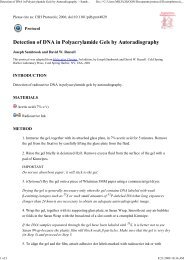
NEWS feature© 2010 Nature America, Inc. All rights reserved.tumors respond to Herceptin alone 2 . “It’s notjust a simple translation of gene overamplificationto susceptibility to the drug,” says LarryNorton, of Memorial Sloan-Kettering CancerCenter in New York.Others wonder if the test is even necessary.Studies from two clinical trials (NSABP B31and NCCTG N9831) presented at the AmericanSociety of Clinical Oncologists (ASCO) annualmeeting in 2007 (ref. 3) suggested that someindividuals with HER2-negative tumorscan benefit from Herceptin. In these trials,which comparedchemotherapyalone with chemotherapyplus CentromereaHerceptin, onlywomen who wereHER2 positivecould participate.Upon retesting,however, sometumor samplescame up negative.Nonetheless,some womenwith negativetest results benefitedfrom thedrug, which hasspurred a nowl ong-runningdebate. Althoughmany expertsbelieve this findingto be an artifactof variationin test accuracy,others think thismay be anotherimportant clue.“It’s easy todismiss a findingyou can’texplain, but thisbis forcing us to reexamine our notions of whatbeing HER2 positive or negative means,” saysNorton.The controversy around these particular trialfindings may be resolved soon. Samples fromthe NCCTG N9831 trial are being retested in around-robin fashion by three different groups.Results will then be sent to a central monitoringgroup to identify any discrepancies and totry to pinpoint their cause. Soonmyung Paikof the National Surgical Adjuvant Breast andBowel Project (a National Cancer Institute(NCI)-sponsored cooperative based at theUniversity of Pittsburgh) postulates that individualswith HER2-negative primary tumorsmay have circulating tumor cells that are HER2Her2 (ERBB2)~190 kbLSI HER2positive, but he admits that the discrepancycould just reflect problems with the tests. Hisgroup is doing further microarray analysis ofthe NSABP trial samples. If the earlier findingsare confirmed, a trial could be launched in thesummer of 2010 to test Herceptin in patientswith HER2-negative tumors. “We have an NCIapprovedprotocol,” Paik writes in an e-mail.Abundance of richesFrom the time Herceptin was launched, expertshave warned that existing tests have problems.The most commonlyused test,an immunohis-Telomere tochemistry-17q11.2–q12 regionbased assay,happens to bethe least dependable,especiallywhen performedin laboratoriesthat do onlyoccasional tests.The immunohistochemistrytestmeasures proteinlevels, whereasthe newer FISHbasedtests measuresgene copynumber andare believed tobe more reliable,especiallyin expert hands.Some thinkthe FISH assayshould be thestandard, butclearly, it makesa big differencewho is doing thetesting. In 2006,ASCO and theCollege of American Pathologists releasedstricter guidelines which, according to Ross,forced many laboratories that had low test volumesto send the samples to laboratories withhigher volumes and more experience. But someexperts were dismayed that the new guidelinesdid not recommend FISH over immunohistochemistry.Others, including Norton, are skeptical of allavailable tests. The FISH probe, he points out,is large (190 kilobases in the case of the Vysisprobe), spanning the gene and then some (Fig. 1).“When you see changes in HER2 at the genecopy number level, is that a reflection of HER2itself or of generalized genomic instability?” heasks. Genomic instability, he points out, is notFigure 1 FISHing for HER2. (a) Probe map shows therelative size of the Vysis LSI HER2 probe and the gene.(b) An example of a FISH test for HER2 amplificationshows multiple copies of the HER2 gene (red clusterssignals) compared to chromosome number (green signals).Source: Abbott.a random event and the region where HER2is found is a ‘hot spot’. Norton thinks that theprescribing of HER2-targeting drugs won’t beimproved until we understand how specificmutations influence a tumor’s susceptibilityand sequencing can be routinely done onbiopsies. Comparative genome hybridization(CGH) studies done in his laboratory suggestthat simple ‘amplified’ and ‘nonamplified’ readingsavailable from FISH do not adequatelyreflect the complex changes that can occur inthis region. For example, CGH studies revealedthat in some samples that were HER2 positiveon FISH, the amplified area was actually adjacentto HER2 and not within it 4 . It may endup that higher resolution methods like CGHare needed to get the right information abouta tumor’s status.Meanwhile, companies like Genomic Healthin Redwood City, California, and Labcorp’sMonogram Sciences of S. San Francisco,California, are jumping in with new approachesto testing breast cancer patients. GenomicHealth claims that an advantage of its quantitativePCR-based test, OncotypeDX, is its accuracy.“Our test is more than 95% concordantwith reference labs’ assessment by FISH,” saysSteve Shak, chief medical officer at GenomicHealth. HER2 is one of 21 genes included inOncotypeDX, which is used to quantify therisk of recurrence of early breast cancer and theresponse to particular types of chemotherapy.Starting in 2008, the company began includingestrogen receptor, progesterone receptor andHER2 status in every report it provides.Monogram’s HERMark test measures HER2total protein as well as functional homodimersin a dual-antibody format. The company claimsthe test has advantages over FISH because it is adirect measurement of the protein, and that itis seven to ten times more sensitive than immunohistochemistrytesting. Albany MedicalCollege’s Ross counters, “Monogram has noprospective randomized data to support thattheir test is better.”Neither company’s test is FDA approvedfor use with Herceptin. For now, the tests’use may be confined to confirming or clarifyingresults obtained using other tests. “Weneed not just technical accuracy but to knowif these tests are actually clinically relevant,”says Edith Perez, of the Mayo Clinic Floridain Jacksonville. But Genomic Health seemsoptimistic. “We have extremely positivefeedback on the value of being able to lookat that result, especially in those cases whenthe results for HER2 testing are uncertain,”says Shak. The company is doing additionalstudies of the test’s ability to predict whetherparticular individuals will benefit fromHER2-targeted therapy.118 volume 28 number 2 february 2010 nature biotechnology
news feature© 2010 Nature America, Inc. All rights reserved.Others wonder whether HER2 is eventhe right thing to test. Strategic Medicine’sLiebman, who was at Vysis (now part of AbbottLaboratories of Abbott Park, Illinois) whenthe first FISH test was developed, says that forcertain patients, the immunohistochemistryand FISH results never agree. “Just becauseyou have a change in gene copy number, thatdoesn’t mean it’s expressed,” he says. The factthat a significant fraction of HER2-positivepatients with metastatic disease fail to respondto the drug also suggests that it is not a causalmarker but a surrogate.There may be room for yet more tests.Microarray studies indicate that between 20to 30 distinct classes of breast cancer exist,according to Charles Perou, of the LinebergerComprehensive Cancer Center in Chapel Hill,North Carolina. A few of those make up themost clinically relevant subtypes, but there areenough differences between those types thatmore and better tests are urgently needed.“Our array data show that there are at leasttwo kinds, and maybe many more, of patientswith HER2-positive disease,” he says. The differencecan be seen in how the patients respondto chemotherapy, with 80% responding in onegroup and only 30% in the other.Son of HerceptinOne other HER2-targeting drug, the smallmoleculeTykerb (lapatinib from London-basedGlaxoSmithKline), is now approved for use inbreast cancer, but a bevy of next-generationversions of Herceptin and new combinationswith the drug are nearing the market, potentiallygiving oncologists even more choiceswhen deciding which drug to use and whento use it.Genentech currently has two new HER2-targeting drugs in phase 3 trials. Pertuzumabis a HER2 dimerization inhibitor that binds toa different epitope on HER2 than Herceptin.The drug inhibits HER2 dimer formation withother HER family members, such as HER3and HER1. Genentech is currently studying acombination of both HER2 inhibitors in breastcancer. “With this approach, we are addressingthe question of what happens when youhave more complete HER2/neu blockade,” saysGenentech’s Sliwkowski. The drug has alreadyshown promise in early trials. In one study,about a quarter of women whose disease hadprogressed while they were taking Herceptinhad their tumors shrink by >50% when pertuzumabwas added to their treatment regimen.The company is also optimistic aboutT-DM1 (trastuzumab-DM1), a drug conjugatethat combines Waltham, Massachusetts–basedImmunoGen’s antimitotic maytansinederivativeDM1 cancer-killing agent withHerceptin. In earlier studies, this drug madetumors shrink even in some women withadvanced breast cancer who had been treatedwith a median of seven different drugs. Thedrug is being “moved up the line,” accordingto Sliwkowski, and will be tested in a randomizedphase 2 trial comparing TDM-1 versusHerceptin plus chemotherapy. “We think it isso active that it’s important to try this,” saysSliwkowski. To be able to use a targeted therapywithout chemotherapy is the dream and it maybe very close to realization.Dennis Slamon, a University of California,Los Angeles, oncologist who was part of theteam that developed Herceptin back in the1980s, is enthusiastic about combining it withGenentech’s vascular endothelial growth factor(VEGF) inhibitor, Avastin (bevacizumab).Slamon points out that the two pathways arelinked. When HER2 is amplified, “one of thepathways that consistently goes up is VEGF,”he says. Trials of the combination (Avastin plusHerceptin) have been encouraging. In phase2 trials, “the two antibodies alone, with nochemo, are giving objective response rates in54% of women with metastatic disease.” Usedat earlier stages, Slamon believes the combinationcould be even more powerful and he isoptimistic that this regimen will eventually betested in a phase 3 trial without concomitantchemotherapy.Growing understanding of the pathwaysrelating to HER2 are also leading to new drugtargets. Phosphatidyl inositol 3-phosphate(PI3) kinase and PTEN (phosphatase andtensin homolog) are two other players thatseem connected to HER2. Mutations in PI3kinase occur in 30% of breast cancers andcause the enzyme to be turned on all the time.“It’s a classic oncogenic activating mutation,”says William Sellers, head of oncology researchat Novartis Institutes for Biomedical Researchin Cambridge, Massachusetts. PTEN, meanwhile,is a tumor suppressor gene which canact by blocking the activation of PI3 kinase.Mutations in that gene can again lead to overactivation.“In many instances, the amplificationof HER2 leads to signaling through thispathway,” Sellers says. This has become thenumber one pathway of interest in cancer.The most advanced new compounds targetingthe pathway are mTOR inhibitors, but thesework far downstream, and researchers wouldlike to hit it earlier on. Novartis’ BKM120 is aselective PI3 kinase inhibitor that the companyhopes will do just that. All these targets, includingHER2, are found in other cancers, whichmeans they could have wider use. Herceptin isbeing tested in stomach cancer, for example. Ifthese drugs are used more broadly, new testswill be needed. The question then, Sellers says,will be, “How do we know which therapeuticto use?”Improving outcomesControversy about testing has doggedHerceptin from the beginning. “Slamon battledfor ten years to prove HER2 was important,”recalls Shak, who worked on Herceptin’sdevelopment while at Genentech. “He had tofight that hard because so many groups weredoing their tests without quality control.” Butexperts are adamant that testing for HER2must be improved. “In the adjuvant setting,you are giving a woman absolutely substandardcare if you are wrongly denying her thedrug,” says Ross. Norton concurs: “We mustdo better.”Although standardizing immunohistochemistryseems to be the most obvious next step,it may not necessarily be the best way toimprove outcomes. “Even when countrieswith a national health service do everythingthey can to standardize this test, we still seeunacceptable margins of error,” says Liebman.Strategic Medicine is working with The MayoClinic and Thompson Reuters, headquarteredin New York, to build data models that willreveal which steps are most likely to improvethe quality of HER2 testing. Most laboratoriesare using immunohistochemistry, andthe cost of making improvements across theentire community, he points out, would likelybe prohibitive. “Our goal is to find the weakestpoints in the system, whether it is an issuewith reimbursement, diagnostic developmentor education. What should be the priority fixthat gets us the biggest impact in improvingpatient care?”Others think the answer clearly lies inapplying some newer technologies. “I thinksequencing will give us the final answer, oncewe have inexpensive-enough techniques,” saysNorton.Malorye Allison, Acton, Massachusetts1. Phillips, K.A. et al. Cancer 115, 5166–5174 (2009).2. McArthur, H.L. & Hudis, C. Clin. Cancer Res. 15,6311–6313 (2009).3. Perez, E.A. et al. J. Clin. Oncol. 25, 512, Suppl. 18S(2007).4. McArthur, H.L. et al., abstract 1005, presented atEuropean CanCer Organization 15 and 34th EuropeanSociety for Medical Oncology MultidisciplinaryCongress, Berlin, Sept. 20–24, 2009.nature biotechnology volume 28 number 2 february 2010 119
- Page 3 and 4: volume 28 number 2 february 2010COM
- Page 5 and 6: in this issue© 2010 Nature America
- Page 7 and 8: © 2010 Nature America, Inc. All ri
- Page 10 and 11: NEWS© 2010 Nature America, Inc. Al
- Page 12 and 13: NEWS© 2010 Nature America, Inc. Al
- Page 14 and 15: NEWS© 2010 Nature America, Inc. Al
- Page 16 and 17: © 2010 Nature America, Inc. All ri
- Page 18 and 19: © 2010 Nature America, Inc. All ri
- Page 20 and 21: © 2010 Nature America, Inc. All ri
- Page 24 and 25: uilding a businessComing to termsDa
- Page 26 and 27: uilding a business© 2010 Nature Am
- Page 28 and 29: correspondence© 2010 Nature Americ
- Page 30 and 31: correspondence© 2010 Nature Americ
- Page 32 and 33: correspondence© 2010 Nature Americ
- Page 34 and 35: correspondence© 2010 Nature Americ
- Page 36 and 37: case studyNever againcommentaryChri
- Page 38 and 39: COMMENTARY© 2010 Nature America, I
- Page 40 and 41: COMMENTARY© 2010 Nature America, I
- Page 42 and 43: patents© 2010 Nature America, Inc.
- Page 44 and 45: patents© 2010 Nature America, Inc.
- Page 46 and 47: news and viewsChIPs and regulatory
- Page 48 and 49: news and viewsFrom genomics to crop
- Page 50 and 51: news and views© 2010 Nature Americ
- Page 52 and 53: news and views© 2010 Nature Americ
- Page 54 and 55: e s o u r c eRational association o
- Page 56 and 57: e s o u r c e© 2010 Nature America
- Page 58 and 59: e s o u r c e© 2010 Nature America
- Page 60 and 61: e s o u r c e© 2010 Nature America
- Page 62 and 63: © 2010 Nature America, Inc. All ri
- Page 64 and 65: B r i e f c o m m u n i c at i o n
- Page 66 and 67: i e f c o m m u n i c at i o n sAUT
- Page 68 and 69: lettersa1.5 kb hVPrIntron 112.5 kbA
- Page 70 and 71: letters© 2010 Nature America, Inc.
- Page 72 and 73:
letters© 2010 Nature America, Inc.
- Page 74 and 75:
l e t t e r sReal-time imaging of h
- Page 76 and 77:
l e t t e r sFigure 2 Time-lapse li
- Page 78 and 79:
l e t t e r s© 2010 Nature America
- Page 80 and 81:
l e t t e r sRational design of cat
- Page 82 and 83:
l e t t e r s© 2010 Nature America
- Page 84 and 85:
l e t t e r s© 2010 Nature America
- Page 86 and 87:
sample fluorescence was measured as
- Page 88 and 89:
careers and recruitmentFourth quart