Dental Asia January/February 2024
For more than two decades, Dental Asia is the premium journal in linking dental innovators and manufacturers to its rightful audience. We devote ourselves in showcasing the latest dental technology and share evidence-based clinical philosophies to serve as an educational platform to dental professionals. Our combined portfolio of print and digital media also allows us to reach a wider market and secure our position as the leading dental media in the Asia Pacific region while facilitating global interactions among our readers.
For more than two decades, Dental Asia is the premium journal in linking dental innovators and manufacturers to its rightful audience. We devote ourselves in showcasing the latest dental technology and share evidence-based clinical philosophies to serve as an educational platform to dental professionals. Our combined portfolio of print and digital media also allows us to reach a wider market and secure our position as the leading dental media in the Asia Pacific region while facilitating global interactions among our readers.
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
CLINICAL FEATURE<br />
Fig. 2: Masks stop viruses much like this strainer collects sand<br />
While this phenomenon might be<br />
one reason why the role of airborne<br />
transmissions in hospital infections<br />
and from dental and orthopedic<br />
aerosols remains debatable, it serves<br />
to question the necessity of masks. 3,4<br />
SIZE MATTERS<br />
A nanometer is one billionth of a<br />
metre. A strand of human hair is<br />
approximately between 80,000-<br />
100,000nm wide. The influenza and<br />
coronaviruses range from 80-120nm,<br />
or approximately 0.1µm in diameter.<br />
This means that approximately 1,000<br />
of these viruses would fit across the<br />
width of a human hair. 5,6 The best<br />
fitting mask will not prevent a single<br />
human hair from passing between it<br />
and the face.<br />
N95 mask fabrics are designed to<br />
filter out 95% of airborne particles<br />
provided they are larger than 0.3µm<br />
in diameter and most surgical mask<br />
materials filter out particles 2.5µm or<br />
larger. 7 Therefore, its effectiveness<br />
in filtering out viruses of 0.1µm in<br />
diameter is highly questionable. Even<br />
if such devices did impede the flow of<br />
influenza and coronaviruses, millions<br />
of stray viruses would continue to pass<br />
through the gaps present around the<br />
periphery of masks.<br />
In practical terms this means that a<br />
mask is no more effective at stopping<br />
viruses than a strainer is at collecting<br />
sand (Fig. 2).<br />
HISTORICAL PERSPECTIVE<br />
Beginning with studies from 1946,<br />
a meta-analysis of masks efficacy<br />
published in <strong>February</strong> 2020 concluded<br />
that surgical-type face masks were<br />
not effective in reducing influenza<br />
transmissions. 8<br />
In 2013, nurses from Ontario, Canada,<br />
filed a grievance against the use<br />
of masks in lieu of receiving a flu<br />
vaccination. Independent arbitrators<br />
in 2015 and 2018 reviewed hundreds<br />
of relevant documents and found<br />
that hospitals could not force mask<br />
mandates because supporting<br />
evidence was insufficient, inadequate,<br />
and completely unpersuasive. 9,10<br />
In 2017 the Centers for Disease<br />
Control and Prevention (CDC) compiled<br />
a report based on a 16-year study of<br />
almost 200 articles concerning nonpharmaceutical<br />
methods of mitigating<br />
the effects of influenza pandemics.<br />
Masks were not mentioned — attesting<br />
to the CDC’s recognition of its<br />
ineffectiveness. 11<br />
The World Health Organization (WHO)<br />
in 2019, while commenting on the use<br />
of non-pharmaceutical measures to<br />
avoid respiratory transmissions, noted<br />
that: “There is also a lack of evidence<br />
for the effectiveness of improved<br />
respiratory etiquette and the use of<br />
face masks in community settings<br />
during influenza epidemics and<br />
pandemics.” 12<br />
In a March 2020 interview on the ’60<br />
minutes’ news programme, Dr Anthony<br />
Fauci stated categorically that “there<br />
is no reason to be walking around<br />
wearing a mask”. 13<br />
The large randomised DANMASK-19<br />
study released in 2021 concluded that<br />
surgical masks did not reduce SARS-<br />
CoV-2 infection rates among wearers in<br />
a community setting. 14<br />
This is but a small sample of the<br />
decades of studies refuting mask<br />
efficacy. For more extensive reviews,<br />
readers are referred to: ‘The Mask<br />
Studies You Should Know’ 15 and ‘More<br />
than 170 Comparative Studies and<br />
Articles on Mask Ineffectiveness and<br />
Harms’. 16<br />
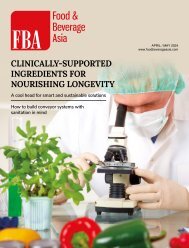
REAL WORLD DATA<br />
In his 2022 book, UNMASKED: The<br />
Global Failure of COVID Mask Mandates,<br />
Ian Millar provides numerous graphs<br />
from around the world comparing<br />
unmasked and masked populations (Fig.<br />
3). These real-world experiences show<br />
no appreciable differences in COVID<br />
infection rates among the two groups. 17<br />
HARMS<br />
A fundamental tenet of health care is:<br />
“First, do no harm”. This applies not only<br />
to the delivery of healthcare but also<br />
to measures taken to mitigate disease<br />
transmission, including the use of<br />
masks.<br />
Fig. 3: Mask wearing results in no appreciable difference in the<br />
number of COVID-19 cases<br />
34 DENTAL ASIA JANUARY / FEBRUARY <strong>2024</strong>