PROVIDER MANUAL - Sendero Health Plans
PROVIDER MANUAL - Sendero Health Plans
PROVIDER MANUAL - Sendero Health Plans
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Sendero</strong> Provider Manual Page 56 of 184<br />
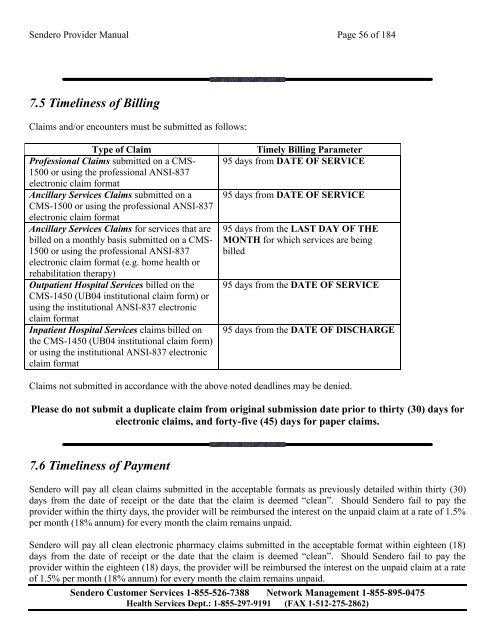
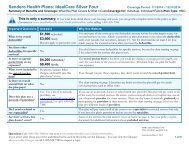
7.5 Timeliness of Billing<br />
Claims and/or encounters must be submitted as follows:<br />
Type of Claim<br />
Professional Claims submitted on a CMS-<br />
1500 or using the professional ANSI-837<br />
electronic claim format<br />
Ancillary Services Claims submitted on a<br />
CMS-1500 or using the professional ANSI-837<br />
electronic claim format<br />
Ancillary Services Claims for services that are<br />
billed on a monthly basis submitted on a CMS-<br />
1500 or using the professional ANSI-837<br />
electronic claim format (e.g. home health or<br />
rehabilitation therapy)<br />
Outpatient Hospital Services billed on the<br />
CMS-1450 (UB04 institutional claim form) or<br />
using the institutional ANSI-837 electronic<br />
claim format<br />
Inpatient Hospital Services claims billed on<br />
the CMS-1450 (UB04 institutional claim form)<br />
or using the institutional ANSI-837 electronic<br />
claim format<br />
Timely Billing Parameter<br />
95 days from DATE OF SERVICE<br />
95 days from DATE OF SERVICE<br />
95 days from the LAST DAY OF THE<br />
MONTH for which services are being<br />
billed<br />
95 days from the DATE OF SERVICE<br />
95 days from the DATE OF DISCHARGE<br />
Claims not submitted in accordance with the above noted deadlines may be denied.<br />
Please do not submit a duplicate claim from original submission date prior to thirty (30) days for<br />
electronic claims, and forty-five (45) days for paper claims.<br />
7.6 Timeliness of Payment<br />
<strong>Sendero</strong> will pay all clean claims submitted in the acceptable formats as previously detailed within thirty (30)<br />
days from the date of receipt or the date that the claim is deemed “clean”. Should <strong>Sendero</strong> fail to pay the<br />
provider within the thirty days, the provider will be reimbursed the interest on the unpaid claim at a rate of 1.5%<br />
per month (18% annum) for every month the claim remains unpaid.<br />
<strong>Sendero</strong> will pay all clean electronic pharmacy claims submitted in the acceptable format within eighteen (18)<br />
days from the date of receipt or the date that the claim is deemed “clean”. Should <strong>Sendero</strong> fail to pay the<br />
provider within the eighteen (18) days, the provider will be reimbursed the interest on the unpaid claim at a rate<br />
of 1.5% per month (18% annum) for every month the claim remains unpaid.<br />
<strong>Sendero</strong> Customer Services 1-855-526-7388 Network Management 1-855-895-0475<br />
<strong>Health</strong> Services Dept.: 1-855-297-9191 (FAX 1-512-275-2862)