Download file, English (1 MB PDF) - RHO
Download file, English (1 MB PDF) - RHO
Download file, English (1 MB PDF) - RHO
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
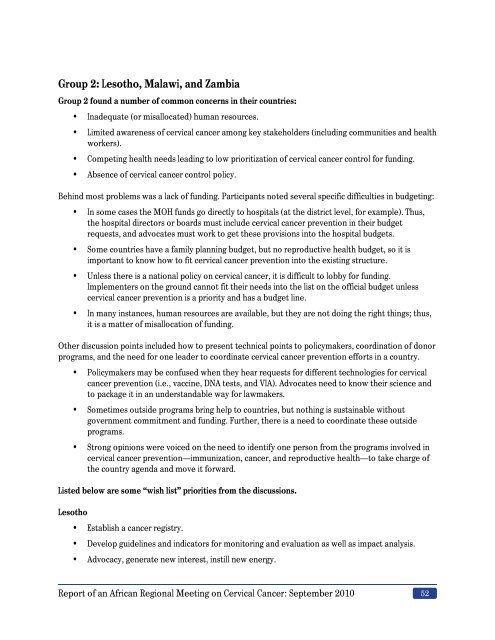
Group 2: Lesotho, Malawi, and Zambia<br />
Group 2 found a number of common concerns in their countries:<br />
• Inadequate (or misallocated) human resources.<br />
• Limited awareness of cervical cancer among key stakeholders (including communities and health<br />
workers).<br />
• Competing health needs leading to low prioritization of cervical cancer control for funding.<br />
• Absence of cervical cancer control policy.<br />
Behind most problems was a lack of funding. Participants noted several specific difficulties in budgeting:<br />
• In some cases the MOH funds go directly to hospitals (at the district level, for example). Thus,<br />
the hospital directors or boards must include cervical cancer prevention in their budget<br />
requests, and advocates must work to get these provisions into the hospital budgets.<br />
• Some countries have a family planning budget, but no reproductive health budget, so it is<br />
important to know how to fit cervical cancer prevention into the existing structure.<br />
• Unless there is a national policy on cervical cancer, it is difficult to lobby for funding.<br />
Implementers on the ground cannot fit their needs into the list on the official budget unless<br />
cervical cancer prevention is a priority and has a budget line.<br />
• In many instances, human resources are available, but they are not doing the right things; thus,<br />
it is a matter of misallocation of funding.<br />
Other discussion points included how to present technical points to policymakers, coordination of donor<br />
programs, and the need for one leader to coordinate cervical cancer prevention efforts in a country.<br />
• Policymakers may be confused when they hear requests for different technologies for cervical<br />
cancer prevention (i.e., vaccine, DNA tests, and VIA). Advocates need to know their science and<br />
to package it in an understandable way for lawmakers.<br />
• Sometimes outside programs bring help to countries, but nothing is sustainable without<br />
government commitment and funding. Further, there is a need to coordinate these outside<br />
programs.<br />
• Strong opinions were voiced on the need to identify one person from the programs involved in<br />
cervical cancer prevention—immunization, cancer, and reproductive health—to take charge of<br />
the country agenda and move it forward.<br />
Listed below are some “wish list” priorities from the discussions.<br />
Lesotho<br />
• Establish a cancer registry.<br />
• Develop guidelines and indicators for monitoring and evaluation as well as impact analysis.<br />
• Advocacy, generate new interest, instill new energy.<br />
Report of an African Regional Meeting on Cervical Cancer: September 2010 52