FY2011 Health Benefits Booklet
FY2011 Health Benefits Booklet
FY2011 Health Benefits Booklet
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
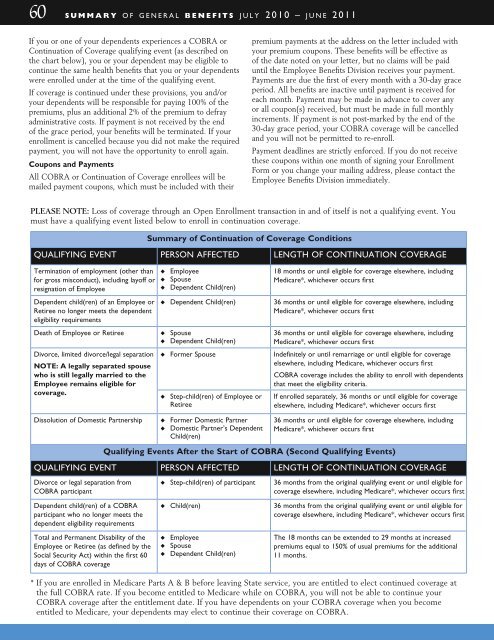
60 s u m m a r y o f g e n e r a l b e n e f i t s j u l y 2 0 1 0 – j u n e 2 0 1 1<br />
If you or one of your dependents experiences a COBRA or<br />
Continuation of Coverage qualifying event (as described on<br />
the chart below), you or your dependent may be eligible to<br />
continue the same health benefits that you or your dependents<br />
were enrolled under at the time of the qualifying event.<br />
If coverage is continued under these provisions, you and/or<br />
your dependents will be responsible for paying 100% of the<br />
premiums, plus an additional 2% of the premium to defray<br />
administrative costs. If payment is not received by the end<br />
of the grace period, your benefits will be terminated. If your<br />
enrollment is cancelled because you did not make the required<br />
payment, you will not have the opportunity to enroll again.<br />
Coupons and Payments<br />
All COBRA or Continuation of Coverage enrollees will be<br />
mailed payment coupons, which must be included with their<br />
premium payments at the address on the letter included with<br />
your premium coupons. These benefits will be effective as<br />
of the date noted on your letter, but no claims will be paid<br />
until the Employee <strong>Benefits</strong> Division receives your payment.<br />
Payments are due the first of every month with a 30-day grace<br />
period. All benefits are inactive until payment is received for<br />
each month. Payment may be made in advance to cover any<br />
or all coupon(s) received, but must be made in full monthly<br />
increments. If payment is not post-marked by the end of the<br />
30-day grace period, your COBRA coverage will be cancelled<br />
and you will not be permitted to re-enroll.<br />
Payment deadlines are strictly enforced. If you do not receive<br />
these coupons within one month of signing your Enrollment<br />
Form or you change your mailing address, please contact the<br />
Employee <strong>Benefits</strong> Division immediately.<br />
PLEASE NOTE: Loss of coverage through an Open Enrollment transaction in and of itself is not a qualifying event. You<br />
must have a qualifying event listed below to enroll in continuation coverage.<br />
Summary of Continuation of Coverage Conditions<br />
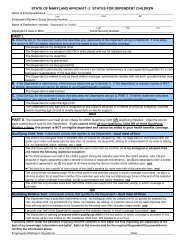
quALIFYINg evENT person AFFECTED lengTH OF CONTINuATION COvERAge<br />
Termination of employment (other than<br />
for gross misconduct), including layoff or<br />
resignation of Employee<br />
Dependent child(ren) of an Employee or<br />
Retiree no longer meets the dependent<br />
eligibility requirements<br />
Death of Employee or Retiree<br />
Divorce, limited divorce/legal separation<br />
NOTE: A legally separated spouse<br />
who is still legally married to the<br />
Employee remains eligible for<br />
coverage.<br />
u Employee<br />
u Spouse<br />
u Dependent Child(ren)<br />
u Dependent Child(ren)<br />
u Spouse<br />
u Dependent Child(ren)<br />
u Former Spouse<br />
u Step-child(ren) of Employee or<br />
Retiree<br />
18 months or until eligible for coverage elsewhere, including<br />
Medicare*, whichever occurs first<br />
36 months or until eligible for coverage elsewhere, including<br />
Medicare*, whichever occurs first<br />
36 months or until eligible for coverage elsewhere, including<br />
Medicare*, whichever occurs first<br />
Indefinitely or until remarriage or until eligible for coverage<br />
elsewhere, including Medicare, whichever occurs first<br />
COBRA coverage includes the ability to enroll with dependents<br />
that meet the eligibility criteria.<br />
If enrolled separately, 36 months or until eligible for coverage<br />
elsewhere, including Medicare*, whichever occurs first<br />
Dissolution of Domestic Partnership<br />
u Former Domestic Partner<br />
u Domestic Partner’s Dependent<br />
Child(ren)<br />
36 months or until eligible for coverage elsewhere, including<br />
Medicare*, whichever occurs first<br />
Qualifying Events After the Start of coBra (Second Qualifying Events)<br />
quALIFYINg evENT person AFFECTED lengTH OF CONTINuATION COvERAge<br />
Divorce or legal separation from<br />
COBRA participant<br />
u Step-child(ren) of participant<br />
36 months from the original qualifying event or until eligible for<br />
coverage elsewhere, including Medicare*, whichever occurs first<br />
Dependent child(ren) of a COBRA<br />
participant who no longer meets the<br />
dependent eligibility requirements<br />
Total and Permanent Disability of the<br />
Employee or Retiree (as defined by the<br />
Social Security Act) within the first 60<br />
days of COBRA coverage<br />
u Child(ren)<br />
u Employee<br />
u Spouse<br />
u Dependent Child(ren)<br />
36 months from the original qualifying event or until eligible for<br />
coverage elsewhere, including Medicare*, whichever occurs first<br />
The 18 months can be extended to 29 months at increased<br />
premiums equal to 150% of usual premiums for the additional<br />
11 months.<br />
* If you are enrolled in Medicare Parts A & B before leaving State service, you are entitled to elect continued coverage at<br />
the full COBRA rate. If you become entitled to Medicare while on COBRA, you will not be able to continue your<br />
COBRA coverage after the entitlement date. If you have dependents on your COBRA coverage when you become<br />
entitled to Medicare, your dependents may elect to continue their coverage on COBRA.