FY2011 Health Benefits Booklet
FY2011 Health Benefits Booklet
FY2011 Health Benefits Booklet
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Maryland State Employees and Retirees 43<br />
Out-of-Area Emergencies<br />
The United Concordia DHMO will pay a maximum<br />
of $50, subject to your fee schedule, for emergency<br />
dental services when you are traveling out of the area<br />
(more than 50 miles from your dentist’s office). To<br />
receive payment for out-of-area emergency care, you<br />
must submit a bill itemizing the charges and services<br />
performed, and forward the claim to UCCI for<br />
processing.<br />
DHMO Network<br />
If you live in an area or move to an area that is not in<br />
the DHMO network of dentists, please contact UCCI<br />
to determine other options. To enroll in the DHMO<br />
plan, you must reside within the Maryland service<br />
area (MD, DC, VA, DE, WV, PA). In addition, you<br />
may request that the plan evaluate the dentist of<br />
your choice for inclusion in the network. However,<br />
there is no guarantee that a provider that you request<br />
will choose to participate in the plan network. In<br />
the DHMO plan, you can only receive coverage for<br />
services from a DHMO plan provider.<br />
The DPPO Plan<br />
The DPPO plan is also available through United<br />
Concordia. Under this Plan, you do not have to select<br />
a PDO. You may choose to receive services from<br />
any dentist of your choice whenever you need care.<br />
If you use an out-of-network dentist, you will need<br />
to submit a claim form for reimbursement and may<br />
be billed by the dentist for the amount charged that<br />
exceeds the allowed amount. No referrals are needed<br />
for specialty care. Orthodontia services are only<br />
covered for eligible children age 25 and younger.<br />
When you use an in-network DPPO dentist, the<br />
in-network dentist will directly bill the plan for the<br />
amount the plan will pay, and will bill you for the<br />
amount you are required to pay under the plan.<br />
DENTAL<br />
BENEFITS<br />
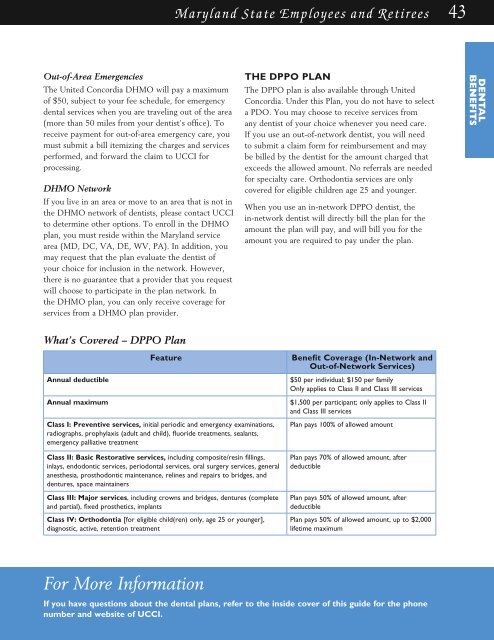
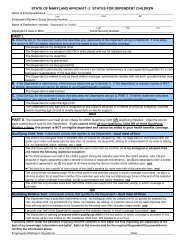
What’s Covered – DPPO Plan<br />
Annual deductible<br />
Annual maximum<br />
Feature<br />
Class I: Preventive services, initial periodic and emergency examinations,<br />
radiographs, prophylaxis (adult and child), fluoride treatments, sealants,<br />
emergency palliative treatment<br />
Class II: Basic Restorative services, including composite/resin fillings,<br />
inlays, endodontic services, periodontal services, oral surgery services, general<br />
anesthesia, prosthodontic maintenance, relines and repairs to bridges, and<br />
dentures, space maintainers<br />
Class III: Major services, including crowns and bridges, dentures (complete<br />
and partial), fixed prosthetics, implants<br />
Class IV: Orthodontia [for eligible child(ren) only, age 25 or younger],<br />
diagnostic, active, retention treatment<br />
Benefit Coverage (In-Network and<br />
Out-of-Network Services)<br />
$50 per individual; $150 per family<br />
Only applies to Class II and Class III services<br />
$1,500 per participant; only applies to Class II<br />
and Class III services<br />
Plan pays 100% of allowed amount<br />
Plan pays 70% of allowed amount, after<br />
deductible<br />
Plan pays 50% of allowed amount, after<br />
deductible<br />
Plan pays 50% of allowed amount, up to $2,000<br />
lifetime maximum<br />
For More Information<br />
If you have questions about the dental plans, refer to the inside cover of this guide for the phone<br />
number and website of UCCI.