PROVIDER MANUAL - Sendero Health Plans
PROVIDER MANUAL - Sendero Health Plans
PROVIDER MANUAL - Sendero Health Plans
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Sendero</strong> Provider Manual Page 24 of 184<br />
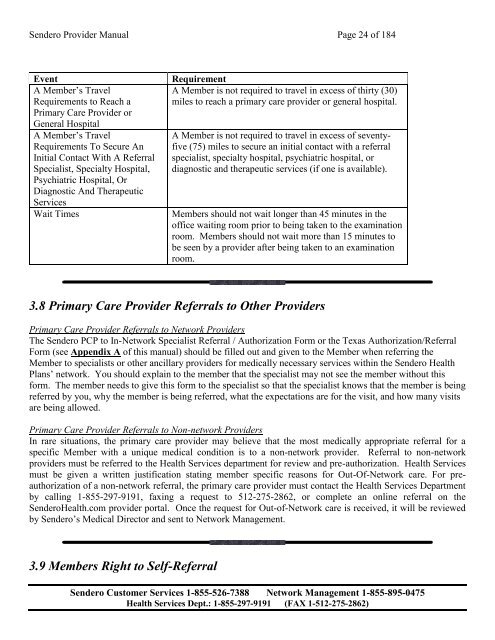
Event<br />
A Member’s Travel<br />
Requirements to Reach a<br />
Primary Care Provider or<br />
General Hospital<br />
A Member’s Travel<br />
Requirements To Secure An<br />
Initial Contact With A Referral<br />
Specialist, Specialty Hospital,<br />
Psychiatric Hospital, Or<br />
Diagnostic And Therapeutic<br />
Services<br />
Wait Times<br />
Requirement<br />
A Member is not required to travel in excess of thirty (30)<br />
miles to reach a primary care provider or general hospital.<br />
A Member is not required to travel in excess of seventyfive<br />
(75) miles to secure an initial contact with a referral<br />
specialist, specialty hospital, psychiatric hospital, or<br />
diagnostic and therapeutic services (if one is available).<br />
Members should not wait longer than 45 minutes in the<br />
office waiting room prior to being taken to the examination<br />
room. Members should not wait more than 15 minutes to<br />
be seen by a provider after being taken to an examination<br />
room.<br />
3.8 Primary Care Provider Referrals to Other Providers<br />
Primary Care Provider Referrals to Network Providers<br />
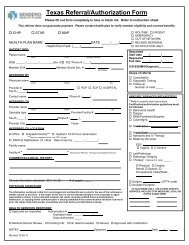
The <strong>Sendero</strong> PCP to In-Network Specialist Referral / Authorization Form or the Texas Authorization/Referral<br />
Form (see Appendix A of this manual) should be filled out and given to the Member when referring the<br />
Member to specialists or other ancillary providers for medically necessary services within the <strong>Sendero</strong> <strong>Health</strong><br />
<strong>Plans</strong>’ network. You should explain to the member that the specialist may not see the member without this<br />
form. The member needs to give this form to the specialist so that the specialist knows that the member is being<br />
referred by you, why the member is being referred, what the expectations are for the visit, and how many visits<br />
are being allowed.<br />
Primary Care Provider Referrals to Non-network Providers<br />
In rare situations, the primary care provider may believe that the most medically appropriate referral for a<br />
specific Member with a unique medical condition is to a non-network provider. Referral to non-network<br />
providers must be referred to the <strong>Health</strong> Services department for review and pre-authorization. <strong>Health</strong> Services<br />
must be given a written justification stating member specific reasons for Out-Of-Network care. For preauthorization<br />
of a non-network referral, the primary care provider must contact the <strong>Health</strong> Services Department<br />
by calling 1-855-297-9191, faxing a request to 512-275-2862, or complete an online referral on the<br />
<strong>Sendero</strong><strong>Health</strong>.com provider portal. Once the request for Out-of-Network care is received, it will be reviewed<br />
by <strong>Sendero</strong>’s Medical Director and sent to Network Management.<br />
3.9 Members Right to Self-Referral<br />
<strong>Sendero</strong> Customer Services 1-855-526-7388 Network Management 1-855-895-0475<br />
<strong>Health</strong> Services Dept.: 1-855-297-9191 (FAX 1-512-275-2862)