Valeurs seuils pour le rapport coût-efficacité en soins de santé - KCE
Valeurs seuils pour le rapport coût-efficacité en soins de santé - KCE
Valeurs seuils pour le rapport coût-efficacité en soins de santé - KCE
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>KCE</strong> reports 100 ICER Thresholds 35<br />
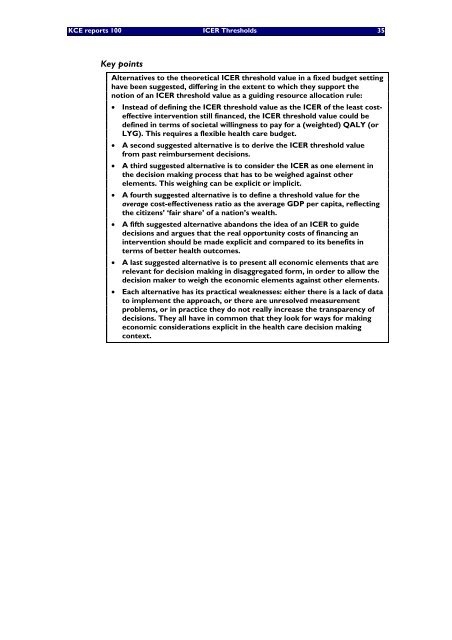
Key points<br />
Alternatives to the theoretical ICER threshold value in a fixed budget setting<br />
have be<strong>en</strong> suggested, differing in the ext<strong>en</strong>t to which they support the<br />
notion of an ICER threshold value as a guiding resource allocation ru<strong>le</strong>:<br />
• Instead of <strong>de</strong>fining the ICER threshold value as the ICER of the <strong>le</strong>ast costeffective<br />
interv<strong>en</strong>tion still financed, the ICER threshold value could be<br />
<strong>de</strong>fined in terms of societal willingness to pay for a (weighted) QALY (or<br />
LYG). This requires a f<strong>le</strong>xib<strong>le</strong> health care budget.<br />
• A second suggested alternative is to <strong>de</strong>rive the ICER threshold value<br />
from past reimbursem<strong>en</strong>t <strong>de</strong>cisions.<br />
• A third suggested alternative is to consi<strong>de</strong>r the ICER as one e<strong>le</strong>m<strong>en</strong>t in<br />
the <strong>de</strong>cision making process that has to be weighed against other<br />
e<strong>le</strong>m<strong>en</strong>ts. This weighing can be explicit or implicit.<br />
• A fourth suggested alternative is to <strong>de</strong>fine a threshold value for the<br />
average cost-effectiv<strong>en</strong>ess ratio as the average GDP per capita, ref<strong>le</strong>cting<br />
the citiz<strong>en</strong>s’ ‘fair share’ of a nation’s wealth.<br />
• A fifth suggested alternative abandons the i<strong>de</strong>a of an ICER to gui<strong>de</strong><br />
<strong>de</strong>cisions and argues that the real opportunity costs of financing an<br />
interv<strong>en</strong>tion should be ma<strong>de</strong> explicit and compared to its b<strong>en</strong>efits in<br />
terms of better health outcomes.<br />
• A last suggested alternative is to pres<strong>en</strong>t all economic e<strong>le</strong>m<strong>en</strong>ts that are<br />
re<strong>le</strong>vant for <strong>de</strong>cision making in disaggregated form, in or<strong>de</strong>r to allow the<br />
<strong>de</strong>cision maker to weigh the economic e<strong>le</strong>m<strong>en</strong>ts against other e<strong>le</strong>m<strong>en</strong>ts.<br />
• Each alternative has its practical weaknesses: either there is a lack of data<br />
to imp<strong>le</strong>m<strong>en</strong>t the approach, or there are unresolved measurem<strong>en</strong>t<br />
prob<strong>le</strong>ms, or in practice they do not really increase the transpar<strong>en</strong>cy of<br />
<strong>de</strong>cisions. They all have in common that they look for ways for making<br />
economic consi<strong>de</strong>rations explicit in the health care <strong>de</strong>cision making<br />
context.