Major Health Issues in Nova Scotia: An Environmental Scan
Major Health Issues in Nova Scotia: An Environmental Scan
Major Health Issues in Nova Scotia: An Environmental Scan
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
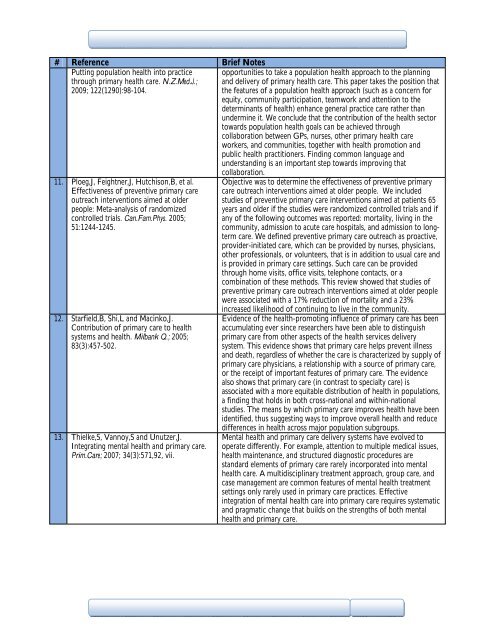
# Reference Brief Notes<br />
Putt<strong>in</strong>g population health <strong>in</strong>to practice<br />
through primary health care. N.Z.Med.J.;<br />
2009; 122(1290):98-104.<br />
opportunities to take a population health approach to the plann<strong>in</strong>g<br />
and delivery of primary health care. This paper takes the position that<br />
the features of a population health approach (such as a concern for<br />
equity, community participation, teamwork and attention to the<br />
determ<strong>in</strong>ants of health) enhance general practice care rather than<br />
underm<strong>in</strong>e it. We conclude that the contribution of the health sector<br />
towards population health goals can be achieved through<br />
collaboration between GPs, nurses, other primary health care<br />
workers, and communities, together with health promotion and<br />
public health practitioners. F<strong>in</strong>d<strong>in</strong>g common language and<br />
understand<strong>in</strong>g is an important step towards improv<strong>in</strong>g that<br />
11. Ploeg,J, Feightner,J, Hutchison,B, et al.<br />
Effectiveness of preventive primary care<br />
outreach <strong>in</strong>terventions aimed at older<br />
people: Meta-analysis of randomized<br />
controlled trials. Can.Fam.Phys. 2005;<br />
51:1244-1245.<br />
12. Starfield,B, Shi,L and Mac<strong>in</strong>ko,J.<br />
Contribution of primary care to health<br />
systems and health. Milbank Q.; 2005;<br />
83(3):457-502.<br />
13. Thielke,S, Vannoy,S and Unutzer,J.<br />
Integrat<strong>in</strong>g mental health and primary care.<br />
Prim.Care; 2007; 34(3):571,92, vii.<br />
collaboration.<br />
Objective was to determ<strong>in</strong>e the effectiveness of preventive primary<br />
care outreach <strong>in</strong>terventions aimed at older people. We <strong>in</strong>cluded<br />
studies of preventive primary care <strong>in</strong>terventions aimed at patients 65<br />
years and older if the studies were randomized controlled trials and if<br />
any of the follow<strong>in</strong>g outcomes was reported: mortality, liv<strong>in</strong>g <strong>in</strong> the<br />
community, admission to acute care hospitals, and admission to longterm<br />
care. We def<strong>in</strong>ed preventive primary care outreach as proactive,<br />
provider-<strong>in</strong>itiated care, which can be provided by nurses, physicians,<br />
other professionals, or volunteers, that is <strong>in</strong> addition to usual care and<br />
is provided <strong>in</strong> primary care sett<strong>in</strong>gs. Such care can be provided<br />
through home visits, office visits, telephone contacts, or a<br />
comb<strong>in</strong>ation of these methods. This review showed that studies of<br />
preventive primary care outreach <strong>in</strong>terventions aimed at older people<br />
were associated with a 17% reduction of mortality and a 23%<br />
<strong>in</strong>creased likelihood of cont<strong>in</strong>u<strong>in</strong>g to live <strong>in</strong> the community.<br />
Evidence of the health-promot<strong>in</strong>g <strong>in</strong>fluence of primary care has been<br />
accumulat<strong>in</strong>g ever s<strong>in</strong>ce researchers have been able to dist<strong>in</strong>guish<br />
primary care from other aspects of the health services delivery<br />
system. This evidence shows that primary care helps prevent illness<br />
and death, regardless of whether the care is characterized by supply of<br />
primary care physicians, a relationship with a source of primary care,<br />
or the receipt of important features of primary care. The evidence<br />
also shows that primary care (<strong>in</strong> contrast to specialty care) is<br />
associated with a more equitable distribution of health <strong>in</strong> populations,<br />
a f<strong>in</strong>d<strong>in</strong>g that holds <strong>in</strong> both cross-national and with<strong>in</strong>-national<br />
studies. The means by which primary care improves health have been<br />
identified, thus suggest<strong>in</strong>g ways to improve overall health and reduce<br />
differences <strong>in</strong> health across major population subgroups.<br />
Mental health and primary care delivery systems have evolved to<br />
operate differently. For example, attention to multiple medical issues,<br />
health ma<strong>in</strong>tenance, and structured diagnostic procedures are<br />
standard elements of primary care rarely <strong>in</strong>corporated <strong>in</strong>to mental<br />
health care. A multidiscipl<strong>in</strong>ary treatment approach, group care, and<br />
case management are common features of mental health treatment<br />
sett<strong>in</strong>gs only rarely used <strong>in</strong> primary care practices. Effective<br />
<strong>in</strong>tegration of mental health care <strong>in</strong>to primary care requires systematic<br />
and pragmatic change that builds on the strengths of both mental<br />
health and primary care.