Volume 8 Issue 3 - Australasian Society for Ultrasound in Medicine
Volume 8 Issue 3 - Australasian Society for Ultrasound in Medicine
Volume 8 Issue 3 - Australasian Society for Ultrasound in Medicine
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
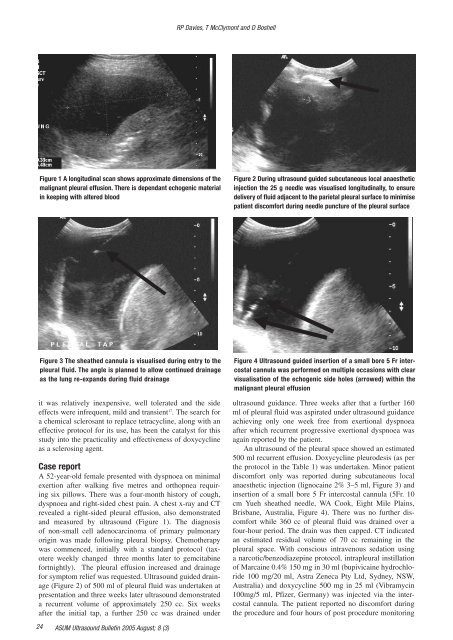
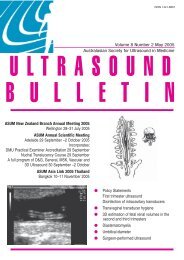
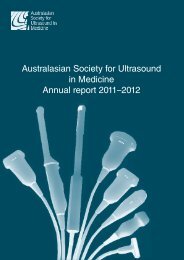
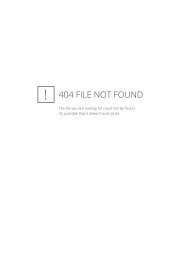
RP Davies, T McClymont and D BoshellFigure 1 A longitud<strong>in</strong>al scan shows approximate dimensions of themalignant pleural effusion. There is dependant echogenic material<strong>in</strong> keep<strong>in</strong>g with altered bloodFigure 2 Dur<strong>in</strong>g ultrasound guided subcutaneous local anaesthetic<strong>in</strong>jection the 25 g needle was visualised longitud<strong>in</strong>ally, to ensuredelivery of fluid adjacent to the parietal pleural surface to m<strong>in</strong>imisepatient discom<strong>for</strong>t dur<strong>in</strong>g needle puncture of the pleural surfaceFigure 3 The sheathed cannula is visualised dur<strong>in</strong>g entry to thepleural fluid. The angle is planned to allow cont<strong>in</strong>ued dra<strong>in</strong>ageas the lung re-expands dur<strong>in</strong>g fluid dra<strong>in</strong>ageit was relatively <strong>in</strong>expensive, well tolerated and the sideeffects were <strong>in</strong>frequent, mild and transient 17 . The search <strong>for</strong>a chemical sclerosant to replace tetracycl<strong>in</strong>e, along with aneffective protocol <strong>for</strong> its use, has been the catalyst <strong>for</strong> thisstudy <strong>in</strong>to the practicality and effectiveness of doxycycl<strong>in</strong>eas a scleros<strong>in</strong>g agent.Case reportA 52-year-old female presented with dyspnoea on m<strong>in</strong>imalexertion after walk<strong>in</strong>g five metres and orthopnea requir<strong>in</strong>gsix pillows. There was a four-month history of cough,dyspnoea and right-sided chest pa<strong>in</strong>. A chest x-ray and CTrevealed a right-sided pleural effusion, also demonstratedand measured by ultrasound (Figure 1). The diagnosisof non-small cell adenocarc<strong>in</strong>oma of primary pulmonaryorig<strong>in</strong> was made follow<strong>in</strong>g pleural biopsy. Chemotherapywas commenced, <strong>in</strong>itially with a standard protocol (taxotereweekly changed three months later to gemcitab<strong>in</strong>e<strong>for</strong>tnightly). The pleural effusion <strong>in</strong>creased and dra<strong>in</strong>age<strong>for</strong> symptom relief was requested. <strong>Ultrasound</strong> guided dra<strong>in</strong>age(Figure 2) of 500 ml of pleural fluid was undertaken atpresentation and three weeks later ultrasound demonstrateda recurrent volume of approximately 250 cc. Six weeksafter the <strong>in</strong>itial tap, a further 250 cc was dra<strong>in</strong>ed underFigure 4 <strong>Ultrasound</strong> guided <strong>in</strong>sertion of a small bore 5 Fr <strong>in</strong>tercostalcannula was per<strong>for</strong>med on multiple occasions with clearvisualisation of the echogenic side holes (arrowed) with<strong>in</strong> themalignant pleural effusionultrasound guidance. Three weeks after that a further 160ml of pleural fluid was aspirated under ultrasound guidanceachiev<strong>in</strong>g only one week free from exertional dyspnoeaafter which recurrent progressive exertional dyspnoea wasaga<strong>in</strong> reported by the patient.An ultrasound of the pleural space showed an estimated500 ml recurrent effusion. Doxycycl<strong>in</strong>e pleurodesis (as perthe protocol <strong>in</strong> the Table 1) was undertaken. M<strong>in</strong>or patientdiscom<strong>for</strong>t only was reported dur<strong>in</strong>g subcutaneous localanaesthetic <strong>in</strong>jection (lignoca<strong>in</strong>e 2% 3–5 ml, Figure 3) and<strong>in</strong>sertion of a small bore 5 Fr <strong>in</strong>tercostal cannula (5Fr. 10cm Yueh sheathed needle, WA Cook, Eight Mile Pla<strong>in</strong>s,Brisbane, Australia, Figure 4). There was no further discom<strong>for</strong>twhile 360 cc of pleural fluid was dra<strong>in</strong>ed over afour-hour period. The dra<strong>in</strong> was then capped. CT <strong>in</strong>dicatedan estimated residual volume of 70 cc rema<strong>in</strong><strong>in</strong>g <strong>in</strong> thepleural space. With conscious <strong>in</strong>travenous sedation us<strong>in</strong>ga narcotic/benzodiazep<strong>in</strong>e protocol, <strong>in</strong>trapleural <strong>in</strong>stillationof Marca<strong>in</strong>e 0.4% 150 mg <strong>in</strong> 30 ml (bupivica<strong>in</strong>e hydrochloride100 mg/20 ml, Astra Zeneca Pty Ltd, Sydney, NSW,Australia) and doxycycl<strong>in</strong>e 500 mg <strong>in</strong> 25 ml (Vibramyc<strong>in</strong>100mg/5 ml, Pfizer, Germany) was <strong>in</strong>jected via the <strong>in</strong>tercostalcannula. The patient reported no discom<strong>for</strong>t dur<strong>in</strong>gthe procedure and four hours of post procedure monitor<strong>in</strong>g24 ASUM <strong>Ultrasound</strong> Bullet<strong>in</strong> 2005 August; 8 (3)