FY2011 Health Benefits Booklet
FY2011 Health Benefits Booklet
FY2011 Health Benefits Booklet
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
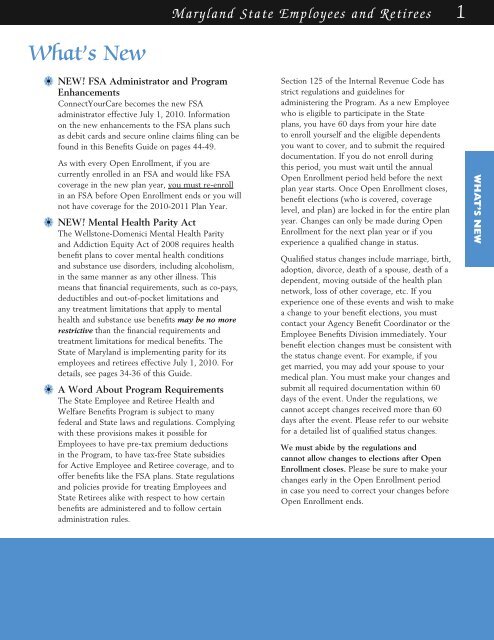
Maryland State Employees and Retirees 1<br />
What’s New<br />
a• NEW! FSA Administrator and Program<br />
Enhancements<br />
ConnectYourCare becomes the new FSA<br />
administrator effective July 1, 2010. Information<br />
on the new enhancements to the FSA plans such<br />
as debit cards and secure online claims filing can be<br />
found in this <strong>Benefits</strong> Guide on pages 44-49.<br />
As with every Open Enrollment, if you are<br />
currently enrolled in an FSA and would like FSA<br />
coverage in the new plan year, you must re-enroll<br />
in an FSA before Open Enrollment ends or you will<br />
not have coverage for the 2010-2011 Plan Year.<br />
a• NEW! Mental <strong>Health</strong> Parity Act<br />
The Wellstone-Domenici Mental <strong>Health</strong> Parity<br />
and Addiction Equity Act of 2008 requires health<br />
benefit plans to cover mental health conditions<br />
and substance use disorders, including alcoholism,<br />
in the same manner as any other illness. This<br />
means that financial requirements, such as co-pays,<br />
deductibles and out-of-pocket limitations and<br />
any treatment limitations that apply to mental<br />
health and substance use benefits may be no more<br />
restrictive than the financial requirements and<br />
treatment limitations for medical benefits. The<br />
State of Maryland is implementing parity for its<br />
employees and retirees effective July 1, 2010. For<br />
details, see pages 34-36 of this Guide.<br />
a• A Word About Program Requirements<br />
The State Employee and Retiree <strong>Health</strong> and<br />
Welfare <strong>Benefits</strong> Program is subject to many<br />
federal and State laws and regulations. Complying<br />
with these provisions makes it possible for<br />
Employees to have pre-tax premium deductions<br />
in the Program, to have tax-free State subsidies<br />
for Active Employee and Retiree coverage, and to<br />
offer benefits like the FSA plans. State regulations<br />
and policies provide for treating Employees and<br />
State Retirees alike with respect to how certain<br />
benefits are administered and to follow certain<br />
administration rules.<br />
Section 125 of the Internal Revenue Code has<br />
strict regulations and guidelines for<br />
administering the Program. As a new Employee<br />
who is eligible to participate in the State<br />
plans, you have 60 days from your hire date<br />
to enroll yourself and the eligible dependents<br />
you want to cover, and to submit the required<br />
documentation. If you do not enroll during<br />
this period, you must wait until the annual<br />
Open Enrollment period held before the next<br />
plan year starts. Once Open Enrollment closes,<br />
benefit elections (who is covered, coverage<br />
level, and plan) are locked in for the entire plan<br />
year. Changes can only be made during Open<br />
Enrollment for the next plan year or if you<br />
experience a qualified change in status.<br />
Qualified status changes include marriage, birth,<br />
adoption, divorce, death of a spouse, death of a<br />
dependent, moving outside of the health plan<br />
network, loss of other coverage, etc. If you<br />
experience one of these events and wish to make<br />
a change to your benefit elections, you must<br />
contact your Agency Benefit Coordinator or the<br />
Employee <strong>Benefits</strong> Division immediately. Your<br />
benefit election changes must be consistent with<br />
the status change event. For example, if you<br />
get married, you may add your spouse to your<br />
medical plan. You must make your changes and<br />
submit all required documentation within 60<br />
days of the event. Under the regulations, we<br />
cannot accept changes received more than 60<br />
days after the event. Please refer to our website<br />
for a detailed list of qualified status changes.<br />
We must abide by the regulations and<br />
cannot allow changes to elections after Open<br />
Enrollment closes. Please be sure to make your<br />
changes early in the Open Enrollment period<br />
in case you need to correct your changes before<br />
Open Enrollment ends.<br />
WHAT’S NEW