You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
CASE REPORT<br />
Examination revealed HR-95 b/m, BP 130/70 mm Hg, oxygen saturation<br />
96% on 2 Litres of oxygen and normal temperature. Abdominal<br />
examination revealed a large pulsatile abdominal mass. PR examination<br />
revealed melaena on glove. She scored 10 points on the Glasgow-<br />
Blatchford Bleeding Score.<br />
After resuscitation with IV fluids and blood products the patient was<br />
transferred to the ward. She had 3 further large episodes of melaena<br />
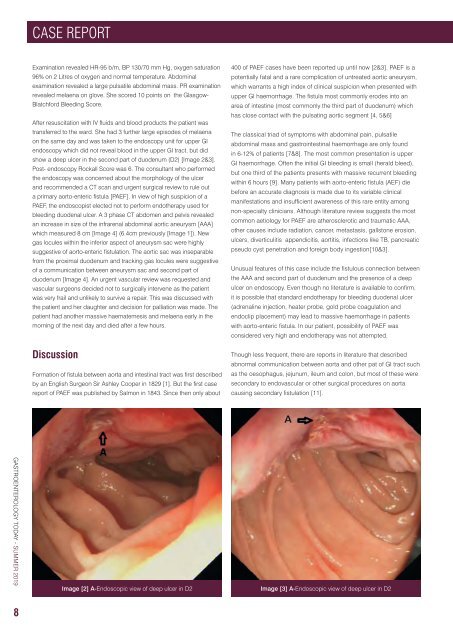
on the same day and was taken to the endoscopy unit for upper GI<br />
endoscopy which did not reveal blood in the upper GI tract, but did<br />
show a deep ulcer in the second part of duodenum (D2) [Image 2&3].<br />
Post- endoscopy Rockall Score was 6. The consultant who performed<br />
the endoscopy was concerned about the morphology of the ulcer<br />
and recommended a CT scan and urgent surgical review to rule out<br />
a primary aorto-enteric fistula [PAEF]. In view of high suspicion of a<br />
PAEF, the endoscopist elected not to perform endotherapy used for<br />
bleeding duodenal ulcer. A 3 phase CT abdomen and pelvis revealed<br />
an increase in size of the infrarenal abdominal aortic aneurysm [AAA]<br />
which measured 8 cm [Image 4] (6.4cm previously [Image 1]). New<br />
gas locules within the inferior aspect of aneurysm sac were highly<br />
suggestive of aorto-enteric fistulation. The aortic sac was inseparable<br />
from the proximal duodenum and tracking gas locules were suggestive<br />
of a communication between aneurysm sac and second part of<br />
duodenum [Image 4]. An urgent vascular review was requested and<br />
vascular surgeons decided not to surgically intervene as the patient<br />
was very frail and unlikely to survive a repair. This was discussed with<br />
the patient and her daughter and decision for palliation was made. The<br />
patient had another massive haematemesis and melaena early in the<br />
morning of the next day and died after a few hours.<br />
Discussion<br />
Formation of fistula between aorta and intestinal tract was first described<br />
by an English Surgeon Sir Ashley Cooper in 1829 [1]. But the first case<br />
report of PAEF was published by Salmon in 1843. Since then only about<br />
400 of PAEF cases have been reported up until now [2&3]. PAEF is a<br />
potentially fatal and a rare complication of untreated aortic aneurysm,<br />
which warrants a high index of clinical suspicion when presented with<br />
upper GI haemorrhage. The fistula most commonly erodes into an<br />
area of intestine (most commonly the third part of duodenum) which<br />
has close contact with the pulsating aortic segment [4, 5&6]<br />
The classical triad of symptoms with abdominal pain, pulsatile<br />
abdominal mass and gastrointestinal haemorrhage are only found<br />
in 6-12% of patients [7&8]. The most common presentation is upper<br />
GI haemorrhage. Often the initial GI bleeding is small (herald bleed),<br />
but one third of the patients presents with massive recurrent bleeding<br />
within 6 hours [9]. Many patients with aorto-enteric fistula (AEF) die<br />
before an accurate diagnosis is made due to its variable clinical<br />
manifestations and insufficient awareness of this rare entity among<br />
non-specialty clinicians. Although literature review suggests the most<br />
common aetiology for PAEF are atherosclerotic and traumatic AAA,<br />
other causes include radiation, cancer, metastasis, gallstone erosion,<br />
ulcers, diverticulitis appendicitis, aortitis, infections like TB, pancreatic<br />
pseudo cyst penetration and foreign body ingestion[10&3].<br />
Unusual features of this case include the fistulous connection between<br />
the AAA and second part of duodenum and the presence of a deep<br />
ulcer on endoscopy. Even though no literature is available to confirm,<br />
it is possible that standard endotherapy for bleeding duodenal ulcer<br />
(adrenaline injection, heater probe, gold probe coagulation and<br />
endoclip placement) may lead to massive haemorrhage in patients<br />
with aorto-enteric fistula. In our patient, possibility of PAEF was<br />
considered very high and endotherapy was not attempted.<br />
Though less frequent, there are reports in literature that described<br />
abnormal communication between aorta and other pat of GI tract such<br />
as the oesophagus, jejunum, ileum and colon, but most of these were<br />
secondary to endovascular or other surgical procedures on aorta<br />
causing secondary fistulation [11].<br />
GASTROENTEROLOGY TODAY - SUMMER <strong>2019</strong><br />
Image [2] A-Endoscopic view of deep ulcer in D2<br />
Image [3] A-Endoscopic view of deep ulcer in D2<br />
Image 2<br />
8<br />
Image 3