Ergothérapie et intervention auprès des personnes présentant des
Ergothérapie et intervention auprès des personnes présentant des
Ergothérapie et intervention auprès des personnes présentant des
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
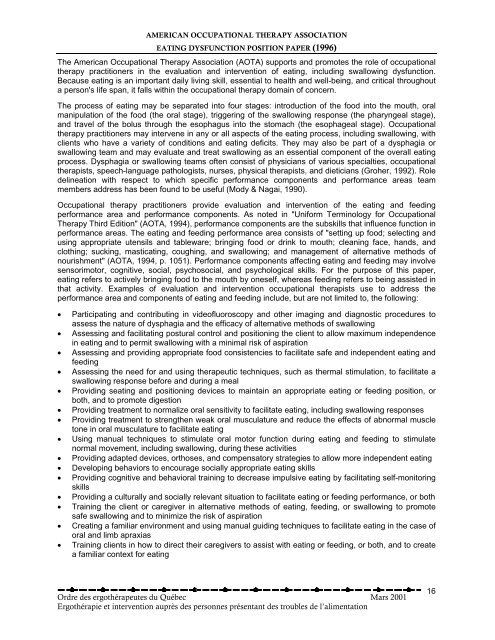
AMERICAN OCCUPATIONAL THERAPY ASSOCIATION<br />
EATING DYSFUNCTION POSITION PAPER (1996)<br />
The American Occupational Therapy Association (AOTA) supports and promotes the role of occupational<br />
therapy practitioners in the evaluation and <strong>intervention</strong> of eating, including swallowing dysfunction.<br />
Because eating is an important daily living skill, essential to health and well-being, and critical throughout<br />
a person's life span, it falls within the occupational therapy domain of concern.<br />
The process of eating may be separated into four stages: introduction of the food into the mouth, oral<br />
manipulation of the food (the oral stage), triggering of the swallowing response (the pharyngeal stage),<br />
and travel of the bolus through the esophagus into the stomach (the esophageal stage). Occupational<br />
therapy practitioners may intervene in any or all aspects of the eating process, including swallowing, with<br />
clients who have a vari<strong>et</strong>y of conditions and eating deficits. They may also be part of a dysphagia or<br />
swallowing team and may evaluate and treat swallowing as an essential component of the overall eating<br />
process. Dysphagia or swallowing teams often consist of physicians of various specialties, occupational<br />
therapists, speech-language pathologists, nurses, physical therapists, and di<strong>et</strong>icians (Groher, 1992). Role<br />
delineation with respect to which specific performance components and performance areas team<br />
members address has been found to be useful (Mody & Nagai, 1990).<br />
Occupational therapy practitioners provide evaluation and <strong>intervention</strong> of the eating and feeding<br />
performance area and performance components. As noted in "Uniform Terminology for Occupational<br />
Therapy Third Edition" (AOTA, 1994), performance components are the subskills that influence function in<br />
performance areas. The eating and feeding performance area consists of "s<strong>et</strong>ting up food; selecting and<br />
using appropriate utensils and tableware; bringing food or drink to mouth; cleaning face, hands, and<br />
clothing; sucking, masticating, coughing, and swallowing; and management of alternative m<strong>et</strong>hods of<br />
nourishment" (AOTA, 1994, p. 1051). Performance components affecting eating and feeding may involve<br />
sensorimotor, cognitive, social, psychosocial, and psychological skills. For the purpose of this paper,<br />
eating refers to actively bringing food to the mouth by oneself, whereas feeding refers to being assisted in<br />
that activity. Examples of evaluation and <strong>intervention</strong> occupational therapists use to address the<br />
performance area and components of eating and feeding include, but are not limited to, the following:<br />
• Participating and contributing in videofluoroscopy and other imaging and diagnostic procedures to<br />
assess the nature of dysphagia and the efficacy of alternative m<strong>et</strong>hods of swallowing<br />
• Assessing and facilitating postural control and positioning the client to allow maximum independence<br />
in eating and to permit swallowing with a minimal risk of aspiration<br />
• Assessing and providing appropriate food consistencies to facilitate safe and independent eating and<br />
feeding<br />
• Assessing the need for and using therapeutic techniques, such as thermal stimulation, to facilitate a<br />
swallowing response before and during a meal<br />
• Providing seating and positioning devices to maintain an appropriate eating or feeding position, or<br />
both, and to promote digestion<br />
• Providing treatment to normalize oral sensitivity to facilitate eating, including swallowing responses<br />
• Providing treatment to strengthen weak oral musculature and reduce the effects of abnormal muscle<br />
tone in oral musculature to facilitate eating<br />
• Using manual techniques to stimulate oral motor function during eating and feeding to stimulate<br />
normal movement, including swallowing, during these activities<br />
• Providing adapted devices, orthoses, and compensatory strategies to allow more independent eating<br />
• Developing behaviors to encourage socially appropriate eating skills<br />
• Providing cognitive and behavioral training to decrease impulsive eating by facilitating self-monitoring<br />
skills<br />
• Providing a culturally and socially relevant situation to facilitate eating or feeding performance, or both<br />
• Training the client or caregiver in alternative m<strong>et</strong>hods of eating, feeding, or swallowing to promote<br />
safe swallowing and to minimize the risk of aspiration<br />
• Creating a familiar environment and using manual guiding techniques to facilitate eating in the case of<br />
oral and limb apraxias<br />
• Training clients in how to direct their caregivers to assist with eating or feeding, or both, and to create<br />
a familiar context for eating<br />
Ordre <strong>des</strong> ergothérapeutes du Québec Mars 2001<br />
Ergothérapie <strong>et</strong> <strong>intervention</strong> auprès <strong>des</strong> <strong>personnes</strong> présentant <strong>des</strong> troubles de l’alimentation<br />
16