Advanced Effective Communication, Cultural Competence, and ...
Advanced Effective Communication, Cultural Competence, and ...
Advanced Effective Communication, Cultural Competence, and ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
A Roadmap for Hospitals<br />
Chapter Two: Assessment<br />
• Make sure the patient has been assigned to a room that<br />
can accommodate his or her mobility needs.<br />
• Make sure any mobility aid the patient uses (such as a<br />
service animal, cane, or walker) is readily accessible to<br />
the patient.<br />
• Determine whether the patient requires<br />
accommodations (such as adaptive switches or an<br />
intercom call system) to access the nurse call system.<br />
• Note the need for mobility assistance in the medical<br />
record <strong>and</strong> communicate these needs to staff.<br />
• Make sure appropriate precautions are in place to<br />
prevent falls. Some hospitals post a sign above the<br />
patient’s bed or door, or use special colored socks or<br />
bracelets to identify a patient at risk for falls.<br />
❑ Identify patient cultural, religious, or<br />
spiritual beliefs <strong>and</strong> practices that<br />
influence care.<br />
<strong>Cultural</strong>, religious, or spiritual beliefs can affect a patient’s<br />
or family’s perception of illness <strong>and</strong> how they approach<br />
treatment. In addition, patients may have unique needs<br />
associated with their cultural, religious, or spiritual beliefs<br />
that staff should acknowledge <strong>and</strong> address.<br />
• Ask the patient if there are any cultural, religious, or<br />
spiritual beliefs or practices that may influence his or<br />
her care.<br />
• Ask the patient if the hospital environment is<br />
welcoming to their cultural <strong>and</strong> religious or spiritual<br />
beliefs. Some religious-based hospitals display items in<br />
patient rooms that reflect the organization’s religious<br />
tradition <strong>and</strong> may conflict with the culture, religion,<br />
or spirituality of the patient <strong>and</strong> family. Consider<br />
removing the items, if possible, or covering them when<br />
necessary.<br />
• Respect the patient’s needs <strong>and</strong> preferences for<br />
modesty by assigning appropriate providers,<br />
uncovering only the parts of the body necessary for<br />
examination <strong>and</strong> treatment, providing privacy in<br />
toileting <strong>and</strong> washing, <strong>and</strong> using full gowns or robes<br />
for walking <strong>and</strong> transport. Many cultures <strong>and</strong> religions<br />
have restrictions on touching, distance, <strong>and</strong> modesty,<br />
which may be affected by providers of the opposite sex<br />
or staff that are younger or older than the patient.<br />
• Determine if the patient uses any complementary or<br />
alternative medicine or practices. Consider<br />
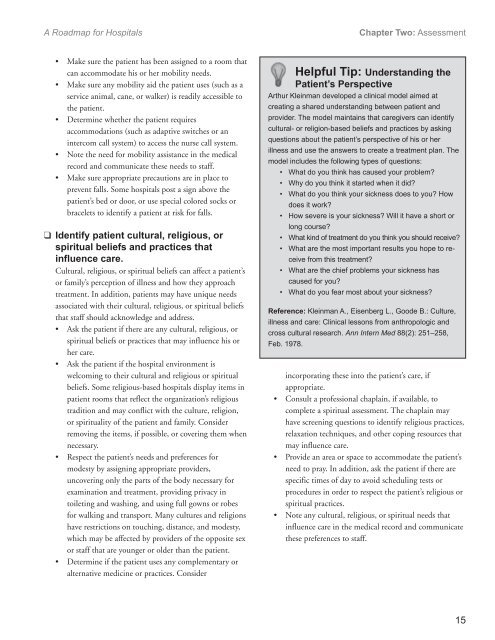
Helpful Tip: Underst<strong>and</strong>ing the<br />
Patient’s Perspective<br />
Arthur Kleinman developed a clinical model aimed at<br />
creating a shared underst<strong>and</strong>ing between patient <strong>and</strong><br />
provider. The model maintains that caregivers can identify<br />
cultural- or religion-based beliefs <strong>and</strong> practices by asking<br />
questions about the patient’s perspective of his or her<br />
illness <strong>and</strong> use the answers to create a treatment plan. The<br />
model includes the following types of questions:<br />
• What do you think has caused your problem?<br />
• Why do you think it started when it did?<br />
• What do you think your sickness does to you? How<br />
does it work?<br />
• How severe is your sickness? Will it have a short or<br />
long course?<br />
• What kind of treatment do you think you should receive?<br />
• What are the most important results you hope to receive<br />
from this treatment?<br />
• What are the chief problems your sickness has<br />
caused for you?<br />
• What do you fear most about your sickness?<br />
Reference: Kleinman A., Eisenberg L., Goode B.: Culture,<br />
illness <strong>and</strong> care: Clinical lessons from anthropologic <strong>and</strong><br />
cross cultural research. Ann Intern Med 88(2): 251–258,<br />
Feb. 1978.<br />
incorporating these into the patient’s care, if<br />
appropriate.<br />
• Consult a professional chaplain, if available, to<br />
complete a spiritual assessment. The chaplain may<br />
have screening questions to identify religious practices,<br />
relaxation techniques, <strong>and</strong> other coping resources that<br />
may influence care.<br />
• Provide an area or space to accommodate the patient’s<br />
need to pray. In addition, ask the patient if there are<br />
specific times of day to avoid scheduling tests or<br />
procedures in order to respect the patient’s religious or<br />
spiritual practices.<br />
• Note any cultural, religious, or spiritual needs that<br />
influence care in the medical record <strong>and</strong> communicate<br />
these preferences to staff.<br />
15