PROVIDER MANUAL - Sendero Health Plans
PROVIDER MANUAL - Sendero Health Plans
PROVIDER MANUAL - Sendero Health Plans
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
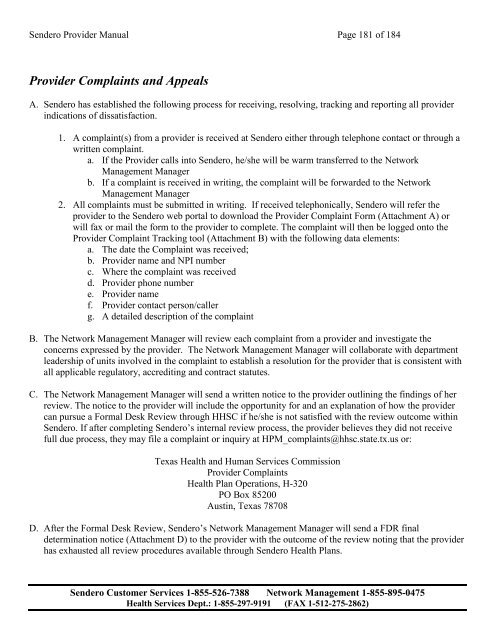
<strong>Sendero</strong> Provider Manual Page 181 of 184<br />
Provider Complaints and Appeals<br />
A. <strong>Sendero</strong> has established the following process for receiving, resolving, tracking and reporting all provider<br />
indications of dissatisfaction.<br />
1. A complaint(s) from a provider is received at <strong>Sendero</strong> either through telephone contact or through a<br />
written complaint.<br />
a. If the Provider calls into <strong>Sendero</strong>, he/she will be warm transferred to the Network<br />
Management Manager<br />
b. If a complaint is received in writing, the complaint will be forwarded to the Network<br />
Management Manager<br />
2. All complaints must be submitted in writing. If received telephonically, <strong>Sendero</strong> will refer the<br />
provider to the <strong>Sendero</strong> web portal to download the Provider Complaint Form (Attachment A) or<br />
will fax or mail the form to the provider to complete. The complaint will then be logged onto the<br />
Provider Complaint Tracking tool (Attachment B) with the following data elements:<br />
a. The date the Complaint was received;<br />
b. Provider name and NPI number<br />
c. Where the complaint was received<br />
d. Provider phone number<br />
e. Provider name<br />
f. Provider contact person/caller<br />
g. A detailed description of the complaint<br />
B. The Network Management Manager will review each complaint from a provider and investigate the<br />
concerns expressed by the provider. The Network Management Manager will collaborate with department<br />
leadership of units involved in the complaint to establish a resolution for the provider that is consistent with<br />
all applicable regulatory, accrediting and contract statutes.<br />
C. The Network Management Manager will send a written notice to the provider outlining the findings of her<br />
review. The notice to the provider will include the opportunity for and an explanation of how the provider<br />
can pursue a Formal Desk Review through HHSC if he/she is not satisfied with the review outcome within<br />
<strong>Sendero</strong>. If after completing <strong>Sendero</strong>’s internal review process, the provider believes they did not receive<br />
full due process, they may file a complaint or inquiry at HPM_complaints@hhsc.state.tx.us or:<br />
Texas <strong>Health</strong> and Human Services Commission<br />
Provider Complaints<br />
<strong>Health</strong> Plan Operations, H-320<br />
PO Box 85200<br />
Austin, Texas 78708<br />
D. After the Formal Desk Review, <strong>Sendero</strong>’s Network Management Manager will send a FDR final<br />
determination notice (Attachment D) to the provider with the outcome of the review noting that the provider<br />
has exhausted all review procedures available through <strong>Sendero</strong> <strong>Health</strong> <strong>Plans</strong>.<br />
<strong>Sendero</strong> Customer Services 1-855-526-7388 Network Management 1-855-895-0475<br />
<strong>Health</strong> Services Dept.: 1-855-297-9191 (FAX 1-512-275-2862)