FY2011 Health Benefits Booklet
FY2011 Health Benefits Booklet
FY2011 Health Benefits Booklet
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
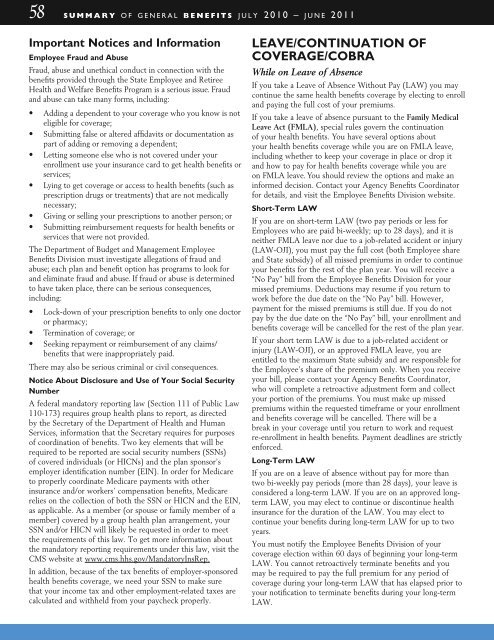
58 s u m m a r y o f g e n e r a l b e n e f i t s j u l y 2 0 1 0 – j u n e 2 0 1 1<br />
Important Notices and Information<br />
Employee Fraud and Abuse<br />
Fraud, abuse and unethical conduct in connection with the<br />
benefits provided through the State Employee and Retiree<br />
<strong>Health</strong> and Welfare <strong>Benefits</strong> Program is a serious issue. Fraud<br />
and abuse can take many forms, including:<br />
• Adding a dependent to your coverage who you know is not<br />
eligible for coverage;<br />
• Submitting false or altered affidavits or documentation as<br />
part of adding or removing a dependent;<br />
• Letting someone else who is not covered under your<br />
enrollment use your insurance card to get health benefits or<br />
services;<br />
• Lying to get coverage or access to health benefits (such as<br />
prescription drugs or treatments) that are not medically<br />
necessary;<br />
• Giving or selling your prescriptions to another person; or<br />
• Submitting reimbursement requests for health benefits or<br />
services that were not provided.<br />
The Department of Budget and Management Employee<br />
<strong>Benefits</strong> Division must investigate allegations of fraud and<br />
abuse; each plan and benefit option has programs to look for<br />
and eliminate fraud and abuse. If fraud or abuse is determined<br />
to have taken place, there can be serious consequences,<br />
including:<br />
• Lock-down of your prescription benefits to only one doctor<br />
or pharmacy;<br />
• Termination of coverage; or<br />
• Seeking repayment or reimbursement of any claims/<br />
benefits that were inappropriately paid.<br />
There may also be serious criminal or civil consequences.<br />
Notice About Disclosure and Use of Your Social Security<br />
Number<br />
A federal mandatory reporting law (Section 111 of Public Law<br />
110-173) requires group health plans to report, as directed<br />
by the Secretary of the Department of <strong>Health</strong> and Human<br />
Services, information that the Secretary requires for purposes<br />
of coordination of benefits. Two key elements that will be<br />
required to be reported are social security numbers (SSNs)<br />
of covered individuals (or HICNs) and the plan sponsor’s<br />
employer identification number (EIN). In order for Medicare<br />
to properly coordinate Medicare payments with other<br />
insurance and/or workers’ compensation benefits, Medicare<br />
relies on the collection of both the SSN or HICN and the EIN,<br />
as applicable. As a member (or spouse or family member of a<br />
member) covered by a group health plan arrangement, your<br />
SSN and/or HICN will likely be requested in order to meet<br />
the requirements of this law. To get more information about<br />
the mandatory reporting requirements under this law, visit the<br />
CMS website at www.cms.hhs.gov/MandatoryInsRep.<br />
In addition, because of the tax benefits of employer-sponsored<br />
health benefits coverage, we need your SSN to make sure<br />
that your income tax and other employment-related taxes are<br />
calculated and withheld from your paycheck properly.<br />
Leave/Continuation of<br />
Coverage/COBRA<br />
While on Leave of Absence<br />
If you take a Leave of Absence Without Pay (LAW) you may<br />
continue the same health benefits coverage by electing to enroll<br />
and paying the full cost of your premiums.<br />
If you take a leave of absence pursuant to the Family Medical<br />
Leave Act (FMLA), special rules govern the continuation<br />
of your health benefits. You have several options about<br />
your health benefits coverage while you are on FMLA leave,<br />
including whether to keep your coverage in place or drop it<br />
and how to pay for health benefits coverage while you are<br />
on FMLA leave. You should review the options and make an<br />
informed decision. Contact your Agency <strong>Benefits</strong> Coordinator<br />
for details, and visit the Employee <strong>Benefits</strong> Division website.<br />
Short-Term LAW<br />
If you are on short-term LAW (two pay periods or less for<br />
Employees who are paid bi-weekly; up to 28 days), and it is<br />
neither FMLA leave nor due to a job-related accident or injury<br />
(LAW-OJI), you must pay the full cost (both Employee share<br />
and State subsidy) of all missed premiums in order to continue<br />
your benefits for the rest of the plan year. You will receive a<br />
“No Pay” bill from the Employee <strong>Benefits</strong> Division for your<br />
missed premiums. Deductions may resume if you return to<br />
work before the due date on the “No Pay” bill. However,<br />
payment for the missed premiums is still due. If you do not<br />
pay by the due date on the “No Pay” bill, your enrollment and<br />
benefits coverage will be cancelled for the rest of the plan year.<br />
If your short term LAW is due to a job-related accident or<br />
injury (LAW-OJI), or an approved FMLA leave, you are<br />
entitled to the maximum State subsidy and are responsible for<br />
the Employee’s share of the premium only. When you receive<br />
your bill, please contact your Agency <strong>Benefits</strong> Coordinator,<br />
who will complete a retroactive adjustment form and collect<br />
your portion of the premiums. You must make up missed<br />
premiums within the requested timeframe or your enrollment<br />
and benefits coverage will be cancelled. There will be a<br />
break in your coverage until you return to work and request<br />
re-enrollment in health benefits. Payment deadlines are strictly<br />
enforced.<br />
Long-Term LAW<br />
If you are on a leave of absence without pay for more than<br />
two bi-weekly pay periods (more than 28 days), your leave is<br />
considered a long-term LAW. If you are on an approved longterm<br />
LAW, you may elect to continue or discontinue health<br />
insurance for the duration of the LAW. You may elect to<br />
continue your benefits during long-term LAW for up to two<br />
years.<br />
You must notify the Employee <strong>Benefits</strong> Division of your<br />
coverage election within 60 days of beginning your long-term<br />
LAW. You cannot retroactively terminate benefits and you<br />
may be required to pay the full premium for any period of<br />
coverage during your long-term LAW that has elapsed prior to<br />
your notification to terminate benefits during your long-term<br />
LAW.