PROVIDER MANUAL - Sendero Health Plans
PROVIDER MANUAL - Sendero Health Plans
PROVIDER MANUAL - Sendero Health Plans
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
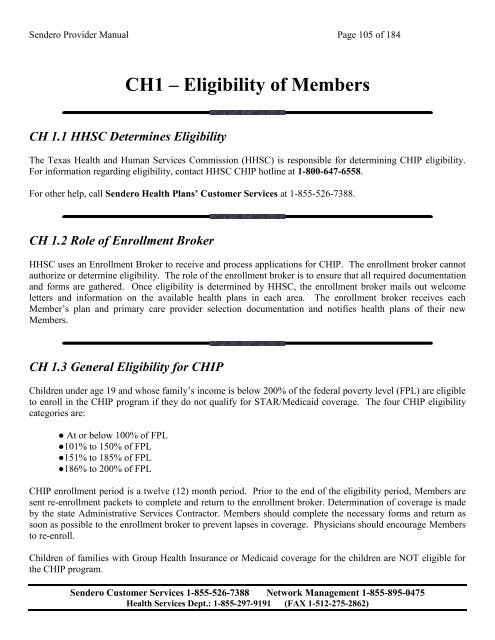
<strong>Sendero</strong> Provider Manual Page 105 of 184<br />
CH1 – Eligibility of Members<br />
CH 1.1 HHSC Determines Eligibility<br />
The Texas <strong>Health</strong> and Human Services Commission (HHSC) is responsible for determining CHIP eligibility.<br />
For information regarding eligibility, contact HHSC CHIP hotline at 1-800-647-6558.<br />
For other help, call <strong>Sendero</strong> <strong>Health</strong> <strong>Plans</strong>’ Customer Services at 1-855-526-7388.<br />
CH 1.2 Role of Enrollment Broker<br />
HHSC uses an Enrollment Broker to receive and process applications for CHIP. The enrollment broker cannot<br />
authorize or determine eligibility. The role of the enrollment broker is to ensure that all required documentation<br />
and forms are gathered. Once eligibility is determined by HHSC, the enrollment broker mails out welcome<br />
letters and information on the available health plans in each area. The enrollment broker receives each<br />
Member’s plan and primary care provider selection documentation and notifies health plans of their new<br />
Members.<br />
CH 1.3 General Eligibility for CHIP<br />
Children under age 19 and whose family’s income is below 200% of the federal poverty level (FPL) are eligible<br />
to enroll in the CHIP program if they do not qualify for STAR/Medicaid coverage. The four CHIP eligibility<br />
categories are:<br />
● At or below 100% of FPL<br />
●101% to 150% of FPL<br />
●151% to 185% of FPL<br />
●186% to 200% of FPL<br />
CHIP enrollment period is a twelve (12) month period. Prior to the end of the eligibility period, Members are<br />
sent re-enrollment packets to complete and return to the enrollment broker. Determination of coverage is made<br />
by the state Administrative Services Contractor. Members should complete the necessary forms and return as<br />
soon as possible to the enrollment broker to prevent lapses in coverage. Physicians should encourage Members<br />
to re-enroll.<br />
Children of families with Group <strong>Health</strong> Insurance or Medicaid coverage for the children are NOT eligible for<br />
the CHIP program.<br />
<strong>Sendero</strong> Customer Services 1-855-526-7388 Network Management 1-855-895-0475<br />
<strong>Health</strong> Services Dept.: 1-855-297-9191 (FAX 1-512-275-2862)