Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
CASE REPORT<br />
GASTROENTEROLOGY TODAY - SUMMER <strong>2019</strong><br />
10<br />
The diagnosis of aorto-enteric fistula typically is delayed, as long as 1<br />
month in 50% of patients in one series, with the diagnosis being made<br />
within 10 days of hospitalization in only 15% of cases [12]. Urgent upper<br />
GI endoscopy is important for exclusion of common causes of massive<br />
upper GI bleeding; but the diagnostic sensitivity for aorto-enteric fistula<br />
has been reported to be as low as 25% [12]. Gastrointestinal bleeding<br />
with endoscopically unclear findings in a patient with aortic aneurysm or<br />
history of aortic repair should points towards an aorto-enteric fistula [13].<br />
The most valuable tool for diagnosing AEF is a CT scan with contrast,<br />
which may reveal gas within the aneurysm, destruction of the fat plane<br />
between the aneurysm and duodenum, proximity and connection<br />
between aorta and intestine and leaking of the contrast into the GI lumen;<br />
all highly suggestive of AEF [14]. MRI is less useful because of its limited<br />
availability in the emergency setting, longer acquisition time, need for<br />
local technical expertise, and potential difficulties differentiating peri-graft<br />
gas from aortic wall calcification. All other investigation modalities like<br />
white blood cell scan are of limited value in diagnosing AEF. Percutaneous<br />
angiography has a sensitivity of 94 percent and a specificity of 85 percent<br />
for detecting aorto-enteric fistula (AEF); but is rarely considered as<br />
most patients are critically ill by the time of a decision is made to do it<br />
[15&16]. ]. A high index of suspicion is paramount, supplemented by the<br />
judicious use of upper endoscopy and CT, and the attending physician<br />
must be willing to recommend exploratory laparotomy if clinical suspicion<br />
is sufficiently high. As immediate and correct diagnosis is difficult, the<br />
mortality is very high and an untreated AEF has 100% mortality. Mortality<br />
of invasively treated patients is approximately 50 %. [17].<br />
Conclusion<br />
Although AEF is an extremely rare cause of upper GI haemorrhage, it<br />
must always be considered and ruled out in GI haemorrhages. A herald<br />
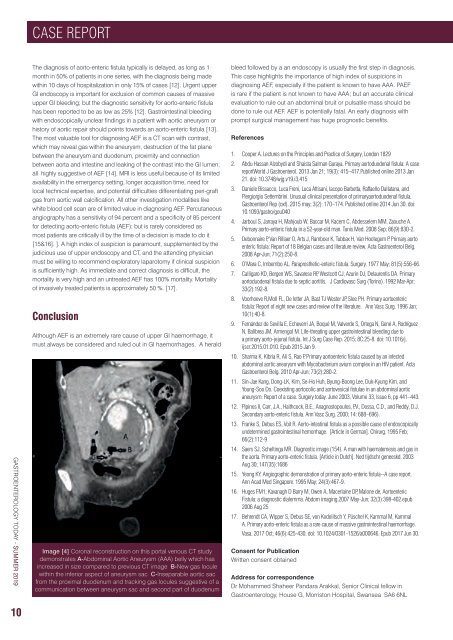
Image [4] Coronal reconstruction on this portal venous CT study<br />
demonstrates A-Abdominal Aortic Aneurysm (AAA) belly which has<br />
increased in size compared to previous CT image B-New gas locule<br />
within the inferior aspect of aneurysm sac C-Inseparable aortic sac<br />
from the proximal duodenum and tracking gas locules suggestive of a<br />
Image communication 4 between aneurysm sac and second part of duodenum<br />
bleed followed by a an endoscopy is usually the first step in diagnosis.<br />
This case highlights the importance of high index of suspicions in<br />
diagnosing AEF, especially if the patient is known to have AAA. PAEF<br />
is rare if the patient is not known to have AAA; but an accurate clinical<br />
evaluation to rule out an abdominal bruit or pulsatile mass should be<br />
done to rule out AEF. AEF is potentially fatal. An early diagnosis with<br />
prompt surgical management has huge prognostic benefits.<br />
References<br />
1. Cooper A. Lectures on the Principles and Practice of Surgery, London 1829<br />
2. Abdu Hassan Alzobydi and Shaista Salman Guraya. Primary aortoduodenal fistula: A case<br />
reportWorld J Gastroenterol. 2013 Jan 21; 19(3): 415–417.Published online 2013 Jan<br />
21. doi: 10.3748/wjg.v19.i3.415<br />
3. Daniele Bissacco, Luca Freni, Luca Attisani, Iacopo Barbetta, Raffaello Dallatana, and<br />
Piergiorgio Settembrini. Unusual clinical presentation of primaryaortoduodenal fistula.<br />
Gastroenterol Rep (oxf). 2015 may; 3(2): 170–174. Published online 2014 Jun 30. doi:<br />
10.1093/gastro/gou040<br />
4. Jarboui S, Jarraya H, Mahjoub W, Baccar M, Kacem C, Abdesselem MM, Zaouche A.<br />
Primary aorto-enteric fistula in a 52-year-old man. Tunis Med. 2008 Sep; 86(9):830-2.<br />
5. Debonnaire P, Van Rillaer O, Arts J, Ramboer K, Tubbax H, Van Hootegem P. Primary aorto<br />
enteric fistula: Report of 18 Belgian cases and literature review. Acta Gastroenterol Belg.<br />
2008 Apr-Jun; 71(2):250-8.<br />
6. O’Mara C, Imbembo AL. Paraprosthetic-enteric fistula. Surgery. 1977 May; 81(5):556-66.<br />
7. Calligaro KD, Bergen WS, Savarese RP, Westcott CJ, Azurin DJ, Delaurentis DA. Primary<br />
aortoduodenal fistula due to septic aortitis. J Cardiovasc Surg (Torino). 1992 Mar-Apr;<br />
33(2):192-8.<br />
8. Voorhoeve R,Moll FL, De letter JA, Bast TJ Wester JP, Slee PH. Primary aortoenteric<br />
fistula: Report of eight new cases and review of the literature. Ann Vasc Surg. 1996 Jan;<br />
10(1):40-8.<br />
9. Fernández de Sevilla E, Echeverri JA, Boqué M, Valverde S, Ortega N, Gené A, Rodríguez<br />
N, Balibrea JM, Armengol M. Life-threating upper gastrointestinal bleeding due to<br />
a primary aorto-jejunal fistula. Int J Surg Case Rep. 2015; 8C:25-8. doi: 10.1016/j.<br />
ijscr.2015.01.010. Epub 2015 Jan 9.<br />
10. Sharma K, Kibria R, Ali S, Rao P. Primary aortoenteric fistula caused by an infected<br />
abdominal aortic aneurysm with Mycobacterium avium complex in an HIV patient. Acta<br />
Gastroenterol Belg. 2010 Apr-Jun; 73(2):280-2.<br />
11. Sin-Jae Kang, Dong-LK, Kim, Se-Ho Huh, Byung-Boong Lee, Duk-Kyung Kim, and<br />
Young-Soo Do. Coexisting aortocolic and aortovesical fistulae in an abdominal aortic<br />
aneurysm: Report of a case. Surgery today. June 2003, Volume 33, Issue 6, pp 441–443.<br />
12. Pipinos II, Carr, J.A., Haithcock, B.E., Anagnostopoulos, P.V., Dossa, C.D., and Reddy, D.J.<br />
Secondary aorto-enteric fistula. Ann Vasc Surg. 2000; 14: 688–696).<br />
13. Franke S, Debus ES, Voit R. Aorto-intestinal fistula as a possible cause of endoscopically<br />
undetermined gastrointestinal hemorrhage. [Article in German]. Chirurg. 1995 Feb;<br />
66(2):112-9<br />
14. Saers SJ, Scheltinga MR. Diagnostic image (154). A man with haematemesis and gas in<br />
the aorta. Primary aorto-enteric fistula. [Article in Dutch]. Ned tijdschr geneeskd. 2003<br />
Aug 30; 147(35):1686<br />
15. Yeong KY. Angiographic demonstration of primary aorto-enteric fistula--A case report.<br />
Ann Acad Med Singapore. 1995 May; 24(3):467-9.<br />
16. Huges FM1, Kavanagh D Barry M, Owen A, Macerlaine DP, Malone de, Aortoenteric<br />
Fistula: a diagnostic dialemma. Abdom imaging.2007 May-Jun; 32(3):398-402.epub<br />
2006 Aug 25<br />
17. Behrendt CA, Wipper S, Debus SE, von Kodolitsch Y, Püschel K, Kammal M, Kammal<br />
A. Primary aorto-enteric fistula as a rare cause of massive gastrointestinal haemorrhage.<br />
Vasa. 2017 Oct; 46(6):425-430. doi: 10.1024/0301-1526/a000646. Epub 2017 Jun 30.<br />
Consent for Publication<br />
Written consent obtained<br />
Address for correspondence<br />
Dr Mohammed Shaheer Pandara Arakkal, Senior Clinical fellow in<br />
<strong>Gastroenterology</strong>, House G, Morriston Hospital, Swansea SA6 6NL