View Full Screen - ADVANCE for NPs & PAs
View Full Screen - ADVANCE for NPs & PAs
View Full Screen - ADVANCE for NPs & PAs
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Diabetes<br />
Unrecognized diabetes is often discovered<br />
when patients are admitted <strong>for</strong><br />
a physiologic stressor such as infection<br />
or myocardial infarction. Hyperglycemia<br />
related to diabetes is usually identified<br />
when the first complete metabolic panel<br />
reveals a fasting blood glucose ≥ 126 mg/<br />
dL, a random blood glucose ≥ 200 mg/<br />
dL, or a hemoglobin A 1c ≥ 6.5%. 3<br />
Hyperglycemia related to hospitalization<br />
may include stress hyperglycemia<br />
Unrecognized diabetes<br />
is often discovered<br />
when patients are<br />
admitted <strong>for</strong> treatment<br />
of a physiologic stressor<br />
such as infection or<br />
heart attack.<br />
Hyperglycemia is usually<br />
identified in a complete<br />
metabolic panel.<br />
resulting from surgical procedures or use<br />
of other medications such as steroids. 4 In<br />
stress hyperglycemia, a patient meets the<br />
criteria <strong>for</strong> hyperglycemia with a random<br />
blood sugar ≥ 140 mg/dL, but he or she<br />
does not meet the hemoglobin A 1c criteria<br />
of > 6.5%. These patients have blood<br />
sugars that often return to normal after<br />
the stress is removed, but they should<br />
be monitored closely <strong>for</strong> development of<br />
prediabetes or diabetes after discharge. 4<br />
Diagnostic Criteria<br />
Diagnose DKA when the blood glucose is<br />
≥ 250 mg/dL, arterial pH is ≤ 7.30, serum<br />
bicarbonate is < 15 mEq/L, and positive<br />
serum ketones are present. 5 Diagnose<br />
HHS when blood glucose is 600 mg/dL or<br />
greater, serum osmolarity is 320 mOsm/<br />
kg or greater, profound dehydration is<br />
present with elevated serum blood urea<br />
nitrogen > 30 mg/dL, small ketonuria are<br />
present, and bicarbonate > 15 mEq/L. 6<br />
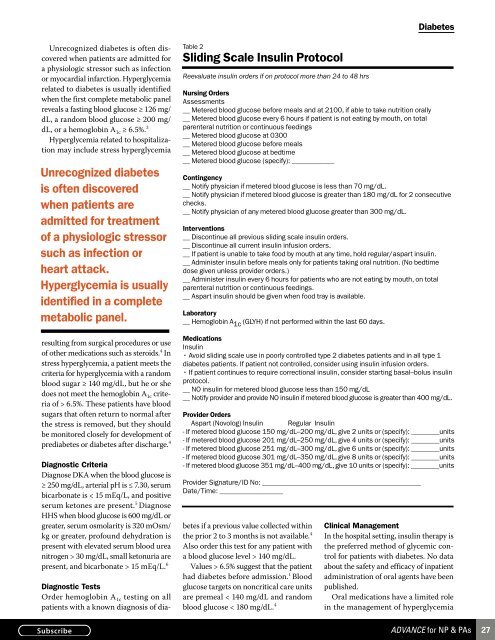
Table 2<br />
Sliding Scale Insulin Protocol<br />
Reevaluate insulin orders if on protocol more than 24 to 48 hrs<br />
Nursing Orders<br />
Assessments<br />
__ Metered blood glucose be<strong>for</strong>e meals and at 2100, if able to take nutrition orally<br />
__ Metered blood glucose every 6 hours if patient is not eating by mouth, on total<br />
parenteral nutrition or continuous feedings<br />
__ Metered blood glucose at 0300<br />
__ Metered blood glucose be<strong>for</strong>e meals<br />
__ Metered blood glucose at bedtime<br />
__ Metered blood glucose (specify): ____________<br />
Contingency<br />
__ Notify physician if metered blood glucose is less than 70 mg/dL.<br />
__ Notify physician if metered blood glucose is greater than 180 mg/dL <strong>for</strong> 2 consecutive<br />
checks.<br />
__ Notify physician of any metered blood glucose greater than 300 mg/dL.<br />
Interventions<br />
__ Discontinue all previous sliding scale insulin orders.<br />
__ Discontinue all current insulin infusion orders.<br />
__ If patient is unable to take food by mouth at any time, hold regular/aspart insulin.<br />
__ Administer insulin be<strong>for</strong>e meals only <strong>for</strong> patients taking oral nutrition. (No bedtime<br />
dose given unless provider orders.)<br />
__ Administer insulin every 6 hours <strong>for</strong> patients who are not eating by mouth, on total<br />
parenteral nutrition or continuous feedings.<br />
__ Aspart insulin should be given when food tray is available.<br />
Laboratory<br />
__ Hemoglobin A 1c (GLYH) if not per<strong>for</strong>med within the last 60 days.<br />
Medications<br />
Insulin<br />
• Avoid sliding scale use in poorly controlled type 2 diabetes patients and in all type 1<br />
diabetes patients. If patient not controlled, consider using insulin infusion orders.<br />
• If patient continues to require correctional insulin, consider starting basal–bolus insulin<br />
protocol.<br />
__ NO insulin <strong>for</strong> metered blood glucose less than 150 mg/dL<br />
__ Notify provider and provide NO insulin if metered blood glucose is greater than 400 mg/dL.<br />
Provider Orders<br />
Aspart (Novolog) Insulin Regular Insulin<br />
- If metered blood glucose 150 mg/dL–200 mg/dL, give 2 units or (specify): ________units<br />
- If metered blood glucose 201 mg/dL–250 mg/dL, give 4 units or (specify): ________units<br />
- If metered blood glucose 251 mg/dL–300 mg/dL, give 6 units or (specify): ________units<br />
- If metered blood glucose 301 mg/dL–350 mg/dL, give 8 units or (specify): ________units<br />
- If metered blood glucose 351 mg/dL–400 mg/dL, give 10 units or (specify): ________units<br />
Provider Signature/ID No: _____________________________________________<br />
Date/Time: __________________<br />
Diagnostic Tests<br />
Order hemoglobin A 1c testing on all<br />
patients with a known diagnosis of diabetes<br />
if a previous value collected within<br />
the prior 2 to 3 months is not available. 4<br />
Also order this test <strong>for</strong> any patient with<br />
a blood glucose level > 140 mg/dL.<br />
Values > 6.5% suggest that the patient<br />
had diabetes be<strong>for</strong>e admission. 1 Blood<br />
glucose targets on noncritical care units<br />
are premeal < 140 mg/dL and random<br />
blood glucose < 180 mg/dL. 4<br />
Clinical Management<br />
In the hospital setting, insulin therapy is<br />
the preferred method of glycemic control<br />
<strong>for</strong> patients with diabetes. No data<br />
about the safety and efficacy of inpatient<br />
administration of oral agents have been<br />
published.<br />
Oral medications have a limited role<br />
in the management of hyperglycemia<br />
<strong>ADVANCE</strong> <strong>for</strong> NP & <strong>PAs</strong><br />
27