Dental Asia March/April 2023
For more than two decades, Dental Asia is the premium journal in linking dental innovators and manufacturers to its rightful audience. We devote ourselves in showcasing the latest dental technology and share evidence-based clinical philosophies to serve as an educational platform to dental professionals. Our combined portfolio of print and digital media also allows us to reach a wider market and secure our position as the leading dental media in the Asia Pacific region while facilitating global interactions among our readers.
For more than two decades, Dental Asia is the premium journal in linking dental innovators
and manufacturers to its rightful audience. We devote ourselves in showcasing the latest dental technology and share evidence-based clinical philosophies to serve as an educational platform to dental professionals. Our combined portfolio of print and digital media also allows us to reach a wider market and secure our position as the leading dental media in the Asia Pacific region while facilitating global interactions among our readers.
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
CLINICAL FEATURE<br />
Intraorally, a gingival sinus was<br />
noted on the buccal aspect between<br />
upper teeth 23 and 24, approximately<br />
6-8mm apical to the marginal gingiva.<br />
Tooth 23 was tender to percussion<br />
and had a palatal temporary filling.<br />
Radiographic periapical examination<br />
revealed a 16mm long broken<br />
instrument, extending from the<br />
coronal third to 0.5mm beyond the<br />
apex, along with an additional smaller<br />
piece of separated file in the middle<br />
third of the root canal (Fig. 2). A<br />
radiolucency in the distal aspect of<br />
the cervical third of the root with<br />
adjacent localised bone loss was<br />
noted — pathognomic of external<br />
cervical root resorption. Radiographic<br />
sinus tracing with gutta-percha<br />
directed to this site of cervical root<br />
resorption (Figs. 1a-b).<br />
A low volume CBCT scan of the<br />
area confirmed the clinical and<br />
radiographic diagnosis and provided<br />
an accurate assessment of the full<br />
extent of the cervical resorption<br />
defect and its boundaries. As the<br />
lesion was not extending<br />
circumferentially into the palatal<br />
aspect of the root, the treatment<br />
of the defect was planned to be<br />
approached directly by surgery. The<br />
scan also showed a single long canal<br />
with minimal curvature, presenting a<br />
favourable and predictable approach<br />
for orthograde retreatment of the<br />
root canal system. The prognosis<br />
for endodontic retreatment was<br />
favourable while long-term prognosis<br />
for cervical root resorption was<br />
guarded (Fig. 2).<br />
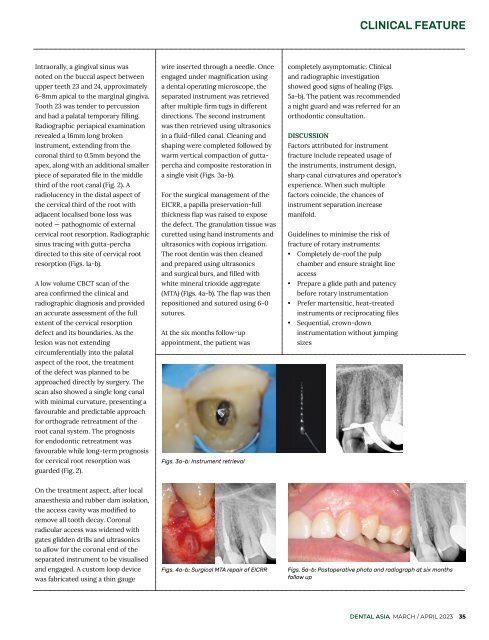
wire inserted through a needle. Once<br />
engaged under magnification using<br />
a dental operating microscope, the<br />
separated instrument was retrieved<br />
after multiple firm tugs in different<br />
directions. The second instrument<br />
was then retrieved using ultrasonics<br />
in a fluid-filled canal. Cleaning and<br />
shaping were completed followed by<br />
warm vertical compaction of guttapercha<br />
and composite restoration in<br />
a single visit (Figs. 3a-b).<br />
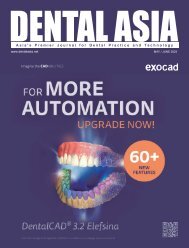
For the surgical management of the<br />
EICRR, a papilla preservation-full<br />
thickness flap was raised to expose<br />
the defect. The granulation tissue was<br />
curetted using hand instruments and<br />
ultrasonics with copious irrigation.<br />
The root dentin was then cleaned<br />
and prepared using ultrasonics<br />
and surgical burs, and filled with<br />
white mineral trioxide aggregate<br />
(MTA) (Figs. 4a-b). The flap was then<br />
repositioned and sutured using 6-0<br />
sutures.<br />
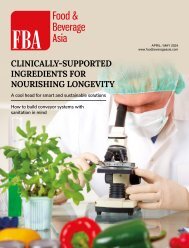
At the six months follow-up<br />
appointment, the patient was<br />
Figs. 3a-b: Instrument retrieval<br />
completely asymptomatic. Clinical<br />
and radiographic investigation<br />
showed good signs of healing (Figs.<br />
5a-b). The patient was recommended<br />
a night guard and was referred for an<br />
orthodontic consultation.<br />
DISCUSSION<br />
Factors attributed for instrument<br />
fracture include repeated usage of<br />
the instruments, instrument design,<br />
sharp canal curvatures and operator’s<br />
experience. When such multiple<br />
factors coincide, the chances of<br />
instrument separation increase<br />
manifold.<br />
Guidelines to minimise the risk of<br />
fracture of rotary instruments:<br />
• Completely de-roof the pulp<br />
chamber and ensure straight line<br />
access<br />
• Prepare a glide path and patency<br />
before rotary instrumentation<br />
• Prefer martensitic, heat-treated<br />
instruments or reciprocating files<br />
• Sequential, crown-down<br />
instrumentation without jumping<br />
sizes<br />
On the treatment aspect, after local<br />
anaesthesia and rubber dam isolation,<br />
the access cavity was modified to<br />
remove all tooth decay. Coronal<br />
radicular access was widened with<br />
gates glidden drills and ultrasonics<br />
to allow for the coronal end of the<br />
separated instrument to be visualised<br />
and engaged. A custom loop device<br />
was fabricated using a thin gauge<br />
Figs. 4a-b: Surgical MTA repair of EICRR<br />
Figs. 5a-b: Postoperative photo and radiograph at six months<br />
follow up<br />
DENTAL ASIA MARCH / APRIL <strong>2023</strong> 35