Silica (crystalline, respirable) - OEHHA
Silica (crystalline, respirable) - OEHHA
Silica (crystalline, respirable) - OEHHA
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
FINAL February 2005<br />
alveolar macrophage-derived growth factor) stimulate fibroblasts to proliferate and to make<br />
collagen. Since silica particles cannot be digested by the macrophage, the inflammatory process<br />
becomes chronic (frustrated phagocytosis). An increased silica burden leads to more foci of<br />
inflammation, nodule formation, and fibrosis. The internal process can continue after external<br />
exposure ends. <strong>Silica</strong> particles also enter into alveolar Type I epithelial cells (Churg, 1996),<br />
which can lead to cell death of Type I cells and to hypertrophy and proliferation of Type II<br />
epithelial cells to replace the Type I cells. The epithelial repair process is associated with a<br />
subsequent increase in collagen formation.<br />
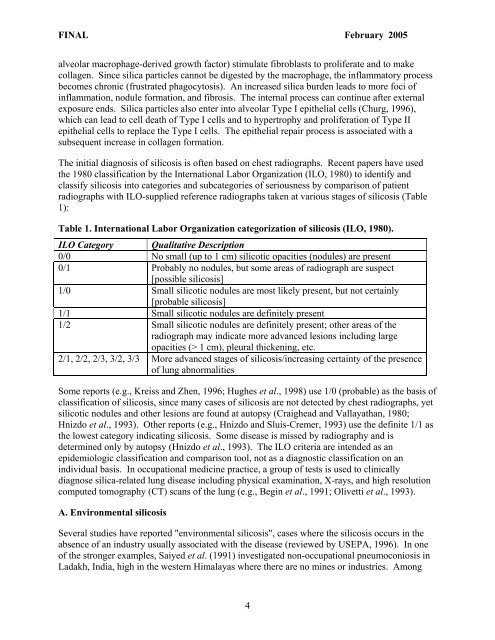
The initial diagnosis of silicosis is often based on chest radiographs. Recent papers have used<br />
the 1980 classification by the International Labor Organization (ILO, 1980) to identify and<br />
classify silicosis into categories and subcategories of seriousness by comparison of patient<br />
radiographs with ILO-supplied reference radiographs taken at various stages of silicosis (Table<br />
1):<br />
Table 1. International Labor Organization categorization of silicosis (ILO, 1980).<br />
ILO Category Qualitative Description<br />
0/0 No small (up to 1 cm) silicotic opacities (nodules) are present<br />
0/1 Probably no nodules, but some areas of radiograph are suspect<br />
[possible silicosis]<br />
1/0 Small silicotic nodules are most likely present, but not certainly<br />
[probable silicosis]<br />
1/1 Small silicotic nodules are definitely present<br />
1/2 Small silicotic nodules are definitely present; other areas of the<br />
radiograph may indicate more advanced lesions including large<br />
opacities (> 1 cm), pleural thickening, etc.<br />
2/1, 2/2, 2/3, 3/2, 3/3 More advanced stages of silicosis/increasing certainty of the presence<br />
of lung abnormalities<br />
Some reports (e.g., Kreiss and Zhen, 1996; Hughes et al., 1998) use 1/0 (probable) as the basis of<br />
classification of silicosis, since many cases of silicosis are not detected by chest radiographs, yet<br />
silicotic nodules and other lesions are found at autopsy (Craighead and Vallayathan, 1980;<br />
Hnizdo et al., 1993). Other reports (e.g., Hnizdo and Sluis-Cremer, 1993) use the definite 1/1 as<br />
the lowest category indicating silicosis. Some disease is missed by radiography and is<br />
determined only by autopsy (Hnizdo et al., 1993). The ILO criteria are intended as an<br />
epidemiologic classification and comparison tool, not as a diagnostic classification on an<br />
individual basis. In occupational medicine practice, a group of tests is used to clinically<br />
diagnose silica-related lung disease including physical examination, X-rays, and high resolution<br />
computed tomography (CT) scans of the lung (e.g., Begin et al., 1991; Olivetti et al., 1993).<br />
A. Environmental silicosis<br />
Several studies have reported "environmental silicosis", cases where the silicosis occurs in the<br />
absence of an industry usually associated with the disease (reviewed by USEPA, 1996). In one<br />
of the stronger examples, Saiyed et al. (1991) investigated non-occupational pneumoconiosis in<br />
Ladakh, India, high in the western Himalayas where there are no mines or industries. Among<br />
4