Vol 41 # 3 September 2009 - Kma.org.kw
Vol 41 # 3 September 2009 - Kma.org.kw
Vol 41 # 3 September 2009 - Kma.org.kw
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
216<br />
External Non-Invasive Cardiac Pacemaker: Evaluation of Usefulness, Function and Capture...<br />
<strong>September</strong> <strong>2009</strong><br />
PATIENTS AND METHODS<br />
Study patients:<br />
Initially we enrolled 162 patients with<br />
symptomatic bradycardia or asystolic cardiac<br />
arrest but only 140 patients (124 male and 16<br />
female) with a mean age of 55.3 ± 6.4 years were<br />
included in the study. Twenty-two patients were<br />
excluded due to incomplete data. All patients were<br />
admitted in the coronary care unit (CCU) of the<br />
department of medicine with hemodynamically<br />
significant bradyarrhythmias between January 1997<br />
and <strong>September</strong> 2004. All patients were evaluated<br />
clinically by looking at history, physical examination,<br />
12-leads ECG, chest X-ray, routine laboratory<br />
investigations and echocardiography and Doppler<br />
study. Thirty- eight patients had type 2 diabetes<br />
mellitus but no patient had ketoacidosis. Twentythree<br />
patients had history of chronic obstructive<br />
pulmonary disease (COPD). Twenty-six patients<br />
had history of coronary artery bypass graft (CABG)<br />
surgery with post-sternotomy scar. The study was<br />
approved by the hospital ethical committee.<br />
Methods:<br />
We trained all CCU nursing staff to perform<br />
transcutaneous pacing in one to two-hour classes.<br />
Informed consent was obtained from patients for<br />
insertion of intravenous temporary pacemaker (ITP)<br />
if necessary.<br />
Pacing devices:<br />
Three different new pacemaker devices were used<br />
in the study and all were devices of the modified<br />
version which was introduced in 1983 [8] .<br />
1. CardioMaster device in 48 patients<br />
2. CardioLife device in 40 patients<br />
3. CardioServe device in 52 patients<br />
The NTP consists of an electric cardiac pacemaker<br />
combined with a cardiac monitor and a paper<br />
recorder. The pacemaker monitor senses voltage<br />
changes of appropriate amplitude and slew rate<br />
from cardiac depolarizations or pacemaker stimuli.<br />
It provides audible and visual signals of such events<br />
with oscilloscopic and paper recordings, displays<br />
their rate and rings an alarm if selected limits are<br />
exceeded. The pacemaker functions in the demand<br />
mode (VVI), emitting stimuli that are synchronized<br />
to the sensed electrical signals at escape rates up to<br />
180 beats/minute and an amplitude upto 140 mA.<br />
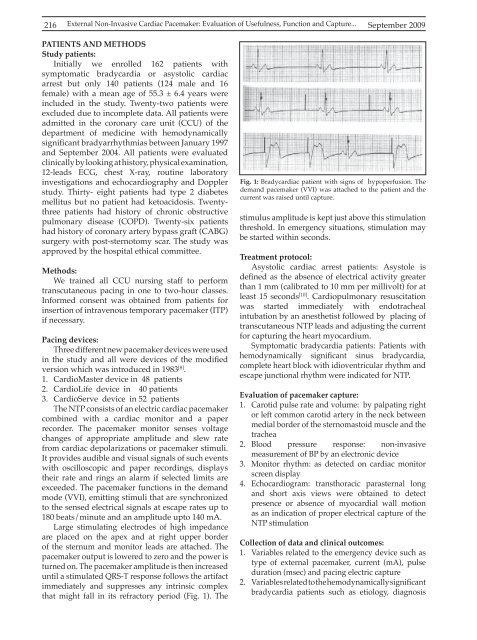
Large stimulating electrodes of high impedance<br />
are placed on the apex and at right upper border<br />
of the sternum and monitor leads are attached. The<br />
pacemaker output is lowered to zero and the power is<br />
turned on. The pacemaker amplitude is then increased<br />
until a stimulated QRS-T response follows the artifact<br />
immediately and suppresses any intrinsic complex<br />
that might fall in its refractory period (Fig. 1). The<br />
Fig. 1: Bradycardiac patient with signs of hypoperfusion. The<br />
demand pacemaker (VVI) was attached to the patient and the<br />
current was raised until capture.<br />
stimulus amplitude is kept just above this stimulation<br />
threshold. In emergency situations, stimulation may<br />
be started within seconds.<br />
Treatment protocol:<br />
Asystolic cardiac arrest patients: Asystole is<br />
defined as the absence of electrical activity greater<br />
than 1 mm (calibrated to 10 mm per millivolt) for at<br />
least 15 seconds [10] . Cardiopulmonary resuscitation<br />
was started immediately with endotracheal<br />
intubation by an anesthetist followed by placing of<br />
transcutaneous NTP leads and adjusting the current<br />
for capturing the heart myocardium.<br />
Symptomatic bradycardia patients: Patients with<br />
hemodynamically significant sinus bradycardia,<br />
complete heart block with idioventricular rhythm and<br />
escape junctional rhythm were indicated for NTP.<br />
Evaluation of pacemaker capture:<br />
1. Carotid pulse rate and volume: by palpating right<br />
or left common carotid artery in the neck between<br />
medial border of the sternomastoid muscle and the<br />
trachea<br />
2. Blood pressure response: non-invasive<br />
measurement of BP by an electronic device<br />
3. Monitor rhythm: as detected on cardiac monitor<br />
screen display<br />
4. Echocardiogram: transthoracic parasternal long<br />
and short axis views were obtained to detect<br />
presence or absence of myocardial wall motion<br />
as an indication of proper electrical capture of the<br />
NTP stimulation<br />
Collection of data and clinical outcomes:<br />
1. Variables related to the emergency device such as<br />
type of external pacemaker, current (mA), pulse<br />
duration (msec) and pacing electric capture<br />
2. Variables related to the hemodynamically significant<br />
bradycardia patients such as etiology, diagnosis