FORENSIC TOXICOLOGY - Bio Medical Forensics
FORENSIC TOXICOLOGY - Bio Medical Forensics
FORENSIC TOXICOLOGY - Bio Medical Forensics
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
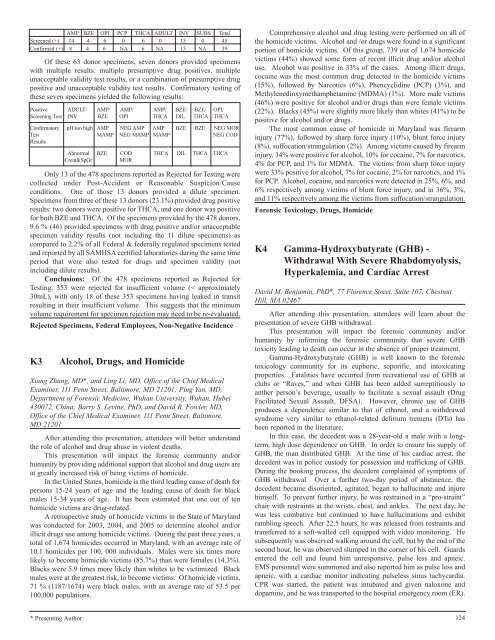
AMP BZE OPI PCP THCA ADULT INV SUBS Total<br />
Screened (+) 14 4 6 0 6 0 15 0 45<br />
Confirmed (+) 8 4 6 NA 6 NA 15 NA 39<br />
Of these 63 donor specimens, seven donors provided specimens<br />
with multiple results: multiple presumptive drug positives, multiple<br />
unacceptable validity test results, or a combination of presumptive drug<br />
positive and unacceptable validity test results. Confirmatory testing of<br />
these seven specimens yielded the following results:<br />
Positive ADULT/ AMP/ AMP/ AMP/ BZE/ BZE/ OPI/<br />
Screening Test INV BZE OPI THCA DIL THCA THCA<br />
Confirmatory pH too high AMP NEG AMP AMP BZE BZE NEG MOR<br />
Test<br />
Results<br />
MAMP NEG MAMP MAMP NEG COD<br />
Abnormal BZE COD THCA DIL THCA THCA<br />
Creat&SpGr MOR<br />
Only 13 of the 478 specimens reported as Rejected for Testing were<br />
collected under Post-Accident or Reasonable Suspicion/Cause<br />
conditions. One of those 13 donors provided a dilute specimen.<br />
Specimens from three of these 13 donors (23.1%) provided drug positive<br />
results: two donors were positive for THCA, and one donor was positive<br />
for both BZE and THCA. Of the specimens provided by the 478 donors,<br />
9.6 % (46) provided specimens with drug positive and/or unacceptable<br />
specimen validity results (not including the 11 dilute specimens) as<br />
compared to 2.2% of all Federal & federally regulated specimens tested<br />
and reported by all SAMHSA certified laboratories during the same time<br />
period that were also tested for drugs and specimen validity (not<br />
including dilute results).<br />
Conclusions: Of the 478 specimens reported as Rejected for<br />
Testing, 353 were rejected for insufficient volume (< approximately<br />
30mL), with only 18 of these 353 specimens having leaked in transit<br />
resulting in their insufficient volume. This suggests that the minimum<br />
volume requirement for specimen rejection may need to be re-evaluated.<br />
Rejected Specimens, Federal Employees, Non-Negative Incidence<br />
K3 Alcohol, Drugs, and Homicide<br />
Xiang Zhang, MD*, and Ling Li, MD, Office of the Chief <strong>Medical</strong><br />
Examiner, 111 Penn Street, Baltimore, MD 21201; Ping Yan, MD,<br />
Department of Forensic Medicine, Wuhan University, Wuhan, Hubei<br />
430072, China; Barry S. Levine, PhD, and David R. Fowler, MD,<br />
Office of the Chief <strong>Medical</strong> Examiner, 111 Penn Street, Baltimore,<br />
MD 21201<br />
After attending this presentation, attendees will better understand<br />
the role of alcohol and drug abuse in violent deaths.<br />
This presentation will impact the forensic community and/or<br />
humanity by providing additional support that alcohol and drug users are<br />
at greatly increased risk of being victims of homicide.<br />
In the United States, homicide is the third leading cause of death for<br />
persons 15-24 years of age and the leading cause of death for black<br />
males 15-34 years of age. It has been estimated that one out of ten<br />
homicide victims are drug-related.<br />
A retrospective study of homicide victims in the State of Maryland<br />
was conducted for 2003, 2004, and 2005 to determine alcohol and/or<br />
illicit drugs use among homicide victims. During the past three years, a<br />
total of 1,674 homicides occurred in Maryland, with an average rate of<br />
10.1 homicides per 100, 000 individuals. Males were six times more<br />
likely to become homicide victims (85.7%) than were females (14.3%).<br />
Blacks were 5.9 times more likely than whites to be victimized. Black<br />
males were at the greatest risk, to become victims. Of homicide victims,<br />
71 % (1187/1674) were black males, with an average rate of 53.5 per<br />
100,000 populations.<br />
* Presenting Author<br />
Comprehensive alcohol and drug testing were performed on all of<br />
the homicide victims. Alcohol and /or drugs were found in a significant<br />
portion of homicide victims. Of this group, 739 out of 1,674 homicide<br />
victims (44%) showed some form of recent illicit drug and/or alcohol<br />
use. Alcohol was positive in 33% of the cases. Among illicit drugs,<br />
cocaine was the most common drug detected in the homicide victims<br />
(15%), followed by Narcotics (6%), Phencyclidine (PCP) (3%), and<br />
Methylenedioxymethamphetamine (MDMA) (1%). More male victims<br />
(46%) were positive for alcohol and/or drugs than were female victims<br />
(22%). Blacks (45%) were slightly more likely than whites (41%) to be<br />
positive for alcohol and/or drugs.<br />
The most common cause of homicide in Maryland was firearm<br />
injury (77%), followed by sharp force injury (10%), blunt force injury<br />
(8%), suffocation/strangulation (2%). Among victims caused by firearm<br />
injury, 34% were positive for alcohol, 10% for cocaine, 7% for narcotics,<br />
4% for PCP, and 1% for MDMA. The victims from sharp force injury<br />
were 33% positive for alcohol, 7% for cocaine, 2% for narcotics, and 1%<br />
for PCP. Alcohol, cocaine, and narcotics were detected in 25%, 6%, and<br />
6% respectively among victims of blunt force injury, and in 36%, 3%,<br />
and 11% respectively among the victims from suffocation/strangulation.<br />
Forensic Toxicology, Drugs, Homicide<br />
K4 Gamma-Hydroxybutyrate (GHB) -<br />
Withdrawal With Severe Rhabdomyolysis,<br />
Hyperkalemia, and Cardiac Arrest<br />
David M. Benjamin, PhD*, 77 Florence Street, Suite 107, Chestnut<br />
Hill, MA 02467<br />
After attending this presentation, attendees will learn about the<br />
presentation of severe GHB withdrawal.<br />
This presentation will impact the forensic community and/or<br />
humanity by informing the forensic community that severe GHB<br />
toxicity leading to death can occur in the absence of proper treatment.<br />
Gamma-Hydroxybutyrate (GHB) is well known to the forensic<br />
toxicology community for its euphoric, soporific, and intoxicating<br />
properties. Fatalities have occurred from recreational use of GHB at<br />
clubs or “Raves,” and when GHB has been added surreptitiously to<br />
anther person’s beverage, usually to facilitate a sexual assault (Drug<br />
Facilitated Sexual Assault, DFSA). However, chronic use of GHB<br />
produces a dependence similar to that of ethanol, and a withdrawal<br />
syndrome very similar to ethanol-related delirium tremens (DTs) has<br />
been reported in the literature.<br />
In this case, the decedent was a 28-year-old a male with a longterm,<br />
high dose dependence on GHB. In order to ensure his supply of<br />
GHB, the man distributed GHB. At the time of his cardiac arrest, the<br />
decedent was in police custody for possession and trafficking of GHB.<br />
During the booking process, the decedent complained of symptoms of<br />
GHB withdrawal. Over a further two-day period of abstinence, the<br />
decedent became disoriented, agitated, began to hallucinate and injure<br />
himself. To prevent further injury, he was restrained in a “pro-straint”<br />
chair with restraints at the wrists, chest, and ankles. The next day, he<br />
was less combative but continued to have hallucinations and exhibit<br />
rambling speech. After 22.5 hours, he was released from restraints and<br />
transferred to a soft-walled cell equipped with video monitoring. He<br />
subsequently was observed walking around the cell, but by the end of the<br />
second hour, he was observed slumped in the corner of his cell. Guards<br />
entered the cell and found him unresponsive, pulse less and apneic.<br />
EMS personnel were summoned and also reported him as pulse less and<br />
apneic, with a cardiac monitor indicating pulseless sinus tachycardia.<br />
CPR was started, the patient was intubated and given naloxone and<br />
dopamine, and he was transported to the hospital emergency room (ER).<br />
124