Advanced Effective Communication, Cultural Competence, and ...
Advanced Effective Communication, Cultural Competence, and ...
Advanced Effective Communication, Cultural Competence, and ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
A Roadmap for Hospitals<br />
Chapter Four: End-of-Life-Care<br />
decision-makers <strong>and</strong> family members whose preferred<br />
language is not English or who have sensory or<br />
communication impairments to facilitate involvement<br />
in end-of-life care. *<br />
• Make sure that appropriate communication supports<br />
are in place during care discussions; staff should not<br />
rely on the patient’s family or friends to interpret.<br />
• Notify the surrogate decision-maker <strong>and</strong> family of<br />
ongoing opportunities to ask questions. Encourage the<br />
surrogate decision-maker <strong>and</strong> family to write down<br />
questions for discussion with the care team.<br />
❑ Address patient mobility needs during<br />
end-of-life care.<br />
Patients receiving end-of-life care may develop new or<br />
additional mobility needs. The patient also may be at an<br />
increased risk for falls.<br />
• Assess whether the patient needs mobility assistance,<br />
including the type of <strong>and</strong> circumstances in which<br />
assistance is required.<br />
• Determine whether the patient requires<br />
accommodations (such as adaptive switches or an<br />
intercom call system) to access the nurse call system.<br />
• Make sure appropriate precautions are in place to<br />
prevent falls. Some hospitals post a sign above the<br />
patient’s bed or door or use special colored socks or<br />
bracelets to identify a patient at risk for falls.<br />
• Note the need for mobility assistance in the medical<br />
record <strong>and</strong> communicate these needs to staff.<br />
❑ Identify patient cultural, religious, or<br />
spiritual beliefs <strong>and</strong> practices at the<br />
end of life.<br />
<strong>Cultural</strong>, religious, or spiritual beliefs can affect the<br />
patient’s or his or her family’s perception of illness <strong>and</strong><br />
how they approach death <strong>and</strong> dying. End-of-life situations<br />
often trigger distress <strong>and</strong> reduce the patient’s ability to<br />
cope, communicate, <strong>and</strong> participate in care decisions.<br />
• Ask the patient if there are any cultural, religious, or<br />
spiritual beliefs or practices that may ease his or her<br />
care at the end of life.<br />
• Consult a professional chaplain, whenever possible,<br />
when staff identify a patient entering the end-of-life<br />
phase of care. The chaplain can complete a spiritual<br />
assessment <strong>and</strong> may have screening questions to<br />
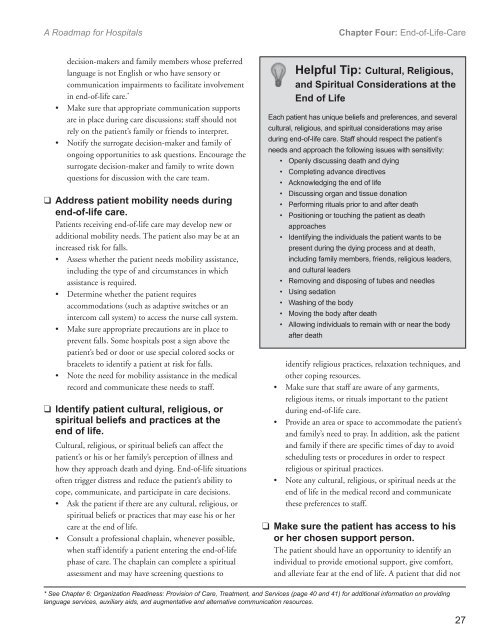
Helpful Tip: <strong>Cultural</strong>, Religious,<br />
<strong>and</strong> Spiritual Considerations at the<br />
End of Life<br />
Each patient has unique beliefs <strong>and</strong> preferences, <strong>and</strong> several<br />
cultural, religious, <strong>and</strong> spiritual considerations may arise<br />
during end-of-life care. Staff should respect the patient’s<br />
needs <strong>and</strong> approach the following issues with sensitivity:<br />
• Openly discussing death <strong>and</strong> dying<br />
• Completing advance directives<br />
• Acknowledging the end of life<br />
• Discussing organ <strong>and</strong> tissue donation<br />
• Performing rituals prior to <strong>and</strong> after death<br />
• Positioning or touching the patient as death<br />
approaches<br />
• Identifying the individuals the patient wants to be<br />
present during the dying process <strong>and</strong> at death,<br />
including family members, friends, religious leaders,<br />
<strong>and</strong> cultural leaders<br />
• Removing <strong>and</strong> disposing of tubes <strong>and</strong> needles<br />
• Using sedation<br />
• Washing of the body<br />
• Moving the body after death<br />
• Allowing individuals to remain with or near the body<br />
after death<br />
identify religious practices, relaxation techniques, <strong>and</strong><br />
other coping resources.<br />
• Make sure that staff are aware of any garments,<br />
religious items, or rituals important to the patient<br />
during end-of-life care.<br />
• Provide an area or space to accommodate the patient’s<br />
<strong>and</strong> family’s need to pray. In addition, ask the patient<br />
<strong>and</strong> family if there are specific times of day to avoid<br />
scheduling tests or procedures in order to respect<br />
religious or spiritual practices.<br />
• Note any cultural, religious, or spiritual needs at the<br />
end of life in the medical record <strong>and</strong> communicate<br />
these preferences to staff.<br />
❑ Make sure the patient has access to his<br />
or her chosen support person.<br />
The patient should have an opportunity to identify an<br />
individual to provide emotional support, give comfort,<br />
<strong>and</strong> alleviate fear at the end of life. A patient that did not<br />
* See Chapter 6: Organization Readiness: Provision of Care, Treatment, <strong>and</strong> Services (page 40 <strong>and</strong> 41) for additional information on providing<br />
language services, auxiliary aids, <strong>and</strong> augmentative <strong>and</strong> alternative communication resources.<br />
27