their website<br />
dedicated to the nursing department that is<br />
available to the public. It is as though nurses are<br />
invisible. While press releases are put out about<br />
new providers at an institution, there is no press<br />
release about new nurse employees and what they<br />
will bring to the organization. Websites post newly<br />
developed programs or technology, but fail to even<br />
mention that nurses will be managing the program<br />
or learning and operating the new equipment. In<br />
my opinion, this failure to demonstrate how we<br />
make a difference reflects on both institutional<br />
administrations and the willingness of nurses to<br />
allow for virtual invisibility. Nursing departments<br />
should invite their Public Relations Department to<br />
key meetings and expect a monthly ‘profile’ article.<br />
Nurses must step up and inform others of their<br />
accomplishments.<br />
The accomplishments in sports, school or nonhealth<br />
care news over the past three months has<br />
been replaced by front page health care news.<br />
Seemingly to fill newspaper space and television<br />
time a few nursing stories related to how the public<br />
has honored nurses have been publicized. But<br />
nurses in masks and scrubs outside facilities waving<br />
to cars or planes going by is not how we make a<br />
difference. It only makes one wonder who is left<br />
inside to care for patients.<br />
Nurses have demonstrated a Nightingale brand of<br />
heroism. While Florence did not accept accolades<br />
easily, she did use her accomplishments to further<br />
her mission. Heroism is in your story that must be<br />
shared. We need to take a lesson from Florence’s<br />
play book. She wrote to the politicians, army<br />
generals and even the Queen to explain the positive<br />
impact of her actions. It is time for nursing to have<br />
virtual visibility, and not just on the back page.
Page 6 • <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s <strong>June</strong>, July, August <strong>2020</strong><br />
Board of Nursing Responds to State of Emergency<br />
On Friday, March 13, <strong>2020</strong>, Governor Chris Sununu<br />
signed Executive Order <strong>2020</strong>-04 declaring a state of<br />
emergency in response to COVID-19. Section 3 of the<br />
Executive Order stated:<br />
Beginning at 11:59 p.m. on Sunday, March 15,<br />
<strong>2020</strong> all assisted living facilities, long term care<br />
facilities, nursing facilities, residential care facilities,<br />
as those terms are defined in RSAs 151-151-H,<br />
or any other similar facilities providing residential<br />
care to elderly or infirm patients, shall prohibit<br />
visitor access to reduce facility based transmission<br />
of COVID-19. This prohibition shall not apply to<br />
medically necessary personnel, visitors for residents<br />
receiving end of life care, or visitors necessary<br />
to provide for a residents psychosocial needs<br />
as determined by a licensed medical care provider.<br />
In effect, the governor's executive order caused nursing<br />
assisted living facilities, long term care facilities, nursing<br />
facilities, residential care facilities, and any other similar<br />
facilities to be "locked down" to all visitors. Visitors<br />
included nursing students. The Board of Nursing Rules<br />
require that programs that prepare LNAs must require that<br />
each LNA student obtain 60 hours of clinical experience<br />
in a skilled nursing facility (Nur 704.09(i)). Yet, the majority<br />
of locations that provide such clinical experience are<br />
closed to all visitors, including nursing students, for the<br />
duration of the state of emergency. For pre-licensure<br />
LPN and RN programs, the rules currently require that<br />
the program's curriculum be approved by the Board of<br />
Nursing, and that any changes to the curriculum also need<br />
to be approved, including any changes to requirements for<br />
clinical experience (Nur 602.16).<br />
The Board of Nursing’s Chair, Vice-Chair, Administrator<br />
along with the Director of the Office of Professional<br />
Licensure requested an emergency rule to address the<br />
concerns related to the current state of emergency in <strong>New</strong><br />
<strong>Hampshire</strong>. A rule related to clinical experience during<br />
a state of emergency was drafted (see Box Nur 101.04).<br />
In an emergency meeting on March 16, <strong>2020</strong> the Board<br />
of Nursing passed the rule, which was submitted and<br />
accepted by the State of NH, and is now in effect until<br />
September 12, <strong>2020</strong>.<br />
Nur 101.04 "Clinical Experience" means practice in<br />
an inpatient, ambulatory care, or community setting<br />
where the student provides care to patients under<br />
the guidance of a nursing instructor or preceptor.<br />
(a.) Clinical Experience may be substituted with<br />
simulation and lab work during a State of<br />
Emergency Declared by the Governor that<br />
impacts clinical site availability; provided,<br />
however, the Board of Nursing is notified<br />
within twenty-four (24) hours of such<br />
substitution. "Simulation" means a technique,<br />
not a technology, to replace or amplify real<br />
experiences with guided experiences that evoke<br />
or replicate substantial aspects of the real world<br />
in a fully interactive manner.<br />
The rule relaxes the requirement for clinical experience<br />
during the course of a declared state of emergency,<br />
and allows the 60 hours of clinical experience to be<br />
substituted with 60 hours of simulation and lab work<br />
during the state of emergency. Nursing programs may<br />
substitute in-person clinical with virtual simulation. The<br />
Board must be given 24 hours’ notice of such substitution.<br />
RN and LPN programs needing to affect changes in<br />
curriculum delivery as a result of the transition from<br />
in-person to online learning are also impacted by Nur<br />
602.16. The rule relates to notification requirements for<br />
curriculum changes, which requires three months prior<br />
written notice when changes occur in more than 10%<br />
of [entire program] credit hours. However as most of the<br />
curriculum revisions necessitated by transition from inperson<br />
to online learning relate to the last six weeks of<br />
the Spring <strong>2020</strong> term the rule is less likely to be applied.<br />
Advance your<br />
nursing career at<br />
the state’s flagship<br />
MASTER OF<br />
SCIENCE IN<br />
NURSING<br />
Primary Care<br />
Family Nurse<br />
Practitioner (FNP)<br />
university<br />
ADVANCED NURSING<br />
EDUCATION<br />
WORKFORCE (ANEW)<br />
Family Nurse Practitioner<br />
traineeships for students<br />
interested in rural and<br />
underserved practice.<br />
POST-<br />
MASTER’S<br />
CERTIFICATE<br />
Primary Care<br />
Family Nurse<br />
Practitioner (FNP)<br />
For example a two-year<br />
nursing program, with<br />
two 16-week terms for<br />
each of two years and<br />
one 8-week summer<br />
term has a total of 72<br />
weeks in the program. If<br />
this program changes from<br />
in-person instruction to online<br />
instruction for six weeks (of the<br />
72 weeks) only 8.33% of the total curriculum hours are<br />
affected. Only a Board of Nursing notification is required<br />
if the 10% threshold is not met.<br />
The relaxation of in-person clinical experiences have<br />
implications for potential employers of Board of Nursing<br />
licensees. Licensed Nursing Assistants that were trained<br />
during the state of emergency may not have received a<br />
comprehensive clinical experience with direct patient<br />
care. They may require extended orientations specifically<br />
in care needs of patients with dementia or cognitive<br />
impairment.<br />
The Board of Nurses has also enacted an amendment to<br />
Nur 303.02 (d) pursuant to Emergency Rule on March<br />
23, <strong>2020</strong>, to extend the time period for taking the NCLEX<br />
exam.<br />
Nur 303.02 (d) Registered and Practical Nurse<br />
Examinations. (d) For graduates of programs<br />
within the US or Canadian Provinces where<br />
the NCLEX is required, the NCLEX shall be<br />
taken within six months of graduation from an<br />
approved school of nursing. Notwithstanding,<br />
during a State of Emergency declared by the<br />
Governor, the Board shall allow Registered<br />
and Practical Examinations to be completed<br />
within 90 days of the Expiration of the State of<br />
Emergency to complete this requirement.<br />
The Governor’s Executive Order called for the temporary<br />
authorization for out of state medical providers to provide<br />
medically necessary services and provide services<br />
through telehealth. The temporary licenses authorized<br />
under this emergency order are issued to any healthcare<br />
provider who can demonstrate a license in good standing<br />
in another State jurisdiction. The temporary licenses are<br />
being provided at no charge and remain valid during the<br />
declared state of emergency. As of May 1, 2002, 1633<br />
temporary licenses were issued to APRNs, 39 to RNs, four<br />
to LPNs and one to an LNA.<br />
The Executive Order declaring a state of emergency<br />
concerns meetings of public bodies. Therefore public<br />
sessions of the meetings of the <strong>New</strong> <strong>Hampshire</strong> Board<br />
of Nursing are being conducted by teleconference and/<br />
or video teleconference. Information on how to connect<br />
and listen to the Board of Nursing meeting is posted on<br />
the website (nhbon.org) under Board Meetings.<br />
Staffing of nursing homes and assisted living facilities has<br />
been dramatically impacted by COVID-19 transmission.<br />
Senator Tom Sherman, Representative Polly Campion<br />
RN, Lindsey Courtney, Interim Director of the Office of<br />
Professional Licensure and Board of Nursing Administrator<br />
Bonnie Crumley-Aybar met to develop a streamlined<br />
process to encourage LNAs with licenses that had lapsed<br />
within the past three years to reenter the workforce.<br />
An outreach to nursing students who had passed<br />
Fundamentals of Nursing was created to secure an LNA<br />
license and practice in long term care facilities. The<br />
$35.00 licensing fee is being waived to encourage nursing<br />
students to become LNAs.<br />
Bonnie Crumley-Aybar, RN, MSN is the Administrator of<br />
the <strong>New</strong> <strong>Hampshire</strong> Board of Nursing.<br />
For more information contact:<br />
Dayle.Sharp@unh.edu<br />
chhs.unh.edu/graduate-nursing
<strong>June</strong>, July, August <strong>2020</strong> <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s • Page 7<br />
NHNA in Alliance to Support Senior Facilities<br />
A newly formed statewide network of volunteers has<br />
now been working for three weeks to provide help<br />
and guidance to senior residential facilities in <strong>New</strong><br />
<strong>Hampshire</strong>, including assisted living and nursing homes,<br />
to enable them to better handle the health crisis caused by<br />
COVID-19.<br />
As of May 4, the network, known as the COVID Alliance<br />
Senior Support Team (SST), had more than 60 volunteer<br />
COVID Response Liaisons serving 65 facilities. The<br />
Liaisons are available daily to gather information about the<br />
facilities’ needs and connect them with state, federal, and<br />
private resources that can help them. The most common<br />
issues Liaisons discuss with facility staff are personal<br />
protective equipment (PPE), staffing and testing needs.<br />
The effort launched on April 13, after having consulted<br />
with residential industry associations, state government<br />
officials, university leaders, medical experts and the<br />
<strong>New</strong> <strong>Hampshire</strong> Nurses Association. The impetus<br />
for the program came from the COVID-19 Policy<br />
Alliance, founded by faculty at the MIT Sloan School<br />
of Management to help reduce the impact of the virus,<br />
particularly on the elderly.<br />
SST Chairman and NH State Senator Tom Sherman, who<br />
is also a practicing physician, points out that the age,<br />
comorbidities and close proximity of the residents of<br />
senior residential facilities put them at especially high<br />
risk of COVID-19 outbreaks. “Experience in Italy, Spain,<br />
Washington State, and a growing list of locations around<br />
the world, shows that COVID-19 can spread quickly<br />
among the residents and staff of senior residential facilities,<br />
and the evidence is clear that older COVID-19 patients are<br />
more likely to require hospitalization or die. This makes<br />
senior care facilities a critical front line in the fight against<br />
COVID-19. The volunteers of the Senior Support Team<br />
intend to do everything they can as remote volunteers to<br />
support senior care facilities through this crisis.”<br />
Each participating facility began by filling out a survey to<br />
evaluate its potential exposure to COVID-19 and to inform<br />
the facility’s Liasons on its risks and needs. The SST also<br />
operates an automatic text messaging tool, developed by<br />
MIT graduate student Jackie Baek, to quickly and easily<br />
document new cases and new needs at each participating<br />
facility each day. This has become a critical technical tool<br />
for the SST and its partners.<br />
The SST first contacted residential facilities to see if they<br />
were interested in participating through a number of<br />
associations, including the <strong>New</strong> <strong>Hampshire</strong> Association of<br />
Residential Care Homes (NHARCH), the <strong>New</strong> <strong>Hampshire</strong><br />
Healthcare Association (NHHCA), LeadingAge ME &<br />
NH, and the NH Association of County Nursing Homes.<br />
The SST collaborates with these associations to share<br />
knowledge and resources, advocating for the needs of<br />
participating senior living and long-term care providers.<br />
With the consent of participating facilities, the SST<br />
provides data on facility status to the associations each day.<br />
“Given the nature of this pandemic, our usual support<br />
systems have been stretched beyond their capacity. The<br />
importance of collaboration with other associations and<br />
organizations has increased a great deal. We welcome the<br />
Alliance’s expertise in data collection, as well as volunteer<br />
coordination, to help our members, and the members of<br />
our industry partners,” said Kelly Adams, Vice President<br />
of the <strong>New</strong> <strong>Hampshire</strong> Association of Residential Care<br />
Homes (NHARCH).<br />
Lisa Henderson, Executive Director of LeadingAge Maine<br />
& <strong>New</strong> <strong>Hampshire</strong>, says “LeadingAge Maine & <strong>New</strong><br />
<strong>Hampshire</strong> is grateful for our partnership with the COVID<br />
Alliance. Their rapid development and deployment of<br />
a daily texting program to help us check in with our<br />
members on the frontline is helping us direct resources to<br />
them and continue to advocate for their most urgent needs<br />
including PPE, staffing and testing.”<br />
The <strong>New</strong> <strong>Hampshire</strong> Nurses Association (NHNA) was<br />
a critical partner for the SST on volunteer recruitment<br />
and organization. “We are proud that NHNA Past<br />
President, Dr. Judith Joy, has been appointed the Statewide<br />
Coordinator for the COVID Response Liaison volunteers.<br />
Paula MacKinnon (President-Elect, School Nurses<br />
Association) has also played a critical role developing the<br />
team’s data collection tools,” said NHNA Nurse Executive<br />
Director Joan Widmer. Nearly all of the volunteer Liaisons<br />
of the SST have some level of healthcare training, and<br />
a majority are current school nurses or retired nurses<br />
recruited by the NHNA. Also represented on the allvolunteer<br />
SST team are MIT student EMTs and graduate<br />
students, professors and physician assistant students from<br />
MCPHS, Dartmouth medical students, political campaign<br />
operations and data experts, and volunteers from the NH<br />
business and nonprofit sectors.<br />
The SST has developed a menu of resources to ensure the<br />
volunteer liaisons are always aware of the latest guidance<br />
for their calls. “I’ve worked closely with nurse educators<br />
from around <strong>New</strong> <strong>Hampshire</strong> to create a searchable FAQ/<br />
reference site where SST liaisons and senior care facilities<br />
alike can quickly find answers to their questions and links<br />
to authoritative public health information,” Deb Baker,<br />
Library Director at Manchester Community College, who<br />
also serves as the Chief Librarian for the SST.<br />
The Medical Advisory Group vetting the materials used<br />
by the SST includes State Rep. Dr. Jerry Knirk, Dr. Paul<br />
Friedrichs, Dr. Karl Singer, Dr. Apara Dave, SST Chairman<br />
and NH State Senator Dr. Tom Sherman, Dr. Daniel<br />
Stadler, Dr. Bruce Bartolini, Dr. Kim Perez, and Prof. Linda<br />
Martino.<br />
“We intend to be ready to serve all of the over 200<br />
licensed senior care facilities in <strong>New</strong> <strong>Hampshire</strong>,” said SST<br />
Executive Director Daniel Curtis. “We have the structure<br />
and the amazing volunteers to do it, and we’ve already<br />
made a big impact to help get the senior care facilities of<br />
<strong>New</strong> <strong>Hampshire</strong> the support they need.” To learn more<br />
about the SST, visit our website at covidalliance.com/sst.
Page 8 • <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s <strong>June</strong>, July, August <strong>2020</strong><br />
APRN COLUMN<br />
Post-Graduate Advanced Practice<br />
Training Programs<br />
Jillian Bellmont,<br />
<strong>New</strong> <strong>Hampshire</strong> Nurse Practitioner Association<br />
Advanced practice providers (APP) are qualified medically<br />
licensed health care providers, who can function<br />
independently or alongside a physician, in population<br />
centered care models, disease management, care<br />
coordination, and direct patient care. This professional<br />
umbrella term includes nurse practitioners (NP) and<br />
physician assistants (PA) among several other subgroups of<br />
non-physician health care providers. In the United States,<br />
there are very few APPs who have undergone formal<br />
postgraduate training. Post-graduate APP educational<br />
programs are becoming more popular and are typically<br />
designed for new graduates and experienced clinicians<br />
interested in change of practice specialty.<br />
The Institute Of Medicine (IOM) has recommended that<br />
“state boards of nursing, accrediting bodies, the federal<br />
government, and healthcare organizations should take<br />
actions to support nurses’ completion of a transition-topractice<br />
program (residency) after they have completed<br />
a prelicensure or advanced practice degree program or<br />
when they are transitioned into new clinical practice areas.”<br />
Many APPs have limited orientation programs as they enter<br />
practice and are expected as new graduates to perform<br />
at an advanced level with minimal support. Fellowships<br />
and residencies are not required for NPs or PAs as these<br />
professionals have met all training requirements needed for<br />
licensure during their graduate programs.<br />
Programs to facilitate APP transition-to-practice programs<br />
have been developed with continued growing numbers<br />
of public and private institutions across the US. Added<br />
support and mentoring after graduation is fundamental to<br />
an effective transition from new grad to expert. Bush and<br />
Lowery (2016) opined that postgraduate education has<br />
demonstrated statistically significant positive influence<br />
on NP job satisfaction. Influence on professional growth,<br />
autonomy and more valuable collegiality in early years of<br />
career development are key factors identified. Post-graduate<br />
programs should complement formal education with a goal<br />
to promote autonomy, aid with adjustment of role transition<br />
and support productivity within a rapidly changing and<br />
demanding healthcare system. Leading programs provide<br />
learning environments that stimulate professional growth<br />
and include mentorship, lectures, supervision, assigned<br />
readings, online courses, active critiques on performance<br />
and case presentations.<br />
100 Saint Anselm Drive<br />
Manchester, NH 03102<br />
(603) 641-7086<br />
www.anselm.edu/cne<br />
Committed to Promoting Excellence<br />
in the Practice of Nursing<br />
Saint Anselm College is approved as a provider of nursing<br />
continuing professional development by the Northeast<br />
Multistate Division, an accredited approver by the American<br />
Nurses Credentialing Center’s Commission on Accreditation<br />
Residency and Fellowship programs for APP can also<br />
have drawbacks and may not be the right path for<br />
everyone. Most post-graduate APP programs are not<br />
widely standardized. However, there are several notable<br />
accrediting bodies who have developed guidelines<br />
and formal standards which are becoming increasingly<br />
appreciated and used. There are no dual-accreditation<br />
options available to include both NPs and PAs. The value<br />
of accreditation for individual programs is still being<br />
evaluated and uniquely dependent on each organization.<br />
Supplemental education is expensive and there is no<br />
published evidence supporting improved patient outcomes<br />
related to these programs. Post-graduate training programs<br />
can cost organizations up to $100,000 per trainee including<br />
support needed to supplement lost preceptor productivity.<br />
Post-graduate training programs typically offer decreased<br />
salaries and have one or two year employment agreement.<br />
There are also inconsistencies among titles of programs (i.e.<br />
residency vs fellowship) which may obscure trainee choices<br />
and contributes to confusion.<br />
As leaders, educators and clinicians, we have a professional<br />
obligation to guide our nurse practitioner and physician<br />
assistant colleagues with the ongoing development of postgraduate<br />
education and training. It is important we avoid<br />
terminology that may indicate or promote downstream<br />
regulatory implications or mandatory requirements, or<br />
suggest APPs are not prepared to enter the workforce upon<br />
completion of formal graduate education. Post-graduate<br />
training programs help promote creative models to bridge<br />
gaps in our rapidly changing health system and add<br />
leadership opportunities for NPs and PAs. It is important to<br />
be aware of novel and growing programs which may help<br />
provide the support and structure a colleague, a graduating<br />
student or even yourself, may need for a successful and<br />
supported transition in clinical practice.<br />
References:<br />
American Association of Nurse Practitioners. The NP roundtable’s<br />
discussion paper on NP education and postgraduate training.<br />
Updated 2013. Retrieved at http://www.aanp.org/component/<br />
content/article/82-legislation-regulation/policy-toolbox/nppolicy-essentials/445-aanp-and-the-np-roundtable-jointstatements/.<br />
Accessed Feb 13, <strong>2020</strong>.<br />
Bush, C. & Lowery, B. (2016). Postgraduate Nurse Practitioner<br />
Education: Impact on Job Satisfaction. The Journal for Nurse<br />
Practitioners. 12(4). April 2016.<br />
Institute of Medicine. The future of nursing: leading<br />
change, advancing health. 2011. Retrieved at http://iom.<br />
nationalacademies.org/Reports/2010/The-Future-of-Nursing-<br />
Leading-Change-Advancing-Health.aspx. Accessed Feb 13,<br />
<strong>2020</strong>.<br />
We’re Looking For The Best.<br />
Come Join Our Team!<br />
We have many opportunities available at<br />
Memorial Hospital’s Merriman House<br />
• RNs, LPNs, and LNAs<br />
• $1,000 sign-on bonus* (for qualified candidates)<br />
• Exceptional MaineHealth benefit package<br />
• Generous shift differential<br />
• Work with a friendly and collaborative team<br />
providing compassionate care to residents<br />
We offer excellent pay, wonderful benefits, paid vacation,<br />
tuition reimbursement, retirement and all in a warm, exciting<br />
and compassionate team setting!<br />
Candidates can apply online at www.memorialhospitalnh.org<br />
An Equal Opportunity Employer<br />
“To every nurse throughout our state and beyond, our<br />
gratitude is as deep as your courage, and we thank you<br />
for your dedication to keeping your community healthy,<br />
and for the bravery, compassion and empathy you<br />
provide to your patients every day.”<br />
Steve Ahern, President of the <strong>New</strong> <strong>Hampshire</strong> Hospital<br />
Association, May <strong>2020</strong><br />
Congratulations to UNH Graduate student Susan<br />
Gonya RN and faculty mentor Pam DiNapoli, RN,<br />
PhD awarded 3 rd place for Student Poster by the Eastern<br />
Nursing Research Society. The poster was titled: Do<br />
We Really Know What's in Our Food? The Connection<br />
between Dietary Mycotoxin Exposure and Pediatric<br />
Crohn's Disease. Unfortunately, the Annual meeting of<br />
ENRS, March 26-7, to be held in Boston was cancelled<br />
though posters were judged virtually.<br />
Dr. Jillian Belmont was recently<br />
elected President of the <strong>New</strong><br />
<strong>Hampshire</strong> Nurse Practitioners<br />
Association. Belmont received<br />
her BSN from St. Anselm’s, MSN<br />
from UNH and DNP from<br />
Northeastern University. Her<br />
focus is neurology which she<br />
practices as an assistant<br />
professor and associate provider<br />
at DHMC. Belmont is also<br />
serving as President of the Green and White Mt. Chapter<br />
for American Academy of Neuroscience Nursing.<br />
Loon Chocolates<br />
Deliver Joy to<br />
Nurses<br />
Loon Chocolates, the small local chocolate maker in<br />
<strong>New</strong> <strong>Hampshire</strong>, located at seven different locations in<br />
the state is delivering chocolate to health care workers<br />
on the front lines of the Covid-19 pandemic. The<br />
company has delivered over 500 of their Hero Bars to<br />
Healthcare Heroes in the state with a goal of 800 Hero<br />
Bars by <strong>June</strong> 1, <strong>2020</strong>.<br />
Loon’s goal is to provide some joy to Healthcare<br />
Heroes while fighting the battle for all of us. They have<br />
donated chocolate bars at Catholic Medical Center,<br />
Parkland Medical Center, Dartmouth Hitchcock Medical<br />
Center, Exeter Hospital, Concord Hospital, NH State<br />
Hospital, Primary Care of Milford and several retirement<br />
communities in southern <strong>New</strong> <strong>Hampshire</strong>. Their website<br />
provides an avenue for public support of the project.<br />
Nurses always appreciate a little chocolate to sweeten<br />
their day.<br />
Jennifer Pitre receives Loon chocolates for<br />
Catholic Medical Center Healthcare Heroes
<strong>June</strong>, July, August <strong>2020</strong> <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s • Page 9<br />
Family centered maternity care and COVID-19<br />
Since the model of family centered maternity care (FCMC) was first<br />
recommended in the late 1970’s, hospitals and birthing centers have moved<br />
toward a model of care that focuses on the needs of the family unit as whole<br />
during an important life transition. While not always a perfect model, FCMC<br />
techniques have been linked to positive outcomes across the spectrum of<br />
perinatal and infant care. Supportive family interventions such as the roomingin<br />
of infants with their parents on postpartum care units reduces hospital<br />
costs, decreases infant infections, supports early initiation of breastfeeding,<br />
encourages bonding, and increases patient satisfaction. Although the motherinfant<br />
couplet is often the focus of the provision of inpatient care, maternity<br />
nurses are experts at supporting mothers, their partners, and extended family<br />
on obstetric and neonatal care units, in the community setting, and in patient’s<br />
homes.<br />
Until recently, the FCMC framework was actualized in many ways in <strong>New</strong><br />
<strong>Hampshire</strong> hospitals. Family waiting rooms allow supportive friends and<br />
family to gather in anticipation and support expectant parents before and after<br />
their deliveries. Whenever possible, patient rooms are single rooms, warmly<br />
lit and decorated to appear more like a welcoming home environment, with<br />
a place for supporting partners to stay overnight. Childbirth preparation<br />
classes welcome pregnant patients and their partners to the hospital in the<br />
weeks before delivery to tour the unit and learn about their options from<br />
nurse childbirth educators. Partners are admitted into the OR for C-section<br />
deliveries, a practice not usually seen in surgical settings. Hospitals offer<br />
sibling and grandparent preparation classes, recognizing that the family unit<br />
extends beyond the parents and provide postpartum care home visits to<br />
continue to support families after discharge. Nurses bring infants to bond<br />
with their mothers through skin-to-skin on adult ICU units, or help mothers<br />
separated due to maternal illness to pump their breastmilk and bring it to the<br />
NICU to give to premature or ill neonates. These recommended practices were<br />
all flourishing before COVID-19 changed the face of obstetrical care.<br />
Tenants of family centered maternity care (JOGNN, 1978, p. 55)<br />
• The family is the basic unit of society.<br />
• The family is viewed as a whole unit within which each member is an<br />
individual enjoying recognition and entitled to consideration.<br />
• That childbearing and childrearing are unique and important functions of the<br />
family.<br />
• The childbearing experience is an experience that is appropriate and beneficial<br />
for the family to share as a unit.<br />
• That childbearing is a developmental opportunity and/or a situational crisis,<br />
during which the family members benefit from the supporting solidarity of the<br />
family unit. (p. 55)<br />
Alyssa O’Brien, PhD, RN is an Assistant Professor of nursing at UNH and member of the<br />
NH AWHONN Steering Committee.<br />
Family Center<br />
nurses at Exeter<br />
Hospital in April<br />
<strong>2020</strong> (Photo<br />
courtesy Michelle<br />
Savoie)<br />
Women and<br />
Children’s Center<br />
nursing staff<br />
at Wentworth-<br />
Douglass Hospital<br />
(Photo courtesy<br />
Diane Proulx)<br />
The CDC, WHO, and professional organizations have been quick to establish<br />
guidelines for safely providing care to patients and families in the time of<br />
COVID-19. Family care units and providers across <strong>New</strong> <strong>Hampshire</strong> have<br />
swiftly put in place protocols to reduce risk to staff and patients. Of primary<br />
concern is the transmission of the virus, but also to find ways to provide safe,<br />
supportive, and affirming care across the perinatal year. Recommendations<br />
include spacing out prenatal visits for low risk pregnant patients and increasing<br />
exposure screenings at prenatal visits and hospital intake, as well as increasing<br />
testing for women who are symptomatic. Under some circumstances an infant<br />
may be separated from their mother, if the birth mother has tested positive for<br />
COVID-19 and the status of the infant is unknown. Pregnant women have been<br />
encouraged to avoid gatherings and remain physically distanced whenever<br />
possible. Other recommendations impact everything from C-section protocols<br />
to hospital visitors.<br />
Precautionary measures have resulted in the provision of perinatal and infant<br />
care in NH that looks very different than just a few months ago. In many<br />
cases, nurses and other care providers are making phone calls or using telepractice<br />
visits to provide additional assessments, education, and support.<br />
Group prenatal exercise and education classes have been canceled with<br />
some organizations recommending online resources or offering virtual<br />
classes.<br />
During their hospital stay pregnant patients are limited to one support person,<br />
support groups have gone virtual. Support partners may not be permitted in<br />
the operating room or in other areas of the hospital. These restrictions have<br />
required nurses providing perinatal care and education to adapt.<br />
Nurses at Monadnock Community Hospital created a virtual hospital tour and<br />
make personal phone calls to all expectant families to establish support and<br />
trusting relationships one-on-one with families. Perinatal education at Catholic<br />
Medical Center has gone virtual, with overwhelmingly positive responses to<br />
Zoom and virtual classes developed by their perinatal education coordinator.<br />
Although the use of popular labor support techniques like nitrous oxide are<br />
not currently allowed due to guidelines, nurses at Wentworth-Douglass<br />
Hospital created shared decision-making documents to use with COVID<br />
positive moms and their support partners. They are also using virtual platforms<br />
for postpartum support groups.<br />
Patients report that this time feels stressful and uncertain, but they are being<br />
well supported by their nurses and providers. For some, the time to bond<br />
alone with their newborns without expectations to entertain numerous<br />
hospital visitors has been a welcome side-effect of changes to family visiting<br />
policies. How COVID-19 will change FCMC practices in the long term is still<br />
unknown, but for now all across <strong>New</strong> <strong>Hampshire</strong> perinatal nurses continue<br />
to deliver high-quality FCMC to their pregnant and postpartum patients,<br />
newborns, and their families.
Page 10 • <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s <strong>June</strong>, July, August <strong>2020</strong><br />
Past, Present and Future of Nurse Anesthetists<br />
Janelle Pickering<br />
In this time of extreme uncertainty, the ingenuity and versatility of the nursing<br />
profession has never been more important. As COVID-19 ransacks not only<br />
our supply lines, but our healthcare staff, nurses have consistently risen to the<br />
challenges associated with working during a pandemic. These challenges do<br />
not solely revolve around patient care, in fact, some of the greatest challenges<br />
have surrounded the uncertainty of personal protective equipment (PPE)<br />
and appropriate utilization. PPE shortages, combined with frequent changes<br />
in protocols regarding the appropriate level of PPE, have left all healthcare<br />
providers nervous. Despite this concern, nurses everywhere have shown their<br />
ability to adapt to these rapidly changing circumstances, and selflessly share<br />
information on current best practices when treating COVID-19 patients. Social<br />
media has allowed for the quick dissemination of information and has brought<br />
into focus the immense value we bring to the healthcare team. This truly is the<br />
‘Year of the Nurse’!<br />
“Patients come to the hospital and stay the night, not because they need a<br />
doctor, but because they need a nurse. If they only needed a doctor, they could<br />
go to a doctor’s office. They come to the hospital and spend the night because<br />
they needed a nurse.” This quote, by Carol Rauen MS, RN-BC, highlights the<br />
value of nurses. During the COVID-19 pandemic, nurses have been on the<br />
frontlines in many capacities. As units attempt to limit contact with COVID-19<br />
positive patients, bedside nursing assessments have become even more critical<br />
in directing patient care. Nursing intuition takes years to develop. It is acquired<br />
not by rote memorization, but by countless interactions with patients and their<br />
families. This hard to define nursing intuition is often described as the “art of<br />
nursing,” and nothing is more alarming than a nurse saying she has a “bad gut<br />
feeling” about a patient’s condition. In a time when all medical providers are<br />
inundated by data, nursing intuition provides an additional tool for decision<br />
making. This reflexive thought is what allows a nurse to meet the constant,<br />
sometimes unexpected needs of the patient.<br />
The vast majority of the public are aware of the advance role of the Nurse<br />
Practitioner, but the role of the certified registered nurse anesthesiologist (CRNA)<br />
is not well understood. This lack of knowledge has created a situation in which<br />
some hospitals do not utilize the CRNA to their fullest potential at a time when<br />
every member of the nursing community is greatly needed.<br />
To understand a specialty, it is important to review its history. The first successful<br />
demonstration of an anesthetic was performed by William T.G. Morton on<br />
October 16, 1846, however, due to poor aseptic practices in the operating room<br />
(OR), lack of antibiotics, and high anesthetic mortality rates, anesthesia did<br />
not gain instant success (Ray & Desai, 2016). During the Civil War, 1861-1865,<br />
Catherine S. Lawrence is credited as the first ‘nurse’ to administer anesthesia in<br />
the form of chloroform to wounded soldiers needing emergent operations on<br />
the battlefield (Ray & Desai, 2016). Due to its characterization as a “subordinate<br />
role,” anesthesia was often delegated to medical students or younger physicians<br />
more eager to observe the surgical<br />
technique than administer the anesthetic.<br />
Despite its “subordinate role,” surgeons<br />
recognized the need for highly trained<br />
professionals to monitor and administer<br />
anesthesia to the patient, and were the<br />
earliest supporters of additional training<br />
for nurses to fulfill this role (Ray & Desai,<br />
2016).<br />
Catherine Lawrence, Civil War<br />
In 1877, Sister Mary Bernard was the first nurse<br />
to rise to the challenge of specializing in the<br />
delivery of anesthesia (Ray & Desai, 2016).<br />
Catholic nuns played an important role in<br />
training nurses to administer anesthesia, but<br />
Alice Magaw is credited as the true “Mother of<br />
Anesthesia.” In 1906, Alice Magaw published<br />
“A Review of Over Fourteen Thousand Surgical<br />
Anesthesias” which highlighted the benefits of<br />
a trained anesthesia provider (Ray & Desai, 2016). Her<br />
innovation and dedication to providing anesthesia safely,<br />
led to the Mayo Clinic being regarded as the best place for nurses to train in<br />
the delivery of anesthesia. With the beginning of World War I, the educational<br />
requirements and demand for trained anesthesia providers increased. Mayo<br />
Clinic and Pennsylvania Hospital responded to this increase by developing a sixweek<br />
course focused on safely administering anesthesia.<br />
Alice Magaw providing anesthesia<br />
circa 1906<br />
It was not until 1931 that a professional<br />
organization for nurse anesthesiologists<br />
was founded by Agatha Hodgins<br />
(Ray & Desai, 2016). The National<br />
Association of Nurse Anesthetist’s<br />
(NANA) name was changed to the<br />
American Association for Nurse<br />
Anesthetists (AANA) in 1939 which<br />
coincided with World War II, and another increase in educational requirements for<br />
nurse anesthesiologists (Ray & Desai, 2016). This brief overview of the anesthesia<br />
specialty shows not only the importance of nurses in its evolution, but also<br />
highlights that during times of chaos, nurses have continued to innovate and adapt<br />
to provide the safest care possible.<br />
The proud history of nursing innovation and versatility may be practiced to its<br />
fullest extent in <strong>New</strong> <strong>Hampshire</strong> where advanced practice nurses can provide<br />
exemplary care to their patients independently, without physician supervision. This<br />
is important as 37% of NH residents live in rural and underserved areas (2(Hub,<br />
<strong>2020</strong>). Historically, it has been difficult to recruit and retain healthcare providers<br />
in rural areas, and APRNs are more likely to provide care for underserved<br />
populations (Patel, Petermann, & Mark, 2018).<br />
Like their Nurse Practitioner counterparts, NH CRNAs licenses are not restricted,<br />
and CRNAs can practice independently, without physician supervision.<br />
Unfortunately, not all hospitals recognize the full scope of practice of the CRNA,<br />
not to mention the versatility, efficiency, accountability and high level of care that<br />
the CRNA provides.<br />
The AANA (<strong>2020</strong>) issued a statement at the beginning of the COVID-19 pandemic<br />
stating that “CRNAs should be given full authority to practice to their highest<br />
level of education and training…and their roles should reflect their high degree<br />
of clinical skill and expertise.” Across the country, individual hospitals’ responses<br />
to this statement have varied. CRNAs have found themselves furloughed or laid<br />
off, as elective case numbers significantly decreased. Some institutions decided to<br />
utilize their CRNAs as critical care nurses, but this approach diminishes the ability<br />
of the hospital to efficiently react to COVID-19. A CRNA working as an ICU nurse<br />
provides care to a single patient. In NH, CRNAs are recognized as APRNs, and this<br />
distinction makes it far easier to utilize CRNAs in the ICU. As APRNs, CRNAs can<br />
rapidly assess patients, provide advanced airway management, oversee ventilator<br />
management, place central lines, and order and assist in the titration of vasoactive<br />
medications and volume resuscitation. This list is far from inclusive, and shows the<br />
utility in the CRNA as part of the healthcare team, not simply as a one on one<br />
provider.<br />
Times of crisis are also times of great innovation, and COVID-19 is no exception.<br />
The value of nurses has never been more appreciated, and once again we have<br />
shown our versatility. We do not yet know what the new “normal” will be for us<br />
in the community and in the hospital. We have seen a crisis that has changed the<br />
very fabric of society and day to day functioning of our nation. Moreover, it has<br />
redefined what is meant by “essential” in both service and providers. Although we<br />
were able to “flatten the curve” we cannot be fooled into believing we are safe. It<br />
is my hope that we, as a nursing community, will use the lessons learned during<br />
this pandemic to forge a larger role in our communities, hospitals, and legislation.<br />
Our unique perspective will be invaluable, and it is important that we advocate<br />
not only to improve patient care, but to secure a future that values all nurses, in<br />
every specialty.<br />
References<br />
AANA (<strong>2020</strong>). CRNAs as advanced practice providers in critical care settings. https://www.<br />
aana.com/, accessed 05/01 <strong>2020</strong>.<br />
Hub, R. (<strong>2020</strong>). https://www.ruralhealthinfo.org/states/new-hampshire, accessed<br />
05/01/<strong>2020</strong>.<br />
Patel, E., Petermann, V., & Mark, B. (2018). Does state-level nurse practitioner scope-ofpractice<br />
policy affect access to care? Western Journal of Nursing Research, 41, 488-518.<br />
Ray, W. T., & Desai, S. P. (2016). The history of the nurse anesthesia profession. Journal of<br />
Clinical Anesthesia, 30, 51–58. https://doi-orrg.unh.idm.oclc.org/10.1016<br />
Janelle Pickering, DNP, CRNA is a nurse anesthetist at Dartmouth Hitchcock in<br />
Lebanon, <strong>New</strong> <strong>Hampshire</strong>.<br />
Ed Note: The <strong>New</strong>s welcomes NHANA as a NHNA Organizational Affiliate and<br />
looks forward to their future contributions to the <strong>New</strong>s.
<strong>June</strong>, July, August <strong>2020</strong> <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s • Page 11<br />
Home Care Nurses Caring for Recovering Patients<br />
Home Healthcare, Hospice and Community Services nurse<br />
Kristina McGuirk visits patients who have returned from the<br />
hospital after battling COVID-19. Staff photo by Ben Conant<br />
(reprinted with permission from Monadnock Ledger-Transcript)<br />
TIM GOODWIN<br />
Originally published by Monadnock Ledger-Transcript on 5/4/<strong>2020</strong>.<br />
Reprinted here with permission from Monadnock Ledger-Transcript<br />
When patients infected with coronavirus first made an appearance<br />
on Kristina McGuirk’s case load, it was hard not to be concerned.<br />
As a nurse with Home Healthcare, Hospice and Community<br />
Services, McGuirk’s job is to go into people’s homes to provide<br />
care for those dealing with a variety of conditions and medical concerns. But the addition<br />
of COVID-19 brought on that question of “what if?”<br />
“You have to assume everyone has it and that’s really the best way,” McGuirk said. “I<br />
obviously don’t know what I was expecting. It’s something we’ve never seen before.”<br />
She’s worried about being infected herself or bringing it home to her fiance. For those on<br />
her weekly caseload who had contracted coronavirus, her visits have so far come after<br />
the patient returned home from hospitalization.<br />
“The acute phase has already passed,” McGuirk said. She said that some patients’<br />
symptoms still remain like a cough and shortness of breath.<br />
“Little things like holding a conversation can be difficult,” she said. “They’re feeling<br />
shortness of breath just talking.”<br />
But as the weeks have gone by, McGuirk said she has seen progress from those patients<br />
who tested positive for the disease, like being able to walk up stairs and go outside.<br />
“It’s been really nice to see the recovery phase,” she said. “But the weekly progress I’ve<br />
seen was pretty gradual.”<br />
Each trip into someone’s home that has been diagnosed with COVID-19 – as well as<br />
everyone else – comes with a heightened sense of precaution. For patients who have<br />
tested positive for the virus, that means an N95 mask with a secondary cloth mask on<br />
top, double gloves, gowns and extra sterilization of the equipment.<br />
“Sure you think about it when you’re at work and on the way to their house for a visit,”<br />
she said.<br />
The <strong>New</strong> <strong>Hampshire</strong> Board of Nursing<br />
considered the following practice questions<br />
posed by licensees.<br />
<strong>New</strong>s<br />
Question: Is an LPN able to administer<br />
cosmetic injectable (dermal fillers, Botox)<br />
under an APRN who is authorized to<br />
practice in <strong>New</strong> <strong>Hampshire</strong>.<br />
BON Response: Yes, an LPN may administer the cosmetic injectable<br />
medication with a valid written order from a provider Physician APRN, or<br />
DDS who is authorized to practice in NH.<br />
McGuirk said that HCS was unable to supply her with booties or a<br />
hair covering due to shortages, but that if they were available, she<br />
would wear those too.<br />
Prior to a visit, HCS conducts screening calls, McGuirk said, and a<br />
lot of what she has done since the pandemic changed the way of<br />
life in <strong>New</strong> <strong>Hampshire</strong> has been to answer questions and educate.<br />
“Just doing our best relaying the information,” McGuirk said.<br />
While there is concern, McGuirk knows she has a job to do and<br />
can’t let fear or reluctance creep in.<br />
“I’m a nurse and I like helping regardless of their diagnosis,”<br />
McGuirk said. “At the end of the day they’re still a patient and need care.”<br />
McGuirk said early on the nurses at HCS were asked if and when they got patients with<br />
COVID-19 who would be willing to add them to their case loads.<br />
“I volunteered because they’re patients that need a nurse, they need care,” she said.<br />
She did so because she considers herself young and healthy at the age of 27, and knows<br />
there are some older nurses on staff that have conditions or are immunocompromised.<br />
When McGuirk goes home for the day, she changes into clothes she leaves in the garage<br />
before heading out for her shift, uses hand sanitizer, and washes her hands thoroughly<br />
once inside.<br />
Branden Howe spends two or three days a week going into homes in his role as<br />
residential supervisor for Monadnock Worksource. He used to conduct in home visits<br />
every day before transitioning into a managerial role.<br />
While the threat of COVID-19 is on Howe’s mind, he’s more concerned with the<br />
individuals he and the staff work with on a weekly basis. After the pandemic, Monadnock<br />
Worksource reduced the number of hours it spends with individuals, which ranges from<br />
11 to 30 hours each week, executive director Janis King said.<br />
They put a stop to transportation because “we can’t provide that safe distance,” King said,<br />
and a number of the places where individuals held jobs or volunteered were suspended<br />
for the time being. And that kind of disruption to the routine is concerning for Howe –<br />
even more so than the looming threat of coronavirus.<br />
But at the top of his priority list is making sure he takes the proper precautions to keep<br />
from getting sick.<br />
“I’m doing everything I can to maintain my health,” Howe said. “Because keeping myself<br />
healthy is part of this.”<br />
Howe said in certain instances they would use PPE during in home care, but now it is<br />
used with every visit.<br />
“It’s been working, but every day is different and has challenges,” Howe said.<br />
But for Howe, it’s just the nature of the job.<br />
“Our job is challenging, but people who do direct care are really invested in the<br />
individuals they support,” Howe said.<br />
Question: Can an RN remove a spinal catheter?<br />
BON Response: Yes, an RN can remove spinal catheters under the<br />
direct order of a physician or APRN, after training and demonstration of<br />
competency.<br />
Question: Can an LNA apply a tourniquet?<br />
BON Response: Yes, an LNA can apply a tourniquet based on training and<br />
demonstration of competency.<br />
Question: Is it within nurse’s scope of practice to calculate a<br />
CMADVASC Score?<br />
BON Response: Yes, it is within the scope of practice of registered nurses<br />
to calculate screening exam scores.<br />
Question: Can a school nurse provide over-the-counter medications without<br />
a provider’s order?<br />
BOD Response: Yes, the school nurse does so in accordance with nursing<br />
knowledge, judgment, and skill and 2. The school nurse in public schools<br />
must follow the NH DOE administrative rule, Ed 311 which states “nonprescription<br />
medication shall be given only with the written request and<br />
permission of the parent and/or guardian” and must follow local policy and<br />
procedures.<br />
Question: Is it within the scope of practice of a RN to remove pins postoperatively<br />
from a patient with a ligament construction?<br />
BOD Response: No, the Board found no research to support the removal of<br />
pins from a site status post ligament reconstruction and tendon interposition<br />
skill as part of the RN scope of practice.<br />
Join a dynamic, caring organization and grow your career<br />
while making a difference in the lives of our residents.<br />
• Resident focused with higher than average<br />
staff-to-resident ratios<br />
• Tuition reimbursement<br />
• Growth opportunities for RNs, LPNs, MNAs and LNAs<br />
Call RiverWoods Exeter at 603.658.1541<br />
or visit RiverWoodsExeter.org/careers<br />
The Board of Nursing is now requiring nursing programs to provide an<br />
analysis of student retention rates and steps to improve retention rate in their<br />
annual reports to the Board.
Page 12 • <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s <strong>June</strong>, July, August <strong>2020</strong><br />
Nurses on the Web<br />
Cheshire Nurses<br />
Interviewed<br />
Ashley Thompson, RN<br />
and Chastity Hodgson,<br />
RN in Cheshire’s<br />
Emergency Department<br />
were interviewed for<br />
the Cheshire Medical<br />
Centers magazine<br />
Health and Wellness.<br />
Elliot Nurse Interviewed<br />
Mary Seigle RN, a<br />
Resource Nurse, in the<br />
CICU at Elliot Health<br />
System was interviewed<br />
for the Elliot Hospital<br />
website. Regarding<br />
caring for COVID-19<br />
patients she noted “It’s<br />
extremely hard and wonderful all at the same time. I will<br />
now forever cry when I hear ‘Here Comes the Sun’ by the<br />
Beatles. That song is played when a COVID-19 patient is<br />
discharged from the hospital and nurses line the hallway to<br />
say goodbye.<br />
Memorial Hospital Pins <strong>New</strong> Graduates<br />
While the COVID-19 pandemic has caused many school<br />
graduations to be cancelled, the nursing staff at Memorial<br />
Hospital made sure to honor their graduating student<br />
nurses with a traditional ceremony welcoming these<br />
new nurses to their profession. “A pinning ceremony is<br />
an invitation to graduates to join the nursing profession,”<br />
said Shauna Ross, RN, a member of the Memorial staff.<br />
“These students have all done their clinical rotations here<br />
and have worked hard.” Each of the students was awarded<br />
a pin. Usually, the nursing pin represents the student’s<br />
nursing school. Since their school pins were not available,<br />
Memorial awarded pins usually presented to recognize<br />
outstanding service by employees. Students also recited the<br />
Nightingale Pledge, promising to “practice my profession<br />
faithfully.” Joining them were a dozen or so other hospital<br />
nurses gathered to congratulate these new professionals<br />
and also reflect on their own service as nurses. Memorial<br />
Hospital Chief Nursing Officer Kris Dascoulias noted<br />
“Nursing is a profession that requires extreme knowledge<br />
and a willingness to put others above yourself. As you start<br />
your journey, remember you are not alone. As a nursing<br />
graduate, you have earned the right to wear a nursing pin.”<br />
Memorial has extended job offers to all of their graduating<br />
student nurses, an acknowledgement of the quality of this<br />
class and the way they have handled the extraordinary<br />
circumstances of their final semester.<br />
Graduates from White Mountains Community College<br />
included Natalie Harmon, Paige Lautenschlager, Emily<br />
Fournier, Nicholas Dukehart, David Frankowski, Amy<br />
Lindgren, Chelsea Schribner and Michael Kane. Elizabeth<br />
Hockmuth was a student at the University of Southern<br />
Maine:<br />
SNHMC Nurse<br />
Irene Arevalo BSN RN was recently highlighted on the<br />
Rivier University website. An alumnus, she practices at<br />
Southern <strong>New</strong><strong>Hampshire</strong> Medical Center. “Never would<br />
I have thought I would be part of a pandemic let alone<br />
working on the very front line. But here we are. I must say<br />
we are doing a decent job in <strong>New</strong> <strong>Hampshire</strong> flattening<br />
White River Junction, VT VA Medical Center<br />
is seeking experienced Registered Nurses for the following clinical areas:<br />
Nurse Manager OR • Asst. Nurse Manager Addiction Treatment<br />
• Asst. Nurse Manager Mental Health • Night/Weekend Hospital Nursing Supervisor<br />
• ED • Primary Care • Med/Surg • OR • Occupational Health<br />
Other vacancies include: NP/PA (Float positions)<br />
• LPN (Dermatology, TeleHealth) • Nursing Assistants<br />
To learn more contact Regina.Radikas@va.gov OR look on USAJOBS.GOV<br />
RNs who join our team receive excellent benefits including:<br />
• 26 annual and accruable paid vacation days<br />
• 13 annual and accruable sick days<br />
• 10 paid Federal holidays<br />
• Retirement thrift savings plan with matching dollars<br />
• Tuition reimbursement after one year of<br />
employment for qualified employees<br />
I'm not just a nurse.<br />
I'm inventing a new<br />
model of health care.<br />
the line. The only thing we<br />
as healthcare providers<br />
can ask is for people to<br />
hang tight, continue staying<br />
home, and please pray<br />
and support your front line<br />
workers because although<br />
now called heroes, we<br />
are people just like you.<br />
Working directly with<br />
COVID patients has been<br />
challenging in many ways, but also rewarding in many<br />
others. I feel that nursing care has become more essential<br />
than ever in the care of patients, as things change quickly<br />
and unexpectedly. It brings me so much joy when a<br />
patient finally begins to improve, especially when we can<br />
celebrate the little things such as going for a short walk<br />
or taking a much-needed shower on their own. But the<br />
biggest cheers come with the discharge paperwork and the<br />
wheelchair ride to the car.”<br />
Maternity Nurse<br />
Hollyann DeCarteret,<br />
BSN, RN, a maternity<br />
nurse at Elliott Hospital,<br />
was profiled on the River<br />
University website. “It’s an<br />
ever-evolving situation<br />
and we are all trying to<br />
roll with the punches. I<br />
am a nurse and I<br />
absolutely love what I do.<br />
It’s a scary and emotional time, but in healthcare, we all<br />
have each other’s back and we are helping to rally each<br />
other. We are a family. We smile with our eyes (because<br />
you can’t see our mouths) and continue to care with every<br />
bit of our hearts.”<br />
Public Health Nurse on<br />
the Front Line<br />
Rivier University alumna<br />
Bobbie Bagley, RN is the<br />
Director of Public Health<br />
and Community Services<br />
in Nashua. In her profile<br />
on the school’s website<br />
they note that Bagley has<br />
been on the front line of<br />
the COVID-19 pandemic<br />
for weeks, working with<br />
City officials and others to keep the community informed,<br />
prepared, and safe. “My job is to promote, preserve,<br />
and protect the health of our community and to lead the<br />
community response to emergent public health issues.<br />
The joint response to COVID-19 has been absolutely<br />
phenomenal. Everyone is working together including the<br />
City of Nashua, the Office of Emergency Management,<br />
hospitals, schools, and faith-based organizations. Together,<br />
as a community, we can stop the spread of COVID-19.”<br />
NHNA Nurse<br />
NHNA’s own Executive<br />
Director Joan Widmer,<br />
RN was profiled on<br />
the Rivier website.<br />
Joan has been keeping<br />
<strong>New</strong> <strong>Hampshire</strong> nurses<br />
informed regarding the<br />
COVID-19 pandemic.<br />
“The NHNA is<br />
addressing concerns raised from nurses around the state,<br />
staying informed on COVID-19 updates from the CDC,<br />
NH Department of Health and Human Services and the<br />
American Nurses Association and communicating this<br />
information through e-flashes and our website.”<br />
DHMC Nurse<br />
Danielle Finn, RN of<br />
DHMC was interviewed<br />
by ABC news. She<br />
speaks Portuguese and<br />
recently translated<br />
for a patient in the<br />
COVID-19 unit in<br />
addition to preparing<br />
language signs to assist<br />
Danielle Finn and<br />
DHMC co-workers.<br />
in communication.<br />
Fenn, who is originally<br />
from Brazil, was living in Germany before she came to the<br />
United States in 2004 to be with her late husband. Now,<br />
her international roots are playing an instrumental role in<br />
caring for her patients.
<strong>June</strong>, July, August <strong>2020</strong> <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s • Page 13<br />
From the Bookshelf<br />
CURE COTTAGES OF SARANAC LAKE:<br />
Architecture and History of a Pioneer Health Resort<br />
by Philip L. Gallos, 1985<br />
Reviewed by Anita Pavlidis RN MSN<br />
For seventy years the name Saranac Lake was<br />
synonymous with tuberculosis. It meant mortal<br />
dread and at the same time transcendent hope. The<br />
only treatment available for the disease was both<br />
researched and dispensed in the isolated village in<br />
<strong>New</strong> York State’s Adirondack Mountains.<br />
Between 1873 and 1945, Saranac Lake, <strong>New</strong> York<br />
became a world-renowned center for the treatment<br />
of tuberculosis, using a treatment that involved<br />
exposing patients to as much fresh air as possible<br />
under conditions of complete bed-rest. In the<br />
process, a specific building type, the "Cure Cottage"<br />
was created.<br />
As a young man Dr. Edward Livingston Trudeau<br />
(1848–1915), watched his elder brother die of<br />
tuberculosis over a period of three months– at the<br />
time, the disease was incurable. He subsequently<br />
trained as a doctor, and, three years after<br />
completing his studies, was himself diagnosed with<br />
tuberculosis. Conventional thinking of the time<br />
called for a change of climate, and he went to live<br />
in the Adirondack Mountains, spending as much<br />
time as possible in the open, and he subsequently<br />
regained his health. In 1876 he moved to Saranac<br />
Lake and established a medical practice. In 1882,<br />
Trudeau read about success in treating tuberculosis<br />
with the "rest cure" in cold, clear mountain air.<br />
Following this example, Trudeau founded the<br />
Adirondack Cottage Sanitarium in February, 1885.<br />
With the fresh air treatment a whole technology<br />
developed and a building type known locally as a<br />
“cure cottage” developed. The requirement for fresh<br />
air lead Trudeau to avoid large institutional settings,<br />
feeling that a cottage-like structure would maximize<br />
the patient's exposure to light and air, and avoid the<br />
sanitation difficulties of a large institutional setting.<br />
Consequently, as the town's increasing fame drew<br />
more and more invalids, "cure cottages" began to<br />
spring up throughout the town. Many were created<br />
by simply adding glassed-in porches to existing<br />
houses. Others were built as cure cottages and/or<br />
apartment buildings, but all had "cure porches" with<br />
sliding glass windows, in which patients spent at<br />
least eight hours a day resting on special day beds<br />
or reclining chairs.<br />
The discovery that tuberculosis was contagious<br />
further contributed to Saranac Lake's importance<br />
as a cure center, as many other venues in the<br />
Adirondacks began to turn "consumptives" away. As<br />
a result, the village grew rapidly, from 533 in 1880<br />
to 1,582 in 1890 to a peak of more than 6,000 by<br />
1920. A number of different types of institutions<br />
developed: boarding houses and cottages, for<br />
relatively ambulatory patients; cottages that did<br />
not provide board, in which case meals would be<br />
provided by a nearby boarding cottage; "nursing<br />
cottages" for patients too weak to get around.<br />
Tuberculosis did not respect wealth or position;<br />
all levels of society were represented, from the<br />
first factory girls to scions of nationally prominent<br />
families.<br />
World War I caused another major increase in<br />
patients— the stress of war and the damage caused<br />
by mustard gas provided fertile ground for the<br />
tuberculosis bacillus. In 1944, an effective drug,<br />
streptomycin, was developed, and by the mid-<br />
1950s, sanatorium treatment of tuberculosis was<br />
nearly entirely supplanted by drug treatment. Many<br />
of the cure cottages were converted into apartment<br />
houses, and some were torn down; some have been<br />
lovingly restored, and some badly renovated.<br />
Christy Mathewson "Cure Cottage" in Saranac<br />
Lake, <strong>New</strong> York. Taken by Mwanner.<br />
This book is of interest to history buffs, researchers<br />
wishing to understand the outdoor life once lived at<br />
Saranac Lake, and to architectural historians tracing the<br />
influence of that life on buildings all over the United<br />
States. The book was an interesting read however, the<br />
writing was methodical and detailed. Considerable space<br />
was devoted to the architecture and history of many<br />
of the cottages. It is a book that you can pick up and<br />
read and put down over a period of time, reflecting on<br />
the dark thread of tuberculosis throughout the fabric of<br />
American Life.<br />
The exploits of Saranac Lake parallel those of <strong>New</strong><br />
<strong>Hampshire</strong>. The Glencliff Home for the Elderly, located<br />
in the White Mountains, was formerly the Glencliff<br />
Sanatorium, which opened in the summer of 1909 for<br />
<strong>New</strong> <strong>Hampshire</strong> residents infected with tuberculosis<br />
seeking respite and cure in the fresh mountain air.<br />
The <strong>New</strong> <strong>Hampshire</strong> State Sanatorium was located at<br />
Glencliff because the site's elevation of 1,650 feet would<br />
provide the fresh mountain air that was then thought to<br />
be therapeutic for tuberculosis patients. Glencliff was<br />
a self-sufficient community, designed to maintain the<br />
isolation that was part of the sanatorium concept. Its<br />
medical facilities included a hospital unit, an open ward,<br />
an x-ray facility, an operating room, and a microbiology<br />
laboratory. The campus encompassed 500 acres and<br />
included a farm with pigs and cows and a vast vegetable<br />
garden. Electricity, water, and sewage disposal were<br />
all provided by the nearby town of Glencliff. Coal was<br />
brought to the base of the mountain by train until the<br />
HUMOR ME<br />
Regularly exercising our sense of humor improves<br />
resiliency, positivity and balances anti-negatively.<br />
Laughter may not solve problems but can change<br />
your chemistry allowing you to face them anew. In this<br />
issue we present one-liners related to the COVID-19<br />
pandemic.<br />
• What should you do if you don’t understand a<br />
coronavirus joke? Be patient.<br />
• If you need 144 rolls of toilet paper for a 14 day<br />
quarantine you probably should have seen a doctor<br />
long before COVID-19.<br />
• With hair salons, nail salons, waxing centers, tanning<br />
places and barbershops closed, it’s about to get ugly<br />
out there.<br />
• What’s the best way to avoid touching your face? A<br />
glass of wine in each hand.<br />
• Sign on a dating site: Single man w/TP seeks single<br />
woman w/Purell for good clean fun.<br />
• Grocery shopping has become a real life version of<br />
PAC-Man. Avoid everyone, get the fruit, and take<br />
any route to avoid contact.<br />
• Man looking at his calendar: Can’t wait until<br />
tomorrow. I have another big day of hand washing<br />
and looking out the window planned.<br />
railroad was discontinued in 1952. The sanatorium even<br />
had its own shortwave radio station. The sanatorium<br />
treated more than 4,000 TB patients during its first 50<br />
years. When the outlook for patients with tuberculosis<br />
changed due to drug therapy Glencliff sent its last active<br />
tuberculosis patient to the Mary Hitchcock Hospital<br />
in Hanover, ending the sanatorium movement in <strong>New</strong><br />
<strong>Hampshire</strong>.<br />
In 1970, the Glencliff Sanatorium was converted into<br />
the Glencliff Home for the Elderly. Many of the unique<br />
architectural features of the original facility have been<br />
preserved. The main patient building still has its floorto-ceiling<br />
windows that admit ample light. The sturdy<br />
columns that used to support the screened porches<br />
which were used for the open-air treatments have now<br />
been framed in to create patient rooms.<br />
Fresh air porch at Glencliff Sanatorium<br />
The themes of both the book and story of Glencliff<br />
Sanatorium are much the same as the COVID-19 world<br />
we live in today. Patients experienced isolation, sickness,<br />
loneliness, separation from family and friends, fear of<br />
never recovering, and loss of income/jobs. For many<br />
years, there was no effective treatment and worry about<br />
the patients returning to society as their health improved<br />
but were not cured of tuberculosis. But this period did<br />
end and although there was a tremendous loss of lives,<br />
people survived this time and met the challenges of that<br />
terrible time. We shall too.<br />
Anita Pavlidis, RN MSN was the former Director of<br />
Nursing at the NHTI, Concord’s Community College<br />
and Program Specialist at the <strong>New</strong> <strong>Hampshire</strong> Board of<br />
Nursing.<br />
• Nobody thought I’d amount to anything. But here I<br />
am lying on the couch, saving the world.<br />
• In 2021: Human Resources: I see a gap in your<br />
resume. What were you doing in <strong>2020</strong>? Job hunter:<br />
Looking for toilet paper.<br />
• We are about three weeks away from finding out<br />
what everyone’s real hair color is.<br />
• Thinking a mask is going to stop COVID-19 is the<br />
same as thinking that your underpants will protect<br />
everyone from a fart.<br />
• Half of us are going to come out of the quarantine as<br />
amazing cooks. The other half will come out with a<br />
drinking problem.<br />
• Some of us need to practice social-distancing from<br />
the refrigerator.<br />
• Public Service Announcement: Every few days try<br />
your jeans on, just to make sure they fit. Pajamas will<br />
have you believe all is well in the kingdom.<br />
• Day five of homeschooling: Which one of you<br />
called in a bomb threat?<br />
• A dog owner: Now I know why dogs are so excited<br />
to go for walks.<br />
• A cat owner: My cat is still trying to figure out why<br />
I’m in his house after 8 AM.
Page 14 • <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s <strong>June</strong>, July, August <strong>2020</strong><br />
WELCOME NEW and RETURNING NHNA MEMBERS!<br />
NHNA welcomes these new and returning members. Thank you!!! What do these 67 nurses and over 1,100 NHNA members know that you don’t?<br />
If you are not a member ask your neighbor on this list why they joined! Go to nhnurses.org where joining is easy and one of the best professional values<br />
for your money! We want to see your name here in the next issue of the NH Nursing NEWS!<br />
Allenstown, NH<br />
Tiffany Hutchins<br />
Atkinson, NH<br />
Charlotte Dimaggio<br />
Auburn, NH<br />
Angela Diorio<br />
Bedford, NH<br />
Julia Duquette<br />
Boscawen, NH<br />
Brooke McLain<br />
Bow, NH<br />
Sally J. Jenkins<br />
Brentwood, NH<br />
Sarah Dinneen<br />
Claremont, NH<br />
Odalie Bernash<br />
Concord, NH<br />
Susan Bryant<br />
Mary Elizabeth Cahan<br />
Dorothy Michelle<br />
DeLisa<br />
Derry, NH<br />
Dawn LaPorte<br />
Stephanie Russo<br />
Barbara Sullivan<br />
Dover, NH<br />
Jeanne Spurlin<br />
Laura Willett<br />
Elkins, NH<br />
Shari Goldberg<br />
Goffstown, NH<br />
Julianne M. Ashton<br />
Hampton, NH<br />
Nicole Susan<br />
Leibundgut<br />
Hooksett, NH<br />
Sabrina Bolianites<br />
Hudson, NH<br />
Elizabeth Duffy<br />
Elizabeth Martell<br />
Intervale, NH<br />
Jennifer Leigh Grise<br />
Keene, NH<br />
Margo Helen Banks<br />
Rachel Hough<br />
Laconia, NH<br />
Deborah E. Bossey<br />
Lebanon, NH<br />
Nadine Nicola Brown<br />
Dayhna Pamela Marti<br />
Ojeda<br />
Janice E. Morton<br />
Lee, NH<br />
Suellen Olson Drake<br />
Lisbon, NH<br />
Sean Destephanis<br />
Littleton, NH<br />
Bailey Dammen<br />
Manchester, NH<br />
Melinda Daigle Bennet<br />
Martha Derkach<br />
Mirline Estiverne<br />
Kathleen Fantozzi<br />
Kathleen Bridget<br />
Forbush<br />
Jessica Gluek<br />
Pamela Lee Gomes<br />
Cindy T. Louxay<br />
Jessica McCardell<br />
Claude Mua<br />
Kim Ozuna<br />
Hannah Pirozzoli<br />
Melissa Vitagliano<br />
Merrimack, NH<br />
Julie Brady<br />
Nashua, NH<br />
Tammi Boudreau<br />
Mellony Cude<br />
Alana Evans<br />
Emily Madison<br />
Lily Roselin Raja<br />
<strong>New</strong> Boston, NH<br />
Emma Angeline Pinard<br />
<strong>New</strong> Hampton, NH<br />
Jaimie N. Walton<br />
<strong>New</strong>ton, NH<br />
Tina Greenwood<br />
Northfield, NH<br />
Michele Ann Murphy<br />
Taylor Thompson<br />
Penacook, NH<br />
Cynthia Bergeron<br />
Peterborough, NH<br />
Brittany Stokes<br />
Plainfield, NH<br />
Sunshyne <strong>June</strong> Rice<br />
Plymouth, NH<br />
Paula Michelle Hurvit<br />
Moulton<br />
Rindge, NH<br />
Donna J. Babb<br />
Salem, NH<br />
Brittany Burke<br />
Bethany A. Pelletier<br />
Stratham, NH<br />
Ericka J. McCarron<br />
Sunapee, NH<br />
Arlene M. Halsted<br />
Thornton, NH<br />
Kimberly Ann Thibault<br />
Wolfeboro, NH<br />
Dara St. Sauveur<br />
Woodsville, NH<br />
Dina Quinn<br />
Nurse in Key Role in <strong>New</strong> Geriatric Program<br />
Dartmouth-Hitchcock Medical<br />
Center (DHMC), in partnership<br />
with West Health of Lebanon,<br />
has launched a three-year<br />
effort to build a hub and spoke<br />
model Geriatric Emergency<br />
Department (GED) aimed at<br />
keeping most geriatric patients<br />
in their communities through<br />
telemedicine. A key player<br />
in the development of this<br />
innovative approach to caring<br />
for geriatric patients in northern<br />
<strong>New</strong> <strong>Hampshire</strong> is Hilary<br />
Hawkins, BSN, RN, Geriatric<br />
Emergency Department<br />
Manager at DHMC. Hawkins<br />
is responsible for developing<br />
Hilary Hawkins,<br />
BSN, RN, Geriatric<br />
Emergency<br />
Department Manager<br />
at DHMC.<br />
care protocols and implementing screening tools to assess<br />
the needs of the geriatric patient. “The idea behind [the<br />
3 rd SHIFT LNA’s WANTED!<br />
Full-time positions, 10pm-6am<br />
Great starting pay with raise in 90 days! Excellent benefit<br />
package for those who qualify including health, dental,<br />
life, 401k with employer match, disability, prepaid<br />
legal, weekend & shift differentials, referral & longevity<br />
incentives, generous PTO plan, professional development<br />
reimbursements and more!<br />
Must have valid NH LNA license.<br />
Please apply online at<br />
www.websteratrye.com<br />
GED] is DHMC (the hub) has many resources such as case<br />
managers, social workers, pharmacists and geriatricians that<br />
can help community hospitals (spokes) with the geriatric<br />
population, to keep them in their community hospitals or<br />
their homes,” states Hawkins. Research has demonstrated<br />
that admitting geriatric patients can often lead to additional<br />
risks versus maintain them in their home or community. Of<br />
course, if these patients need to be at DHMC they will be<br />
welcomed.<br />
Hilary Hawkins, BSN, MBA, RN, CEN, CPEN, TNRN<br />
always knew she wanted to be in health care. Her father<br />
was a nursing home administrator and she spent time there<br />
growing up. “I first started in healthcare in EMS and then<br />
obtained my BSN. As a nurse, I have worked in the adult<br />
intensive care unit, the emergency department, trauma<br />
performance improvement and then running trauma<br />
programs. Statics show that trauma in NH is predominantly<br />
65 years and older which led me to work closely with<br />
palliative care, hospice and ethics committees,” remarks<br />
Hawkins. Hawkins is certified in Geriatric Emergency<br />
Nursing Education (GENE), as designated by the Emergency<br />
Nursing Association, the leading professional organization<br />
for emergency nurses.<br />
“We’re delighted to have Hilary’s insight, experience<br />
and expertise so tightly woven into the development of<br />
our GED,” says Karen Clements, RN, FACHE, D-H Chief<br />
Nursing Officer. “This investment will have a lasting<br />
positive impact on our patients and our communities,<br />
and for that reason it’s absolutely imperative that we have<br />
qualified nurses, like Hilary, so closely engage in what we’re<br />
creating.”<br />
GED nurses are aware of the nuances in care required<br />
by geriatric patients, including the need for additional<br />
assessments to detect underlying issues with mental<br />
health, physical health or in need of additional resources.<br />
“They work closely with care management to ensure that<br />
the patient has the appropriate resources or equipment at<br />
home and that they understand their discharge plans or<br />
follow up,” notes Hawkins. GED nurses also ensure that the<br />
patient is receiving the care that matters most to them. Most<br />
often that care is at home.<br />
The goal of the GED is to recognize those patients who will<br />
benefit from inpatient care, and to effectively implement<br />
outpatient care to those who do not require inpatient<br />
resources. The GED utilizes additional staffing, equipment,<br />
education, policies and procedures, follow-up care, and<br />
performance improvement measures. When implemented<br />
collectively, the GED hopes to see improvements in patient<br />
care, customer service, and staff satisfaction. Improved<br />
attention to the needs of this challenging population has<br />
the opportunity to more effectively allocate health care<br />
resources, optimize admission and readmission rates,<br />
while simultaneously decreasing iatrogenic complications<br />
and the resultant increased length-of-stay and decreased<br />
reimbursement.<br />
Developing the care protocols the GED will use has been a<br />
multidisciplinary team approach based on evidence. These<br />
disciplines include and are not limited to pharmacists,<br />
nurses, physicians, care managers, social workers, physical<br />
therapists, occupation therapists, as well as community<br />
resources and experts in the area of aging. Additionally, the<br />
team is developing a robust data analysis process that will<br />
guide much of the work going forward and help to identify<br />
quality measures and understand related outcomes.<br />
“The Geriatric Team at DHMC is still working on<br />
developing and refining their processes and the<br />
application,” comments Hawkins. The spoke and hub<br />
implementation has slowed down as resources are needed<br />
to focus on COVID -19. The Geriatric Team continues to be<br />
a presence in the ED during the pandemic and is live-time<br />
providing support to our older families. The Geriatric Team<br />
is also adding their collective experience to the Nursing<br />
Home Collaborative which is meeting to discuss how<br />
nursing facilities can maximize the use of their resources<br />
in the best interest of all patients, and still protect their<br />
residents who are some of our most vulnerable.
<strong>June</strong>, July, August <strong>2020</strong> <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s • Page 15<br />
NCLEX<br />
Reconsidered<br />
Focus on IV<br />
Therapy<br />
Ed Note: Where it has been a year or<br />
years since you took the NCLEX (AKA<br />
“Boards”), how well would you do<br />
now?<br />
1. A patient is receiving an infusion of lactated ringer’s<br />
solution at 100 ml/hr. The IV site appears red with<br />
moderate swelling. The infusion is sluggish as the pump<br />
keeps alarming. The nurse recognizes these findings as:<br />
A. Extravasation<br />
B. Infiltration<br />
C. Phlebitis<br />
D. Occluded catheter<br />
2. The nurse reports a patient’s central venous pressure<br />
as 1mmHG. Which provider order for fluids should be<br />
questioned by the nurse? (Select all that apply).<br />
A. 0.9% NaCl<br />
B. 0.45% NaCl<br />
C. 3% NaCl<br />
D. Lactated Ringers<br />
E. D5LR<br />
3. For which patient would a colloid be administered?<br />
A. A patient with chronic heart failure with slight JVD<br />
and BP 96/50<br />
B. A patient with chronic anemia and Hg/Hct report of<br />
9/31<br />
C. A patient with cirrhosis and pitting edema of the<br />
extremities<br />
D. A patient requiring volume replacement for chronic<br />
diarrhea<br />
4. A home care nurse is conducting a follow-up home visit<br />
to a patient who has been discharged with a parenteral<br />
nutrition (PN). Which of the following should the nurse<br />
most closely monitor in this kind of therapy?<br />
A. Blood pressure and temperature.<br />
B. Blood pressure and pulse rate.<br />
C. Height and weight.<br />
D. Temperature and weight.<br />
5. A patient that has been receiving parenteral nutrition at<br />
80 ml/hr has been cleared to begin a liquid diet. The<br />
nurse expects that which of the following orders?<br />
A. Decrease parenteral nutrition to 40ml/hr.<br />
B. Start 0.9% normal saline at 30 ml/hr.<br />
C. Maintain the present infusion rate.<br />
D. Discontinue the parenteral nutrition.<br />
Answers on page 17<br />
NH Nurses Make It Happen<br />
Elliot ICU nurse Heidi Kukla, right, decided to take<br />
the need for vital PPE into her own hands. She and<br />
other volunteers were working around the clock<br />
in a making-marathon of protective gowns she<br />
designed. (Photo courtesy Elliot Hospital)<br />
Personal protective equipment or PPE has been in<br />
been in short supply in <strong>New</strong> <strong>Hampshire</strong> and across<br />
the country. While Elliot Hospital and Southern <strong>New</strong><br />
<strong>Hampshire</strong> Medical Center, both part of Solution Health,<br />
have been managing supplies and orders in advance<br />
of the surge, isolation gowns have been of particular<br />
concern. With a mix of talent and innovative spirit, some<br />
inspired nurses at Elliot Hospital took on the challenge of<br />
enhancing supplies.<br />
Heidi Kukla, RN, who practices in the Intensive Care<br />
Unit at Elliot developed a pattern for a disposable,<br />
detachable gown. Working with colleagues who<br />
volunteered their time, Kukla developed prototypes that<br />
went to Infection Prevention staff for testing and review.<br />
A socially-distant but unified volunteer crew has<br />
taken over AR Workshop on Elm Street to make<br />
the gowns. (Photo courtesy Elliot Hospital)<br />
Once the teams landed on a design and material that<br />
met the necessary clinical standards, Kukla reached<br />
out to fellow ICU nurse, Stephanie Joyce who had a<br />
strong connection at AR Workshop on Elm Street in<br />
Manchester. Joyce helped AR owner Laura McKelligan<br />
set up the shop, which has been closed because of<br />
the “stay at home” order. McKelligan was more than<br />
happy to open her doors and transformed the crafting<br />
workshop into a gown-making shop. SolutionHealth<br />
purchased materials for the group to create more<br />
gowns to be used at Elliot Hospital and Southern <strong>New</strong><br />
<strong>Hampshire</strong> Health, and McKelligan was able to bring<br />
back some of her staff to help.<br />
“Stephanie asked if the space was being used, and I told<br />
her they were more than welcome. One day turned into<br />
a weekend, and now we are planning for the whole<br />
week,” McKelligan said on Monday.<br />
Kukla says the disposable gowns will cost less than 25<br />
cents/each and the washable gowns will cost about $10/<br />
each. She says volunteer labor was key to keeping costs<br />
down. The group spent the weekend cranking out gowns<br />
at the AR Workshop.<br />
Be Part of<br />
Research<br />
Ed Note: The Nursing <strong>New</strong>s receives requests<br />
from researchers to solicit study subjects or<br />
participants. All studies must demonstrate<br />
evidence of Institutional Review Board approval.<br />
Cynthia Horton Dias RN, a PhD Candidate<br />
at the University of South Carolina is seeking<br />
participants for a research study to understanding<br />
of the experiences of hospital nurses with free<br />
food in the workplace. Qualified participants for<br />
this study are registered nurses (RN), working<br />
at least 50% of the time inside a U.S. hospital<br />
and participation will involve filling out a survey<br />
taking no more than 15 minutes. Participants will<br />
be entered into a raffle for one of two US $100<br />
Amazon gift cards. Once the drawings for the<br />
raffles are completed, email address collected for<br />
the drawing will be deleted. No other personally<br />
identifiable information will be collected in this<br />
study, other than certain demographic measures.<br />
Nurses who meet the study criteria can take<br />
the research survey at this link: https://is.gd/<br />
RNfreefood
Page 16 • <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s <strong>June</strong>, July, August <strong>2020</strong><br />
Due to the coronavirus pandemic, Plymouth State<br />
University (PSU) senior nursing students quickly adjusted<br />
to virtual simulations and other alternative methods to<br />
complete their final semester of clinical training. The nursing<br />
students graduated early – a full month ahead of schedule.<br />
The combination of earlier graduation and the <strong>New</strong><br />
<strong>Hampshire</strong> Board of Nursing issuing temporary licenses to<br />
new graduate nurses allowed healthcare facilities to start<br />
the onboarding process weeks earlier than usual. “This is<br />
especially important now,” said Kim Force, Clinical Director<br />
of Inpatient Services at Littleton Regional Hospital. Seventy<br />
percent of PSU’s nursing graduates expect to become<br />
licensed in <strong>New</strong> <strong>Hampshire</strong>, and many will begin working<br />
at the hospitals where they completed their senior capstone<br />
semesters.<br />
St. Joseph School of Nursing, with approval of the NH<br />
Board of Nursing, has added an evening cohort of 24<br />
students to their associate degree nursing program.<br />
Shannon Murdock a graduating senior nursing<br />
student at the University of <strong>New</strong> <strong>Hampshire</strong> was<br />
honored as a 2019-20 America East Winter Scholar-<br />
Athletes. This was Murdock’s second year as a<br />
Scholar-Athlete. She earned her BSN with a 4.0<br />
GPA in nursing and 3.72 GPA overall. Murdock won<br />
the 5,000 meter track event at the America East<br />
Championship and also placed second in the mile.<br />
The Salter School which offers a program to prepare practice<br />
nurses among other non-licensed health careers was renamed<br />
the American School of Nursing and Medical Careers.<br />
The campus remains in Manchester, <strong>New</strong> <strong>Hampshire</strong>. The<br />
American School of Nursing and Medical Careers is owned by<br />
Premier Education Group, L.P.; registered limited partnership<br />
in the Commonwealth of Pennsylvania.<br />
ED Note: <strong>New</strong>s from nursing schools, faculty,<br />
students or alumni are welcome. Please direct<br />
submissions to office@nhnurses.org with NHNN<br />
in the subject line.
<strong>June</strong>, July, August <strong>2020</strong> <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s • Page 17<br />
Florence Nightingale – Lamp of Scutari<br />
Ed Note: This is the third in a four part series celebrating<br />
the 200th birthday of Florence Nightingale and the Year<br />
of the Nurse<br />
Sue Fetzer<br />
In March 1854, England, France and Turkey declared<br />
war on Russia to protect themselves against the Russian<br />
expansion, marking the beginning of the Crimean War.<br />
England had not been in a foreign war for 40 years and<br />
the 27,000 English troops had gone to Turkey with little<br />
support from a Medical Department.<br />
After accepting, Sidney Hebert’s request, Florence<br />
recruited nurses from the Irish Catholic Sisters of Mercy<br />
(10), Anglican Sisters of Mercy (8), St. John’s House<br />
of the Church of England (6) and 14 lay nurses from<br />
hospitals around London. Together with Florence and<br />
her housekeeper from Upper Harley Street and Mr. and<br />
Mrs. Bracebridge, 41 members of her group departed<br />
London on October 21, 1854. The travelled to Paris then<br />
to Marseilles where they boarded the cargo ship Vectis.<br />
Despite nearly all developing seasickness, they arrived at<br />
Constantinople (today known as Istanbul) on November<br />
4. Constantinople is divided by the Bosporus, a strait of<br />
water connecting the Black Sea to the Mediterranean<br />
and Atlantic Oceans. The French Hospitals were on the<br />
west side, while the British wounded had been taken to<br />
Scutari, on the Asiatic, or east side of the Bosporus.<br />
Florence was given the nursing responsibility of<br />
Superintendent of Hospitals in the East of eight hospitals,<br />
but she spent most of her time at the Barracks Hospital<br />
on the hill overlooking the town of Scutari. The hospital<br />
had been created out of a Turkish army barracks, and the<br />
large square building was nearly a mile in circumference,<br />
three stories tall with towers on each corner. In the<br />
central court up to 12,000 men could exercise. There<br />
was over four miles of corridors for wounded and sick<br />
men to inhabit, up to 2,500 men at a time. The Hospital<br />
was located over a network of cesspools, the sewer<br />
lines were blocked and overflowing into the hallways.<br />
Windows were closed against the cold.<br />
The reception provided to Nightingale and her nurses<br />
was nonexistent. Soon after her arrival Florence<br />
approached the medical officers to offer her services.<br />
Dr. Hall, Inspector General of the Hospital declined.<br />
Most of the medical staff believed the intruders would<br />
be a hindrance. The environment, rats, vermin, the lack<br />
of bedding, clothing, no kitchens, provision for washing,<br />
or medical supplies, they believed was not appropriate<br />
for women. The Nightingale party was quartered in two<br />
floors of one of the Towers.<br />
Twenty-four hours after their arrival, more wounded<br />
arrived from the Battle of Inkerman, across the Black Sea<br />
Answers to NCLEX Reconsidered from page 15<br />
1. C 2. B,C 3. C 4. D 5. A<br />
from Scutari. Wounded men would have to be carried<br />
to the docks, transported by boat, unloaded onto the<br />
docks and transported to the Barrack Hospital. The<br />
ordeal could take up to two weeks. There was little<br />
nourishment during the trip, and little upon arriving at<br />
the hospital. Nightingale’s nurses first set up a kitchen,<br />
and the smell of soup was enough to prompt the<br />
medical officers to allow the group to feed the wounded.<br />
Obtaining and storing supplies was one of Nightingale’s<br />
ongoing efforts. Medical supplies were often rerouted,<br />
not unloaded or stolen. Three different government<br />
agencies were responsible for supplies with little<br />
communication. Food preparation was primitive, boiled<br />
in huge copper pots. Vegetables were rare. There were<br />
no laundry facilities as the boiler had broken. She<br />
wrote home, to the English newspaper Times and to<br />
the officials that had sent her, proclaiming the lack of<br />
supplies and conditions. Soon, supplies were sent to her<br />
directly, and she maintained a ‘warehouse’ in the tower.<br />
Sash worn by one of<br />
the Nightingale<br />
nurses.<br />
From the beginning,<br />
Florence kept track of<br />
the wounded, those<br />
suffering from disease,<br />
and the dead. She hunted<br />
down cleaning supplies,<br />
created kitchens, got<br />
the boilers fixed and<br />
created a laundry. An<br />
oft repeated story relates<br />
that one night, the surgeons triaged five soldiers aside to<br />
die, deeming their condition hopeless. Nightingale got<br />
‘permission’ to care for the men through the night and by<br />
morning they were fit for surgery. She would reply ‘we<br />
must’ to medical officers who would say ‘we can’t.’<br />
The winter of 1855 recorded temperatures at Scutari of<br />
–10 degrees C. The hospital was full of cases of frostbite,<br />
gangrene, and dysentery. Nightingale calculated the<br />
mortality rate of 1,000 per 1,174 men. Nightingale’s<br />
letters to her benefactor in England, Sidney Herbert,<br />
were shared with Queen Victoria who responded.<br />
Nightingale would administer the hospital during the<br />
day and make rounds after the surgeons had retired for<br />
the night. She would carry a small lamp in her hand and<br />
would pause for anyone in need. The practice would<br />
be responsible for her reputation as the “Lady with the<br />
Lamp.”<br />
Turkish lamp of style<br />
used by Nightingale<br />
Cholera, a bacterial<br />
infection from water<br />
or food contaminated<br />
by human waste,<br />
was rampant during<br />
the Crimean War.<br />
Diagnosed by watery<br />
diarrhea, vomiting,<br />
and muscle cramps,<br />
the dehydration and<br />
electrolyte imbalance<br />
resulted in a blueish<br />
tinge to the skin. There<br />
was no cure, only care. Throughout 1855, typhus<br />
fever also ran rampant. Typhus, caused by bacteria<br />
transmitted by flea, mite, louse, or tick bites, results in a<br />
severe headache, fever over 102, rash, hypotension and<br />
photosensitivity. Unfortunately the medical staff and<br />
Florence’s nurses were not immune.<br />
CALLING ALL<br />
Nurses!<br />
Looking for a change? How about sharing your<br />
knowledge and skill by teaching LNA classes!<br />
We are currently hiring Nurses to teach per diem, who meet the following criteria:<br />
• Min. 2 years experience 1 year in LTC and 1 year as a nurse supervising LNA’s<br />
• Strong ability to multi-task• Positive and enthusiastic attitude!<br />
• Team player • Desire to help others learn and grow<br />
You can learn more about us and what we offer,<br />
online at www.LNAHealthCareers.com<br />
Interested candidates should submit a resume<br />
to info@LNAHC.com or fax 603-647-2175.<br />
On May 1855, Florence set out across the Black Sea<br />
for Balaclava to determine how the sick and wounded<br />
were cared for near the fighting front and to inspect<br />
the hospitals. Arriving at the dock was a much different<br />
scene than when she arrived in Scutari six months<br />
previously. Her successes at the Barracks Hospital were<br />
well known, and some of the men she had cared for had<br />
returned to the front lines. While on this trip, Florence<br />
is stricken with Crimean fever. While historians have<br />
debated the cause, it was most likely brucellosis, a<br />
bacterial infection transmitted from animals by ingestion<br />
of raw milk, infected food or contact with an infected<br />
animal. Symptoms include fever, sweats, headaches,<br />
back pains, and physical weakness. One form of the<br />
illness may also cause long-lasting symptoms, including<br />
recurrent fevers, joint pain, and fatigue, complaints that<br />
Florence would manifest for the rest of her life.<br />
After a month being cared for by her own nurses,<br />
Nightingale returned to Scutari for additional<br />
recuperation, by August she was back administering the<br />
Barracks Hospital. Her recovery was heralded in England<br />
as a heroic. In November, Florence received a letter and<br />
gift from Queen Victoria. Designed by Prince Albert, the<br />
brooch with the inscription “Blessed are the merciful,”<br />
the word “Crimea” and a St. George cross surmounted<br />
by a crown of diamonds. A Crimean Peace was declared<br />
in March, 1856, but the hospitals did not close until the<br />
summer. Florence left Turkey late in July traveling as<br />
‘Miss Smith;’ she arrived at Lea Hurst unnoticed.<br />
The Florence<br />
Nightingale brooch<br />
bestowed by Queen<br />
Victoria in 1855<br />
served as the<br />
inspiration for the<br />
current nursing pin<br />
bestowed on nursing<br />
schools graduates.<br />
Despite her success<br />
during 20 months in<br />
Scutari, Nightingale felt<br />
she had failed to reform the Medical Department of the<br />
Army. Although, she was comforted in the thought that<br />
she met her calling to do “God’s work.” At 36 years old,<br />
she saw her achievements as starting point for her future<br />
work.<br />
Upon returning from<br />
the Crimea,<br />
Nightingale’s hair has<br />
started to grow back<br />
after being cropped<br />
short during her<br />
experience with<br />
Crimean Fever.<br />
Next Issue: Florence Nightingale – Shaping the Profession<br />
RN 2nd Shift Supervisor Needed – Charge Nurse Role<br />
Are you a nurse looking for a position in which you have an<br />
opportunity to not only provide exceptional care, but also make a<br />
positive difference in the life of another? If so, please consider joining<br />
us at the Rose Meadow Group! Our 16-bed programs provide care<br />
to individuals with acquired brain injury, spinal cord injury, and other<br />
neurological diseases in a home-like, residential setting.<br />
The RN Charge Nurse position will have a consistent schedule<br />
(Monday-Friday, 4pm to Midnight) and is well suited for new nursing<br />
graduates OR more tenured nurses looking to provide care in an<br />
environment where they can truly get to know the needs of our<br />
individual residents. Our ideal candidate will possess a high degree<br />
of empathy, compassion, and a willingness to work as a team with<br />
other like-minded nurses and caregivers.<br />
A valid, current RN Licensure is required.<br />
If interested, please email your resume<br />
and salary requirements to:<br />
hr@rosemeadowgroup.com
Page 18 • <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s <strong>June</strong>, July, August <strong>2020</strong><br />
IN MEMORY OF OUR COLLEAGUES<br />
The <strong>New</strong> <strong>Hampshire</strong> Nurses Association honors the<br />
memory of and acknowledges the work of deceased<br />
nurses who have graduated from <strong>New</strong> <strong>Hampshire</strong><br />
nursing schools or who have actively practiced in<br />
<strong>New</strong> <strong>Hampshire</strong> during their career. Sharing the<br />
names and information about these nurses is one way<br />
we honor their contribution to the profession. Brief<br />
submissions are welcome.<br />
Navy Nurse<br />
Barbara A. Cirincione, 86, formerly of<br />
Manchester and Holderness, died on<br />
Februrary 14, <strong>2020</strong>. She proudly served<br />
in the U.S. Navy as a nurse. Before<br />
retiring, Barbara worked as an APRN<br />
for Elliot Hospital. She was especially<br />
proud to serve as the parish nurse at<br />
her local church for many years. Barbara was also a<br />
camp nurse for the American Diabetes Association<br />
Insurance Nurse<br />
Louise C. Marchand, passed away<br />
February 14, <strong>2020</strong>, After high school<br />
she was a manager of dental offices<br />
and at age 40 decided to change her<br />
career path. She graduated from NHTI<br />
with her AD degree and practiced in<br />
Manchester area hospitals. Later, after<br />
earning her National Case Management Certification,<br />
Louise became an administrative insurance nurse first<br />
for Cigna and later for Alicare Medical Management,<br />
where she worked at the national level managing<br />
complex cases.<br />
Sacred Heart Grad<br />
Marlene Eudora (Cilley) Eddy, 72, died<br />
February 19th, <strong>2020</strong>. She was a native<br />
of Concord, graduating from Sacred<br />
Heart Nursing School. With a 40+ year<br />
career as an RN, she retired from<br />
Havenwood Heritage Heights in 2011.<br />
NursingALD.com can point you<br />
right to that perfect NURSING JOB!<br />
NursingALD.com<br />
Free to Nurses<br />
Privacy Assured<br />
Easy to Use<br />
E-mailed Job Leads<br />
REGISTERED NURSES<br />
Full Time & Part Time – All Shifts<br />
Psychiatric Specialty Areas:<br />
Young Adult, Adult, Geriatric & Crisis Stabilization<br />
Competitive Benefits & Pay Scale<br />
Extensive Paid Orientation<br />
Recent Graduates Welcome!<br />
View job specifications and how to apply<br />
for external RN postings:<br />
http://das.nh.gov/jobsearch/Employment.aspx<br />
<strong>New</strong> <strong>Hampshire</strong> Hospital<br />
NH Department of Health and Human Services<br />
36 Clinton Street Concord, NH 03301<br />
Human Resources 603-271-5855<br />
LPN<br />
Rachel M. (Snow) Crane, 82, of<br />
Hillsborough, passed away on February<br />
22, <strong>2020</strong>. As an LPN she worked for<br />
Hillsboro House Nursing Home and<br />
Hillsboro Visiting Nurses Association.<br />
Gero Nurse<br />
Rita A. Latham, 91, died on February<br />
22, <strong>2020</strong>. She obtained her nursing<br />
diploma in Massachusetts and as a<br />
Concord native practiced at Concord<br />
Hospital. For many years she was a<br />
nursing supervisor at McKerly’s Nursing<br />
Home, and in 1992 opened the first<br />
Adult Medical Day Care center in NH where she<br />
practiced for nearly 20 years.<br />
Public Health Expert<br />
Kathleen A. (Katie) Dunn 61, died on<br />
February 20, <strong>2020</strong> after a courageous<br />
three year battle with brain cancer. She<br />
obtained her nursing diploma at the<br />
Concord Hospital School of Nursing<br />
where she graduated as valedictorian.<br />
She earned a BS from <strong>New</strong> England<br />
College in Psychology and Sociology and a MPH from<br />
Boston University School of Medicine, School of<br />
Public Health. She practiced at Concord Hospital for<br />
twenty years as an ICU/CCU, PACU RN. She<br />
supervised ER Admitting. She opened the <strong>New</strong><br />
<strong>Hampshire</strong> office of the <strong>New</strong> England Organ Bank.<br />
She spent 23 years employed by the State of <strong>New</strong><br />
<strong>Hampshire</strong>. Beginning in Maternal and Child Health as<br />
a nurse consultant, bureau Chief of Communicable<br />
Disease, and Director of Public Health. She was<br />
Associate Commissioner of Health and Human<br />
Services. One of her career highlights was writing the<br />
CHIP (Children’s Health Insurance Program), a pilot<br />
program for the country, under then Governor Jeanne<br />
Shaheen. She was a compassionate advocate for the<br />
disabled and their families. Her career concluded as<br />
Senior Program Director for the National Academy of<br />
State Health Policy in Portland, Maine and<br />
Washington, DC. She was a Robert Wood Johnson<br />
Medicaid Leadership Fellow.<br />
Gero Nurse<br />
Rita P. Annicchiarico died peacefully<br />
on March 8, <strong>2020</strong> She earned a nursing<br />
diploma in 1951 and practiced in<br />
private duty as well as a nurse at the<br />
former Centennial Home.<br />
Mary Hitchcock Grad<br />
Ethel Amy (Norcross) Crane, 86, died<br />
on March 11, <strong>2020</strong> after a long hardfought<br />
battle with dementia. She<br />
received her nursing diploma in 1955<br />
from Mary Hitchcock Memorial School<br />
of Nursing. She practiced at the State<br />
Hospital and Concord Hospital in<br />
Concord, the <strong>New</strong>port Hospital in <strong>New</strong>port, NH,<br />
Hillsboro House Nursing Home and the Office of Dr.<br />
Richard Douglass in Hillsboro, NH.<br />
Sacred Heart Grad<br />
Maryanna (Casey) Commerford, 85,<br />
died March 12, <strong>2020</strong> at the CRVNA<br />
Hospice House in Concord surrounded<br />
by her children. She obtained her<br />
nursing diploma from Sacred Heart<br />
Hospital School of Nursing. She had a<br />
long career as a Registered Nurse, practicing at<br />
Concord Hospital and St. Paul’s School.<br />
Founding Nursing Educator<br />
Barbara “Ann” Manchester Kelley, 85,<br />
died on March 14, <strong>2020</strong>. Ann received<br />
her nursing diploma in 1955 from Peter<br />
Bent Brigham Hospital School of Nursing<br />
in Boston and her master’s degree in<br />
nursing education from Boston<br />
University. She moved to the University<br />
of <strong>New</strong> <strong>Hampshire</strong> in 1964 to help develop a new<br />
baccalaureate nursing program. As a founding nursing<br />
faculty member, she remained on the faculty until her<br />
retirement in 1998. Ann was a highly esteemed<br />
colleague serving terms as Interim and elected<br />
Department Chair. In recognition of her contributions,<br />
the Department of Nursing established the Ann<br />
Manchester Kelley Nursing Inquiry Day, a research<br />
presentation day for UNH undergraduate and graduate<br />
nursing students. She served as President of the <strong>New</strong><br />
<strong>Hampshire</strong> Nurses’ Association and founding member<br />
of Eta Iota Chapter, Sigma Theta Tau International<br />
Honor Society of Nursing. Ann received the Joseph D.<br />
Vaughn Award in 2011 for 29 years as a founding<br />
volunteer of the NH Long Term Care Ombudsman<br />
Program. A fond memory was the summer she crossed<br />
the US in a camping trailer with her<br />
husband, visiting schools of nursing to<br />
study their nursing simulation<br />
laboratories. After returning to UNH,<br />
she wrote and received a federally<br />
funded grant to develop and direct the<br />
first nursing simulation laboratory at<br />
UNH.<br />
A Tribute to Ann Kelley<br />
My fondest memories of Ann Kelley were from<br />
the time that I served on the leadership team for<br />
<strong>New</strong> <strong>Hampshire</strong> Nurses’ Association (NHNA).<br />
This was back in the late 80’s and through<br />
the 90’s. During this time, I served as a board<br />
member, then an officer, and eventually from<br />
1994-1996, as the Association’s president. I<br />
recall that Ann was a constant presence in<br />
the NHNA leadership, having herself been the<br />
NHNA president in a prior decade. She was<br />
a constant source of wisdom, support and<br />
guidance, not only for me, but for the many<br />
NHNA presidents that would come after me.<br />
Well after her formal retirement, I would always<br />
see Anne at NH nursing gatherings......always<br />
invested and interested in what was happening<br />
with nurses in our state and how the work of<br />
the profession was evolving. Never without<br />
an opinion, she was one of nursing’s greatest<br />
advocates.<br />
This said, I believe the pivotal role she played<br />
was as the steward of NH nursing’s and the<br />
Association’s history. She meticulously archived<br />
materials, documents and artifacts that she<br />
personally collected over the many years of her<br />
nursing career spent in NH. It would always<br />
amaze me when Ann could produce a sentinel<br />
document from years past that would actually<br />
help to inform a current dilemma. Preserving<br />
our history was truly a passion for Ann.<br />
Ann reigns among the many unsung heroes<br />
of <strong>New</strong> <strong>Hampshire</strong> nursing for her perpetual<br />
efforts to help us preserve our history. She will<br />
be greatly missed. – Susan Reeves, EdD, RN,<br />
CENP, Chief Nurse Executive, Dartmouth-<br />
Hitchcock Health<br />
School Nurse<br />
Diane Brown McClintock, 79, died on<br />
March 18, <strong>2020</strong>. She was a diploma<br />
graduate of the Elliot Hospital School of<br />
Nursing in Keene, obtained a BSN from<br />
Saint Anselm College, a degree in<br />
Psychology at <strong>New</strong> England College<br />
and earned a Masters in Education from<br />
Antioch University. She practiced as a<br />
school nurse for 28 years at ConVal High School in<br />
Peterborough, NH.<br />
Home Health Nurse<br />
Nancy A. (Perry) Leppanen, 84, passed<br />
away March 19, <strong>2020</strong>. She practiced at<br />
Home Health and Hospice, Merrimack,<br />
N.H., for over 30 years.<br />
Keene Nurse<br />
Joyce Winnette Sawyer, 83, passed<br />
away on March 19, <strong>2020</strong>. A Keene<br />
native she obtained her nursing diploma<br />
from the Elliott Community Hospital
<strong>June</strong>, July, August <strong>2020</strong> <strong>New</strong> <strong>Hampshire</strong> Nursing <strong>New</strong>s • Page 19<br />
IN MEMORY OF OUR COLLEAGUES<br />
School of Nursing in Keene. She practiced as a head<br />
nurse in the Emergency Department at Cheshire<br />
Medical Center.<br />
Day Surgery Pioneer<br />
Joan (Jamrog) McCann, 85, died on<br />
March 27, <strong>2020</strong>, after a period of<br />
declining health. She received her<br />
nursing diploma from the Elliot Hospital<br />
School of Nursing in Manchester and<br />
practiced as a registered nurse at the<br />
<strong>New</strong> <strong>Hampshire</strong> State Hospital and Concord Hospital.<br />
Joan also provided private duty nursing care and in<br />
the mid-1970s, she was asked to open the Day Surgery<br />
Unit at Concord Hospital. Joan successfully took on<br />
the challenge ran the unit with another nurse. Upon<br />
her retirement, Joan worked for the Department of<br />
Health and Human Services for the State of <strong>New</strong><br />
<strong>Hampshire</strong>, using her nursing skills to oversee the<br />
Katie Beckett Medicaid program and the Children’s<br />
Prosthetics Program.<br />
Concord Hospital Nurse<br />
Brian J. Trombly Sr., 68, passed away<br />
on April 26, <strong>2020</strong>. Brian’s first career<br />
included participating in the<br />
construction of the Seabrook Nuclear<br />
Power Plant in Seabrook, NH. Brian<br />
changed careers and as a RN practiced<br />
at Concord Hospital where he was a<br />
member of the staff for over ten years.<br />
Gero Nurse<br />
Claire D. (Ouelette) Provencher, 85,<br />
passed away April 30, <strong>2020</strong>. After<br />
obtaining her nursing diploma she<br />
practiced at Notre Dame Hospital as<br />
well as several nursing homes.<br />
Seacoast Nurse<br />
Nancy Jean (Collopy) Ferris, 76,<br />
passed away March 29, <strong>2020</strong> at home<br />
surrounded by family. After obtaining a<br />
nursing diploma in 1964 she practiced<br />
in Connecticut and <strong>New</strong> <strong>Hampshire</strong>.<br />
Mary Hitchcock Grad<br />
Hazel Howe McNamara, 95, passed<br />
away on April 1, <strong>2020</strong>. She graduated<br />
from Green Mountain College in<br />
Vermont and went on to pursue her<br />
nursing degree at Mary Hitchcock<br />
School of Nursing, graduating in 1947.<br />
She had a long nursing career, finishing<br />
it as a visiting nurse for the town of Hanover.<br />
Nurse Educator<br />
Nancy Bradley Chandler, 85, died May<br />
5, <strong>2020</strong>. She obtained her BSN and<br />
MSN from Boston College. She<br />
practiced in Boston, and <strong>New</strong> York and<br />
taught nursing in Massachusetts<br />
including as the Director of Lawrence<br />
General Hospital School of Nursing.<br />
Relocating to <strong>New</strong> <strong>Hampshire</strong> she taught nursing at St.<br />
Anselm College and NHTI. She was a pioneer in<br />
childbirth education, teaching classess in Laconia, and<br />
Franklin, NH. She established Prenatal Programs at<br />
Concord and Franklin Hospitals. Later in life she found<br />
great joy as a school nurse in Winnisquam and<br />
Warren schools and then as a camp nurse at Camp<br />
Walt Whitman and Camp Moosilauke.<br />
Nurse Educator<br />
Marjorie Lillian Allen, 87, passed away<br />
April 2, <strong>2020</strong>. She obtained a BA from<br />
Fitchburg State University and then her<br />
nursing diploma. She taught nursing at<br />
St. Joseph Hospital in Nashua. She also<br />
practiced at the Derry Medical Center<br />
for nearly eight years and coordinated<br />
the community’s visiting nurse and<br />
home-makers program.<br />
North Country Nurse<br />
Cynthia L. (Brown) Griffin, 61, of Berlin,<br />
died on April 10, <strong>2020</strong>. She was a<br />
diploma graduate of the Concord<br />
Hospital School of Nursing. She practiced<br />
for many years at Littleton Hospital, North<br />
Country Home Health and Coos County<br />
Family Health Services.<br />
• Emergency Room<br />
• Maternal Child Health<br />
• Inpatient Medical Surgical Unit<br />
• Office RN<br />
• PACU<br />
UNH Grad<br />
Rhonda Irene (Knapp) Hebert, 69,<br />
passed away in Texas April 29, <strong>2020</strong>.<br />
She graduated Cum Laude from the<br />
University of <strong>New</strong> <strong>Hampshire</strong> with a<br />
Bachelor of Science degree in Nursing.