Sustaining Generic Medicines Markets in Europe
Sustaining Generic Medicines Markets in Europe
Sustaining Generic Medicines Markets in Europe
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es marketsiiThe authorsResearch Centre for Pharmaceutical Care and Pharmaco-economicsS<strong>in</strong>ce the early 1990s, the Research Centre for Pharmaceutical Care and Pharmaco-economicsat the Katholieke Universiteit Leuven has made a scientific contribution to the efficient, effectiveand safe use of medic<strong>in</strong>es, medical devices and related products. In addition to research <strong>in</strong>tothe key areas of pharmaco-economics, pharmaco-therapeutics and pharmaceutical care, theCentre is committed to transferr<strong>in</strong>g scientific knowledge <strong>in</strong> these areas to health careprofessionals, policy makers, pharmaceutical <strong>in</strong>dustry, and patients.Steven SimoensSteven is a Professor at the Research Centre for Pharmaceutical Care and Pharmacoeconomics.He is a health economist and leads the Centre’s research <strong>in</strong>to the economics ofmedic<strong>in</strong>es, medical devices and related products. His research <strong>in</strong>terests focus on issuessurround<strong>in</strong>g competition and regulation of the pharmaceutical <strong>in</strong>dustry, and economicevaluation of medic<strong>in</strong>es and medical devices. Previously, Steven worked at the Organization forEconomic Co-operation and Development and at the University of Aberdeen. He holds a degree<strong>in</strong> commercial eng<strong>in</strong>eer<strong>in</strong>g from the Katholieke Universiteit Leuven, a MSc <strong>in</strong> Health Economicsfrom the University of York and a PhD <strong>in</strong> Economics from the University of Aberdeen.Sandra De CosterSandra graduated from the Katholieke Universiteit Leuven as a pharmacist. She spent twoyears <strong>in</strong> the pharmaceutical <strong>in</strong>dustry, where she participated <strong>in</strong> the regulatory affairs of herbalmedic<strong>in</strong>es. She then jo<strong>in</strong>ed the Research Centre for Pharmaceutical Care and Pharmacoeconomicsas a research fellow. Her research <strong>in</strong>terests focus on pharmacotherapy. In additionto this, she works part-time as a community pharmacist.
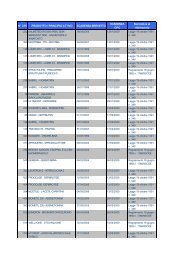
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es marketsviiiFigure 25. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> Italy, 2004 87Figure 26. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> the Netherlands,200488Figure 27. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> Poland, 2004 88Figure 28. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> Portugal, 2004 89Figure 29. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> Spa<strong>in</strong>, 2004 89Figure 30. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> United K<strong>in</strong>gdom,200490
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 11Demand-side policiesPhysician budgets created a stimulus to prescribe generic medic<strong>in</strong>es <strong>in</strong> Germany and the UnitedK<strong>in</strong>gdom, but rewards and sanctions for budget surpluses and deficits, respectively, are anecessary condition for mak<strong>in</strong>g budgets effective. Initiatives to promote INN prescrib<strong>in</strong>g provideimpetus for generic medic<strong>in</strong>es use only if regulation specify<strong>in</strong>g which medic<strong>in</strong>e pharmacists needto dispense and the system of pharmacist remuneration favour the delivery of generic medic<strong>in</strong>es.<strong>Generic</strong> substitution aids generic medic<strong>in</strong>es use if it is f<strong>in</strong>ancially attractive to pharmacists tosubstitute generic for orig<strong>in</strong>ator medic<strong>in</strong>es. However, the remuneration system of pharmacists <strong>in</strong>the majority of selected countries provides a f<strong>in</strong>ancial dis<strong>in</strong>centive to dispense generic medic<strong>in</strong>es.Belgian and French remuneration systems that guarantee the same absolute marg<strong>in</strong> on orig<strong>in</strong>atorand generic medic<strong>in</strong>es provide a neutral f<strong>in</strong>ancial <strong>in</strong>centive to pharmacists, but <strong>in</strong>crease the priceof generic medic<strong>in</strong>es relative to orig<strong>in</strong>ator medic<strong>in</strong>es. Few countries have <strong>in</strong> place systems thatf<strong>in</strong>ancially reward pharmacists for substitut<strong>in</strong>g generic for orig<strong>in</strong>ator medic<strong>in</strong>es. In countries wherecompanies compete by offer<strong>in</strong>g discounts to pharmacists, health care payers and patients do notcapture the potential sav<strong>in</strong>gs from generic medic<strong>in</strong>es use.Patient co-payment seems to play a role <strong>in</strong> stimulat<strong>in</strong>g demand for generic medic<strong>in</strong>es <strong>in</strong> Polandand Portugal. This <strong>in</strong>centive does not exist <strong>in</strong> France where co-payments tend to be covered byprivate <strong>in</strong>surance. Many countries have launched advertis<strong>in</strong>g campaigns to <strong>in</strong>form patients ofgeneric medic<strong>in</strong>es, but the effectiveness of such campaigns has not been evaluated.Sav<strong>in</strong>gs from generic medic<strong>in</strong>es useAn illustrative exercise showed that <strong>in</strong>creased substitution of generic for orig<strong>in</strong>ator medic<strong>in</strong>es canyield substantial sav<strong>in</strong>gs. For the top 10 active substances by expenditure of orig<strong>in</strong>atormedic<strong>in</strong>es, generic substitution would reduce public expenditure on the orig<strong>in</strong>ator medic<strong>in</strong>esconta<strong>in</strong><strong>in</strong>g these active substances by 21%-48% <strong>in</strong> selected countries, with a proportionalreduction of 27% <strong>in</strong> Austria, 42% <strong>in</strong> Belgium, 48% <strong>in</strong> Denmark, 35% <strong>in</strong> France, 47% <strong>in</strong> Germany,31% <strong>in</strong> Italy, 41% <strong>in</strong> the Netherlands, 21% <strong>in</strong> Poland, 42% <strong>in</strong> Portugal, 33% <strong>in</strong> Spa<strong>in</strong>, and 33% <strong>in</strong>the United K<strong>in</strong>gdom.Recommendations to susta<strong>in</strong> <strong>Europe</strong>an generic medic<strong>in</strong>es marketsTo susta<strong>in</strong> the development of a competitive generic medic<strong>in</strong>es market, the follow<strong>in</strong>grecommendations are proposed:
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 13Proprietary Name dur<strong>in</strong>g their undergraduate education; by demonstrat<strong>in</strong>g to physicians theamount of sav<strong>in</strong>gs that can be made from generic medic<strong>in</strong>es use; by support<strong>in</strong>g physicianprescrib<strong>in</strong>g with electronic prescrib<strong>in</strong>g systems, medic<strong>in</strong>e databases, audit of and feedback onprescrib<strong>in</strong>g data, prescrib<strong>in</strong>g guidel<strong>in</strong>es and formularies, substitution lists, and local pharmacotherapeuticdiscussions between physicians and pharmacists. These policy tools need to beaccompanied by rewards/sanctions for physicians who do/do not adhere to them, respectively.6. Remove f<strong>in</strong>ancial dis<strong>in</strong>centives for pharmacists to dispense generic medic<strong>in</strong>esPharmacists need to receive a remuneration that does not f<strong>in</strong>ancially penalise them fordispens<strong>in</strong>g generic medic<strong>in</strong>es. Countries need to move away from distribution marg<strong>in</strong>s that areset as a fixed percentage of the public price of medic<strong>in</strong>es or marg<strong>in</strong>s that, even though they areregressive, still favour the delivery of orig<strong>in</strong>ator medic<strong>in</strong>es. Instead, countries need to consider<strong>in</strong>troduc<strong>in</strong>g pharmacist remuneration systems that are neutral or favour the delivery of genericmedic<strong>in</strong>es from a f<strong>in</strong>ancial perspective.7. Provide <strong>in</strong>centives for patients to demand generic medic<strong>in</strong>esCountries need to <strong>in</strong>cite patients to demand generic medic<strong>in</strong>es. This may take the form off<strong>in</strong>ancial <strong>in</strong>centives that reduce co-payment on generic medic<strong>in</strong>es or impose higher co-paymenton orig<strong>in</strong>ator medic<strong>in</strong>es.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 141 IntroductionOver the past decades, medic<strong>in</strong>es have made a major contribution to improv<strong>in</strong>g the health statusof patients. At the same time, pharmaceutical expenditure has <strong>in</strong>creased rapidly, with spend<strong>in</strong>gon medic<strong>in</strong>es outpac<strong>in</strong>g economic growth <strong>in</strong> many <strong>Europe</strong>an countries (OECD, 2005). As aresult, Governments seek to implement effective pharmaceutical policies that support furtherhealth improvements by accommodat<strong>in</strong>g the <strong>in</strong>troduction of new and more effective medic<strong>in</strong>es,whilst conta<strong>in</strong><strong>in</strong>g pharmaceutical expenditure.In the face of these pressures, a grow<strong>in</strong>g number of <strong>Europe</strong>an countries pursue the developmentof their domestic generic medic<strong>in</strong>es market. A generic medic<strong>in</strong>e is a medic<strong>in</strong>al product which hasthe same qualitative and quantitative composition <strong>in</strong> active substances and the samepharmaceutical form as the reference medic<strong>in</strong>al product, and whose bio-equivalence with thereference medic<strong>in</strong>al product has been demonstrated by appropriate bio-availability studies(Directive 2004/27/EC).A favourable environment for generic medic<strong>in</strong>es is likely to aid Governments <strong>in</strong> susta<strong>in</strong><strong>in</strong>g healthcare provision and controll<strong>in</strong>g pharmaceutical expenditure because generic medic<strong>in</strong>es have thesame quality, safety and therapeutic efficacy as the orig<strong>in</strong>ator medic<strong>in</strong>e, but are less expensivethan orig<strong>in</strong>ator medic<strong>in</strong>es. Their lower cost derives from the fact that companies of genericmedic<strong>in</strong>es do not <strong>in</strong>cur the development costs of <strong>in</strong>novative medic<strong>in</strong>es. Competition from genericmedic<strong>in</strong>es also <strong>in</strong>cites orig<strong>in</strong>ator companies to develop <strong>in</strong>novative medic<strong>in</strong>es and to reduce priceson off-patent orig<strong>in</strong>ator medic<strong>in</strong>es, thus generat<strong>in</strong>g additional sav<strong>in</strong>gs to patients (<strong>Europe</strong>anCommission, 2004). Sav<strong>in</strong>gs on the pharmaceutical budget, <strong>in</strong> turn, enable Governments toreimburse newer, more expensive medic<strong>in</strong>es.The size of generic medic<strong>in</strong>es retail markets varies widely between <strong>Europe</strong>an countries. Twogroups of countries can be dist<strong>in</strong>guished <strong>in</strong> terms of the market share of generic medic<strong>in</strong>es byvolume <strong>in</strong> 2004 (IMS Health, 2004). Countries with a mature generic medic<strong>in</strong>es market exhibiteda generic market share exceed<strong>in</strong>g 40% (e.g. Denmark, Germany, Netherlands, Poland, UnitedK<strong>in</strong>gdom). In countries with develop<strong>in</strong>g generic medic<strong>in</strong>es markets, market share of genericmedic<strong>in</strong>es did not surpass 20% (e.g. Austria, Belgium, France, Italy, Portugal, Spa<strong>in</strong>). Variation <strong>in</strong>the development of national generic medic<strong>in</strong>es retail markets owes, amongst other th<strong>in</strong>gs, todifferences <strong>in</strong> the policy and regulatory environment surround<strong>in</strong>g generic medic<strong>in</strong>es.This study aims to analyse the policy environment surround<strong>in</strong>g the generic medic<strong>in</strong>es retailmarket <strong>in</strong> selected <strong>Europe</strong>an countries s<strong>in</strong>ce 1990. A sample of countries with mature generic
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 15medic<strong>in</strong>es markets as well as countries with develop<strong>in</strong>g markets was <strong>in</strong>cluded. Analysis of thepolicy environment focuses on pric<strong>in</strong>g and reimbursement systems, and other <strong>in</strong>centives forphysicians to prescribe, for pharmacists to dispense and for patients to use generic medic<strong>in</strong>es. Inlight of Directive 2004/27/EC which harmonizes data exclusivity provisions and market<strong>in</strong>gauthorisation procedures across EU countries, such issues are not discussed <strong>in</strong> this report,except for when they had a clear impact on the development of a domestic generic medic<strong>in</strong>esmarket over the last 15 years.The material presented <strong>in</strong> this report was derived from a review of the <strong>in</strong>ternational peer-reviewedliterature and relevant legal texts. This was supplemented by <strong>in</strong>formation collected by the 2005and 2006 EGA surveys of pric<strong>in</strong>g and reimbursement systems govern<strong>in</strong>g generic medic<strong>in</strong>esmarkets (EGA, 2005 and 2006). Information derived from these sources was validated byrepresentatives of the EGA Healthcare Economics Committee, national generic medic<strong>in</strong>esassociations, M<strong>in</strong>istries of Health and National <strong>Medic<strong>in</strong>es</strong> Agencies.The study is structured as follows. For each of the selected countries, an overview is presented ofgeneric medic<strong>in</strong>es policy dur<strong>in</strong>g the last 15 years. Incentives created by policy measures areanalysed and key factors aid<strong>in</strong>g and h<strong>in</strong>der<strong>in</strong>g the development of the domestic genericmedic<strong>in</strong>es market are identified. This is followed by a comparative analysis of the policy tools thatcountries have used to strengthen their generic medic<strong>in</strong>es market and of their experience withthem. A set of general and country-specific recommendations is developed that can aid policymakers <strong>in</strong> susta<strong>in</strong><strong>in</strong>g their domestic generic medic<strong>in</strong>es market. F<strong>in</strong>ally, the potential sav<strong>in</strong>gs thatcould be realized from <strong>in</strong>creased substitution of generic for orig<strong>in</strong>ator medic<strong>in</strong>es are illustrated.The analysis is exemplified by data from IMS Health. Differences were noted between the IMSHealth classification of orig<strong>in</strong>ator and generic medic<strong>in</strong>es, and EGA def<strong>in</strong>itions. Therefore, datawere presented only for those countries where a close match could be obta<strong>in</strong>ed between IMSHealth and EGA def<strong>in</strong>itions. Further work is undertaken by IMS Health and EGA to resolverema<strong>in</strong><strong>in</strong>g data issues.The report hopes to aid policy makers <strong>in</strong> ga<strong>in</strong><strong>in</strong>g a better understand<strong>in</strong>g of how pharmaceuticalcompanies, physicians, pharmacists and patients react to <strong>in</strong>centives created by genericmedic<strong>in</strong>es policy, and to propose tools that policy makers can use to cont<strong>in</strong>ue develop<strong>in</strong>gdomestic generic medic<strong>in</strong>es retail markets.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 16PART IGENERIC MEDICINES POLICYIN COUNTRIES WITH MATURE MARKETS
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 172 Denmark2.1 <strong>Generic</strong> medic<strong>in</strong>es marketDanish generic medic<strong>in</strong>es policy has created conditions foster<strong>in</strong>g a low-price, high-volumegeneric medic<strong>in</strong>es market. Market shares of generic medic<strong>in</strong>es <strong>in</strong> terms of value of consumptionhave decreased from 39.3% <strong>in</strong> 1994 to 29.7% <strong>in</strong> 2004 as a result of fall<strong>in</strong>g prices of genericmedic<strong>in</strong>es. This has been accompanied by <strong>in</strong>creased volume of consumption of genericmedic<strong>in</strong>es, with market shares ris<strong>in</strong>g from 61.3% <strong>in</strong> 1994 to 69.7% <strong>in</strong> 2004.Figure 1. Market share of generic medic<strong>in</strong>es by value <strong>in</strong> Denmark, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%39,3%36,2%34,2%32,9%31,8%30,3%30,1%29,3%29,0% 28,3%29,7%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004YearNote: Data relate to both hospital and retail pharmacy.Figure 2. Market share of generic medic<strong>in</strong>es by volume <strong>in</strong> Denmark, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%61,3%58,5%58,1%58,4%58,3%59,0%63,3%59,8%72,8% 69,7%66,0%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004YearNote: Data relate to both hospital and retail pharmacy.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 182.2 <strong>Generic</strong> medic<strong>in</strong>es policy2.2.1 Pric<strong>in</strong>gIn Denmark, pharmaceutical companies are essentially free to set medic<strong>in</strong>e prices. Forreimbursement purposes, generic medic<strong>in</strong>es generally need to be priced below the price level oforig<strong>in</strong>ator medic<strong>in</strong>es.2.2.2 Reference pric<strong>in</strong>gA RPS by active substance was launched <strong>in</strong> 1993. Physicians can exempt patients from the RPSon specific medical grounds. Orig<strong>in</strong>ally, the RP was set at the average price per dosage unit ofthe two lowest-priced medic<strong>in</strong>es <strong>in</strong> the homogeneous group. S<strong>in</strong>ce 2001, the price of thecheapest medic<strong>in</strong>e <strong>in</strong> the group has been used to determ<strong>in</strong>e the RP. The level of RPs tends tochange every two weeks.2.2.3 Incentives for physiciansThe Danish <strong>Medic<strong>in</strong>es</strong> Agency has <strong>in</strong>troduced the ‘Medic<strong>in</strong>e Profile’, a database that GPs andpatients can access to check their <strong>in</strong>dividual medic<strong>in</strong>e use and to compare the price of theprescribed medic<strong>in</strong>e with that of equivalent medic<strong>in</strong>es. The Agency also publishes a monthlynewsletter targeted at physicians giv<strong>in</strong>g them advice on cost-effective prescrib<strong>in</strong>g.Decentralised <strong>in</strong>itiatives exist <strong>in</strong> all counties that stimulate generic prescrib<strong>in</strong>g through the use ofdatabases which report only the cheapest medic<strong>in</strong>e, through medical audit and dissem<strong>in</strong>ation ofprescrib<strong>in</strong>g data, and through visits to GPs to discuss their prescrib<strong>in</strong>g behaviour. These<strong>in</strong>itiatives have contributed to reduc<strong>in</strong>g the proportion of prescriptions where physicians forbidgeneric substitution.The Danish College of General Practice and the Medical Colleges of the various specialties havecompiled practice guidel<strong>in</strong>es, but no <strong>in</strong>centives or sanctions have been attached to physician(lack of) adherence to these guidel<strong>in</strong>es. Physicians are neither legally required nor encouraged toprescribe medic<strong>in</strong>es by INN.2.2.4 Incentives for pharmacistsIn 1991, generic substitution by pharmacists was <strong>in</strong>troduced. If the price of the prescribedmedic<strong>in</strong>e is less than 100 DKK, the pharmacist must substitute with the least expensive (generic
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 19or orig<strong>in</strong>ator) medic<strong>in</strong>e that is at least 5 DKK cheaper than the prescribed medic<strong>in</strong>e. Formedic<strong>in</strong>es priced between 100 and 400 DKK, substitution with the cheapest medic<strong>in</strong>e ismandatory if it is at least 5% cheaper than the prescribed medic<strong>in</strong>e. If the price of the prescribedmedic<strong>in</strong>e exceeds 400 DKK, the pharmacist must dispense the cheapest medic<strong>in</strong>e that is at least20 DKK below the price of the prescribed medic<strong>in</strong>e.Physicians can write on the prescription form that generic substitution is forbidden. In the thirdquarter of 2005, generic substitution was not allowed on 6.1% of prescriptions (Danish <strong>Medic<strong>in</strong>es</strong>Agency, 2006). The responsibility of <strong>in</strong>form<strong>in</strong>g patients of the availability of generic medic<strong>in</strong>es lieswith the pharmacist. Patients have the right to refuse substitution, but <strong>in</strong>cur a higher patient copaymentif they do so.<strong>Generic</strong> substitution is re<strong>in</strong>forced by dispens<strong>in</strong>g budgets for pharmacists, which provide an<strong>in</strong>centive to dispense cheap generic medic<strong>in</strong>es. Pharmacists have no personal f<strong>in</strong>ancial <strong>in</strong>terest<strong>in</strong> dispens<strong>in</strong>g generic medic<strong>in</strong>es as their remuneration is made up of a fee per prescription itemand a percentage marg<strong>in</strong>, the regressive nature of which is limited.2.2.5 Incentives for patientsS<strong>in</strong>ce 2005, patients <strong>in</strong>cur the full costs of medic<strong>in</strong>es up to 520 DKK per year. Once expendituresurpasses that level, patient co-payment as a percentage of medic<strong>in</strong>e costs decreases asexpenditure crosses specific thresholds: 50% co-payment from 520 to 1,260 DKK; 25% from1,260 to 2,950 DKK; and 15% from 2,950 DKK onwards. Reimbursement is calculated on thebasis of the price of the cheapest medic<strong>in</strong>e among the different products with the same activesubstance and effect. No campaigns to raise patient awareness of generic medic<strong>in</strong>es have beenconducted.2.3 Policy analysisThe Danish generic medic<strong>in</strong>es market is a low-price, high-volume market. This is because theRPS and generic substitution by pharmacists create a set of conditions that reward genericmedic<strong>in</strong>es companies that have competitive prices for an active substance with high sales. Formost active substances, the market consists of around ten companies that compete on price. Lowprices also stimulate patient demand for generic medic<strong>in</strong>es. This approach ensures the economicviability of the generic medic<strong>in</strong>es market.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 20Demand for generic medic<strong>in</strong>es is supported by generic substitution by pharmacists. <strong>Generic</strong>substitution rules require pharmacists to dispense the cheapest medic<strong>in</strong>e. Also, genericsubstitution by pharmacists is not <strong>in</strong>hibited by physician opposition. F<strong>in</strong>ancial <strong>in</strong>centives forpharmacists tend to be neutral or <strong>in</strong> favour of dispens<strong>in</strong>g generic medic<strong>in</strong>es. F<strong>in</strong>ally, genericprescrib<strong>in</strong>g is promoted by non-f<strong>in</strong>ancial <strong>in</strong>centives fac<strong>in</strong>g physicians.The Danish generic medic<strong>in</strong>es market is a competitive market where RPs change regularly andsome companies specialise <strong>in</strong> offer<strong>in</strong>g a limited number of generic medic<strong>in</strong>es at the lowest cost.Price competition and low prices could endanger the long-term susta<strong>in</strong>ability of the genericmedic<strong>in</strong>es <strong>in</strong>dustry, particularly those companies that offer a broad range of medic<strong>in</strong>es.Key factors aid<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• The RPS and generic substitution by pharmacists reward generic medic<strong>in</strong>es companies thatset competitive prices for an active substance with high sales• Physicians tend to have a favourable attitude towards generic substitution by pharmacistsand face non-f<strong>in</strong>ancial <strong>in</strong>centives to prescribe generic medic<strong>in</strong>esKey factors h<strong>in</strong>der<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• Strong price competition and low prices could endanger the long-term susta<strong>in</strong>ability of thegeneric medic<strong>in</strong>es <strong>in</strong>dustry
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 213 Germany3.1 <strong>Generic</strong> medic<strong>in</strong>es marketData on the market share of generic medic<strong>in</strong>es are not reported due to <strong>in</strong>compatibility of IMSHealth and EGA def<strong>in</strong>itions of generic medic<strong>in</strong>es.3.2 <strong>Generic</strong> medic<strong>in</strong>es policy3.2.1 Pric<strong>in</strong>gIn Germany, free medic<strong>in</strong>e pric<strong>in</strong>g prevails <strong>in</strong> that ex-factory prices of medic<strong>in</strong>es are set<strong>in</strong>dependently by pharmaceutical companies. Medic<strong>in</strong>e prices <strong>in</strong> Germany tend to be higher thanthose <strong>in</strong> other EU countries (Mrazek, 2002).An illustrative analysis focus<strong>in</strong>g on five active substances revealed that generic medic<strong>in</strong>es <strong>in</strong>Germany were priced at an average level as compared with prices <strong>in</strong> France, Italy, Spa<strong>in</strong> and theUnited K<strong>in</strong>gdom <strong>in</strong> 2005 (Accenture, 2005).3.2.2 Reference pric<strong>in</strong>gA RPS was launched <strong>in</strong> 1989 and gradually <strong>in</strong>troduced <strong>in</strong> the early 1990s. Physicians have thelegal obligation to <strong>in</strong>form patients of the surcharge when prescrib<strong>in</strong>g a medic<strong>in</strong>e priced above theRP. RPs were set for homogeneous groups of medic<strong>in</strong>es, which were def<strong>in</strong>ed at three levels.Level 1, implemented <strong>in</strong> 1989, related to off-patent medic<strong>in</strong>es with the same active substance. Asof 1991, level 2 applied to medic<strong>in</strong>es with pharmacologically and therapeutically comparableactive substances. Level 3 was <strong>in</strong>troduced <strong>in</strong> 1992 and grouped medic<strong>in</strong>es with a comparabletherapeutic effect without restrictions on chemical similarity. Initially, levels 2 and 3 of the RPScovered patented medic<strong>in</strong>es from the moment that the first patent for an active substance <strong>in</strong> thegroup had expired. Subsequently, newly-patented medic<strong>in</strong>es were exempted from the RPS after1996. The RP is calculated as a function of ex-factory prices, medic<strong>in</strong>e dosage and package size,and the number of generic competitors. In 1998, an additional condition was imposed, specify<strong>in</strong>gthat the RP could not surpass the highest price <strong>in</strong> the bottom third of the price range for thehomogeneous group.3.2.3 Incentives for physiciansDur<strong>in</strong>g the 1990s, Germany has experimented with different models of budgets at regional leveland budgets at physician level. In 1993, regional budgets were <strong>in</strong>troduced, the level of which was
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 22determ<strong>in</strong>ed by law from 1993 to 1995 and negotiated between regional sickness funds andphysician associations thereafter. Although legislation called for any deficit on medic<strong>in</strong>e budgetsto be paid by physician associations, such collective sanctions were never executed. Despite an<strong>in</strong>itial drop <strong>in</strong> medic<strong>in</strong>e prescriptions <strong>in</strong> 1993, costs started to rise <strong>in</strong> 1994 and exceeded themedic<strong>in</strong>e budget <strong>in</strong> a number of regions from 1995 onwards (Ess et al., 2003). There is alsosome evidence po<strong>in</strong>t<strong>in</strong>g to physicians <strong>in</strong>creas<strong>in</strong>g the number of referrals and hospital admissionsfollow<strong>in</strong>g the <strong>in</strong>troduction of budgets (Schoffski, 1996; von der Schulenburg, 1997).In the late 1990s, regional budgets met with legal challenges. They were abolished <strong>in</strong> 1998, re<strong>in</strong>troduced<strong>in</strong> 1999 and discont<strong>in</strong>ued aga<strong>in</strong> <strong>in</strong> 2001. From 1998 onwards, <strong>in</strong> practice, regionalbudgets were replaced by physician budgets based on practice-specific prescription targets.Physicians surpass<strong>in</strong>g their <strong>in</strong>dividual target by more than 15% received written notice <strong>in</strong>form<strong>in</strong>gthem to reconsider their prescrib<strong>in</strong>g practices. Physicians exceed<strong>in</strong>g 125% of the medic<strong>in</strong>ebudget were required to refund the difference between the actual budget and 115% of the targetbudget <strong>in</strong> the absence of a justification for the budget deficit. Although this recourse proceduregenerally took years, it was successfully carried out <strong>in</strong> a number of regions (Schreyogg et al.,2004).Physician budgets based on prescription targets were supported by feedback on prescrib<strong>in</strong>gbehaviour. From 2000 onwards, data on regional prescrib<strong>in</strong>g practices were sent to eachphysician. Additionally, physicians received <strong>in</strong>formation about a three-monthly volume ofprescriptions of their specialty group <strong>in</strong> the region and their <strong>in</strong>dividual prescription volume s<strong>in</strong>ce2003. Physicians can also draw on computerised prescrib<strong>in</strong>g to <strong>in</strong>form their prescrib<strong>in</strong>gbehaviour. However, physicians are neither legally required nor stimulated to issue prescriptionsby INN.Both the RPS and physician budgets appear to have boosted the German generic medic<strong>in</strong>esmarket dur<strong>in</strong>g the 1990s: actual generic prescriptions as a percentage of potential genericprescriptions <strong>in</strong>creased from 60% <strong>in</strong> 1992 to 75% <strong>in</strong> 2003 (Busse and Riesberg, 2004). However,no studies have been able to assess the separate effect of RPS and physician budgets ongeneric medic<strong>in</strong>es prescription rates as these policy measures were <strong>in</strong>troduced concomitantly.Additionally, physicians and their patients accept and have confidence <strong>in</strong> generic medic<strong>in</strong>es dueto well-known company brand<strong>in</strong>g of generic medic<strong>in</strong>es.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 233.2.4 Incentives for pharmacistsRules govern<strong>in</strong>g generic substitution by pharmacists have changed over time. Until 2001,physicians had to <strong>in</strong>dicate on the prescription form that they allowed substitution. S<strong>in</strong>ce 2002,pharmacists were required to substitute and dispense lower-cost, equivalent medic<strong>in</strong>es, unlessthe physician forbids it. In the case of a prescription by INN, the pharmacist must dispense one ofthe three cheapest medic<strong>in</strong>es. If the physician issues a prescription for a specific medic<strong>in</strong>ewithout exclud<strong>in</strong>g substitution, the pharmacist must dispense the prescribed medic<strong>in</strong>e or one ofthe three cheapest alternatives provided that they have an identical dosage and package size, an<strong>in</strong>terchangeable pharmaceutical form and same range of <strong>in</strong>dications.From 1980 to 2003, pharmacists were paid by regressive marg<strong>in</strong>s. However, as the regressiveeffect was restricted and the absolute size of the marg<strong>in</strong> still <strong>in</strong>creased with medic<strong>in</strong>e prices, thedelivery of generic medic<strong>in</strong>es was penalised. Marg<strong>in</strong>s of pharmacists were reduced <strong>in</strong> 2002. From2004 onwards, pharmacists are paid a fixed marg<strong>in</strong> of 3% <strong>in</strong> addition to a flat-rate payment of8.10 €. This remuneration system implies that pharmacists f<strong>in</strong>ancially benefit from dispens<strong>in</strong>g anorig<strong>in</strong>ator medic<strong>in</strong>e.3.2.5 Incentives for patientsPatient co-payments are currently set as a percentage of the public price of medic<strong>in</strong>es. NoGovernment <strong>in</strong>itiatives have been undertaken to <strong>in</strong>form patients of generic medic<strong>in</strong>es.3.3 Policy analysisHigh medic<strong>in</strong>e prices assist market entry of generic medic<strong>in</strong>es. Regulation govern<strong>in</strong>g theestablishment of RPs stimulates the German generic medic<strong>in</strong>es market by facilitat<strong>in</strong>g marketentry of generic medic<strong>in</strong>es (higher prices are awarded <strong>in</strong> groups with fewer generic competitors).Furthermore, price competition is stimulated <strong>in</strong> established markets, but not to the extent that itbecomes economically unviable for generic medic<strong>in</strong>es companies to rema<strong>in</strong> on the market.Germany has <strong>in</strong>centives for physicians (physician budgets <strong>in</strong> comb<strong>in</strong>ation with prescriptiontargets and feedback on prescrib<strong>in</strong>g behaviour) that, as they are primarily geared towardsconta<strong>in</strong><strong>in</strong>g costs, promote generic prescrib<strong>in</strong>g by physicians. The experience with regionalbudgets seems to suggest that rewards or sanctions are a necessary condition for mak<strong>in</strong>gbudgets effective. It also <strong>in</strong>dicates that budgets may have un<strong>in</strong>tended side effects. Budgets mayprovide an <strong>in</strong>centive for physicians to refer costly patients to hospital or may encourage the
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 24selection of less risky patients if they do not take <strong>in</strong>to account patient profiles or do not cover acomprehensive range of health care services. Significantly, there is a high rate of confidence andacceptance of generic medic<strong>in</strong>es among both physicians and patients ma<strong>in</strong>ly due to well-knowncompany brand<strong>in</strong>g of generic medic<strong>in</strong>es.Demand for generic medic<strong>in</strong>es is supported by generic substitution by pharmacists. Furthermore,conditions govern<strong>in</strong>g substitution have been losened from physicians hav<strong>in</strong>g to allow substitutionto physicians opposed to substitution hav<strong>in</strong>g to forbid it. The former <strong>in</strong>centive not to substitute hasthereby been removed. However, pharmacists are f<strong>in</strong>ancially penalised for dispens<strong>in</strong>g genericmedic<strong>in</strong>es.Key factors aid<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• Market entry of generic medic<strong>in</strong>es benefits from a RPS that sets higher RPs <strong>in</strong> medic<strong>in</strong>egroups with fewer generic competitors and that stimulates price competition, but still makes itpossible for generic medic<strong>in</strong>es companies to earn profits• Demand for generic medic<strong>in</strong>es is driven by generic substitution by pharmacists and byphysician budgets <strong>in</strong> comb<strong>in</strong>ation with prescription targets and feedback on prescrib<strong>in</strong>gbehaviourKey factors h<strong>in</strong>der<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• Pharmacists are f<strong>in</strong>ancially penalised for dispens<strong>in</strong>g generic medic<strong>in</strong>es
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 254 Netherlands4.1 <strong>Generic</strong> medic<strong>in</strong>es marketThe Dutch generic medic<strong>in</strong>es market has grown rapidly over time, with public expenditure<strong>in</strong>creas<strong>in</strong>g from 185 million € <strong>in</strong> 1994 (market share by value of 8.5%) to 830 million € <strong>in</strong> 2004(market share of 17.7%). The fall <strong>in</strong> market share of generic medic<strong>in</strong>es by value between 2003and 2004 is likely to orig<strong>in</strong>ate from a 2004 policy that substantially reduced prices of genericmedic<strong>in</strong>es. Market share of generic medic<strong>in</strong>es by volume has more than doubled from 19.9% <strong>in</strong>1994 to 44.3% <strong>in</strong> 2004.Figure 3. Market share of generic medic<strong>in</strong>es by value <strong>in</strong> the Netherlands, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%8,5%8,9%8,9%9,8%10,8%12,0%13,5%14,2%17,9%21,9%17,7%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004YearFigure 4. Market share of generic medic<strong>in</strong>es by volume <strong>in</strong> the Netherlands, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%43,1%39,6%44,3%34,7% 35,9%28,9%33,0%25,3% 27,1%19,9% 22,6%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004Year
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 264.2 <strong>Generic</strong> medic<strong>in</strong>es policy4.2.1 Pric<strong>in</strong>gThe Netherlands enforced pric<strong>in</strong>g regulation sett<strong>in</strong>g maximum prices of medic<strong>in</strong>es <strong>in</strong> 1996.Companies that set prices above the maximum level are liable for crim<strong>in</strong>al <strong>in</strong>junction. Themaximum price is based on the average price of both orig<strong>in</strong>ator and generic medic<strong>in</strong>es hav<strong>in</strong>g thesame active substance, strength and dosage form <strong>in</strong> Belgium, France, Germany and the UnitedK<strong>in</strong>gdom. In general, this led to a 15% fall <strong>in</strong> medic<strong>in</strong>e prices (Danzon and Ketcham, 2003).However, the level of medic<strong>in</strong>e prices still tended to be higher <strong>in</strong> the Netherlands as compared toother EU countries <strong>in</strong> the early 2000s (Koopmanschap and Rutten, 2003). Health <strong>in</strong>surancefunds, pharmacists, generic medic<strong>in</strong>es companies, and the Government agreed to reduce pricesof generic medic<strong>in</strong>es by 40% (<strong>in</strong>clud<strong>in</strong>g claw-back) on average <strong>in</strong> 2004. Medic<strong>in</strong>e prices were atthe average level of EU prices <strong>in</strong> 2005.4.2.2 Reference pric<strong>in</strong>gIn 1991, a RPS by therapeutic class was <strong>in</strong>troduced. Irrespective of patent status, medic<strong>in</strong>es witha comparable therapeutic effect were grouped if they had the same mechanism of action, asimilar route of adm<strong>in</strong>istration for treat<strong>in</strong>g the same <strong>in</strong>dication <strong>in</strong> the same age group and acomparable cl<strong>in</strong>ical effect. For each active substance <strong>in</strong> a homogeneous group, the average priceper def<strong>in</strong>ed daily dose of all orig<strong>in</strong>ator and generic medic<strong>in</strong>es with that active substance iscalculated. The RP is then set as the median of the distribution across all active substances <strong>in</strong> thegroup.The 1996 pric<strong>in</strong>g regulation <strong>in</strong>troduced maximum prices for many medic<strong>in</strong>es below the level ofRPs (Danzon and Ketcham, 2003). In 1999, RP levels were recalculated tak<strong>in</strong>g <strong>in</strong>to accountactual prices.4.2.3 Incentives for physiciansS<strong>in</strong>ce 1995, the Dutch Government has stimulated physicians to prescribe by INN. This has beensupported by the <strong>in</strong>troduction of an electronic prescription system, although this system is not yetwidely used.The Netherlands has a tradition of develop<strong>in</strong>g and implement<strong>in</strong>g prescrib<strong>in</strong>g guidel<strong>in</strong>es andtreatment protocols that promote the efficient use of medic<strong>in</strong>es. Local pharmaco-therapeuticdiscussions take place periodically between GPs and community pharmacists to evaluate
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 27medic<strong>in</strong>e prescrib<strong>in</strong>g and dispens<strong>in</strong>g, and formularies have been developed to rationaliseprescrib<strong>in</strong>g practices. Information campaigns have urged physicians to use generic names ratherthan brand names. There are no sanctions for physicians who do not respond to these <strong>in</strong>centives.A recent <strong>in</strong>itiative by one health <strong>in</strong>surance fund is the <strong>in</strong>troduction of a f<strong>in</strong>ancial stimulus for thedoctor if (s)he uses generic medic<strong>in</strong>es more frequently. This <strong>in</strong>itiative has been legally challengedby the orig<strong>in</strong>ator medic<strong>in</strong>e <strong>in</strong>dustry.4.2.4 Incentives for pharmacists<strong>Generic</strong> substitution by pharmacists is allowed if physicians and patients agree with it. Physicianscan <strong>in</strong>dicate on the prescription form that generic substitution is not permitted for medicalreasons. When the physician prescribes a branded orig<strong>in</strong>ator medic<strong>in</strong>e that is out of patent andgeneric substitution is allowed, the pharmacist can dispense any generic medic<strong>in</strong>e withoutreference to the physician. If the prescription is issued by INN, the pharmacist may dispense anyorig<strong>in</strong>ator or generic medic<strong>in</strong>e. Health <strong>in</strong>surance funds have also agreed a target rate of genericsubstitution with pharmacists.Pharmacists receive a fixed dispens<strong>in</strong>g fee per prescription. This implies that the delivery of ageneric or orig<strong>in</strong>ator medic<strong>in</strong>e is neutral from a f<strong>in</strong>ancial perspective. As a consequence, it is <strong>in</strong>the <strong>in</strong>terests of pharmacists to dispense the medic<strong>in</strong>e with the highest profit marg<strong>in</strong>. Two policymeasures were <strong>in</strong>troduced <strong>in</strong> the early 1990s that have a f<strong>in</strong>ancial impact on pharmacistdispens<strong>in</strong>g practices. First, if the pharmacist issues a medic<strong>in</strong>e that is priced below the level ofthe RP, the pharmacist can reta<strong>in</strong> one third of the price difference between the price of themedic<strong>in</strong>e and the RP. Second, pharmacists can keep any discounts awarded by pharmaceuticalcompanies s<strong>in</strong>ce 1991. Pharmacists are thus able to reta<strong>in</strong> 100% of discounts offered bywholesalers, but only 33% of the difference between the medic<strong>in</strong>e price and the RP. This led tocompetition between companies through discounts to pharmacists rather than lower medic<strong>in</strong>eprices. In fact, prices of several generic medic<strong>in</strong>es were raised to the level of the RP (Brouwerand Rutten, 2002). Therefore, s<strong>in</strong>ce 1998, a claw-back system imposed a mandatory reduction <strong>in</strong>pharmacists’ reimbursement of 6.82% of medic<strong>in</strong>e acquisition costs. This claw-back mechanismdoes not <strong>in</strong>tend to fully recover discounts as discounts are seen by the Government as an<strong>in</strong>strument to remunerate pharmacists, obviat<strong>in</strong>g the need to <strong>in</strong>crease the fixed dispens<strong>in</strong>g fee.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 284.2.5 Incentives for patientsIn the Netherlands, patients don’t have a f<strong>in</strong>ancial <strong>in</strong>centive to buy generic medic<strong>in</strong>es becausethere are no patient co-payments, except for the difference between the price of the medic<strong>in</strong>e andthe RP if the patient buys a medic<strong>in</strong>e priced above the level of the RP. A specific policy measuretargets three active substances (omeprazole, pravastat<strong>in</strong> and simvastat<strong>in</strong>). For these activesubstances, reimbursement is granted on the basis of the medic<strong>in</strong>e with the lowest pharmacyacquisition cost plus a pharmacist marg<strong>in</strong>. No campaigns to raise patient awareness of genericmedic<strong>in</strong>es have been run.4.3 Policy analysisThe ma<strong>in</strong> driver of generic medic<strong>in</strong>es use <strong>in</strong> the Netherlands is the f<strong>in</strong>ancial attractiveness ofgeneric substitution to pharmacists. A f<strong>in</strong>ancial <strong>in</strong>centive and discounts awarded bypharmaceutical companies has encouraged pharmacists to dispense generic medic<strong>in</strong>es.However, competition <strong>in</strong> the form of discounts to pharmacists rather than by price implies thathealth <strong>in</strong>surance funds do not fully benefit from the cost-sav<strong>in</strong>g potential of generic medic<strong>in</strong>es. Inresponse to this, a claw-back mechanism was <strong>in</strong>troduced. This type of government <strong>in</strong>tervention isunlikely to be as efficient as a market mechanism where pharmaceutical companies compete onthe basis of prices rather than discounts to pharmacists.Additionally, the Dutch generic medic<strong>in</strong>es market is supported by the lower prices of genericmedic<strong>in</strong>es. The Government has provided a range of f<strong>in</strong>ancial and non-f<strong>in</strong>ancial <strong>in</strong>centives forphysicians to prescribe generic medic<strong>in</strong>es, but adherence to these <strong>in</strong>centives is voluntary. Health<strong>in</strong>surance funds have set generic substitution target rates <strong>in</strong> consultation with pharmacists.Key factors aid<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• The f<strong>in</strong>ancial attractiveness of generic substitution by pharmacists susta<strong>in</strong>s genericmedic<strong>in</strong>es use• The generic medic<strong>in</strong>es market is driven by the lower prices of generic medic<strong>in</strong>es• A range of f<strong>in</strong>ancial and non-f<strong>in</strong>ancial <strong>in</strong>centives for physicians support generic prescrib<strong>in</strong>g• Health <strong>in</strong>surance funds have agreed generic substitution target rates <strong>in</strong> consultation withpharmacistsKey factors h<strong>in</strong>der<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• Patients have few <strong>in</strong>centives to buy generic medic<strong>in</strong>es
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 295 Poland5.1 <strong>Generic</strong> medic<strong>in</strong>es marketPoland has a mature generic medic<strong>in</strong>es market. Irrespective of express<strong>in</strong>g shares by value or byvolume, market shares of generic medic<strong>in</strong>es have fallen <strong>in</strong> the 1990s, but stabilized <strong>in</strong> the early2000s. In 2004, market shares of generic medic<strong>in</strong>es atta<strong>in</strong>ed 60% by value and 85% by volume.Figure 5. Market share of generic medic<strong>in</strong>es by value <strong>in</strong> Poland, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%66,4%66,8%65,7%62,1%58,4%59,2%57,6%57,8%57,6%60,5%56,9%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004YearFigure 6. Market share of generic medic<strong>in</strong>es by volume <strong>in</strong> Poland, 1994-2004Market share of generic medic<strong>in</strong>es100,0%80,0%60,0%90,8%89,6%88,5%86,9%85,0%84,3%83,8%83,8%84,0%84,7%83,9%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004Year
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 305.2 <strong>Generic</strong> medic<strong>in</strong>es policy5.2.1 Intellectual property rightsAs <strong>in</strong> many Central and Eastern <strong>Europe</strong>an countries, prescription of generic medic<strong>in</strong>es iscommon practice due to the limited availability of orig<strong>in</strong>ator medic<strong>in</strong>es <strong>in</strong> ambulatory care prior tothe end of communism <strong>in</strong> 1989 and due to the absence of product patents until the early 1990s.The Polish generic medic<strong>in</strong>es market benefited from regulation impos<strong>in</strong>g a three-year dataexclusivity period until EU accession of Poland. Dur<strong>in</strong>g the data exclusivity period, the applicationfor market<strong>in</strong>g authorisation for a generic medic<strong>in</strong>e cannot refer to the pre-cl<strong>in</strong>ical and cl<strong>in</strong>icaldocumentation of the orig<strong>in</strong>ator medic<strong>in</strong>e. As the Polish data exclusivity period was shorter thanthe 6-10 years of data exclusivity granted <strong>in</strong> the EU at that time, this served to speed up entry ofgeneric medic<strong>in</strong>es <strong>in</strong>to the Polish market.In recent years, there has been a significant <strong>in</strong>crease <strong>in</strong> the market share of imported orig<strong>in</strong>atormedic<strong>in</strong>es (Krumschmidt, 2006). Furthermore, the <strong>in</strong>troduction of Supplementary ProtectionCertificates for all patented medic<strong>in</strong>es registered <strong>in</strong> Poland s<strong>in</strong>ce 2000 can be expected to reducegeneric medic<strong>in</strong>es market shares <strong>in</strong> future years.5.2.2 Pric<strong>in</strong>gPolish medic<strong>in</strong>e prices tend to be lower than those <strong>in</strong> other EU countries (Pharmacos, 2005).Poland operates a price-regulated system for medic<strong>in</strong>es that wish to be entered on thereimbursement list.5.2.3 Reference pric<strong>in</strong>gPoland runs two RPS <strong>in</strong> parallel, one by active substance and the other by pharmacologicalclass. The RP is set below or equal to the price of the cheapest generic medic<strong>in</strong>e.5.2.4 Incentives for physiciansPrescrib<strong>in</strong>g of branded and unbranded generic medic<strong>in</strong>es is common because physicians havelong-term, positive experience with generic medic<strong>in</strong>es and because they are conscious of thelimited ability of patients to meet co-payments. Physicians are not encouraged to prescribe byINN and they are not assisted <strong>in</strong> generic prescrib<strong>in</strong>g.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 315.2.5 Incentives for pharmacists<strong>Generic</strong> substitution by pharmacists is allowed. In the case of the prescription of a brandedgeneric medic<strong>in</strong>e, the pharmacist can dispense any generic medic<strong>in</strong>e. If the physician prescribesby INN, the pharmacist may deliver any orig<strong>in</strong>ator or generic medic<strong>in</strong>e. Pharmacists are requiredto <strong>in</strong>form patients of the availability of cheaper generic medic<strong>in</strong>es and of generic substitution.<strong>Generic</strong> substitution by pharmacists is conditional on physicians not forbidd<strong>in</strong>g substitution.Until the mid-1990s, pharmacists earned a marg<strong>in</strong> of 33% on local medic<strong>in</strong>es and 25% onimported medic<strong>in</strong>es irrespective of whether this concerned orig<strong>in</strong>ator or generic medic<strong>in</strong>es. S<strong>in</strong>ce1995, pharmacist marg<strong>in</strong>s are regressive, but this did not completely remove the f<strong>in</strong>ancial<strong>in</strong>centive to dispense orig<strong>in</strong>ator medic<strong>in</strong>es. Discounts awarded by pharmaceutical companiesencourage pharmacists to dispense generic medic<strong>in</strong>es.5.2.6 Incentives for patientsFour rates of patient co-payment apply depend<strong>in</strong>g on therapeutic class and patientcharacteristics. Patient co-payment consists of a fixed amount per prescription for essentialmedic<strong>in</strong>es (list 1). Supplementary medic<strong>in</strong>es are subject to a patient co-payment of 30% (list 2) or50% (list 3). Other prescription medic<strong>in</strong>es that are not <strong>in</strong>cluded <strong>in</strong> the reimbursement lists as wellas over-the-counter medic<strong>in</strong>es are fully paid for by the patient. Initiatives to <strong>in</strong>form patients ofgeneric medic<strong>in</strong>es have not been undertaken.5.3 Policy analysisThe development of the Polish generic medic<strong>in</strong>es market has benefited from the limitedavailability of orig<strong>in</strong>ator medic<strong>in</strong>es and a short data exclusivity period. Sett<strong>in</strong>g the RP at the priceof the cheapest generic medic<strong>in</strong>e <strong>in</strong> comb<strong>in</strong>ation with the low level of medic<strong>in</strong>e prices <strong>in</strong> Polandwould be expected to keep down profitability of generic medic<strong>in</strong>es. However, the economicviability of the Polish generic medic<strong>in</strong>es market derives from the fact that it is a high-volumemarket as a result of the positive attitude of physicians towards generic medic<strong>in</strong>es and the highlevel of patient co-payments.The absence of <strong>in</strong>centives for physicians to prescribe generic medic<strong>in</strong>es <strong>in</strong>hibits the furtherdevelopment of the market. Pharmacists are f<strong>in</strong>ancially penalised for dispens<strong>in</strong>g genericmedic<strong>in</strong>es, except for discounts awarded by pharmaceutical companies.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 32Key factors aid<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• The economic viability of the generic medic<strong>in</strong>es market orig<strong>in</strong>ates from low prices and highvolume of consumption• Sett<strong>in</strong>g the RP at the level of the cheapest generic medic<strong>in</strong>e has led to low prices of genericmedic<strong>in</strong>es• The high volume of consumption derives from the positive experience of physicians withgeneric medic<strong>in</strong>es and the high level of patient co-paymentsKey factors h<strong>in</strong>der<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• Physicians have no <strong>in</strong>centives to prescribe generic medic<strong>in</strong>es• Pharmacists are f<strong>in</strong>ancially penalised for dispens<strong>in</strong>g generic medic<strong>in</strong>es
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 336 United K<strong>in</strong>gdom6.1 <strong>Generic</strong> medic<strong>in</strong>es marketThe market share of generic medic<strong>in</strong>es has more than doubled over a decade <strong>in</strong> the UnitedK<strong>in</strong>gdom. Public expenditure on generic medic<strong>in</strong>es rose from 655 million € <strong>in</strong> 1994 (market shareby value of 8.6%) to 3,625 million € <strong>in</strong> 2004 (market share of 20.1%).Figure 7. Market share of generic medic<strong>in</strong>es by value <strong>in</strong> the United K<strong>in</strong>gdom, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%20,1%17,0%11,8% 13,8% 11,1%13,3%8,6%8,9% 10,3% 10,4%8,3%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004YearData on generic medic<strong>in</strong>es market share by volume are not reported due to <strong>in</strong>compatibility of IMSHealth and EGA def<strong>in</strong>itions of generic medic<strong>in</strong>es.6.2 <strong>Generic</strong> medic<strong>in</strong>es policy6.2.1 Pric<strong>in</strong>gRegulation of orig<strong>in</strong>ator medic<strong>in</strong>e prices is governed by the Pharmaceutical Price RegulationScheme. This voluntary scheme between the British Pharmaceutical Industry and the Departmentof Health does not control prices directly. Instead, pharmaceutical companies strike an agreementenabl<strong>in</strong>g them to ga<strong>in</strong> a specific return on capital which is set equal to profits from sales to theNHS m<strong>in</strong>us allowable costs. Companies are free to set launch prices of new medic<strong>in</strong>es as long asthey do not systematically exceed the target rate of return on capital. This system has led tomedic<strong>in</strong>e prices <strong>in</strong> the United K<strong>in</strong>gdom be<strong>in</strong>g higher than <strong>in</strong> other EU countries (Burstall, 1997).The Pharmaceutical Price Regulation Scheme does not apply to generic medic<strong>in</strong>es andcompanies are free to set prices of generic medic<strong>in</strong>es. This system led to price competitionbetween generic medic<strong>in</strong>es and fall<strong>in</strong>g prices for those medic<strong>in</strong>es supplied by multiple companies
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 34<strong>in</strong> the late 1990s. For drugs <strong>in</strong> short supply, price <strong>in</strong>creases were observed <strong>in</strong> 1999 (Kay andBa<strong>in</strong>es, 2000). In response to this, the Government <strong>in</strong>troduced a statutory price ceil<strong>in</strong>g for thema<strong>in</strong> generic medic<strong>in</strong>es <strong>in</strong> 2000.A new pric<strong>in</strong>g system for Category M generic medic<strong>in</strong>es came <strong>in</strong>to effect <strong>in</strong> 2005 which allowsfreedom of pric<strong>in</strong>g. It also <strong>in</strong>corporates an additional measure to stimulate price competitionbetween generic medic<strong>in</strong>es by enabl<strong>in</strong>g the Department of Health to <strong>in</strong>tervene <strong>in</strong> the marketplaceif trends <strong>in</strong> medic<strong>in</strong>e expenditure suggest that market mechanisms have failed to create pricecompetition. To date, the Department of Health has not availed itself of this measure.6.2.2 Reference pric<strong>in</strong>gThe United K<strong>in</strong>gdom does not have a RPS.6.2.3 Incentives for physiciansA pr<strong>in</strong>cipal factor <strong>in</strong> stimulat<strong>in</strong>g generic medic<strong>in</strong>es use has been the fact that medical students aretaught to prescribe by INN <strong>in</strong> British medical schools. In 2004, 79% of all prescription items wereprescribed by INN <strong>in</strong> England (Health and Social Care Information Centre, 2005).The United K<strong>in</strong>gdom has used medic<strong>in</strong>e budgets to control pharmaceutical expenditure and to<strong>in</strong>cite generic prescrib<strong>in</strong>g by GPs. Initially, medic<strong>in</strong>e budgets were set at the level of the generalpractice under the fundhold<strong>in</strong>g scheme which ran from 1991 to 1997. Although budgets for GPswho did not become fundholders were <strong>in</strong>dicative only, prescrib<strong>in</strong>g behaviour was controlled bypeer pressure and the threat of sanctions for GPs who overspent. Fundhold<strong>in</strong>g practices held anactual budget not only for medic<strong>in</strong>es, but also for outpatient care, diagnostic test<strong>in</strong>g, electivesurgery and community care. Sav<strong>in</strong>gs on the budget could be re<strong>in</strong>vested <strong>in</strong> patient care or couldbe used to upgrade premises and practice-based facilities. Review<strong>in</strong>g the fundhold<strong>in</strong>gexperience, Gosden and Torgerson (1997) concluded that medic<strong>in</strong>e costs of fundhold<strong>in</strong>gpractices had <strong>in</strong>creased at a lower rate as a consequence of <strong>in</strong>creased generic prescrib<strong>in</strong>g thanthose of non-fundholders. However, as fundhold<strong>in</strong>g practices had different characteristics thannon-fundholders, this effect may have stemmed from selection bias rather than from fundhold<strong>in</strong>g.Budgets have also been set for groups of general practices as for example <strong>in</strong> the case of GP andlocality commission<strong>in</strong>g groups, total purchas<strong>in</strong>g pilots and, more recently, primary care trusts. Areview of the first three years of operation of a sample of primary care trusts showed that manytrusts had set generic prescrib<strong>in</strong>g targets supported by <strong>in</strong>centive schemes, prescrib<strong>in</strong>g guidel<strong>in</strong>es
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 35and formularies, and guidance issued through the National Institute of Cl<strong>in</strong>ical Excellence, theRoyal Colleges and National Service Frameworks (Wilk<strong>in</strong> et al., 1999, 2001 and 2002).<strong>Generic</strong> prescrib<strong>in</strong>g by GPs has been supported by computer programmes such as PRODIGY(PRescrib<strong>in</strong>g ratiOnally with Decision support In General practice studY) which <strong>in</strong>dicates genericalternatives to the GP. Prelim<strong>in</strong>ary f<strong>in</strong>d<strong>in</strong>gs po<strong>in</strong>ted to a 3.2% <strong>in</strong>crease <strong>in</strong> generic prescrib<strong>in</strong>gfollow<strong>in</strong>g the <strong>in</strong>troduction of PRODIGY (Purves, 1996).6.2.4 Incentives for pharmacists<strong>Generic</strong> substitution by pharmacists is not permitted. Pharmacists earn a fixed fee perprescription item for a m<strong>in</strong>ority of medic<strong>in</strong>es and the difference between NHS reimbursement (socalled‘Drug Tariff’) and the purchase price. In the case of an INN prescription, the reimbursementlevel is listed <strong>in</strong> Part VIII of the Drug Tariff and depends on the category <strong>in</strong> which a medic<strong>in</strong>e isplaced. Category A consists of generic medic<strong>in</strong>es that are readily available. The correspond<strong>in</strong>gDrug tariff is calculated as the average price charged by two major wholesalers and threecompanies. Drug Tariff reimbursement levels tend to be well below the price level of orig<strong>in</strong>atormedic<strong>in</strong>es. Therefore, pharmacists generally fill INN prescriptions with generic medic<strong>in</strong>es and<strong>in</strong>crease their <strong>in</strong>come by dispens<strong>in</strong>g generic medic<strong>in</strong>es that offer discounts.In response to this, companies of orig<strong>in</strong>ator medic<strong>in</strong>es compiled a ‘brand equalisation formulary’,a list consist<strong>in</strong>g of orig<strong>in</strong>ator medic<strong>in</strong>es that may be substituted for INN prescriptions. Thisenables companies to sell orig<strong>in</strong>ator medic<strong>in</strong>es at Drug Tariff level that otherwise would have ledto the dispens<strong>in</strong>g of a generic medic<strong>in</strong>e. In addition, pharmacists receive a discount, whichappears to be attractive enough to pharmacists to not dispense a generic medic<strong>in</strong>e.As competition <strong>in</strong> the generic medic<strong>in</strong>es market takes the form of discounts to pharmacists andthe NHS does not fully benefit from the cost-sav<strong>in</strong>g potential of generic medic<strong>in</strong>es, a claw-backsystem was <strong>in</strong>troduced that aims to recover the discounts that pharmacists receive. However, astudy of the United K<strong>in</strong>gdom generic medic<strong>in</strong>es market estimated that a significant portion ofdiscounts is not recouped by the NHS (Senior et al., 2000). To reduce NHS reimbursement, anew category M of generic medic<strong>in</strong>es was added to Part VIII of the Drug Tariff <strong>in</strong> 2005 which<strong>in</strong>cludes some medic<strong>in</strong>es previously <strong>in</strong> Category A. The reimbursement level for Category Mmedic<strong>in</strong>es is set at a volume-weighted, average price charged by pharmaceutical companies netof discounts.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 366.2.5 Incentives for patientsPatient co-payment consists of a fixed fee per prescription item for a m<strong>in</strong>ority of medic<strong>in</strong>es. TheGovernment has attempted to <strong>in</strong>form patients of generic medic<strong>in</strong>es through leaflets.6.3 Policy analysisRegulation govern<strong>in</strong>g profits rather than prices of medic<strong>in</strong>es has led to high medic<strong>in</strong>e prices andstimulated market entry of generic medic<strong>in</strong>es.The economic viability of the generic medic<strong>in</strong>es market derives from low prices and high volumeof generic medic<strong>in</strong>es use. The United K<strong>in</strong>gdom has moved away from a reimbursement systemthat rewarded pharmacists for seek<strong>in</strong>g discounts to a system that determ<strong>in</strong>es reimbursement <strong>in</strong>relation to market prices. This creates the conditions for a competitive generic medic<strong>in</strong>es marketthat has low prices, is transparent, rewards companies that atta<strong>in</strong> efficiency ga<strong>in</strong>s, and enablesthe NHS to capture the cost-sav<strong>in</strong>g potential of generic medic<strong>in</strong>es.The high volume of generic medic<strong>in</strong>es sales orig<strong>in</strong>ates from strong <strong>in</strong>centives for physicians toprescribe generic medic<strong>in</strong>es. INN prescrib<strong>in</strong>g is common practice, even for patented medic<strong>in</strong>es.Budgetary <strong>in</strong>centives at the level of <strong>in</strong>dividual general practices and groups of practices haveencouraged generic prescrib<strong>in</strong>g by GPs. <strong>Generic</strong> prescrib<strong>in</strong>g is further supported by the<strong>in</strong>stallation of software packages <strong>in</strong> general practice. However, demand is <strong>in</strong>hibited by the lack of<strong>in</strong>centives for patients to buy generic medic<strong>in</strong>es.Key factors aid<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• <strong>Generic</strong> medic<strong>in</strong>es companies compete with each other on price, enabl<strong>in</strong>g the NHS tocapture the cost-sav<strong>in</strong>g potential of generic medic<strong>in</strong>es• Medical students are taught to prescribe by INN and INN prescrib<strong>in</strong>g by physicians iscommon practice• <strong>Generic</strong> prescrib<strong>in</strong>g has been stimulated by sett<strong>in</strong>g physician budgets <strong>in</strong> comb<strong>in</strong>ation withgeneric medic<strong>in</strong>es prescrib<strong>in</strong>g targets, <strong>in</strong>centive schemes, and prescrib<strong>in</strong>g guidel<strong>in</strong>esKey factors h<strong>in</strong>der<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• Patients have no <strong>in</strong>centives to buy generic medic<strong>in</strong>es
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 37PART IIGENERIC MEDICINES POLICYIN COUNTRIES WITH DEVELOPING MARKETS
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 387 Austria7.1 <strong>Generic</strong> medic<strong>in</strong>es marketIn the context of a generic medic<strong>in</strong>es policy that consists of some supply-side measures, but nodemand-side measures, the Austrian generic medic<strong>in</strong>es market has developed slowly over theyears. Market share of generic medic<strong>in</strong>es has grown from 5.5% <strong>in</strong> 1994 to 8.8% <strong>in</strong> 2004 <strong>in</strong> termsof value of consumption and from 9.2% <strong>in</strong> 1994 to 15.8% <strong>in</strong> 2004 <strong>in</strong> terms of volume ofconsumption.Figure 8. Market share of generic medic<strong>in</strong>es by value <strong>in</strong> Austria, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%5,5% 5,8% 5,9% 6,1% 5,8% 5,7% 5,8% 6,1% 6,5% 7,6% 8,8%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004YearFigure 9. Market share of generic medic<strong>in</strong>es by volume <strong>in</strong> Austria, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%9,2%9,8%10,2%10,6%10,7%11,0%11,5%12,3%13,1%15,8%14,3%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004Year
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 397.2 <strong>Generic</strong> medic<strong>in</strong>es policy7.2.1 Pric<strong>in</strong>gThe Austrian medic<strong>in</strong>e market is characterised by low prices (Pharmig, 2002). In the 1990s,generic medic<strong>in</strong>es were <strong>in</strong>cluded <strong>in</strong> the social <strong>in</strong>surance fund’s approved list of reimbursedmedic<strong>in</strong>es if they were priced at least 30% lower than the orig<strong>in</strong>ator medic<strong>in</strong>e. This was followedby a demand to reduce the price of the orig<strong>in</strong>ator medic<strong>in</strong>e by 23%. This means that genericmedic<strong>in</strong>es tended to be around 7%-10% cheaper than orig<strong>in</strong>ator medic<strong>in</strong>es.In 2004, a new pharmaceutical pric<strong>in</strong>g policy came <strong>in</strong>to force, with medic<strong>in</strong>e prices based onaverage prices of some EU countries. Furthermore, prices of generic medic<strong>in</strong>es and orig<strong>in</strong>atormedic<strong>in</strong>es that are off-patent were regulated as follows. The first generic medic<strong>in</strong>e is priced 44%<strong>in</strong> 2004, 46% <strong>in</strong> 2005, and 48% from 2006 onwards below the price level of the orig<strong>in</strong>atormedic<strong>in</strong>e. The price of the orig<strong>in</strong>ator medic<strong>in</strong>e needs to decrease by 30% three months afterentry of the first generic medic<strong>in</strong>e. The price of the second generic medic<strong>in</strong>e is 15% below theprice level of the first generic and the third generic medic<strong>in</strong>e is priced 10% below the level of thesecond generic medic<strong>in</strong>e. Additionally, the prices of the orig<strong>in</strong>ator, first and second genericmedic<strong>in</strong>es need to go down to the price level of the third generic medic<strong>in</strong>e not later than threemonths follow<strong>in</strong>g the market entry of the third generic medic<strong>in</strong>e. The fourth and any subsequentgeneric medic<strong>in</strong>e needs to be at least 0.10 € cheaper than the least expensive generic medic<strong>in</strong>e.7.2.2 Reference pric<strong>in</strong>gAustria does not have a RPS.7.2.3 Incentives for physiciansPhysicians who have a contract with a social <strong>in</strong>surance fund need to observe guidel<strong>in</strong>es on thecost-effective prescrib<strong>in</strong>g of medic<strong>in</strong>es. Adherence to guidel<strong>in</strong>es is monitored by social <strong>in</strong>surancefunds by compar<strong>in</strong>g prescription rates among peers. Failure to comply with guidel<strong>in</strong>es may result<strong>in</strong> a reprimand, obligation to refund the social <strong>in</strong>surance fund or loss of contract with the fund.Physician generic prescrib<strong>in</strong>g targets have been successfully implemented <strong>in</strong> Vienna, but havenot been extended to other prov<strong>in</strong>ces. There is no legal obligation or encouragement forphysicians to prescribe by INN. However, the hospital discharge letter po<strong>in</strong>ts out that physicianscan prescribe a generic medic<strong>in</strong>e. Physicians are assisted <strong>in</strong> their prescrib<strong>in</strong>g by computerisedprescrib<strong>in</strong>g and a medic<strong>in</strong>e database.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 407.2.4 Incentives for pharmacists<strong>Generic</strong> substitution by pharmacists is not permitted by law. In practice, the pharmacist cansubstitute a branded orig<strong>in</strong>ator medic<strong>in</strong>e that is out of patent or a branded generic medic<strong>in</strong>e byany generic medic<strong>in</strong>e with reference to the physician.Austria has <strong>in</strong> place a system of regressive pharmacist marg<strong>in</strong>s, with pharmacy marg<strong>in</strong>s formedic<strong>in</strong>es purchased by <strong>in</strong>sured patients rang<strong>in</strong>g from 27% for pharmacy purchase prices lessthan 10 € to 3.8% for prices above 357.08 € from 2004 onwards. However, pharmacists still earna lower marg<strong>in</strong> on generic medic<strong>in</strong>es <strong>in</strong> absolute terms than on orig<strong>in</strong>ator medic<strong>in</strong>es.7.2.5 Incentives for patientsPatients usually have to pay a fixed fee per prescription (4.6 €) for each prescribed medic<strong>in</strong>e<strong>in</strong>cluded <strong>in</strong> the reimbursement list. In some cases, two packs can be prescribed for a s<strong>in</strong>gle fee.For medic<strong>in</strong>es not <strong>in</strong>cluded <strong>in</strong> the reimbursement list, patients have to pay the full price, unlessthe prescription is permitted by a senior consultant of the social <strong>in</strong>surance fund. Exemption fromco-payment is also granted to patients <strong>in</strong> need of social protection and patients whose <strong>in</strong>comedoes not surpass a specific level.7.3 Policy analysisIn the 1990s, pric<strong>in</strong>g regulation has restricted demand for generic medic<strong>in</strong>es by reduc<strong>in</strong>g prices oforig<strong>in</strong>ator medic<strong>in</strong>es, lead<strong>in</strong>g to a small price differential between generic and orig<strong>in</strong>atormedic<strong>in</strong>es. Added to that, low price levels of medic<strong>in</strong>es <strong>in</strong> Austria limited market entry for genericmedic<strong>in</strong>es.The 2004 pharmaceutical pric<strong>in</strong>g policy is designed to conta<strong>in</strong> public pharmaceutical expenditureby reduc<strong>in</strong>g prices of orig<strong>in</strong>ator and generic medic<strong>in</strong>es. Incentives embodied by the pric<strong>in</strong>g policyfor generic medic<strong>in</strong>es are mixed. On the one hand, this policy stimulates market entry of genericmedic<strong>in</strong>es by enforc<strong>in</strong>g a substantial price difference between the orig<strong>in</strong>ator medic<strong>in</strong>e and the firstthree generic medic<strong>in</strong>es for a limited period of time. On the other hand, the policy imposes pricereductions on successive generic medic<strong>in</strong>es enter<strong>in</strong>g the market, thereby reduc<strong>in</strong>g theirprofitability. Furthermore, price differences between orig<strong>in</strong>ator and generic medic<strong>in</strong>es are nonexistentor limited <strong>in</strong> established markets with three or more generic medic<strong>in</strong>es, respectively. Thisis likely to <strong>in</strong>hibit patient demand for generic medic<strong>in</strong>es.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 41The role that several stakeholders can play <strong>in</strong> develop<strong>in</strong>g the Austrian generic medic<strong>in</strong>es markethas been ignored to date. Few <strong>in</strong>centives exist for physicians to prescribe generic medic<strong>in</strong>es.<strong>Generic</strong> substitution by pharmacists is not allowed and pharmacists are f<strong>in</strong>ancially penalised fordispens<strong>in</strong>g generic medic<strong>in</strong>es. There are no <strong>in</strong>centives for patients to demand generic medic<strong>in</strong>es.Key factors h<strong>in</strong>der<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• In the 1990s, the Austrian generic medic<strong>in</strong>es market suffered from the low level of medic<strong>in</strong>eprices, reductions <strong>in</strong> the price level of orig<strong>in</strong>ator medic<strong>in</strong>es, and limited price differencesbetween orig<strong>in</strong>ator and generic medic<strong>in</strong>es• Few <strong>in</strong>centives exist for physicians to prescribe generic medic<strong>in</strong>es• Pharmacists are f<strong>in</strong>ancially penalised for dispens<strong>in</strong>g generic medic<strong>in</strong>esKey factors aid<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• S<strong>in</strong>ce 2004, substantial price differences between orig<strong>in</strong>ator and generic medic<strong>in</strong>es <strong>in</strong>develop<strong>in</strong>g markets stimulate market entry
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 428 Belgium8.1 <strong>Generic</strong> medic<strong>in</strong>es marketBelgium had a small generic medic<strong>in</strong>es market dur<strong>in</strong>g the second half of the 1990s. Itsdevelopment was boosted by the <strong>in</strong>troduction of a generic medic<strong>in</strong>es policy <strong>in</strong> 2001. Publicexpenditure on generic medic<strong>in</strong>es rose from 18 million € <strong>in</strong> 1994 (market share by value of 0.8%)to 213 million € <strong>in</strong> 2004 (market share of 4.8%). Market share of generic medic<strong>in</strong>es by volumenearly quadrupled from 2.2% <strong>in</strong> 1994 to 8.0% <strong>in</strong> 2004.Figure 10. Market share of generic medic<strong>in</strong>es by value <strong>in</strong> Belgium, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%0,8% 0,8% 0,9% 1,0% 1,1% 1,2% 1,3% 2,2%2,6%3,8%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004Year4,8%Figure 11. Market share of generic medic<strong>in</strong>es by volume <strong>in</strong> Belgium, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%5,7% 6,9% 8,0%2,3% 2,6% 2,9% 3,1% 3,1% 3,3% 4,7%2,2%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004Year
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 438.2 <strong>Generic</strong> medic<strong>in</strong>es policy8.2.1 Pric<strong>in</strong>g<strong>Generic</strong> medic<strong>in</strong>es need to be priced at or below the level of the RP <strong>in</strong> order to qualify forreimbursement.In 2006, a policy measure reduces turnover of pharmaceutical companies by 2%. This reductioncan be accomplished by a 2% price decrease of medic<strong>in</strong>es. Alternatively, companies can chooseto reduce the price of specific medic<strong>in</strong>es by a m<strong>in</strong>imum of 4% <strong>in</strong> order to achieve a total fall <strong>in</strong>turnover of 2%.8.2.2 Reference pric<strong>in</strong>gA RPS by active substance was implemented <strong>in</strong> June 2001. Over time, the Belgian Governmenthas progressively reduced the RP from 84% (until July 2002), 80% (until January 2003) to 74% ofthe price of the orig<strong>in</strong>ator medic<strong>in</strong>e (until July 2005). The current level stands at 70% of the priceof the orig<strong>in</strong>ator medic<strong>in</strong>e. The RPS was associated with an <strong>in</strong>creased market share of genericmedic<strong>in</strong>es (Simoens et al., 2005). The RPS was enlarged <strong>in</strong> 2005 to <strong>in</strong>clude all pharmaceuticalforms and dosages of the same active substance. Additionally, the law offers the possibility to seta RP for a class of medic<strong>in</strong>es with a similar therapeutic <strong>in</strong>dication. If prices of orig<strong>in</strong>ator medic<strong>in</strong>esfall under the 2006 pric<strong>in</strong>g policy, the correspond<strong>in</strong>g RPs decreases as well.8.2.3 Incentives for physiciansPhysicians face some <strong>in</strong>centives that aim to promote generic prescrib<strong>in</strong>g. Prescrib<strong>in</strong>g guidel<strong>in</strong>esexist that provide comparative <strong>in</strong>formation about, amongst other th<strong>in</strong>gs, costs of medic<strong>in</strong>es <strong>in</strong> anumber of therapeutic classes. There are no <strong>in</strong>centives for physicians to prescribe the mostefficient medic<strong>in</strong>e and physicians do not have to adhere to these guidel<strong>in</strong>es.Pharmanet is an <strong>in</strong>formation system that was created <strong>in</strong> 1996 and that collects data onprescriptions for reimbursed medic<strong>in</strong>es <strong>in</strong> ambulatory care. From late 1998 onwards, each<strong>in</strong>dividual GP received periodic updates of his/her <strong>in</strong>dividual medic<strong>in</strong>e prescription profile fromPharmanet. This tool purported to improve prescrib<strong>in</strong>g behaviour through peer pressure.Prescription profiles were discussed and compared <strong>in</strong> local peer review groups, with physicianaccreditation depend<strong>in</strong>g on their participation <strong>in</strong> such groups. Although penalties were attachedfor physicians who do not prescribe appropriately, such penalties have never been imposed <strong>in</strong>practice.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 44In 2005, a regulatory framework govern<strong>in</strong>g INN prescrib<strong>in</strong>g was <strong>in</strong>troduced. This makes itpossible, but not compulsory, for physicians to prescribe by INN.In 2006, quotas for prescrib<strong>in</strong>g low-cost medic<strong>in</strong>es – generic medic<strong>in</strong>es or orig<strong>in</strong>ator medic<strong>in</strong>esthat have reduced their price – are assigned to physicians. Pharmanet data are used to checkwhether physicians comply with quotas. If physicians prescribe expensive medic<strong>in</strong>es<strong>in</strong>appropriately, they are monitored by the M<strong>in</strong>istry of Health for at least six months and receive<strong>in</strong>formation and tra<strong>in</strong><strong>in</strong>g <strong>in</strong> low-cost prescrib<strong>in</strong>g.8.2.4 Incentives for pharmacistsA law permitt<strong>in</strong>g generic substitution by pharmacists conditional on gett<strong>in</strong>g approval from theprescrib<strong>in</strong>g physician and patient was passed <strong>in</strong> 1993. However, as the royal decree necessary toput this legislation <strong>in</strong>to practice has not been passed to date, generic substitution by pharmacistsis not allowed.If the physician prescribes by INN, the pharmacist can dispense an orig<strong>in</strong>ator medic<strong>in</strong>e or anygeneric medic<strong>in</strong>e priced at or below the level of the RP <strong>in</strong> consultation with the patient. If thisoption does not exist, the pharmacist can dispense an orig<strong>in</strong>ator medic<strong>in</strong>e priced above the levelof the RP. Fail<strong>in</strong>g this second option, the pharmacist can deliver an orig<strong>in</strong>ator medic<strong>in</strong>e not<strong>in</strong>cluded <strong>in</strong> the RPS. The choice of medic<strong>in</strong>e by the pharmacist is <strong>in</strong>spired <strong>in</strong> the first <strong>in</strong>stance, bythe therapeutic <strong>in</strong>terests and cont<strong>in</strong>uity of care of the patient; and <strong>in</strong> the second <strong>in</strong>stance, by theprice of the medic<strong>in</strong>e.Pharmacist marg<strong>in</strong>s <strong>in</strong> Belgium are set at a specific percentage of the public price of medic<strong>in</strong>es (amaximum of 31%, with a limit on the absolute amount of 7.44 €). This system did not favourgeneric medic<strong>in</strong>es as pharmacists received less <strong>in</strong> absolute terms when deliver<strong>in</strong>g a genericmedic<strong>in</strong>e. To make sure that pharmacists were not f<strong>in</strong>ancially penalised for deliver<strong>in</strong>g genericmedic<strong>in</strong>es, pharmacists’ profits on generic medic<strong>in</strong>es were set equal to their profits on orig<strong>in</strong>atormedic<strong>in</strong>es <strong>in</strong> absolute terms <strong>in</strong> 2001. The delivery of generic medic<strong>in</strong>es is therefore neutral topharmacists from a f<strong>in</strong>ancial perspective. Even though discounts to pharmacists and othercommercial practices do not violate pharmaceutical legislation, questions rema<strong>in</strong> over the legalityof discount<strong>in</strong>g <strong>in</strong> Belgium.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 458.2.5 Incentives for patientsPatient co-payments range from 0% to 80% of the medic<strong>in</strong>e price depend<strong>in</strong>g on the type ofpatient and medic<strong>in</strong>e. Belgian policy attempts to foster demand for generic medic<strong>in</strong>es by<strong>in</strong>creas<strong>in</strong>g patient co-payment for specific medic<strong>in</strong>e classes. Maximum patient co-payment on arange of not-life-sav<strong>in</strong>g medic<strong>in</strong>es for which the ATC4 class conta<strong>in</strong>s a generic medic<strong>in</strong>e<strong>in</strong>creased at the end of 2005.In 2004, the Government launched an <strong>in</strong>formation campaign to <strong>in</strong>crease patient awareness ofgeneric medic<strong>in</strong>es. However, the campaign was short-lived and had limited exposure, so that itsimpact is likely to have been limited.8.3 Policy analysisAlthough the <strong>in</strong>troduction of the RPS was accompanied by an <strong>in</strong>crease <strong>in</strong> generic market share,regulation govern<strong>in</strong>g the establishment of the RP appears to be guided by a concern to conta<strong>in</strong>pharmaceutical expenditure, ignor<strong>in</strong>g the negative impact of successive reductions <strong>in</strong> the level ofRPs on the economic viability of generic medic<strong>in</strong>es to enter and rema<strong>in</strong> on the market.The 2006 pric<strong>in</strong>g policy may produce a negative pric<strong>in</strong>g spiral where orig<strong>in</strong>al medic<strong>in</strong>es reducetheir prices and correspond<strong>in</strong>g RPs fall as well. As generic medic<strong>in</strong>es need to be priced at orbelow the level of the RP, the prices of generic medic<strong>in</strong>es need to fall as well. Hypothetically,companies could choose a few market segments where they reduce the price of orig<strong>in</strong>atormedic<strong>in</strong>es by a substantial proportion <strong>in</strong> order to atta<strong>in</strong> the 2% reduction <strong>in</strong> turnover. <strong>Generic</strong>medic<strong>in</strong>es, which need to be at least 30% cheaper than the reduced price of the orig<strong>in</strong>atormedic<strong>in</strong>e, could be priced out of the market.Physicians face few <strong>in</strong>centives to prescribe generic medic<strong>in</strong>es and <strong>in</strong>centives tend to be weak.Furthermore, some features of the INN prescrib<strong>in</strong>g policy are likely to restrict its impact onsusta<strong>in</strong><strong>in</strong>g generic medic<strong>in</strong>es use. First, physicians do not tend to be <strong>in</strong> favour of INN prescrib<strong>in</strong>gas this allows pharmacists to decide which medic<strong>in</strong>e to dispense. Second, pharmacists cancont<strong>in</strong>ue to dispense the orig<strong>in</strong>ator medic<strong>in</strong>e if this is considered to be <strong>in</strong> the therapeutic <strong>in</strong>terestsof the patient. Third, the patient needs to agree with a switch from an orig<strong>in</strong>ator to a genericmedic<strong>in</strong>e.Belgian policy makers have removed the f<strong>in</strong>ancial dis<strong>in</strong>centive for pharmacists to dispensegeneric medic<strong>in</strong>es. Dispens<strong>in</strong>g an orig<strong>in</strong>ator or generic medic<strong>in</strong>e is now neutral to pharmacists
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 46from a f<strong>in</strong>ancial perspective. However, generic substitution by pharmacists is not allowed <strong>in</strong>practice. Furthermore, the impact of the guarantee of pharmacists’ absolute marg<strong>in</strong>s on thedevelopment of the generic medic<strong>in</strong>es market needs to be analysed <strong>in</strong> conjunction with the RPS.On the one hand, the reduction <strong>in</strong> RPs over time translates <strong>in</strong>to decreased public prices ofgeneric medic<strong>in</strong>es. On the other hand, pharmacist marg<strong>in</strong>s on generic medic<strong>in</strong>es are guaranteed<strong>in</strong> absolute terms. This puts pressure on pharmaceutical companies to reduce ex-factory pricelevels and may jeopardise entry and survival of generic medic<strong>in</strong>es.Key factors h<strong>in</strong>der<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• Successive reductions of the RP and the guarantee of absolute pharmacist marg<strong>in</strong>s threatenthe economic viability of the generic medic<strong>in</strong>es market• Physicians have few <strong>in</strong>centives to prescribe generic medic<strong>in</strong>es• There are no <strong>in</strong>centives for pharmacists to dispense generic medic<strong>in</strong>esKey factors aid<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• <strong>Generic</strong> medic<strong>in</strong>es use has been stimulated by the <strong>in</strong>troduction of a RPS
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 479 France9.1 <strong>Generic</strong> medic<strong>in</strong>es marketFrance had an undeveloped generic medic<strong>in</strong>es market dur<strong>in</strong>g the second half of the 1990s. Thischanged with the <strong>in</strong>troduction of <strong>in</strong>centives for physicians and pharmacists <strong>in</strong> the early 2000s.Market share of generic medic<strong>in</strong>es has grown from 0.9% <strong>in</strong> 1994 to 6.6% <strong>in</strong> 2004 <strong>in</strong> terms ofvalue of consumption and from 1.8% <strong>in</strong> 1994 to 10.4% <strong>in</strong> 2004 <strong>in</strong> terms of volume ofconsumption.Figure 12. Market share of generic medic<strong>in</strong>es by value <strong>in</strong> France, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%0,9%2,8% 3,9% 5,3% 6,6%0,8% 0,8% 0,8% 0,9% 1,2% 2,2%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004YearFigure 13. Market share of generic medic<strong>in</strong>es by volume <strong>in</strong> France, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%9,1% 10,4%5,0%6,7%1,8% 1,6% 1,6% 1,6% 1,7% 2,2% 3,9%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004Year
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 489.2 <strong>Generic</strong> medic<strong>in</strong>es policy9.2.1 Intellectual property rightsTo compensate for the delay between the date of fil<strong>in</strong>g the patent application and the date ofmarket<strong>in</strong>g authorisation of the medic<strong>in</strong>e, patent protection could be extended by up to sevenyears. This legislation was <strong>in</strong>troduced <strong>in</strong> France <strong>in</strong> 1990, three years before the implementation ofthe EU Supplementary Protection Certificate for a maximum period of five years <strong>in</strong> 1993. Theconcept of a ‘generic medic<strong>in</strong>e’ has only been def<strong>in</strong>ed as recently as 1997.9.2.2 Pric<strong>in</strong>gMedic<strong>in</strong>e prices <strong>in</strong> France tend to be lower than <strong>in</strong> other EU countries (Le Pen, 2003). <strong>Generic</strong>medic<strong>in</strong>es need to be at least 30% cheaper than the orig<strong>in</strong>ator medic<strong>in</strong>e. In 2005, theGovernment imposed an additional price cut of 10% on exist<strong>in</strong>g generic medic<strong>in</strong>es and the priceof new generic medic<strong>in</strong>es was set at 40% below the price level of the orig<strong>in</strong>ator medic<strong>in</strong>e. Them<strong>in</strong>imum price difference between orig<strong>in</strong>ator and generic medic<strong>in</strong>es <strong>in</strong>creases to 50% <strong>in</strong> 2006.Additionally, prices of off-patent medic<strong>in</strong>es are reduced by 15%-19% <strong>in</strong> 2006.9.2.3 Reference pric<strong>in</strong>gA RPS by active substance was launched for those active substances with generic medic<strong>in</strong>esubstitution rates of less than 45% <strong>in</strong> 2003. The average price of generic medic<strong>in</strong>es determ<strong>in</strong>esthe RP. Follow<strong>in</strong>g the implementation of the RPS, the price of 65% of orig<strong>in</strong>ator medic<strong>in</strong>esdropped to the level of the RP (Peny, 2005). Furthermore, as reference groups are organized byactive substance, re-allocation of demand away from a RPS group to patented medic<strong>in</strong>es with asimilar therapeutic <strong>in</strong>dication seems to have occurred (Le Pen, 2005).9.2.4 Incentives for physiciansIn France, physicians have tended to be reluctant to prescribe generic medic<strong>in</strong>es because theyvalue their prescrib<strong>in</strong>g freedom, are visited by orig<strong>in</strong>ator medic<strong>in</strong>e companies, and are used toprescrib<strong>in</strong>g brand-name medic<strong>in</strong>es (Blachier and Kanavos, 2005).Physicians face some <strong>in</strong>centives to prescribe generic medic<strong>in</strong>es:• Cl<strong>in</strong>ical guidel<strong>in</strong>es have been implemented, but no sanctions have been imposed on noncompliancewith guidel<strong>in</strong>es (Durieux et al., 2000).
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 49• Physicians have been allowed to prescribe by INN s<strong>in</strong>ce 2002. An agreement was struck withphysicians’ unions that raised physician fees for patient visits by 5 € <strong>in</strong> exchange for writ<strong>in</strong>g atleast 25% of prescriptions by INN. No specific penalties for failure to adhere to thisagreement were specified (Le Pen, 2003). INN prescrib<strong>in</strong>g has not been successful to date,with an INN prescription rate of around 7% <strong>in</strong> the year lead<strong>in</strong>g up to May 2005 (MutualitéFrançaise, 2006).• Patients have a f<strong>in</strong>ancial <strong>in</strong>centive to register with a gatekeep<strong>in</strong>g GP who determ<strong>in</strong>es accessto specialist services. As they aim to provide efficient health care services, gatekeep<strong>in</strong>g GPsmay generate sav<strong>in</strong>gs by prescrib<strong>in</strong>g generic medic<strong>in</strong>es.• Physicians are contacted by local authorities with a view to encourag<strong>in</strong>g generic prescrib<strong>in</strong>g.• Physicians are assisted <strong>in</strong> their prescrib<strong>in</strong>g behaviour by a quarterly medic<strong>in</strong>e databasepublished by the Social Security.• Restrictions are placed on the number of visits that orig<strong>in</strong>ator medic<strong>in</strong>e companies can maketo physicians for specific categories of brand-name medic<strong>in</strong>es <strong>in</strong> 2006.9.2.5 Incentives for pharmacistsIn 1999, legislation was approved that allows pharmacists to substitute generic for orig<strong>in</strong>atormedic<strong>in</strong>es, unless the prescrib<strong>in</strong>g physician specifically prohibits substitution. In the case ofsubstitution, the pharmacist is obliged to <strong>in</strong>form the patient who can refuse substitution. When thephysician prescribes a branded orig<strong>in</strong>ator medic<strong>in</strong>e that is out of patent or a branded genericmedic<strong>in</strong>e, the pharmacist can dispense any generic medic<strong>in</strong>e without reference to the physician.If the prescription is issued by INN, the pharmacist may dispense any generic medic<strong>in</strong>e. In 2006,the Government has set an objective of atta<strong>in</strong><strong>in</strong>g a generic substitution rate of 70%.Until 1999, pharmacists were paid by means of a regressive marg<strong>in</strong> on public prices ofmedic<strong>in</strong>es, thereby restrict<strong>in</strong>g the development of the generic medic<strong>in</strong>es market. S<strong>in</strong>ce 1999,pharmacist remuneration consists of a fixed sum of 0.53 € per prescription item and a slid<strong>in</strong>gscale marg<strong>in</strong> (26.1% of the amount of the ex-factory price exclud<strong>in</strong>g VAT below 23 € and 10% ofthe amount above 23 €).
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 50To make the dispens<strong>in</strong>g of generic medic<strong>in</strong>es neutral from a f<strong>in</strong>ancial perspective, pharmacistsare guaranteed the same absolute marg<strong>in</strong> <strong>in</strong> euros on generic and orig<strong>in</strong>ator medic<strong>in</strong>es if a 35%substitution rate between generic and orig<strong>in</strong>ator medic<strong>in</strong>es is atta<strong>in</strong>ed. If this target rate is notachieved, pharmacists’ compensation is supposed to be reduced, although this has neveractually happened.A f<strong>in</strong>ancial <strong>in</strong>centive to dispense generic medic<strong>in</strong>es has been created with pharmacists be<strong>in</strong>gentitled to receive discounts of up to 10.74% of the ex-factory price for generic medic<strong>in</strong>es ascompared with 2.5% for orig<strong>in</strong>ator medic<strong>in</strong>es. In practice, these discount ceil<strong>in</strong>gs were notadhered to. In 2004, estimates of discounts awarded to pharmacists amounted to 45% for genericmedic<strong>in</strong>es and 6% for orig<strong>in</strong>ator medic<strong>in</strong>es (Peny, 2005). Consequently, pharmacists are <strong>in</strong>cluded<strong>in</strong> the Jacob law which regulates discounts awarded <strong>in</strong> the distribution cha<strong>in</strong> to a maximum of20% <strong>in</strong> 2006 and 15% <strong>in</strong> 2007.9.2.6 Incentives for patientsPatient co-payment consists of a fixed amount per prescription and a proportion of the publicprice which varies accord<strong>in</strong>g to the type of medic<strong>in</strong>e. Patient co-payments are generally coveredby an additional private <strong>in</strong>surance taken out by the patient.In 2005, patients suffer<strong>in</strong>g from a chronic illness and who regularly take an orig<strong>in</strong>ator medic<strong>in</strong>ewere contacted by the third-party payer to <strong>in</strong>form them of the existence of a generic equivalent. Ina first <strong>in</strong>stance, patients were sent a personalized letter. If consumption patterns did not change,patients received a telephone call <strong>in</strong> the second <strong>in</strong>stance. This policy measure followsexperiments <strong>in</strong>dicat<strong>in</strong>g that nearly half of patients started us<strong>in</strong>g a generic medic<strong>in</strong>e after they hadbeen contacted (Medical Insurance, 2005).9.3 Policy analysisThe growth of the French generic medic<strong>in</strong>es market has been slowed down by the existence oflegislation regulat<strong>in</strong>g medic<strong>in</strong>e patent extension.The fact that medic<strong>in</strong>e prices <strong>in</strong> France tend to be lower than <strong>in</strong> other EU countries <strong>in</strong> comb<strong>in</strong>ationwith the requirement that generic medic<strong>in</strong>es need to be at least 30% cheaper than the orig<strong>in</strong>atormedic<strong>in</strong>e <strong>in</strong>hibits generic medic<strong>in</strong>e entry. Pressure on generic medic<strong>in</strong>es prices <strong>in</strong>creased as aresult of the <strong>in</strong>troduction of additional price cuts <strong>in</strong> 2005 and 2006.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 51The implementation of the RPS has been accompanied by price reductions of orig<strong>in</strong>atormedic<strong>in</strong>es, thereby remov<strong>in</strong>g the competitive price advantage of generic medic<strong>in</strong>es. Also, there issome evidence of re-allocation of demand towards patented medic<strong>in</strong>es with a similar therapeutic<strong>in</strong>dication.The development of the French generic medic<strong>in</strong>es market has been <strong>in</strong>hibited by the lack of<strong>in</strong>centives fac<strong>in</strong>g physicians and patients to demand generic medic<strong>in</strong>es. Physicians traditionallytend to prescribe brand-name, orig<strong>in</strong>ator medic<strong>in</strong>es and <strong>in</strong>centives to prescribe generic medic<strong>in</strong>esare limited. Patients have no f<strong>in</strong>ancial <strong>in</strong>centive to demand generic medic<strong>in</strong>es as they have to paynoth<strong>in</strong>g or a small percentage of already low-priced medic<strong>in</strong>es.The generic medic<strong>in</strong>es market has been driven by generic substitution which is f<strong>in</strong>anciallyattractive to pharmacists as a result of discounts awarded by generic medic<strong>in</strong>es companies.However, these discounts benefit pharmacists, but not patients. They also <strong>in</strong>hibit thedevelopment of a competitive French generic medic<strong>in</strong>es market where companies compete onthe basis of price. The Jacob law sett<strong>in</strong>g a maximum discount level reduces, but does notelim<strong>in</strong>ate competition on the basis of discounts.Key factors h<strong>in</strong>der<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• In the 1990s, the French generic medic<strong>in</strong>es market was <strong>in</strong>hibited by legislation extend<strong>in</strong>g theperiod of patent protection, low medic<strong>in</strong>e prices, the prescription of brand-name medic<strong>in</strong>es byphysicians, and a f<strong>in</strong>ancial dis<strong>in</strong>centive for pharmacists to dispense generic medic<strong>in</strong>es• <strong>Generic</strong> medic<strong>in</strong>es have tended to lose their price advantage as compared with orig<strong>in</strong>atormedic<strong>in</strong>es as a result of the RPS• Patients have no f<strong>in</strong>ancial <strong>in</strong>centive to buy generic medic<strong>in</strong>esKey factors aid<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• Some policy measures to encourage physicians to prescribe generic medic<strong>in</strong>es have beentaken <strong>in</strong> recent years• Substitution of generic for orig<strong>in</strong>ator medic<strong>in</strong>es is f<strong>in</strong>ancially attractive to pharmacists
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 5210 Italy10.1 <strong>Generic</strong> medic<strong>in</strong>es marketThe Italian generic medic<strong>in</strong>es market tends to be small <strong>in</strong> comparison to the medic<strong>in</strong>e market asa whole. Policy measures to stimulate the generic medic<strong>in</strong>es market <strong>in</strong> the early 2000s appear tohave had little impact on generic medic<strong>in</strong>es market share. Market share of generic medic<strong>in</strong>esgrew from 0.9% <strong>in</strong> 1994 to 2.5% <strong>in</strong> 2004 <strong>in</strong> terms of value of consumption and from 1.4% <strong>in</strong> 1994to 4.5% <strong>in</strong> 2004 <strong>in</strong> terms of volume of consumption.Figure 14. Market share of generic medic<strong>in</strong>es by value <strong>in</strong> Italy, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%0,9% 0,9% 0,8% 0,7% 0,7% 0,7% 0,7% 0,9% 1,7% 2,2% 2,5%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004YearFigure 15. Market share of generic medic<strong>in</strong>es by volume <strong>in</strong> Italy, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%1,4% 1,5% 1,4% 1,2% 1,2% 1,2% 1,2% 1,7% 2,8% 3,8% 4,5%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004Year
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 5310.2 <strong>Generic</strong> medic<strong>in</strong>es policy10.2.1 Intellectual property rightsCopies have thrived <strong>in</strong> Italy (Ghislandi et al., 2005). This orig<strong>in</strong>ates from the historical absence ofpatent protection offered to medic<strong>in</strong>es, with protection be<strong>in</strong>g granted as late as 1978.In addition to patent coverage for a period of 20 years, a Supplementary Certificate of Protectionwas <strong>in</strong>troduced <strong>in</strong> 1991 which can extend patent protection for up to 18 years. The supplementaryterm of protection is calculated as the number of years that have elapsed from the date of fil<strong>in</strong>gthe patent application to the date of the <strong>in</strong>itial market<strong>in</strong>g authorisation. This prolongation of patentcoverage was granted to around 400 active substances (Lucioni, 1995). In the long-term, thesystem of the Supplementary Certificate of Protection will be abolished. From 2003 onwards, thesupplementary term of protection is be<strong>in</strong>g reduced every two years by one year.The term ‘generic medic<strong>in</strong>e’ was first def<strong>in</strong>ed <strong>in</strong> legislation <strong>in</strong> 1996. A generic medic<strong>in</strong>e is to bemarketed under the INN followed by the name of the company. The def<strong>in</strong>ition of ‘genericmedic<strong>in</strong>e’ was extended <strong>in</strong> 2003 to cover all off-patent medic<strong>in</strong>es, <strong>in</strong>clud<strong>in</strong>g copies.10.2.2 Pric<strong>in</strong>g<strong>Generic</strong> medic<strong>in</strong>es need to be at least 20% cheaper than the orig<strong>in</strong>ator medic<strong>in</strong>e if they wish tobe listed <strong>in</strong> the same patient co-payment class as the orig<strong>in</strong>ator medic<strong>in</strong>e.10.2.3 Reference pric<strong>in</strong>gA RPS by active substance was launched <strong>in</strong> 2001. The RP was orig<strong>in</strong>ally calculated as theaverage price, weighted by volume of sales, of equivalent medic<strong>in</strong>es where the price is <strong>in</strong>ferior tothat of the most expensive generic medic<strong>in</strong>e. The RP was reduced at the end of 2001 and is nowset at the level of the price of the cheapest medic<strong>in</strong>e. Case studies perta<strong>in</strong><strong>in</strong>g to three activesubstances revealed that prices of orig<strong>in</strong>ator medic<strong>in</strong>es dropped follow<strong>in</strong>g the implementation ofthe 2001 rules govern<strong>in</strong>g the establishment of RPs (Ghislandi et al., 2005).There is some evidence that the RPS <strong>in</strong>duced pharmaceutical companies to shift demand awayfrom medic<strong>in</strong>es covered by the RPS to medic<strong>in</strong>es not covered by the RPS (so-called ‘reallocationof demand’). The M<strong>in</strong>istry of Health estimated that reallocation of demand wasresponsible for an <strong>in</strong>crease of 3.1% of public pharmaceutical expenditure <strong>in</strong> 2003 (OsMed, 2003).The case of ranitid<strong>in</strong>e shows that the fall<strong>in</strong>g market share of ranitid<strong>in</strong>e follow<strong>in</strong>g the advent of
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 54generic medic<strong>in</strong>es was offset by <strong>in</strong>creas<strong>in</strong>g sales of patented medic<strong>in</strong>es with the sametherapeutic <strong>in</strong>dication (e.g. omeprazole and its derivatives) (Ghislandi et al., 2005).10.2.4 Incentives for physiciansPhysicians face few <strong>in</strong>centives to prescribe generic medic<strong>in</strong>es. They are obliged to <strong>in</strong>formpatients of the existence of generic medic<strong>in</strong>es if the prescription concerns off-patent medic<strong>in</strong>es.The more efficient prescription of medic<strong>in</strong>es by physicians at local level has been stimulated by<strong>in</strong>itiatives that periodically report to GPs on their prescrib<strong>in</strong>g patterns; by local agreements withGPs on pharmaceutical expenditure; and by the implementation of cl<strong>in</strong>ical guidel<strong>in</strong>es.10.2.5 Incentives for pharmacistsFrom 2001 onwards, pharmacists were allowed to substitute the cheapest generic medic<strong>in</strong>e foran orig<strong>in</strong>ator medic<strong>in</strong>e subject to patient agreement and absence of physician prohibition tosubstitute.In Italy, the remuneration of pharmacists consists of a fixed mark-up on the public price(exclud<strong>in</strong>g VAT) of reimbursed medic<strong>in</strong>es. Mandatory discounts on pharmacist marg<strong>in</strong>s formedic<strong>in</strong>es covered by the NHS were <strong>in</strong>itiated <strong>in</strong> 1997, with higher discount rates apply<strong>in</strong>g tohigher price ranges (discounts ranged from 3.75% for prices less than 25.82 € to 19% for pricesgreater than 154.94 € <strong>in</strong> 2003). This system of regressive pharmacist marg<strong>in</strong>s contributed to, butdid not completely succeed <strong>in</strong>, remov<strong>in</strong>g the f<strong>in</strong>ancial dis<strong>in</strong>centive to dispense the cheapergeneric medic<strong>in</strong>es. In 2003, NHS mandatory discounts on pharmacist marg<strong>in</strong>s on genericmedic<strong>in</strong>es priced below or at the level of the RP were abolished. Nevertheless, the regressiveeffect of this system rema<strong>in</strong>s limited. Pharmacists are still f<strong>in</strong>ancially better off by dispens<strong>in</strong>g themore expensive orig<strong>in</strong>ator medic<strong>in</strong>es. They can ga<strong>in</strong> extra discounts from generic medic<strong>in</strong>escompanies, but the legality of this practice is arguable.10.2.6 Incentives for patientsMedic<strong>in</strong>e co-payments and charges were <strong>in</strong>troduced <strong>in</strong> Italy <strong>in</strong> 1978, but abolished <strong>in</strong> 2001. Tocurb the subsequent <strong>in</strong>crease <strong>in</strong> pharmaceutical expenditure, some regions have re-<strong>in</strong>itiatedpatient co-payments <strong>in</strong> 2002. Information campaigns have been run <strong>in</strong> 2001 and 2005 to raisepatient awareness of generic medic<strong>in</strong>es.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 5510.3 Policy analysisThe market<strong>in</strong>g of copies dur<strong>in</strong>g the period covered by the patent has presented an obstacle togeneric medic<strong>in</strong>es entry. Furthermore, the prolongation of patent coverage postponed the onsetof generic competition.Establish<strong>in</strong>g the RP at the level of the price of the cheapest medic<strong>in</strong>e and the absence of<strong>in</strong>centives for physicians and pharmacists to demand generic medic<strong>in</strong>es has led to a low-price,low-volume market. This <strong>in</strong>hibits the economic viability of generic medic<strong>in</strong>es enter<strong>in</strong>g andrema<strong>in</strong><strong>in</strong>g on the market. In the absence of generic medic<strong>in</strong>es, there is no <strong>in</strong>centive for orig<strong>in</strong>atoroff-patent medic<strong>in</strong>es to reduce prices and the RPS has little impact. Furthermore, theimplementation of the RPS seems to have been accompanied by some re-allocation of demandtowards medic<strong>in</strong>es not covered by the RPS.Physicians face few <strong>in</strong>centives to prescribe generic medic<strong>in</strong>es and exist<strong>in</strong>g <strong>in</strong>centives are weak.The impact of <strong>in</strong>itiatives promot<strong>in</strong>g generic medic<strong>in</strong>es use is likely to be limited. Initiatives arevoluntary and there is substantial variation <strong>in</strong> the extent to which local health enterprises haveimplemented them. Moreover, the absence of effective sanctions if physicians fail to adhere tothese <strong>in</strong>itiatives is likely to restrict their effectiveness. There are few <strong>in</strong>centives for pharmacists topromote generic medic<strong>in</strong>es use as generic substitution is voluntary and not <strong>in</strong> the f<strong>in</strong>ancial<strong>in</strong>terests of pharmacists.Key factors h<strong>in</strong>der<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• The existence of a market of copies and the extension of patent coverage posed barriers tothe development of the Italian generic medic<strong>in</strong>es market• Sett<strong>in</strong>g the RP at the level of the cheapest generic medic<strong>in</strong>e <strong>in</strong>hibits generic medic<strong>in</strong>es entry,especially when considered <strong>in</strong> comb<strong>in</strong>ation with the low volume of generic medic<strong>in</strong>esconsumption• Physicians face few <strong>in</strong>centives to prescribe generic medic<strong>in</strong>es• Pharmacists are f<strong>in</strong>ancially penalised for dispens<strong>in</strong>g generic medic<strong>in</strong>es
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 5611 Portugal11.1 <strong>Generic</strong> medic<strong>in</strong>es marketMarket shares of generic medic<strong>in</strong>es did not exceed 1% <strong>in</strong> the second half of the 1990s. The<strong>in</strong>troduction of a generic medic<strong>in</strong>es policy <strong>in</strong> the early 2000s has driven the development of thePortuguese generic medic<strong>in</strong>es market. Public expenditure on generic medic<strong>in</strong>es <strong>in</strong>creased from 6million € <strong>in</strong> 1994 (market share by value of 0.5%) to 253 million € <strong>in</strong> 2004 (market share of 8.6%).Market share of generic medic<strong>in</strong>es by volume rose from 0.8% <strong>in</strong> 1994 to 7.2% <strong>in</strong> 2004.Figure 16. Market share of generic medic<strong>in</strong>es by value <strong>in</strong> Portugal, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%6,7%8,6%0,5% 0,5% 0,5% 0,5% 0,5% 0,5% 0,6% 0,8% 2,5%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004YearFigure 17. Market share of generic medic<strong>in</strong>es by volume <strong>in</strong> Portugal, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%0,8%7,2%2,3% 5,6%0,8% 0,9% 0,8% 0,9% 0,9% 0,9% 1,2%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004Year
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 5711.2 <strong>Generic</strong> medic<strong>in</strong>es policy11.2.1 Intellectual property rightsHistorically, Portugal has a developed market for copies as a result of process patent legislation.Legislation was amended <strong>in</strong> 1995 to regulate product patents for medic<strong>in</strong>es, although companieswere allowed to cont<strong>in</strong>ue market<strong>in</strong>g copies if these were <strong>in</strong>itially authorized prior to 1995. In 2003,a programme was launched to convert copies of off-patent medic<strong>in</strong>es <strong>in</strong>to generic medic<strong>in</strong>es.11.2.2 Pric<strong>in</strong>gS<strong>in</strong>ce 2001, the m<strong>in</strong>imum price difference between generic and orig<strong>in</strong>ator medic<strong>in</strong>es needs to be35% of the price of the orig<strong>in</strong>ator medic<strong>in</strong>e.In 2005, a decree came <strong>in</strong>to effect reduc<strong>in</strong>g prices of all marketed medic<strong>in</strong>es by 6%, with 4.17%of the reduction be<strong>in</strong>g borne by pharmaceutical companies and the rema<strong>in</strong>der by wholesalers andpharmacists.11.2.3 Reference pric<strong>in</strong>gA RPS by active substance was launched <strong>in</strong> 2003. The RP is established at the level of the mostexpensive generic medic<strong>in</strong>e.11.2.4 Incentives for physiciansIn 2002, a law stipulated that physicians need to prescribe medic<strong>in</strong>es for which genericequivalents exist by their INN, even though they are free to add a brand name or a market<strong>in</strong>gauthorisation holder name. Moreover, physicians and pharmacists were forced to <strong>in</strong>form patientsabout the range of available generic medic<strong>in</strong>es and their costs at the time of prescrib<strong>in</strong>g anddispens<strong>in</strong>g a medic<strong>in</strong>e. Although guidel<strong>in</strong>es regard<strong>in</strong>g appropriate prescrib<strong>in</strong>g behaviour wereissued to physicians, compliance with such guidel<strong>in</strong>es is not rewarded or sanctioned. To <strong>in</strong>formgeneric prescrib<strong>in</strong>g by physicians, a medic<strong>in</strong>es database and computerised prescrib<strong>in</strong>g havebeen pilot tested s<strong>in</strong>ce 2004, but have not yet been fully implemented. Physicians can alsoconsult a ‘generic medic<strong>in</strong>es guide’ booklet, published every quarter by INFARMED, the NationalInstitute of Pharmaceuticals and <strong>Medic<strong>in</strong>es</strong>, or on the website of INFARMED.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 5811.2.5 Incentives for pharmacists<strong>Generic</strong> substitution by pharmacists is allowed s<strong>in</strong>ce 2003. The physician can <strong>in</strong>dicate on theprescription form whether (s)he permits or forbids substitution. If the physician prescribes by INN,the pharmacist must dispense the cheapest generic medic<strong>in</strong>e available. If the physician issues aprescription by INN followed by a brand name, the pharmacist may substitute with a genericmedic<strong>in</strong>e if the physician allows substitution. If the physician ticks neither boxpermitt<strong>in</strong>g/forbidd<strong>in</strong>g substitution, substitution with a generic medic<strong>in</strong>e by the pharmacist isallowed.Pharmacists have no f<strong>in</strong>ancial <strong>in</strong>centive to dispense generic medic<strong>in</strong>es as pharmacist marg<strong>in</strong>samount to a flat rate of 19.15% s<strong>in</strong>ce September 2005. Discounts of 3%-5% are offered bygeneric medic<strong>in</strong>es companies to pharmacists.11.2.6 Incentives for patients<strong>Medic<strong>in</strong>es</strong> can fall under five different reimbursement regimes with rates of 100% for medic<strong>in</strong>esclassified as life-sav<strong>in</strong>g products, 95% <strong>in</strong> category A, 70% <strong>in</strong> category B, 40% <strong>in</strong> category C, and20% <strong>in</strong> category D. Patients with low <strong>in</strong>comes receive an additional reimbursement of 15%. In2000, patient demand for generic medic<strong>in</strong>es was stimulated by an <strong>in</strong>crease <strong>in</strong> the reimbursementrate of generic medic<strong>in</strong>es by 10% (until October 2005).Tak<strong>in</strong>g together the impact of the withdrawal of the 10% additional reimbursement for genericmedic<strong>in</strong>es and the price reduction of 6% of all marketed medic<strong>in</strong>es, generic medic<strong>in</strong>es cost 4%more to patients s<strong>in</strong>ce October 2005.The Government has conducted pro-generic-medic<strong>in</strong>e media campaigns, targeted at patients <strong>in</strong>addition to physicians and pharmacists. These media campaigns appear to have contributed torais<strong>in</strong>g demand for generic medic<strong>in</strong>es (INFARMED, 2006), although no formal evaluation of theimpact of campaigns exist.11.3 Policy analysisThe development of the Portuguese generic medic<strong>in</strong>es market has been restra<strong>in</strong>ed by theexistence of a market for copies. Pric<strong>in</strong>g regulation establish<strong>in</strong>g a m<strong>in</strong>imum price differentialbetween generic and orig<strong>in</strong>ator medic<strong>in</strong>es encouraged companies to focus on launch<strong>in</strong>g genericmedic<strong>in</strong>es for more expensive active substances or those with higher market shares. The 2005
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 59price reductions are likely to contribute to conta<strong>in</strong><strong>in</strong>g public pharmaceutical expenditure, butadversely affect the profitability of generic medic<strong>in</strong>es and h<strong>in</strong>der the development of the genericmedic<strong>in</strong>es market.Regulation establish<strong>in</strong>g a m<strong>in</strong>imum price difference between generic and orig<strong>in</strong>ator medic<strong>in</strong>esand sett<strong>in</strong>g the RP at the level of the most expensive generic medic<strong>in</strong>e stimulates genericmedic<strong>in</strong>es companies to concentrate prices around the maximum level that is allowed. It does not<strong>in</strong>cite companies to compete on price and reduce prices below the level of the RP.The Portuguese generic medic<strong>in</strong>es market has been susta<strong>in</strong>ed by <strong>in</strong>cit<strong>in</strong>g physicians to prescribeby INN, by permitt<strong>in</strong>g generic substitution by pharmacists, and by a temporary <strong>in</strong>crease <strong>in</strong>reimbursement of generic medic<strong>in</strong>es. However, physicians face few <strong>in</strong>centives that <strong>in</strong>fluence theirdecision to permit or forbid generic substitution. Furthermore, generic substitution is not <strong>in</strong> thef<strong>in</strong>ancial <strong>in</strong>terests of pharmacists.Key factors h<strong>in</strong>der<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• Regulation requir<strong>in</strong>g that generic medic<strong>in</strong>es are at least 35% cheaper than orig<strong>in</strong>atormedic<strong>in</strong>es and sett<strong>in</strong>g the RP at the level of the most expensive generic medic<strong>in</strong>e stimulatescompanies to launch generic medic<strong>in</strong>es for expensive active substances and limits pricecompetition between generic medic<strong>in</strong>es companies• Physicians face few <strong>in</strong>centives that <strong>in</strong>fluence their decision to permit or forbid genericsubstitution• Pharmacists are f<strong>in</strong>ancially penalised for dispens<strong>in</strong>g generic medic<strong>in</strong>esKey factors aid<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• Portugal developed a successful generic medic<strong>in</strong>es policy by <strong>in</strong>creas<strong>in</strong>g reimbursement ofgeneric medic<strong>in</strong>es (until October 2005), by encourag<strong>in</strong>g physicians to prescribe by INN, andby allow<strong>in</strong>g generic substitution by pharmacists
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 6012 Spa<strong>in</strong>12.1 <strong>Generic</strong> medic<strong>in</strong>es marketMarket shares of generic medic<strong>in</strong>es were small <strong>in</strong> the second half of the 1990s, hover<strong>in</strong>g around1.5% <strong>in</strong> terms of value of consumption and 2% <strong>in</strong> terms of volume of consumption. The 2000 and2003 generic medic<strong>in</strong>e policies appear to have had a limited impact on the development of theSpanish generic medic<strong>in</strong>es market. With respect to value of consumption, market shares ofgeneric medic<strong>in</strong>es grew from 1.7% <strong>in</strong> 1994 to 5.0% <strong>in</strong> 2004. With respect to volume ofconsumption, market shares of generic medic<strong>in</strong>es <strong>in</strong>creased from 2.0% <strong>in</strong> 1994 to 8.1% <strong>in</strong> 2004.Figure 18. Market share of generic medic<strong>in</strong>es by value <strong>in</strong> Spa<strong>in</strong>, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%1,7% 1,5% 1,4% 1,3% 1,4% 1,9% 2,8% 3,6% 4,0% 4,5% 5,0%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004YearFigure 19. Market share of generic medic<strong>in</strong>es by volume <strong>in</strong> Spa<strong>in</strong>, 1994-2004Market share of generic medic<strong>in</strong>es100%80%60%40%20%0%6,1%8,1%2,5% 3,1% 4,0% 4,9%2,0% 1,9% 1,9% 1,9% 2,0%1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004Year
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 6112.2 <strong>Generic</strong> medic<strong>in</strong>es policy12.2.1 Intellectual property rightsThe nature of the Spanish patent system until 1992 has contributed to the success of the marketof copies. This system allows to patent processes to prepare medic<strong>in</strong>es rather than medic<strong>in</strong>esthemselves. In 1992, new legislation was <strong>in</strong>troduced recognis<strong>in</strong>g product patents.In legislation passed <strong>in</strong> 1996, the term ‘generic medic<strong>in</strong>e’ was outl<strong>in</strong>ed and the requisites forregistration of a generic medic<strong>in</strong>e were specified. This legislation clearly dist<strong>in</strong>guished genericmedic<strong>in</strong>es from copies, clear<strong>in</strong>g up previous confusion surround<strong>in</strong>g these concepts (Rovira andAlbarrac<strong>in</strong>, 2001).12.2.2 Pric<strong>in</strong>gIn the 1990s, medic<strong>in</strong>e prices <strong>in</strong> Spa<strong>in</strong> tended to be lower than <strong>in</strong> other countries (Rovira andDarba, 2001). Furthermore, Spa<strong>in</strong> took a number of measures to reduce medic<strong>in</strong>e prices andencourage price competition. The <strong>in</strong>troduction of the 2000 RPS was accompanied by mandatoryprice reductions of copies to the level of the RP <strong>in</strong> 2000 and a 15% decrease <strong>in</strong> the price of activesubstances if their price exceeded the average price of the three cheapest medic<strong>in</strong>es <strong>in</strong> thehomogeneous group by more than 15% <strong>in</strong> 2001. Direct pric<strong>in</strong>g regulation made market<strong>in</strong>gauthorisation of new generic medic<strong>in</strong>es conditional on sett<strong>in</strong>g their price below the level of thelowest-priced medic<strong>in</strong>e <strong>in</strong> the homogeneous group.In 2003, pric<strong>in</strong>g regulation established the price of the first generic medic<strong>in</strong>e at least 30% belowthe price level of the orig<strong>in</strong>ator medic<strong>in</strong>e. Moreover, the price of a generic medic<strong>in</strong>e cannotexceed the RP.12.2.3 Reference pric<strong>in</strong>gA RPS by active substance was implemented <strong>in</strong> 2000, and is annually updated and progressivelyexpanded to cover most off-patent medic<strong>in</strong>es. The RP is calculated with respect to the average,weighted by volume of sales, of the lowest-priced medic<strong>in</strong>es that make up at least 20% of sales.If the difference between this average price and that of the highest-priced medic<strong>in</strong>e <strong>in</strong> the groupdoes not surpass 15%, the RP is set at 90% of the highest price. If the difference exceeds 50%,the RP is established at 50% of the highest price. The RP cannot be <strong>in</strong>ferior to that of the lowestpricedgeneric medic<strong>in</strong>e.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 62The RPS <strong>in</strong>itially applied to a small proportion of the pharmaceutical market: 114 homogeneousgroups conta<strong>in</strong><strong>in</strong>g 590 medic<strong>in</strong>es, account<strong>in</strong>g for 10% of public pharmaceutical expenditure(Antonanzas, 2003). S<strong>in</strong>ce then, the scope of the RPS has been enlarged to cover, for example,200 groups of medic<strong>in</strong>es <strong>in</strong> 2002.In 2003, some features of the RPS were changed. The breadth of homogeneous groups wasenlarged to <strong>in</strong>clude all presentations and pharmaceutical forms (except for retard and paediatricforms) of the same active substance. The RP was calculated as the average of the three lowestcosts per daily def<strong>in</strong>ed dose for each pharmaceutical form of an active substance. In 2004, theaddition of new active substances to the RPS was suspended.12.2.4 Incentives for physiciansThe prescrib<strong>in</strong>g behaviour of physicians is assisted by computerised prescrib<strong>in</strong>g and a medic<strong>in</strong>edatabase. In most Spanish regions, primary care physicians can earn additional annual lumpsums if they meet targets relat<strong>in</strong>g to, for example, generic medic<strong>in</strong>es prescription rates. Theimpact of such measures is likely to be limited as these <strong>in</strong>centive payments make upapproximately 2% of the physician’s gross salary (Antonanzas, 2003). On the other hand,physicians are not obliged or stimulated to prescribe by INN.12.2.5 Incentives for pharmacistsThe implementation of the 2000 RPS was supported by the ability of pharmacists to substitutegeneric for orig<strong>in</strong>ator medic<strong>in</strong>es (unless the patient specifically demands the orig<strong>in</strong>ator medic<strong>in</strong>e).<strong>Generic</strong> substitution by pharmacists encountered physician resistance (Rovira and Albarrac<strong>in</strong>,2001), although no evidence of its effect on substitution rates has been discovered.A new system of regressive pharmacist marg<strong>in</strong>s was <strong>in</strong>troduced <strong>in</strong> 2000. For medic<strong>in</strong>es with anex-factory price at or below 78.34 €, pharmacist marg<strong>in</strong>s were set at 33% for generic medic<strong>in</strong>esas compared with 27.9% for non-generic medic<strong>in</strong>es. For medic<strong>in</strong>es priced above 78.34 €,pharmacist marg<strong>in</strong>s were fixed at 33.54 €. Currently, pharmacists receive a marg<strong>in</strong> of 27.9%,irrespective of whether it concerns an orig<strong>in</strong>ator or generic medic<strong>in</strong>e.In 2003, explicit rules govern<strong>in</strong>g generic substitution by pharmacists were specified. <strong>Generic</strong>substitution of brand-name (orig<strong>in</strong>ator or generic) medic<strong>in</strong>es depends on the price of themedic<strong>in</strong>e. If the medic<strong>in</strong>e price is <strong>in</strong>ferior or equal to the RP, the pharmacist has to dispense thebrand-name medic<strong>in</strong>e. If the medic<strong>in</strong>e price surpasses the RP and the medic<strong>in</strong>e class conta<strong>in</strong>s
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 63generic medic<strong>in</strong>es, the pharmacist is required to dispense the cheapest generic medic<strong>in</strong>e. This, <strong>in</strong>effect, means that medic<strong>in</strong>es priced above the RP are excluded from public reimbursement. If themedic<strong>in</strong>e price is superior to the RP, but generic medic<strong>in</strong>es <strong>in</strong> the class are not available or, be<strong>in</strong>gavailable, are not <strong>in</strong>cluded <strong>in</strong> the list of medic<strong>in</strong>es reimbursed by the NHS, then the pharmacisthas to dispense the brand-name medic<strong>in</strong>e, but at the level of the RP. If the physician prescribesby INN, the pharmacist must dispense the cheapest generic medic<strong>in</strong>e <strong>in</strong> the medic<strong>in</strong>e class or thebrand-name medic<strong>in</strong>e at the RP level <strong>in</strong> the absence of a generic medic<strong>in</strong>e.12.2.6 Incentives for patientsSpa<strong>in</strong> operates a system of patient co-payments for medic<strong>in</strong>es prescribed by NHS physicians,which range from 0% to 40% depend<strong>in</strong>g on the type of patient and medic<strong>in</strong>e. The Governmenthas launched an advertis<strong>in</strong>g campaign to <strong>in</strong>form patients of generic medic<strong>in</strong>es.12.3 Policy analysisThe 2000 generic medic<strong>in</strong>es policy consist<strong>in</strong>g of pric<strong>in</strong>g regulation, a RPS and genericsubstitution by pharmacists did little to boost the Spanish generic medic<strong>in</strong>es market for a numberof reasons. First, pric<strong>in</strong>g regulation <strong>in</strong> comb<strong>in</strong>ation with historically low medic<strong>in</strong>e prices createdless room for generic medic<strong>in</strong>es to enter the market. Second, the impact of the RPS was <strong>in</strong>hibitedby the fact that the RPS <strong>in</strong>itially applied to a small proportion of the pharmaceutical market. Third,the system of pharmacist marg<strong>in</strong>s did not promote generic substitution as the high prices oforig<strong>in</strong>ator medic<strong>in</strong>es compensated for the lower pharmacist marg<strong>in</strong>s on them. Furthermore,<strong>in</strong>creased marg<strong>in</strong>s for generic medic<strong>in</strong>es encouraged pharmacists to dispense the highest-pricedgeneric medic<strong>in</strong>es. The limited price difference between orig<strong>in</strong>ator medic<strong>in</strong>es and the highestpricedgeneric medic<strong>in</strong>es did not provide <strong>in</strong>centives for patients to buy generic medic<strong>in</strong>es. Fourth,<strong>in</strong>centives for pharmacists <strong>in</strong> the form of generic substitution and higher pharmacist marg<strong>in</strong>s forgeneric medic<strong>in</strong>es, <strong>in</strong> comb<strong>in</strong>ation with rules govern<strong>in</strong>g the level of the RP appear to have led toprice competition, not <strong>in</strong> the form of lower medic<strong>in</strong>e prices, but <strong>in</strong> the form of lower acquisitioncosts for pharmacists. The benefits of price competition therefore did not accrue to patients,<strong>in</strong>hibit<strong>in</strong>g demand for generic medic<strong>in</strong>es.The 2003 generic medic<strong>in</strong>es policy conta<strong>in</strong>ed a number of measures exert<strong>in</strong>g pressure on pricesof generic medic<strong>in</strong>es. First, pric<strong>in</strong>g rules established a m<strong>in</strong>imum price difference between genericand orig<strong>in</strong>ator medic<strong>in</strong>es. Second, the RP was set close to the level of marg<strong>in</strong>al costs. Third,regulation govern<strong>in</strong>g generic substitution by pharmacists provided strong <strong>in</strong>centives for orig<strong>in</strong>atormedic<strong>in</strong>es to reduce their prices to the level of the RP, erod<strong>in</strong>g the price advantage of generic
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 64medic<strong>in</strong>es. The generic medic<strong>in</strong>es policy failed to support generic medic<strong>in</strong>es consumption, apartfrom regulation govern<strong>in</strong>g generic substitution by pharmacists, which tends to favour theconsumption of generic medic<strong>in</strong>es. Pharmacists are now f<strong>in</strong>ancially penalised for dispens<strong>in</strong>ggeneric medic<strong>in</strong>es. Few <strong>in</strong>centives for physicians to prescribe generic medic<strong>in</strong>es have beenimplemented. As a result, the Spanish generic medic<strong>in</strong>es market tends to be a low-price, lowvolumemarket, thus h<strong>in</strong>der<strong>in</strong>g the economic viability of generic medic<strong>in</strong>es to enter and rema<strong>in</strong> onthe market.Key factors h<strong>in</strong>der<strong>in</strong>g the development of the generic medic<strong>in</strong>es market:• Historically, the Spanish generic medic<strong>in</strong>es market has been small due to the existence of adeveloped market of copies and low medic<strong>in</strong>e prices• Competition created by the 2000 generic medic<strong>in</strong>es policy benefited pharmacists rather thanpatients, thus <strong>in</strong>hibit<strong>in</strong>g demand for generic medic<strong>in</strong>es• The 2003 generic medic<strong>in</strong>es policy <strong>in</strong>cited companies to reduce prices of orig<strong>in</strong>atormedic<strong>in</strong>es to RPs that are set close to marg<strong>in</strong>al costs, thus limit<strong>in</strong>g the profitability of anddemand for generic medic<strong>in</strong>es• Few <strong>in</strong>centives exist for physicians to prescribe generic medic<strong>in</strong>es• Pharmacists are f<strong>in</strong>ancially penalised for dispens<strong>in</strong>g generic medic<strong>in</strong>es
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 65PART IIICOMPARATIVE ANALYSIS OF GENERIC MEDICINES POLICIES
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 6613 Experience with generic medic<strong>in</strong>es policyThere is no s<strong>in</strong>gle approach towards develop<strong>in</strong>g a generic medic<strong>in</strong>es market. For <strong>in</strong>stance,demand for generic medic<strong>in</strong>es <strong>in</strong> mature markets is driven by generic substitution by pharmacists<strong>in</strong> Denmark and the Netherlands, a favourable attitude of physicians towards generic medic<strong>in</strong>es<strong>in</strong> Poland, physician budgets <strong>in</strong> Germany and the United K<strong>in</strong>gdom. Furthermore, genericmedic<strong>in</strong>es policy has grown <strong>in</strong>crementally <strong>in</strong> countries over time and reflects demographic,cultural, economic and <strong>in</strong>stitutional constra<strong>in</strong>ts. Therefore, there is no reference set of policymeasures that countries can adopt to promote their generic medic<strong>in</strong>es market.Countries that have promoted generic medic<strong>in</strong>es for 10-15 years (e.g. Denmark, Germany, theNetherlands) naturally have a more mature generic medic<strong>in</strong>es market than countries that haveonly recently implemented measures to stimulate generic medic<strong>in</strong>es use (e.g. Austria, Belgium,Portugal). This suggests that the development of a generic medic<strong>in</strong>es market needs to be activelysusta<strong>in</strong>ed by a generic medic<strong>in</strong>es policy.Countries have drawn on supply-side policies relat<strong>in</strong>g to pric<strong>in</strong>g and reimbursement to provideimpetus to the development of the generic medic<strong>in</strong>es market. However, limit<strong>in</strong>g policy to supplysidemeasures only, as is the case <strong>in</strong> Austria, is <strong>in</strong>sufficient to realise the full potential of a genericmedic<strong>in</strong>es market. Therefore, countries tend to complement supply-side policies with demandsidepolicies, creat<strong>in</strong>g <strong>in</strong>centives for physicians to prescribe, pharmacists to dispense, andpatients to demand generic medic<strong>in</strong>es. Demand-side policies are critical to a susta<strong>in</strong>able genericmedic<strong>in</strong>es market.The ability of the generic medic<strong>in</strong>es <strong>in</strong>dustry to deliver competitive prices can only be achievedand susta<strong>in</strong>ed if it is ensured a high volume of the pharmaceutical market. This high volume isdependent on demand-side policies. On the one hand, countries with mature generic medic<strong>in</strong>esmarkets have <strong>in</strong> place <strong>in</strong>centives for physicians, pharmacists and/or patients to demand genericmedic<strong>in</strong>es. On the other hand, there are few <strong>in</strong>centives to stimulate generic medic<strong>in</strong>esconsumption <strong>in</strong> countries with develop<strong>in</strong>g generic medic<strong>in</strong>es markets. In Italy and Spa<strong>in</strong>, thelimited volume of generic medic<strong>in</strong>es consumption <strong>in</strong> comb<strong>in</strong>ation with low medic<strong>in</strong>e prices hasunderm<strong>in</strong>ed the economic viability of the generic medic<strong>in</strong>es market.The rema<strong>in</strong>der of this part of the report contrasts the specific policy tools that countries have usedto strengthen their generic medic<strong>in</strong>es market and their experience with them. Table 1 outl<strong>in</strong>es thestrengths and weaknesses of policy <strong>in</strong>struments.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 6713.1 Market entryHav<strong>in</strong>g a market<strong>in</strong>g authorisation does not tend to suffice for a generic medic<strong>in</strong>e to enter themarket. <strong>Generic</strong> medic<strong>in</strong>es enter the market follow<strong>in</strong>g determ<strong>in</strong>ation of price and reimbursementstatus by authorities. Each EU country has national responsibility over pric<strong>in</strong>g and reimbursementdecisions. Procedures for determ<strong>in</strong><strong>in</strong>g pric<strong>in</strong>g and reimbursement delay market entry of genericmedic<strong>in</strong>es and appear to be unnecessarily long <strong>in</strong> the case of generic medic<strong>in</strong>es that havedemonstrated the same quality, safety and therapeutic efficacy as the orig<strong>in</strong>ator medic<strong>in</strong>e. Theredoes not seem to be a case for delay<strong>in</strong>g market access to generic medic<strong>in</strong>es once all <strong>in</strong>tellectualproperty and data exclusivity periods are exhausted.The Transparency Directive 89/105/EEC specifies a 90-day limit for adopt<strong>in</strong>g a decision on priceand a 90-day limit for reimbursement. Several studies have shown that, <strong>in</strong> practice, delays <strong>in</strong>obta<strong>in</strong><strong>in</strong>g pric<strong>in</strong>g and reimbursement approval have exceeded these time limits (<strong>Europe</strong>Economics, 1998; Cambridge Pharma Consultancy, 2002). An EGA survey revealed that the timedelay for price approval <strong>in</strong> January 2005 surpassed 90 days <strong>in</strong> Austria and Italy, equalled 90 days<strong>in</strong> Belgium and Portugal, was shorter than 90 days <strong>in</strong> France, the Netherlands and Spa<strong>in</strong> (EGA,2005). There is no formal pric<strong>in</strong>g approval process <strong>in</strong> Denmark. In Germany and the UnitedK<strong>in</strong>gdom, generic medic<strong>in</strong>es can be put on the market follow<strong>in</strong>g market<strong>in</strong>g authorisation. Furtherdelays are experienced as a result of reimbursement and substitution policies.Variation <strong>in</strong> delays for pric<strong>in</strong>g and reimbursement approval obstructs the creation of a levelplay<strong>in</strong>g field for market entry across EU countries and h<strong>in</strong>ders the development of a competitive<strong>Europe</strong>an generic medic<strong>in</strong>es <strong>in</strong>dustry.13.2 Pric<strong>in</strong>gPenetration of generic medic<strong>in</strong>es is more successful <strong>in</strong> countries that permit (relatively) freepric<strong>in</strong>g of medic<strong>in</strong>es (e.g. Germany, the Netherlands, United K<strong>in</strong>gdom) than <strong>in</strong> countries that havepric<strong>in</strong>g regulation (e.g. Austria, Belgium, France, Italy, Portugal, Spa<strong>in</strong>).Countries that adhere to free market pric<strong>in</strong>g generally have higher medic<strong>in</strong>e prices. Averagemedic<strong>in</strong>e prices <strong>in</strong> Germany, the Netherlands and the United K<strong>in</strong>gdom surpassed those <strong>in</strong>France, Italy and Spa<strong>in</strong> <strong>in</strong> 2001 (Schulz, 2004). Higher medic<strong>in</strong>e prices stimulate genericmedic<strong>in</strong>es companies to enter the market. This contrasts with regulated markets, where pric<strong>in</strong>gregulation drives down the orig<strong>in</strong>ator price over the life cycle of the medic<strong>in</strong>e. This lowers thepotential profit marg<strong>in</strong> for a generic medic<strong>in</strong>e company and discourages market entry.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 68Table 1. Country experiences with policy tools to promote generic medic<strong>in</strong>es useType of policy Country of policy Policy strengths Policy weaknessesMarket entry- Pric<strong>in</strong>g andreimbursementapproval processAustria, Belgium,Denmark, France, Italy,Netherlands, Poland,Portugal, Spa<strong>in</strong>Mechanism to checkjustification for price andreimbursement statusDelays market entry ofgeneric medic<strong>in</strong>es andprevents level play<strong>in</strong>g fieldacross countries.Pric<strong>in</strong>g- Free pric<strong>in</strong>g ofmedic<strong>in</strong>esGermany, Netherlands,United K<strong>in</strong>gdomHigh medic<strong>in</strong>e prices createattractive conditions formarket entry by genericmedic<strong>in</strong>es. Large pricedifferences betweenorig<strong>in</strong>ator and genericmedic<strong>in</strong>es stimulate patientdemand for genericmedic<strong>in</strong>es.Strong price competitioncould endanger the longtermsusta<strong>in</strong>ability of thegeneric medic<strong>in</strong>es <strong>in</strong>dustry.- Pric<strong>in</strong>g regulation Austria, Belgium, France,Italy, Portugal, Spa<strong>in</strong>Mechanism to conta<strong>in</strong> publicpharmaceutical expenditure.Lower medic<strong>in</strong>e pricesdiscourage market entry ofgeneric medic<strong>in</strong>es. Smallerprice differences betweenorig<strong>in</strong>ator and genericmedic<strong>in</strong>es restrict patientdemand for genericmedic<strong>in</strong>es.Reference pric<strong>in</strong>g- Reference-pric<strong>in</strong>gsystemBelgium, Denmark,France, Germany, Italy,Netherlands, Poland,Portugal, Spa<strong>in</strong>F<strong>in</strong>ancial <strong>in</strong>centive forpatients to demand genericmedic<strong>in</strong>es priced belowreference price.Does not stimulate genericmedic<strong>in</strong>es use if orig<strong>in</strong>atormedic<strong>in</strong>es reduce their pricebelow level of referenceprice.° Low reference price Denmark, Italy, Poland Establishes clear pricedifferential betweenorig<strong>in</strong>ator and genericmedic<strong>in</strong>es.° High reference price Portugal Facilitates market entry ofgeneric medic<strong>in</strong>es.Forces companies to pricegeneric medic<strong>in</strong>es close tomarg<strong>in</strong>al costs andthreatens economic viability.Small price differencebetween orig<strong>in</strong>ator andgeneric medic<strong>in</strong>es restrictspatient demand for genericmedic<strong>in</strong>es.° Narrow referencegroupsDenmark, France, Italy,PortugalHomogeneous groups ofmedic<strong>in</strong>es.Re-allocation of demandbetween groups or betweengroup and patentedmedic<strong>in</strong>es not covered byRPS.° Broad referencegroupsGermany, NetherlandsStimulates competitionamong medic<strong>in</strong>es that targetthe same illness. Reducespotential for re-allocation ofdemand.Heterogeneous groups ofmedic<strong>in</strong>es with potential ofprescription of less effectivemedic<strong>in</strong>e <strong>in</strong> order to avoidco-payment.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 69Table 1 (cont). Country experiences with policy tools to promote generic medic<strong>in</strong>es useType of policy Country of policy Policy strengths Policy weaknessesIncentives for physicians- Budgets Germany, UnitedK<strong>in</strong>gdom- INN prescrib<strong>in</strong>g Denmark, Netherlands,Portugal, United K<strong>in</strong>gdom- Non-f<strong>in</strong>ancial <strong>in</strong>centives Austria, Belgium,Denmark, France,Netherlands, Italy,PortugalIncreases genericprescription rates.Creates potential for deliveryof generic medic<strong>in</strong>es bypharmacists.Tools that support low-costprescrib<strong>in</strong>g by physicians.Only effective <strong>in</strong> comb<strong>in</strong>ationwith sanctions for budgetoverruns. May encouragereferral or admission tohospital.Depends on attitude ofphysicians, dispens<strong>in</strong>gregulation and remunerationof pharmacists.Voluntary nature of schemeswith unproven effect ongeneric prescription rates.Incentives for pharmacists- Absolute pharmacistmarg<strong>in</strong>s on medic<strong>in</strong>esBelgium, FrancePharmacists ga<strong>in</strong> samemarg<strong>in</strong> on orig<strong>in</strong>ator andgeneric medic<strong>in</strong>es.Increases price of genericmedic<strong>in</strong>es relative toorig<strong>in</strong>ator medic<strong>in</strong>es.Incentives for patients- Patient co-payment Belgium, Denmark,France, Germany, Italy,Netherlands, Poland,Portugal, Spa<strong>in</strong>- Information campaign Belgium, Italy, Portugal,Spa<strong>in</strong>, United K<strong>in</strong>gdomHigher co-payment onorig<strong>in</strong>ator medic<strong>in</strong>esstimulates demand forgeneric medic<strong>in</strong>es.Increases patient awarenessof and demand for genericmedic<strong>in</strong>es.Stimulus weakened ifphysicians are not costconsciousor co-paymentcovered by additional<strong>in</strong>surance.Small effect if campaign isshort-lived and has limitedexposure.In countries with free pric<strong>in</strong>g, the price difference between orig<strong>in</strong>ator and generic medic<strong>in</strong>es tendsto be higher than <strong>in</strong> countries with pric<strong>in</strong>g regulation. International comparisons <strong>in</strong>dicate that theprice differential for blockbuster medic<strong>in</strong>es of 80% <strong>in</strong> Germany, the United K<strong>in</strong>gdom and theUnited States (de Joncheere et al., 2002; K<strong>in</strong>g and Kanavos, 2002) exceeded the m<strong>in</strong>imum pricedifference of 10% <strong>in</strong> Austria, 20% <strong>in</strong> Italy, 30% <strong>in</strong> France, and 35% <strong>in</strong> Portugal at the end of the1990s / early 2000s.13.3 Reference pric<strong>in</strong>gThe majority of countries <strong>in</strong>cluded <strong>in</strong> this report have <strong>in</strong>troduced a RPS. The objective of a RPS isto conta<strong>in</strong> public pharmaceutical expenditure by controll<strong>in</strong>g the reimbursement level of medic<strong>in</strong>es.A RPS may aid generic market penetration because orig<strong>in</strong>ator medic<strong>in</strong>es priced above the levelof the RP are likely to lose market share as a result of an additional patient co-payment.Conversely, if the RPS is accompanied by price reductions of orig<strong>in</strong>ator medic<strong>in</strong>es to the level ofthe RP, the RPS does not aid the development of the generic medic<strong>in</strong>es market. Evidence ofsuch a pric<strong>in</strong>g strategy of orig<strong>in</strong>ator medic<strong>in</strong>e companies <strong>in</strong> the context of a RPS was found forFrance and Italy. A RPS tends to be more successful <strong>in</strong> markets characterised by a developed
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 70generic medic<strong>in</strong>es segment, substantial price differences between medic<strong>in</strong>es with<strong>in</strong> a group, anda high level of medic<strong>in</strong>e prices (Lopez-Casasnovas and Puig-Junoy, 2000).13.3.1 Level of reference priceThe RP is generally calculated as a function of market prices of medic<strong>in</strong>es, with differencesbetween countries as to which medic<strong>in</strong>es are taken <strong>in</strong>to account. A low reimbursement level ischosen <strong>in</strong> Denmark, Italy and Poland where the RP equals the price of the cheapest (generic)medic<strong>in</strong>e. A higher reimbursement level applies <strong>in</strong> the Netherlands, where the RP is set as themedian price of all medic<strong>in</strong>es <strong>in</strong> the group, or <strong>in</strong> Portugal, where the highest price of availablegeneric medic<strong>in</strong>es makes up the RP. These differences <strong>in</strong> the level of the RP <strong>in</strong>fluence theeconomic viability of generic medic<strong>in</strong>es companies to enter the market and the competitive priceadvantage of generic versus orig<strong>in</strong>ator medic<strong>in</strong>es. By calculat<strong>in</strong>g the RP as a function of pricesand the level of generic competition as for example <strong>in</strong> Germany, a RPS can stimulate thedevelopment of the generic medic<strong>in</strong>es market, while conta<strong>in</strong><strong>in</strong>g public pharmaceuticalexpenditure.13.3.2 Breadth of reference groupsAs equivalence criteria for select<strong>in</strong>g a group of <strong>in</strong>terchangeable medic<strong>in</strong>es are broadened fromactive substance to pharmacological class and, ultimately, to therapeutic class, heterogeneity ofmedic<strong>in</strong>es with<strong>in</strong> the same group <strong>in</strong>creases. A RPS by therapeutic class may lead to theprescription of a less effective medic<strong>in</strong>e with<strong>in</strong> the group if it allows the patient to avoid a copayment.Therefore, countries tend to def<strong>in</strong>e more narrow groups of medic<strong>in</strong>es by activesubstance or pharmacological class. However, the experience of France and Italy shows thatsuch systems may suffer from re-allocation of demand away from a RPS group to patentedmedic<strong>in</strong>es with a similar therapeutic <strong>in</strong>dication that do not fall under the RPS.13.4 Incentives for physiciansIn their capacity of prescrib<strong>in</strong>g medic<strong>in</strong>es, physicians play a key role <strong>in</strong> the development of ageneric medic<strong>in</strong>es market. Therefore, countries have <strong>in</strong>troduced a variety of f<strong>in</strong>ancial and nonf<strong>in</strong>ancial<strong>in</strong>centives to encourage generic prescrib<strong>in</strong>g.Some countries have experimented with budgets at regional level (e.g. Germany) or budgets atthe level of an <strong>in</strong>dividual physician (e.g. United K<strong>in</strong>gdom). The experience of these countries withbudgets suggests that rewards or sanctions are a necessary condition for mak<strong>in</strong>g budgets
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 71effective. Budgetary schemes may require careful monitor<strong>in</strong>g and regulation because f<strong>in</strong>ancial<strong>in</strong>centives which <strong>in</strong> fact reward cost conta<strong>in</strong>ment may reward selection of less risky patients,stimulate referrals and hospital admissions, and jeopardise quality of care and health outcomes.Additional remuneration if physicians atta<strong>in</strong> specific generic medic<strong>in</strong>es prescription rates appearto have had little impact <strong>in</strong> France and Spa<strong>in</strong>.Some countries have attempted to stimulate generic medic<strong>in</strong>es use through INN prescrib<strong>in</strong>g.Successful INN prescrib<strong>in</strong>g policies have been implemented <strong>in</strong> Denmark and the UnitedK<strong>in</strong>gdom, where students are taught to prescribe by INN <strong>in</strong> medical school; <strong>in</strong> the Netherlands,where physicians are stimulated to engage <strong>in</strong> INN prescrib<strong>in</strong>g; and <strong>in</strong> Portugal, where physiciansare required to prescribe reimbursed medic<strong>in</strong>es for which generic equivalents exist by INN. Theattitude of physicians towards INN prescrib<strong>in</strong>g is a crucial determ<strong>in</strong>ant of the success of suchpolicies. INN prescrib<strong>in</strong>g has been limited <strong>in</strong> countries such as Belgium and France <strong>in</strong> light ofopposition by physicians who value their prescrib<strong>in</strong>g freedom and their tradition to prescribebrand-name medic<strong>in</strong>es.INN prescrib<strong>in</strong>g does not necessarily lead to generic medic<strong>in</strong>es use. The success of INNprescrib<strong>in</strong>g policies <strong>in</strong> stimulat<strong>in</strong>g generic medic<strong>in</strong>es use depends on regulation govern<strong>in</strong>g whichmedic<strong>in</strong>e the pharmacist needs to dispense. The decision of which medic<strong>in</strong>e to dispense is also<strong>in</strong>fluenced by the f<strong>in</strong>ancial remuneration of pharmacists. Only if INN dispens<strong>in</strong>g regulation andremuneration of pharmacists favours generic medic<strong>in</strong>es, then INN prescrib<strong>in</strong>g can be expected toraise generic medic<strong>in</strong>es use.Countries have <strong>in</strong>itiated various non-f<strong>in</strong>ancial <strong>in</strong>centives to stimulate generic medic<strong>in</strong>es use.<strong>Generic</strong> prescrib<strong>in</strong>g by physicians has been supported by electronic prescrib<strong>in</strong>g systems,medic<strong>in</strong>e databases, audit of and feedback on prescrib<strong>in</strong>g data, prescrib<strong>in</strong>g guidel<strong>in</strong>es andformularies, and local pharmaco-therapeutic discussions between physicians and pharmacists.Such policy measures generally are voluntary and the absence of sanctions if physicians do notadhere to these <strong>in</strong>itiatives is likely to restrict their effectiveness. The impact of non-f<strong>in</strong>ancial<strong>in</strong>centives on promot<strong>in</strong>g generic medic<strong>in</strong>es use has rarely been <strong>in</strong>vestigated.13.5 Incentives for pharmacists<strong>Generic</strong> substitution may aid generic medic<strong>in</strong>es use if it is f<strong>in</strong>ancially neutral or attractive topharmacists to substitute generic for orig<strong>in</strong>ator medic<strong>in</strong>es.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 72The remuneration system of pharmacists <strong>in</strong> some countries provides a f<strong>in</strong>ancial dis<strong>in</strong>centive todispense generic medic<strong>in</strong>es. Sett<strong>in</strong>g pharmacists’ remuneration as a fixed percentage of thepublic price of medic<strong>in</strong>es as <strong>in</strong> Portugal and Spa<strong>in</strong> rewards the delivery of orig<strong>in</strong>ator medic<strong>in</strong>es.Countries such as Italy and Poland have adopted slid<strong>in</strong>g scales where the percentageremuneration decreases as prices rise. However, the regressive effect of such scales is notsufficient to remove the f<strong>in</strong>ancial <strong>in</strong>centive to dispense orig<strong>in</strong>ator medic<strong>in</strong>es.Other remuneration systems have been used that make the delivery of a generic or orig<strong>in</strong>almedic<strong>in</strong>e neutral to pharmacists from a f<strong>in</strong>ancial perspective. Pharmacists earn the same marg<strong>in</strong><strong>in</strong> absolute terms on orig<strong>in</strong>ator and generic medic<strong>in</strong>es <strong>in</strong> Belgium and France. However, a systemof absolute marg<strong>in</strong>s <strong>in</strong>creases prices of generic medic<strong>in</strong>es relative to orig<strong>in</strong>ator medic<strong>in</strong>es,thereby <strong>in</strong>hibit<strong>in</strong>g generic medic<strong>in</strong>es use. Alternatively, pharmacists can be paid by means of afixed fee per prescription (item). This provides a neutral f<strong>in</strong>ancial <strong>in</strong>centive for pharmacists todispense a generic or orig<strong>in</strong>ator medic<strong>in</strong>e.Few countries have <strong>in</strong> place systems that f<strong>in</strong>ancially reward pharmacists for substitut<strong>in</strong>g genericfor orig<strong>in</strong>ator medic<strong>in</strong>es. In the Netherlands, pharmacists are encouraged to dispense medic<strong>in</strong>esthat are priced below the RP by be<strong>in</strong>g able to reta<strong>in</strong> a percentage of the difference between themedic<strong>in</strong>e price and the RP. In France, pharmacists are entitled to higher discounts on genericmedic<strong>in</strong>es than on orig<strong>in</strong>ator medic<strong>in</strong>es. In Spa<strong>in</strong>, higher percentage marg<strong>in</strong>s for genericmedic<strong>in</strong>es than for orig<strong>in</strong>ator medic<strong>in</strong>es stimulate pharmacists to dispense the most expensivegeneric medic<strong>in</strong>es. Pharmacist remuneration <strong>in</strong> these countries attenuates the <strong>in</strong>centive forcompanies to compete with each other on price and reduce prices of generic medic<strong>in</strong>es below thelevel of the RP. Instead, companies compete through offer<strong>in</strong>g discounts to pharmacists. Such asystem may f<strong>in</strong>ancially benefit pharmacists, but is not susta<strong>in</strong>able <strong>in</strong> the long run as health carepayers and patients do not capture the potential sav<strong>in</strong>gs from a generic medic<strong>in</strong>es market wherecompanies compete on price.13.6 Incentives for patientsCountries have not fully recognised the role that patients play <strong>in</strong> generic medic<strong>in</strong>es consumption.Generally, few policy measures are <strong>in</strong> place that either <strong>in</strong>cite patients to demand genericmedic<strong>in</strong>es or penalise patients for not demand<strong>in</strong>g generic medic<strong>in</strong>es.The extent to which patients contribute to the cost of drugs is likely to play a role <strong>in</strong> the use ofgeneric medic<strong>in</strong>es. A RPS may promote generic medic<strong>in</strong>es use by impos<strong>in</strong>g a co-payment onorig<strong>in</strong>ator medic<strong>in</strong>es priced above the level of the RP. Also, a lower percentage co-payment on
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 73generic medic<strong>in</strong>es appears to have stimulated the Portuguese generic medic<strong>in</strong>es market. ThePolish experience <strong>in</strong>dicates that the impact of patient co-payments depends on the extent towhich physicians are conscious of the level of patient co-payments and take it <strong>in</strong>to account <strong>in</strong>their prescrib<strong>in</strong>g decisions. Furthermore, the stimulus to prescribe generic medic<strong>in</strong>es is likely todisappear if co-payments are covered by the private <strong>in</strong>surance of patients such as <strong>in</strong> France.Several countries <strong>in</strong>clud<strong>in</strong>g Belgium, Italy, Portugal, Spa<strong>in</strong> and the United K<strong>in</strong>gdom havelaunched advertis<strong>in</strong>g campaigns to <strong>in</strong>form patients of generic medic<strong>in</strong>es. In Belgium, thecampaign was short-lived and had limited exposure. In Portugal, pro-generic-medic<strong>in</strong>e mediacampaigns aimed at physicians and pharmacists <strong>in</strong> addition to patients appear to havecontributed to rais<strong>in</strong>g demand for generic medic<strong>in</strong>es. No formal evaluations of the impact ofadvertis<strong>in</strong>g campaigns on generic medic<strong>in</strong>es consumption exist.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 74PART IVRECOMMENDATIONS TO STRENGTHENGENERIC MEDICINES MARKETS
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 7514 Strengthen<strong>in</strong>g generic medic<strong>in</strong>es marketsBased on the experience of develop<strong>in</strong>g generic medic<strong>in</strong>es markets <strong>in</strong> selected countries, this partof the report proposes a number of recommendations to strengthen generic medic<strong>in</strong>es markets.The guid<strong>in</strong>g pr<strong>in</strong>ciple used here is recommendation 4 of the report prepared by the G10 HighLevel Group on Innovation and Provision of <strong>Medic<strong>in</strong>es</strong> <strong>in</strong> the <strong>Europe</strong>an Union <strong>in</strong> 2002:“To secure the development of a competitive generic market. Member States – facilitated by theCommission – should explore ways of <strong>in</strong>creas<strong>in</strong>g generic penetration <strong>in</strong> <strong>in</strong>dividual markets(<strong>in</strong>clud<strong>in</strong>g generic prescrib<strong>in</strong>g and dispens<strong>in</strong>g. Particular attention should be given to improvedmarket mechanisms <strong>in</strong> full respect of public health considerations.”General recommendations for the group of selected countries as well as recommendations foreach <strong>in</strong>dividual country are suggested.14.1 General recommendations1. Introduce a coherent generic medic<strong>in</strong>es policyPolicy <strong>in</strong>tervention is required to develop a competitive generic medic<strong>in</strong>es market. A genericmedic<strong>in</strong>es policy requires both supply-side measures (pric<strong>in</strong>g and reimbursement) and demandsidemeasures (<strong>in</strong>centives for physicians, pharmacists, patients). Attention needs to be paid to<strong>in</strong>teractions between policy measures. Different policy measures need to re<strong>in</strong>force each otherand be part of a coherent generic medic<strong>in</strong>es policy.2. Encourage price differentiation / competition with<strong>in</strong> exist<strong>in</strong>g regulatory frameworksAll countries studied have <strong>in</strong>troduced pric<strong>in</strong>g regulation to some extent. This has taken the form ofdirect fixed price controls, profit controls or reference pric<strong>in</strong>g. Countries can establish a system offixed m<strong>in</strong>imum price differences between generic and orig<strong>in</strong>ator medic<strong>in</strong>es <strong>in</strong> the context ofexist<strong>in</strong>g RPS. This approach has the benefit of guarantee<strong>in</strong>g sav<strong>in</strong>gs to health <strong>in</strong>surance funds,although it is not clear at what level maximum prices need to be set. Health <strong>in</strong>surance funds willlose out if they have established prices at a higher level than would have been observed <strong>in</strong> acompetitive market.An alternative approach is to establish a free pric<strong>in</strong>g system with<strong>in</strong> the context of exist<strong>in</strong>g RPS.The RP can be set at the average price level of generic medic<strong>in</strong>es <strong>in</strong> the reference group or at a
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 76lower price level, once the generic medic<strong>in</strong>es market has reached a m<strong>in</strong>imum level ofdevelopment. This m<strong>in</strong>imum level could, for <strong>in</strong>stance, be set at a generic market share by volumeof 40%. In comb<strong>in</strong>ation with <strong>in</strong>centives to stimulate demand for generic medic<strong>in</strong>es, genericmedic<strong>in</strong>e companies would have an <strong>in</strong>centive to compete, thereby driv<strong>in</strong>g down (reference) pricesof medic<strong>in</strong>es. In countries with develop<strong>in</strong>g generic medic<strong>in</strong>es markets, sett<strong>in</strong>g the RP at a higherlevel to encourage market entry can be <strong>in</strong>troduced as a temporary measure to boost the genericmedic<strong>in</strong>es market until it reaches a more mature level of development.Information about prices needs to be transparent. This may not be the case <strong>in</strong> countries wheregeneric medic<strong>in</strong>es companies compete with each other through offer<strong>in</strong>g discounts to pharmacists.The practice of discount<strong>in</strong>g is not clear to market actors and is not fair as pharmacists are notrewarded for services rendered, but for their ability to negotiate discounts on artificial prices.Therefore, countries need to consider mov<strong>in</strong>g away from competition by discount to competitionby price. Such a system would be transparent and easy for all market actors to understand, andwould ensure that prices paid by health <strong>in</strong>surance funds reflect best value for money.3. Dissem<strong>in</strong>ate pric<strong>in</strong>g <strong>in</strong>formation to actorsInformation about the price difference between orig<strong>in</strong>ator and generic medic<strong>in</strong>es needs to becommunicated to relevant actors, thus creat<strong>in</strong>g an <strong>in</strong>centive for physicians to prescribe,pharmacists to dispense, and patients to ask for generic medic<strong>in</strong>es. It is important to ensure thatactors have access to <strong>in</strong>formation about medic<strong>in</strong>e prices that is correct, comprehensive, and upto-date.The collection and dissem<strong>in</strong>ation of pric<strong>in</strong>g <strong>in</strong>formation may be carried out by nationalmedic<strong>in</strong>e agencies through the regular publication of a medic<strong>in</strong>e pric<strong>in</strong>g guide. Additionally,pric<strong>in</strong>g <strong>in</strong>formation can be <strong>in</strong>cluded <strong>in</strong> medic<strong>in</strong>e databases, electronic prescription systems,prescrib<strong>in</strong>g guidel<strong>in</strong>es and treatment protocols.4. Increase confidence of actors <strong>in</strong> generic medic<strong>in</strong>esMore emphasis needs to be placed on conv<strong>in</strong>c<strong>in</strong>g physicians, pharmacists and patients of thebio-equivalence of generic and orig<strong>in</strong>ator medic<strong>in</strong>es. This entails provid<strong>in</strong>g actors with <strong>in</strong>formationabout the quality, safety and efficacy of generic medic<strong>in</strong>es. National medic<strong>in</strong>e agencies can playa role by periodically publish<strong>in</strong>g lists of all active <strong>in</strong>gredients for which generic medic<strong>in</strong>es havebeen approved by regulatory authorities.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 775. Provide <strong>in</strong>centives for physicians to prescribe generic medic<strong>in</strong>esPrescrib<strong>in</strong>g decisions by physicians play a key role <strong>in</strong> the use of generic and orig<strong>in</strong>ator medic<strong>in</strong>es.Countries need to recommend to physicians to prescribe low-cost medic<strong>in</strong>es, unless a moreexpensive, orig<strong>in</strong>ator medic<strong>in</strong>e is required for therapeutic reasons.Countries need to <strong>in</strong>itiate f<strong>in</strong>ancial and non-f<strong>in</strong>ancial <strong>in</strong>centives for physicians to prescribe genericmedic<strong>in</strong>es. Recommended policy tools <strong>in</strong>clude the follow<strong>in</strong>g:• Improve prescrib<strong>in</strong>g education at undergraduate level and make medical students aware ofINN prescrib<strong>in</strong>g;• Demonstrate to physicians the amount of sav<strong>in</strong>gs to pharmaceutical and physician budgetsthat can be atta<strong>in</strong>ed from prescrib<strong>in</strong>g generic medic<strong>in</strong>es;• Support physician prescrib<strong>in</strong>g by electronic prescrib<strong>in</strong>g systems, medic<strong>in</strong>e databases, audit ofand feedback on prescrib<strong>in</strong>g data, prescrib<strong>in</strong>g guidel<strong>in</strong>es and formularies, substitution lists,and local pharmaco-therapeutic discussions between physicians and pharmacists.These policy tools need to be accompanied by rewards/sanctions for physicians who do/do notadhere to them, respectively.6. Remove f<strong>in</strong>ancial dis<strong>in</strong>centives for pharmacists to dispense generic medic<strong>in</strong>esPharmacists need to receive a remuneration that does not f<strong>in</strong>ancially penalise them fordispens<strong>in</strong>g generic medic<strong>in</strong>es. Countries need to move away from distribution marg<strong>in</strong>s that areset as a fixed percentage of the public price of medic<strong>in</strong>es or marg<strong>in</strong>s that, even though they areregressive, still favour the delivery of orig<strong>in</strong>ator medic<strong>in</strong>es. Instead, countries need to consider<strong>in</strong>troduc<strong>in</strong>g pharmacist remuneration systems that are neutral or favour the delivery of genericmedic<strong>in</strong>es from a f<strong>in</strong>ancial perspective.7. Provide <strong>in</strong>centives for patients to demand generic medic<strong>in</strong>esCountries need to <strong>in</strong>cite patients to demand generic medic<strong>in</strong>es or penalise patients who do notdemand generic medic<strong>in</strong>es. This may take the form of f<strong>in</strong>ancial <strong>in</strong>centives that reduce copaymenton generic medic<strong>in</strong>es or impose higher co-payment on orig<strong>in</strong>ator medic<strong>in</strong>es.Furthermore, countries can raise patient awareness of generic medic<strong>in</strong>es by means of advertis<strong>in</strong>gcampaigns. Initiatives that attempt to <strong>in</strong>fluence consumption patterns by personally contact<strong>in</strong>gpatients can also be envisaged.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 7814.2 Country-specific recommendationsFor each country, recommendations are proposed that build on the key factors aid<strong>in</strong>g / h<strong>in</strong>der<strong>in</strong>gthe development of the national generic medic<strong>in</strong>es market as set out <strong>in</strong> the first two parts of thereport.14.2.1 AustriaAustria has adopted a rigid pharmaceutical pric<strong>in</strong>g policy that regulates the price level oforig<strong>in</strong>ator and generic medic<strong>in</strong>es. This policy has not stimulated market entry of genericmedic<strong>in</strong>es or supported the economic viability of the generic medic<strong>in</strong>es market. The pric<strong>in</strong>gsystem needs to be deregulated and market forces should determ<strong>in</strong>e the price differencebetween orig<strong>in</strong>ator and generic medic<strong>in</strong>es.There are no policy measures <strong>in</strong> place that stimulate demand for generic medic<strong>in</strong>es. Therefore,policy makers need to focus on creat<strong>in</strong>g <strong>in</strong>centives for physicians to prescribe, pharmacists todispense, and patients to demand generic medic<strong>in</strong>es. Incentives for physicians may take the formof national implementation of generic prescrib<strong>in</strong>g targets. <strong>Generic</strong> substitution by pharmacistsneeds to be allowed and the f<strong>in</strong>ancial dis<strong>in</strong>centive for pharmacists to dispense generic medic<strong>in</strong>esneeds to be removed.14.2.2 BelgiumBy sett<strong>in</strong>g the RP at a certa<strong>in</strong> percentage below the price of the orig<strong>in</strong>ator medic<strong>in</strong>e, the RPScontributes to conta<strong>in</strong><strong>in</strong>g public pharmaceutical expenditure, but does not stimulate pricecompetition between companies. It is proposed to abolish m<strong>in</strong>imum price differences betweengeneric and orig<strong>in</strong>ator medic<strong>in</strong>es, and establish the RP at the average price level of genericmedic<strong>in</strong>es <strong>in</strong> the reference group or at a lower price level. This would be expected to create pricecompetition between companies as well as restrict public expenditure.To ensure the economic viability of the Belgian generic medic<strong>in</strong>es market, competitive priceswould need to be accompanied by demand-side measures support<strong>in</strong>g the volume of genericmedic<strong>in</strong>es consumption.Although Belgium has recently implemented <strong>in</strong>itiatives that <strong>in</strong>cite physicians to promote genericmedic<strong>in</strong>es use, these <strong>in</strong>centives tend to be weak and need to be re<strong>in</strong>forced. Allow<strong>in</strong>g INNprescrib<strong>in</strong>g is likely to be <strong>in</strong>sufficient <strong>in</strong> a climate of physician opposition to INN prescrib<strong>in</strong>g.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 79Therefore, medical students need to be taught and physicians need to be actively encouraged toprescribe by INN. Furthermore, generic prescrib<strong>in</strong>g by physicians needs to be supported byelectronic prescrib<strong>in</strong>g systems, medic<strong>in</strong>e databases, substitution lists, and local pharmacotherapeuticdiscussions between physicians and pharmacists. Physician adherence to prescrib<strong>in</strong>gguidel<strong>in</strong>es needs to be stimulated.INN prescrib<strong>in</strong>g needs to be complemented by <strong>in</strong>centives for pharmacists. One option is to<strong>in</strong>troduce a requirement that the pharmacist dispenses the cheapest medic<strong>in</strong>e <strong>in</strong> the case of anINN prescription. An alternative option is to allow pharmacists to dispense an orig<strong>in</strong>ator or genericmedic<strong>in</strong>e when the prescription is issued by INN. In addition to this, pharmacists would reta<strong>in</strong> apercentage of the difference between the RP and the price of the medic<strong>in</strong>e dispensed. This wouldencourage pharmacists not to seek discounts as this practice is questionable from a legalperspective, but to dispense the medic<strong>in</strong>e with the lowest price. This proposed pharmacistremuneration system would replace the current system which drives up generic medic<strong>in</strong>e pricesand <strong>in</strong>hibits patient demand by guarantee<strong>in</strong>g the same absolute marg<strong>in</strong> on generic and orig<strong>in</strong>atormedic<strong>in</strong>es.14.2.3 DenmarkDenmark has a competitive generic medic<strong>in</strong>es market where regulation govern<strong>in</strong>g theestablishment of RPs and generic substitution by pharmacists creates low prices and a highvolume of generic medic<strong>in</strong>es consumption. However, the adm<strong>in</strong>istrative burden of runn<strong>in</strong>g theRPS is considerable. In a market where price competition is tak<strong>in</strong>g place as a result of genericsubstitution rules, there may not be a need for a RPS.There may be scope to <strong>in</strong>crease demand for generic medic<strong>in</strong>es by creat<strong>in</strong>g <strong>in</strong>centives forphysicians and patients. The Government may consider tak<strong>in</strong>g <strong>in</strong>itiatives to <strong>in</strong>form and persuadephysicians and patients of the substitutability of generic for orig<strong>in</strong>ator medic<strong>in</strong>es. This may reducethe (low) proportion of prescriptions where the physician has forbidden substitution and theproportion of patients who refuse substitution.14.2.4 FranceLow medic<strong>in</strong>e prices and regulation impos<strong>in</strong>g a substantial price difference between generic andorig<strong>in</strong>ator medic<strong>in</strong>es has h<strong>in</strong>dered market entry of generic medic<strong>in</strong>es. Abolish<strong>in</strong>g m<strong>in</strong>imum pricedifferences between generic and orig<strong>in</strong>ator medic<strong>in</strong>es <strong>in</strong> comb<strong>in</strong>ation with the exist<strong>in</strong>g RPS wouldbe expected to support entry of generic medic<strong>in</strong>es <strong>in</strong> market segments with few competitors and
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 80<strong>in</strong>cite price competition <strong>in</strong> market segments with many competitors. Price competition can also bestrengthened by further reduc<strong>in</strong>g the level of discounts that companies are allowed to award topharmacists.There is a need for policy to boost demand for generic medic<strong>in</strong>es. Although some <strong>in</strong>centives forphysicians to prescribe generic medic<strong>in</strong>es have been <strong>in</strong>troduced <strong>in</strong> recent years, more effortneeds to be put <strong>in</strong>to promot<strong>in</strong>g professional acceptance of generic medic<strong>in</strong>es by physicians. Inparticular, INN prescrib<strong>in</strong>g needs to be actively stimulated by <strong>in</strong>clud<strong>in</strong>g it <strong>in</strong> the education ofmedical students or by reward<strong>in</strong>g physicians who reach specific INN prescrib<strong>in</strong>g target rates. Thiswill stimulate demand for generic medic<strong>in</strong>es as pharmacists may dispense any generic medic<strong>in</strong>e<strong>in</strong> the case of an INN prescription. To reduce re-allocation of demand, the Government couldcollect data on the physician prescription profile of off-patent medic<strong>in</strong>es and patented medic<strong>in</strong>eswith the same therapeutic <strong>in</strong>dication, and set target prescription rates of off-patent medic<strong>in</strong>es.As co-payment tends to be covered by additional private <strong>in</strong>surance, patients do not have af<strong>in</strong>ancial <strong>in</strong>centive to demand generic medic<strong>in</strong>es. Government or health <strong>in</strong>surance fund <strong>in</strong>itiativesthat <strong>in</strong>form patients of the existence of a generic equivalent need to be expanded as pilot projectshave shown a positive <strong>in</strong>fluence on generic medic<strong>in</strong>es use.14.2.5 GermanyThe RPS appears to have contributed to develop<strong>in</strong>g the German generic medic<strong>in</strong>es market, butits operation represents a considerable adm<strong>in</strong>istrative burden. In this mature generic medic<strong>in</strong>esmarket characterised by price competition and generic medic<strong>in</strong>es priced substantially below thelevel of orig<strong>in</strong>ator medic<strong>in</strong>es, there may not be a need for a RPS. If the RPS was to be abolished,<strong>in</strong>centives for generic substitution and dispens<strong>in</strong>g by pharmacists would need to be re<strong>in</strong>forced.Regulation requir<strong>in</strong>g pharmacists to substitute with the least expensive medic<strong>in</strong>e if neitherphysician nor patient objects to such substitution and a dispens<strong>in</strong>g budget for pharmacists arelikely to susta<strong>in</strong> price competition and provide a stimulus for generic medic<strong>in</strong>es use. The f<strong>in</strong>ancial<strong>in</strong>centive for pharmacists to dispense orig<strong>in</strong>ator medic<strong>in</strong>es needs to be abolished.The German generic medic<strong>in</strong>es market is driven by physician prescrib<strong>in</strong>g of generic medic<strong>in</strong>es.F<strong>in</strong>ancial and non-f<strong>in</strong>ancial <strong>in</strong>centives for physicians appear to have supported generic medic<strong>in</strong>esuse, but their effectiveness can be strengthened by execut<strong>in</strong>g sanctions for physicians who donot adhere to them or by award<strong>in</strong>g a bonus to physicians who adhere.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 8114.2.6 ItalyThe Italian generic medic<strong>in</strong>es market is <strong>in</strong> the early stages of development and suffers from lowprices and low volume of generic medic<strong>in</strong>es consumption.Sett<strong>in</strong>g the RP at the level of the least expensive medic<strong>in</strong>e poses a barrier to market entry,especially when considered <strong>in</strong> comb<strong>in</strong>ation with low demand for generic medic<strong>in</strong>es. To facilitatemarket entry of generic medic<strong>in</strong>es, the RP needs to be set at a higher level (for <strong>in</strong>stance, price ofmost expensive generic medic<strong>in</strong>e). This should be seen as a short-term measure to start off theItalian generic medic<strong>in</strong>es market. Once it reaches a more mature level of development, themeasure can be resc<strong>in</strong>ded and the RP can be set at the average price level of generic medic<strong>in</strong>es<strong>in</strong> the reference group or at a lower price level.It is imperative that measures are taken to boost demand for generic medic<strong>in</strong>es by physicians,pharmacists and patients. Policy needs to focus on physician prescrib<strong>in</strong>g attitudes and <strong>in</strong>troducef<strong>in</strong>ancial and non-f<strong>in</strong>ancial <strong>in</strong>centives for physicians to prescribe generic medic<strong>in</strong>es. The currentf<strong>in</strong>ancial <strong>in</strong>centive for pharmacists to dispense orig<strong>in</strong>ator medic<strong>in</strong>es needs to be removed.Exemption from co-payment on generic medic<strong>in</strong>es may be considered to augment patientdemand.14.2.7 Netherlands<strong>Generic</strong> substitution and competition between generic medic<strong>in</strong>es companies through discounts topharmacists drive demand for generic medic<strong>in</strong>es and are key features underly<strong>in</strong>g the success ofthe Dutch generic medic<strong>in</strong>es market. Discounts are seen by the Government as a way ofremunerat<strong>in</strong>g pharmacists. To recoup the rema<strong>in</strong>der of discounts, a claw-back mechanism was<strong>in</strong>troduced. This system requires government <strong>in</strong>tervention, <strong>in</strong>curs an adm<strong>in</strong>istrative cost, and isunlikely to be as efficient as a system where pharmaceutical companies compete on the basis ofprices.In order to re<strong>in</strong>force market transparency, the practice of discount<strong>in</strong>g should be outlawed <strong>in</strong>favour of a system where generic medic<strong>in</strong>es companies compete with each other on price. Sucha system would create a competitive generic medic<strong>in</strong>es market where prices paid by health<strong>in</strong>surance funds reflect best value for money from an efficiency perspective. Pharmacists wouldstill have an <strong>in</strong>centive to dispense cheap medic<strong>in</strong>es as they are able to reta<strong>in</strong> one third of theprice difference between the RP and the price of the medic<strong>in</strong>e dispensed. In addition to this, the
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 82fixed dispens<strong>in</strong>g fee per prescription could be augmented to compensate pharmacists for thef<strong>in</strong>ancial loss as a result of bann<strong>in</strong>g discounts.14.2.8 PolandThe Polish generic medic<strong>in</strong>es market is a mature market where the establishment of the RP atthe level of the cheapest generic medic<strong>in</strong>e promotes price competition between genericmedic<strong>in</strong>es companies. Even though price competition is occurr<strong>in</strong>g, there appears to be somescope for pharmaceutical companies to award discounts to pharmacists. Bann<strong>in</strong>g the practice ofdiscount<strong>in</strong>g would provide an added stimulus for price competition, <strong>in</strong>crease market transparency,and stimulate patient demand for generic medic<strong>in</strong>es.Physicians face no <strong>in</strong>centives to prescribe generic medic<strong>in</strong>es. To susta<strong>in</strong> demand for genericmedic<strong>in</strong>es, consideration could be given to <strong>in</strong>troduc<strong>in</strong>g budgetary <strong>in</strong>centives for physicians andassistance <strong>in</strong> generic prescrib<strong>in</strong>g through electronic prescrib<strong>in</strong>g systems, medic<strong>in</strong>e databases,audit of and feedback on prescrib<strong>in</strong>g data, prescrib<strong>in</strong>g guidel<strong>in</strong>es and formularies, andsubstitution lists. The f<strong>in</strong>ancial dis<strong>in</strong>centive for pharmacists to dispense generic medic<strong>in</strong>es needsto be removed.14.2.9 PortugalIn Portugal, regulation impos<strong>in</strong>g a m<strong>in</strong>imum price difference between generic and orig<strong>in</strong>atormedic<strong>in</strong>es needs to be abandoned. Free generic medic<strong>in</strong>e pric<strong>in</strong>g would stimulate companies to<strong>in</strong>troduce generic medic<strong>in</strong>es for less expensive active substances. Also, sett<strong>in</strong>g the RP at theaverage price level of generic medic<strong>in</strong>es <strong>in</strong> the reference group or at a lower price level, <strong>in</strong>steadof the most expensive, generic medic<strong>in</strong>e could be envisaged to <strong>in</strong>crease price competitionbetween generic medic<strong>in</strong>es companies, raise demand for generic medic<strong>in</strong>es, and reducepharmaceutical expenditure.Demand for generic medic<strong>in</strong>es has been driven by policy measures encourag<strong>in</strong>g INN prescrib<strong>in</strong>gby physicians and by requir<strong>in</strong>g pharmacists to dispense the cheapest generic medic<strong>in</strong>e whenphysicians prescribe by INN. INN prescrib<strong>in</strong>g can be supported by expand<strong>in</strong>g a project pilot<strong>in</strong>g amedic<strong>in</strong>es database and computerised prescrib<strong>in</strong>g. INFARMED could play a role <strong>in</strong> conv<strong>in</strong>c<strong>in</strong>gphysicians of the substitutability of generic and orig<strong>in</strong>ator medic<strong>in</strong>es, thereby <strong>in</strong>fluenc<strong>in</strong>g the rateof prescription items for which physicians permit or forbid substitution. The f<strong>in</strong>ancial dis<strong>in</strong>centivefor pharmacists to dispense generic medic<strong>in</strong>es needs to be removed.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 8314.2.10 Spa<strong>in</strong>Spanish generic medic<strong>in</strong>es policy tends to be a pric<strong>in</strong>g policy <strong>in</strong>cit<strong>in</strong>g companies of orig<strong>in</strong>ator andgeneric medic<strong>in</strong>es to reduce their prices to the level of the RP which is set close to marg<strong>in</strong>alcosts. In a context where generic and orig<strong>in</strong>ator medic<strong>in</strong>es have similar price levels, patients arelikely to prefer orig<strong>in</strong>ator medic<strong>in</strong>es out of brand loyalty and demand for generic medic<strong>in</strong>es isstifled.The Spanish generic medic<strong>in</strong>es market needs to be developed by boost<strong>in</strong>g demand. There is aneed to implement <strong>in</strong>centives that support physician and pharmacist demand for genericmedic<strong>in</strong>es. Medical students need to be taught to prescribe by INN and INN prescrib<strong>in</strong>g needs tobe compulsory. If the prescription is by INN, pharmacists should be required to dispense thecheapest medic<strong>in</strong>e. Such a system would support price competition between generic andorig<strong>in</strong>ator medic<strong>in</strong>e companies. The f<strong>in</strong>ancial dis<strong>in</strong>centive for pharmacists to dispense genericmedic<strong>in</strong>es needs to be abolished.14.2.11 United K<strong>in</strong>gdomThe United K<strong>in</strong>gdom has implemented a coherent generic medic<strong>in</strong>es policy that <strong>in</strong>cites allrelevant stakeholders to promote generic medic<strong>in</strong>es use. Supply-side measures relat<strong>in</strong>g to pric<strong>in</strong>gand reimbursement have created conditions for a generic medic<strong>in</strong>es market where companiescompete on price and the NHS maximises the cost-sav<strong>in</strong>g potential of generic medic<strong>in</strong>es.Demand for generic medic<strong>in</strong>es has been susta<strong>in</strong>ed by f<strong>in</strong>ancial and non-f<strong>in</strong>ancial <strong>in</strong>centives forphysicians. The proportion of INN prescription items has steadily <strong>in</strong>creased over time, althoughthere appears to be scope to further raise this percentage by means of electronic prescrib<strong>in</strong>gsystems, <strong>in</strong>centive schemes with<strong>in</strong> primary care trusts, prescrib<strong>in</strong>g guidel<strong>in</strong>es and formularies.Pharmacists have a f<strong>in</strong>ancial <strong>in</strong>centive to dispense generic medic<strong>in</strong>es when physicians prescribeby INN, although this <strong>in</strong>centive has been attenuated recently by the 2005 reimbursement scheme.Patients have no <strong>in</strong>centive to demand generic medic<strong>in</strong>es. Initiatives could be launched that <strong>in</strong>formpatients of the existence of a generic equivalent and aim to <strong>in</strong>fluence consumption patterns.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 84PART VSAVINGS FROM GENERIC MEDICINES USE
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 8515 Potential sav<strong>in</strong>gs from generic substitutionTo underl<strong>in</strong>e the need for develop<strong>in</strong>g generic medic<strong>in</strong>es markets, an exercise was conductedquantify<strong>in</strong>g the potential sav<strong>in</strong>gs from <strong>in</strong>creased substitution of generic for orig<strong>in</strong>ator medic<strong>in</strong>es <strong>in</strong>a number of countries for which data were available <strong>in</strong> 2004.Focus<strong>in</strong>g on the off-patent market, the top 10 active substances were selected by expenditure oforig<strong>in</strong>ator medic<strong>in</strong>es <strong>in</strong> 2004. As these active substances have the highest expenditure oforig<strong>in</strong>ator medic<strong>in</strong>es, they would be expected to generate the largest potential sav<strong>in</strong>gs fromgeneric substitution. This exercise calculates the sav<strong>in</strong>gs that can be made if orig<strong>in</strong>ator medic<strong>in</strong>esfor the top 10 active substances are replaced by generic medic<strong>in</strong>es. There is no country thatatta<strong>in</strong>s a 100% generic substitution rate <strong>in</strong> the off-patent market. Therefore, our analysis assumedthat, follow<strong>in</strong>g generic substitution, 5% of market volume for each active substance would bemade up by orig<strong>in</strong>ator medic<strong>in</strong>es and 95% by generic medic<strong>in</strong>es. Hence, the term “<strong>in</strong>creased”generic substitution is used.Annual sav<strong>in</strong>gs from generic substitution were obta<strong>in</strong>ed by calculat<strong>in</strong>g the average price level forthe group of orig<strong>in</strong>ator medic<strong>in</strong>es and for the group of generic medic<strong>in</strong>es. The price differencebetween orig<strong>in</strong>ator and generic medic<strong>in</strong>es was then multiplied by the volume of orig<strong>in</strong>atormedic<strong>in</strong>es to be substituted. The follow<strong>in</strong>g equation was used to calculate sav<strong>in</strong>gs from genericsubstitution:Annual sav<strong>in</strong>gs = (average price of orig<strong>in</strong>ator medic<strong>in</strong>es – average price of generic medic<strong>in</strong>es) x(volume of orig<strong>in</strong>ator medic<strong>in</strong>es – 0.05 x (volume of orig<strong>in</strong>ator and generic medic<strong>in</strong>es))It is important to stress that this exercise is carried out for illustrative purposes and does not claimto generate an exact estimate of sav<strong>in</strong>gs from generic substitution. Also, generic medic<strong>in</strong>esmarkets evolve rapidly so that, even though the most recent data relat<strong>in</strong>g to 2004 were used, thedata may no longer reflect the market situation. One additional limitation of the analysis needs tobe noted. An active substance may conta<strong>in</strong> medic<strong>in</strong>es <strong>in</strong> different forms, strengths and packagesizes. Our analysis did not account for differences <strong>in</strong> form, strength or package size between<strong>in</strong>dividual products, but substituted generic for orig<strong>in</strong>ator medic<strong>in</strong>es at aggregate level.Figures 20 to 30 show the top 10 active substances for a country, public expenditure on orig<strong>in</strong>atormedic<strong>in</strong>es with that active substance, sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> absoluteterms and as a proportion of expenditure on orig<strong>in</strong>ator medic<strong>in</strong>es. These Figures <strong>in</strong>dicate that<strong>in</strong>creased substitution of generic for orig<strong>in</strong>ator medic<strong>in</strong>es can yield substantial sav<strong>in</strong>gs. For the
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 86top 10 active substances by expenditure of orig<strong>in</strong>ator medic<strong>in</strong>es, generic substitution wouldreduce public expenditure on the orig<strong>in</strong>ator medic<strong>in</strong>es conta<strong>in</strong><strong>in</strong>g these active substances by atleast 20% <strong>in</strong> selected countries, with the proportional reduction vary<strong>in</strong>g between 21% <strong>in</strong> Polandand 48% <strong>in</strong> Denmark.15.1 AustriaFigure 20. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> Austria, 2004Active substancePublic expenditure onorig<strong>in</strong>ator medic<strong>in</strong>es(€)Sav<strong>in</strong>gs from genericsubstitution(€)1. Lis<strong>in</strong>opril 33,545,548 7,973,2472. Ramipril 26,715,264 11,717,7703. Ciclospor<strong>in</strong> 22,456,438 3,545,5054. Amlodip<strong>in</strong>e 22,379,694 3,701,2595. Metoprolol 22,017,335 9,580,5706. Carvedilol 21,043,749 2,998,0967. Pravastat<strong>in</strong> 19,565,709 5,364,8508. Lamotrig<strong>in</strong>e 17,006,227 5,539,1109. Enalapril 16,588,539 2,183,51710. Omeprazole 16,292,170 5,358,914Total 217,610,673 57,962,838 (27%)15.2 BelgiumFigure 21. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> Belgium, 2004Active substancePublic expenditure onorig<strong>in</strong>ator medic<strong>in</strong>es(€)Sav<strong>in</strong>gs from genericsubstitution(€)1. Pravastat<strong>in</strong> 67,863,755 45,053,0832. Simvastat<strong>in</strong> 64,440,658 22,766,9413. Paroxet<strong>in</strong>e 50,898,729 25,860,1044. Amoxicill<strong>in</strong> 39,097,970 10,130,9495. Bisoprolol 35,277,554 10,521,5946. Fluconazole 29,793,234 9,688,8547. Lis<strong>in</strong>opril 27,124,437 9,290,2598. Hydrochlorothiazide 25,613,208 13,723,9629. Tramadol 24,274,928 4,758,12710. Domperidone 20,534,051 8,990,262Total 384,918,524 160,784,134 (42%)
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 8715.3 DenmarkFigure 22. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> Denmark, 2004Active substancePublic expenditure onorig<strong>in</strong>ator medic<strong>in</strong>es(€)Sav<strong>in</strong>gs from genericsubstitution(€)1. Metoprolol 19,289,107 4,833,8612. Eth<strong>in</strong>ylestradiol 16,955,876 9,630,1743. Citalopram 16,500,176 6,177,4734. Fentanyl 15,974,500 13,323,8415. Amlodip<strong>in</strong>e 14,821,236 10,932,9136. Mirtazap<strong>in</strong>e 10,151,964 5,266,1047. Interferon beta 1a 9,731,771 4,058,2378. Sertral<strong>in</strong>e 8,305,894 763,2449. Ciprofloxac<strong>in</strong> 7,139,290 4,039,86610. Gestodene 6,399,640 1,165,579Total 125,269,454 60,191,292 (48%)Note: Data relate to both hospital and retail pharmacy.15.4 FranceFigure 23. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> France, 2004Active substancePublic expenditure onorig<strong>in</strong>ator medic<strong>in</strong>es(€)Sav<strong>in</strong>gs from genericsubstitution(€)1. Omeprazole 446,515,016 117,723,0862. Paracetamol 145,522,610 23,838,8833. Paroxet<strong>in</strong>e 137,898,121 45,042,8994. Eth<strong>in</strong>ylestradiol 137,520,042 101,370,6875. Bisoprolol 135,870,312 60,368,1566. Hydrochlorothiazide 115,174,757 41,624,7597. Citalopram 101,443,283 38,817,1978. Trimetazid<strong>in</strong>e 100,035,279 35,760,8219. Fenofibrate 97,599,601 38,537,64310. Gliclazide 92,798,116 22,206,603Total 1,510,377,137 525,290,734 (35%)
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 8815.5 GermanyFigure 24. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> Germany, 2004Active substancePublic expenditure onorig<strong>in</strong>ator medic<strong>in</strong>es(€)Sav<strong>in</strong>gs from genericsubstitution(€)1. Hydrochlorothiazide 743,868,532 481,855,4042. Fentanyl 357,910,602 231,209,6703. Ramipril 209,363,878 78,004,9984. Metoprolol 193,642,730 90,953,8465. Ciclospor<strong>in</strong> 126,479,271 82,1896. Pravastat<strong>in</strong> 111,223,448 32,111,3327. Carvedilol 98,232,964 44,951,1768. Formoterol 93,867,715 9,722,2549. Mirtazap<strong>in</strong>e 93,308,038 18,744,55710. Budesonide 70,218,590 4,868,830Total 2,098,115,768 992,504,255 (47%)15.6 ItalyFigure 25. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> Italy, 2004Active substancePublic expenditure onorig<strong>in</strong>ator medic<strong>in</strong>es(€)Sav<strong>in</strong>gs from genericsubstitution(€)1. Ceftriaxone 125,640,866 48,480,1742. Citalopram 100,430,819 50,486,8893. Lorazepam 98,028,700 38,695,6384. Carvedilol 82,540,290 24,387,4745. Alprazolam 79,877,958 23,171,1576. Paroxet<strong>in</strong>e 78,529,774 1,616,6457. Nimesulide 76,111,366 29,513,7688. Gentamic<strong>in</strong> 76,028,312 12,857,4759. Bromazepam 65,943,659 14,886,73810. Gabapent<strong>in</strong> 61,822,545 19,412,604Total 844,954,289 263,508,563 (31%)
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 8915.7 NetherlandsFigure 26. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> the Netherlands, 2004Active substancePublic expenditure onorig<strong>in</strong>ator medic<strong>in</strong>es(€)Sav<strong>in</strong>gs from genericsubstitution(€)1. Pravastat<strong>in</strong> 67,314,038 29,605,9182. Fluticasone 67,306,151 5,329,6353. Omeprazole 56,793,271 28,253,1504. Budesonide 38,842,590 24,000,8065. Fentanyl 31,043,301 27,339,0176. Paroxet<strong>in</strong>e 21,299,697 5,544,0487. Itraconazole 20,180,460 905,8928. Mirtazap<strong>in</strong>e 20,167,057 8,238,8069. Gabapent<strong>in</strong> 19,244,761 8,265,27010. Salbutamol 18,034,798 9,078,160Total 360,226,124 146,560,702 (41%)15.8 PolandFigure 27. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> Poland, 2004Active substancePublic expenditure onorig<strong>in</strong>ator medic<strong>in</strong>es(€)Sav<strong>in</strong>gs from genericsubstitution(€)1. Simvastat<strong>in</strong> 10,088,853 623,5002. Gliclazide 8,145,560 304,8413. Azithromyc<strong>in</strong> 7,756,479 84,4584. Amoxicill<strong>in</strong> 6,232,929 811,8005. Donepezil 6,028,764 3,012,7836. Budesonide 6,317,025 3,855,4957. Atorvastat<strong>in</strong> 4,990,985 2,000,7058. Cetiriz<strong>in</strong>e 4,646,962 484,645Total 54,207,557 11,178,228 (21%)
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 9015.9 PortugalFigure 28. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> Portugal, 2004Active substancePublic expenditure onorig<strong>in</strong>ator medic<strong>in</strong>es(€)Sav<strong>in</strong>gs from genericsubstitution(€)1. Eth<strong>in</strong>ylestradiol 47,817,774 40,705,2112. Hydrochlorothiazide 37,685,108 7,691,8303. Nimesulide 30,030,728 19,016,3504. Lis<strong>in</strong>opril 26,747,517 9,446,7555. Trimetazid<strong>in</strong>e 25,518,526 8,540,0416. Pravastat<strong>in</strong> 23,891,425 10,132,4287. Diclofenac 23,483,241 6,858,1298. Ramipril 22,675,143 3,584,0409. Sertral<strong>in</strong>e 21,653,772 7,916,84510. Amoxicill<strong>in</strong> 21,145,870 3,909,730Total 280,649,104 117,801,359 (42%)15.10 Spa<strong>in</strong>Figure 29. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> Spa<strong>in</strong>, 2004Active substancePublic expenditure onorig<strong>in</strong>ator medic<strong>in</strong>es(€)Sav<strong>in</strong>gs from genericsubstitution(€)1. Paroxet<strong>in</strong>e 132,429,541 29,471,7522. Sertral<strong>in</strong>e 129,299,355 40,615,2603. Lansoprazole 110,407,204 32,498,5774. Amoxicill<strong>in</strong> 97,950,628 31,451,2005. Gabapent<strong>in</strong> 82,137,404 31,228,2696. Ibuprofen 76,860,517 27,478,0847. Pravastat<strong>in</strong> 76,281,565 22,670,8668. Doxazos<strong>in</strong> 74,941,029 33,637,2179. Citalopram 72,419,900 14,683,57210. Budesonide 64,183,290 38,005,375Total 916,910,433 301,740,171 (33%)
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 9115.11 United K<strong>in</strong>gdomFigure 30. Potential sav<strong>in</strong>gs from <strong>in</strong>creased generic substitution <strong>in</strong> United K<strong>in</strong>gdom, 2004Active substancePublic expenditure onorig<strong>in</strong>ator medic<strong>in</strong>es(€)Sav<strong>in</strong>gs from genericsubstitution(€)1. Pravastat<strong>in</strong> 173,926,201 1,827,3212. Doxazos<strong>in</strong> 167,861,096 120,582,8783. Beclometasone 141,198,568 8,721,0024. Simvastat<strong>in</strong> 130,721,082 36,535,8105. Nifedip<strong>in</strong>e 93,826,729 40,906,0976. Budesonide 88,848,854 30,632,5317. Omeprazole 79,995,288 28,369,7918. Fentanyl 73,644,518 67,750,1889. Gabapent<strong>in</strong> 60,788,304 1,526,22210. Paroxet<strong>in</strong>e 59,976,234 12,993,094Total 1,070,786,874 349,844,935 (33%)
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 92PART VIANNEXES
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 9316 AcknowledgementsF<strong>in</strong>ancial support for this research project was received from the <strong>Europe</strong>an <strong>Generic</strong> <strong>Medic<strong>in</strong>es</strong>Association. The authors would like to express their gratitude to Ana Wisse Teixeira for giv<strong>in</strong>gaccess to pric<strong>in</strong>g and reimbursement surveys of the <strong>Europe</strong>an <strong>Generic</strong> <strong>Medic<strong>in</strong>es</strong> Associationand for her assistance <strong>in</strong> analys<strong>in</strong>g IMS Health data. The authors are also <strong>in</strong>debted torepresentatives of the EGA Healthcare Economics Committee, national generic medic<strong>in</strong>esassociations, M<strong>in</strong>istries of Health and National <strong>Medic<strong>in</strong>es</strong> Agencies for provid<strong>in</strong>g and validat<strong>in</strong>g<strong>in</strong>formation about generic medic<strong>in</strong>es policy <strong>in</strong> their country.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 9417 AbbreviationsATCEGAEUGPINNNHSOECDRPRPSAnatomical Therapeutic Chemical classification system for drugs<strong>Europe</strong>an <strong>Generic</strong> <strong>Medic<strong>in</strong>es</strong> Association<strong>Europe</strong>an UnionGeneral PractitionerInternational Non-proprietary NameNational Health ServiceOrganisation for Economic Co-operation and DevelopmentReference PriceReference-Pric<strong>in</strong>g System
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 9518 GlossaryActive substance: that component of a medic<strong>in</strong>e that gives it its therapeutic effect.ATC classification: a standard for classify<strong>in</strong>g drugs <strong>in</strong>to different groups accord<strong>in</strong>g to the organor system on which they act and their chemical, pharmacological and therapeutic properties.Bio-availability: the amount of an active substance that is absorbed by the organism and thespeed at which this occurs when <strong>in</strong>troduced <strong>in</strong> a given dosage form.Bio-equivalence: bio-equivalent medic<strong>in</strong>es conta<strong>in</strong> the same amount of active substance andhave the same bio-availability when adm<strong>in</strong>istered <strong>in</strong> equal doses under equal conditions.Copy: an off-patent medic<strong>in</strong>e that is neither an orig<strong>in</strong>ator medic<strong>in</strong>e, nor a licensed medic<strong>in</strong>e, nora generic medic<strong>in</strong>e through the Abridged Procedure and has, for example, been approvedthrough the Well-Established Use Procedure. For a copy, bio-equivalence with the orig<strong>in</strong>atormedic<strong>in</strong>e has not been approved.Data exclusivity: the period of time dur<strong>in</strong>g which the application for market<strong>in</strong>g authorisation of ageneric medic<strong>in</strong>e cannot refer to the pre-cl<strong>in</strong>ical and cl<strong>in</strong>ical documentation of the orig<strong>in</strong>atormedic<strong>in</strong>e.Def<strong>in</strong>ed daily dose: the assumed average daily dose of a medic<strong>in</strong>e needed to treat its ma<strong>in</strong><strong>in</strong>dication <strong>in</strong> an adult person weigh<strong>in</strong>g 70 kg.Dosage: amount of a medic<strong>in</strong>e that is adm<strong>in</strong>istered to a patient.<strong>Generic</strong> medic<strong>in</strong>e: a medic<strong>in</strong>al product that has the same qualitative and quantitativecomposition <strong>in</strong> active substances and the same pharmaceutical form as the reference medic<strong>in</strong>alproduct, and whose bio-equivalence with the reference medic<strong>in</strong>al product has been demonstratedby appropriate bio-availability studies (Directive 2004/27/EC). A generic medic<strong>in</strong>e is approvedthrough the Abridged Procedure and marketed by a company other than the orig<strong>in</strong>ator medic<strong>in</strong>ecompany.<strong>Generic</strong> substitution: procedure by which a physician prescribes a specific medic<strong>in</strong>e, but thepharmacist replaces it by a generic medic<strong>in</strong>e that has the same active substance and bioavailabilityas the medic<strong>in</strong>e that is prescribed.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 96International non-proprietary name: a s<strong>in</strong>gle name awarded by the World Health Organizationfor each active substance that is marketed as a medic<strong>in</strong>e. This name identifies the activesubstance rather than the f<strong>in</strong>al product which can be sold under different brand names.Licensed medic<strong>in</strong>e: medic<strong>in</strong>e with the same active substance as the orig<strong>in</strong>ator medic<strong>in</strong>e thathas an official licens<strong>in</strong>g, distribution or co-market<strong>in</strong>g agreement with the orig<strong>in</strong>ator medic<strong>in</strong>ecompany.Orig<strong>in</strong>ator medic<strong>in</strong>e: the first version of a medic<strong>in</strong>e developed and patented by an orig<strong>in</strong>atorpharmaceutical company which receives exclusive rights to market<strong>in</strong>g the medic<strong>in</strong>e <strong>in</strong> the<strong>Europe</strong>an Union for 15 years.Patent: a document grant<strong>in</strong>g a company exclusive rights to exploit a new medic<strong>in</strong>e for a givenperiod of time. The patent prohibits others from sell<strong>in</strong>g this medic<strong>in</strong>e without the permission of thecompany <strong>in</strong> the territory where the patent was issued.Pharmaceutical form: the physical form <strong>in</strong> which a medic<strong>in</strong>e is taken by patients as determ<strong>in</strong>edby its route of adm<strong>in</strong>istration. Pharmaceutical forms <strong>in</strong>clude tablets, capsules, <strong>in</strong>jectables andliquids.Reference-pric<strong>in</strong>g system: a system that establishes a reimbursement level or reference pricefor a group of <strong>in</strong>terchangeable medic<strong>in</strong>es. If a medic<strong>in</strong>e is priced above the reference price, thepatient pays the difference between the price of the medic<strong>in</strong>e and the reference price.Equivalence between medic<strong>in</strong>es can be def<strong>in</strong>ed at three levels: 1) by active substance, i.e.medic<strong>in</strong>es with the same active substance; 2) by pharmacological class, i.e. medic<strong>in</strong>es withchemically-related active substances that are pharmacologically equivalent; 3) by therapeuticclass, i.e. medic<strong>in</strong>es that have a comparable therapeutic effect.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 9719 BibliographyAccenture. Die Bedeutung der Generika<strong>in</strong>dustrie für die Gesundheitsversorgung <strong>in</strong> Deutschland(The importance of the generic medic<strong>in</strong>es <strong>in</strong>dustry for the German health care system).Accenture, 2005.Antonanzas F. Challenges to achiev<strong>in</strong>g value <strong>in</strong> medic<strong>in</strong>e spend<strong>in</strong>g <strong>in</strong> a decentralized country:the Spanish case. Value <strong>in</strong> Health 2003, vol. 6, suppl. 1, p. S52-S63.Blachier C., Kanavos P. France – pharmaceutical pric<strong>in</strong>g and reimbursement. <strong>Europe</strong>anCommission, Enterprise and Industry DG, Directorate F – Consumer goods, 2005.(http://pharmacos.eudra.org/g10/docs/tse/France.pdf).Brouwer W.B.F., Rutten F.F.H. Golden pill for pharmacists: generic prescription is barely costsav<strong>in</strong>g.Medical Contact 2002, vol. 57, p. 737-740.Burstall M.L. The management of the cost and utilization of pharmaceuticals <strong>in</strong> the UnitedK<strong>in</strong>gdom. Health Policy 1997, vol. 41, p. S27-S43.Busse R., Riesberg A. Health care systems <strong>in</strong> transition: Germany. WHO Regional Office for<strong>Europe</strong> on behalf of the <strong>Europe</strong>an Observatory on Health Systems and Policies: Copenhagen,2004.Cambridge Pharma Consultancy. Delays to market access <strong>in</strong> <strong>Europe</strong>. Cambridge PharmaConsultancy: Cambridge, 2002.(http://www.efpia.org/2_<strong>in</strong>dust/CambridgePharmaConsultancy1102.pdf)Danish Medic<strong>in</strong>e Agency. The use of ‘not S’ <strong>in</strong> 2005. Danish <strong>Medic<strong>in</strong>es</strong> Agency: Copenhagen,2006.Danzon P.M. Reference pric<strong>in</strong>g: theory and evidence. University of Pennsylvania: Philadelphia,2001.Danzon P.M., Ketcham J.D. Reference pric<strong>in</strong>g of pharmaceuticals for Medicare: evidence fromGermany, the Netherlands and New Zealand. NBER Work<strong>in</strong>g Paper no. 10007. National Bureauof Economic Research: Cambridge, 2003.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 98de Joncheere K., Rietveld A.H., Hutt<strong>in</strong> C. Experiences with generics. International Journal of Riskand Safety <strong>in</strong> Medic<strong>in</strong>e 2002, vol. 15, p. 101-109.Directive 1989/105/EEC of 21 December 1988 relat<strong>in</strong>g to the transparency of measuresregulat<strong>in</strong>g the pric<strong>in</strong>g of medic<strong>in</strong>al products for human use and their <strong>in</strong>clusion <strong>in</strong> the scope ofnational health <strong>in</strong>surance systems. Official Journal of the <strong>Europe</strong>an Union L40 of 11 February1989, p. 8-11.Directive 2004/27/EC of the <strong>Europe</strong>an Parliament and of the Council of 31 st March 2004amend<strong>in</strong>g Directive 2001/83/EC on the Community code relat<strong>in</strong>g to medic<strong>in</strong>al products for humanuse. Official Journal of the <strong>Europe</strong>an Union L 136/34-57.Durieux P., Chaix-Couturier C., Durand-Zaleski I., Ravaud P. From cl<strong>in</strong>ical recommendations tomandatory practice. International Journal of Technology Assessment <strong>in</strong> Health Care 2000, vol.16, no. 4, p. 969-975.Ess S.M., Schneeweiss S., Szucs T.D. <strong>Europe</strong>an healthcare policies for controll<strong>in</strong>g medic<strong>in</strong>eexpenditure. Pharmacoeconomics 2003, vol. 21, no. 2, p. 89-103.<strong>Europe</strong> Economics. Access to important new medic<strong>in</strong>es: where and why do patients wait? <strong>Europe</strong>Economics: London, 1998. (http://www.eer.co.uk)<strong>Europe</strong>an Commission. Innovation <strong>in</strong> the pharmaceutical sector. A study undertaken for the<strong>Europe</strong>an Commission by Charles River Associates. Brussels, 2004.(http://pharmacos.eudra.org/F2/pharmacos/docs/Doc2004/nov/EU%20Pharma%20Innovation_25-11-04.pdf)<strong>Europe</strong>an <strong>Generic</strong> <strong>Medic<strong>in</strong>es</strong> Association. 2005 market review. The <strong>Europe</strong>an genericpharmaceutical markets. <strong>Europe</strong>an <strong>Generic</strong> <strong>Medic<strong>in</strong>es</strong> Association: Brussels, 2005. Unpublisheddocument.<strong>Europe</strong>an <strong>Generic</strong> <strong>Medic<strong>in</strong>es</strong> Association. 2006 market review. The <strong>Europe</strong>an genericpharmaceutical markets. <strong>Europe</strong>an <strong>Generic</strong> <strong>Medic<strong>in</strong>es</strong> Association: Brussels, 2006. In press.G10 High Level Group on Innovation and Provision of <strong>Medic<strong>in</strong>es</strong> <strong>in</strong> the <strong>Europe</strong>an Union.Recommendations for action. <strong>Europe</strong>an Commission: Brussels, 2002.(http://europa.eu.<strong>in</strong>t/comm/health/ph_overview/Documents/key08_en.pdf).
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 99Ghislandi S., Krulichova I., Garatt<strong>in</strong>i L. Pharmaceutical policy <strong>in</strong> Italy: towards a structuralchange? Health Policy 2005, vol. 72, p. 53-63.Gosden T., Torgerson D.J. The effect of fundhold<strong>in</strong>g on prescrib<strong>in</strong>g and referral costs: a review ofthe literature. Health Policy 1997, vol. 40, p. 103-114.Health and Social Care Information Centre. Prescriptions dispensed <strong>in</strong> the community. Statisticsfor 1994 to 2004: England. Health and Social Care Information Centre: Leeds, 2005.(http://www.dh.gov.uk/assetRoot/04/11/58/87/04115887.pdf).IMS Health. Midas database. IMS Health: London, 2004.INFARMED. Newsletter no. 19. INFARMED: Lisbon, 2006.(http://www.<strong>in</strong>farmed.pt/<strong>in</strong>farmed_noticias/<strong>in</strong>farmed_noticias_01_02_2006.pdf)Kay A., Ba<strong>in</strong>es D. The rapid <strong>in</strong>crease <strong>in</strong> generic prices <strong>in</strong> the UK: a failure of competition orregulation? Public Money and Management 2000, vol. 20, no. 3, p. 35-38.K<strong>in</strong>g D.R., Kanavos P. Encourag<strong>in</strong>g the use of generic medic<strong>in</strong>es: implications for transitioneconomies. Croatian Medical Journal 2002, vol. 43, no. 4, p. 462-469.Koopmanschap M.A., Rutten F.F.H. The medic<strong>in</strong>e budget silo mentality: the Dutch case. Value <strong>in</strong>Health 2003, vol. 6, suppl. 1, p. S46-S51.Krumschmidt R. Analysis of the pharmacy market <strong>in</strong>clud<strong>in</strong>g breakdown <strong>in</strong>to domestic and foreigndrugs. Drugs Market 2006.Le Pen C. The medic<strong>in</strong>e budget silo mentality: the French case. Value <strong>in</strong> Health 2003, vol. 6,suppl. 1, p. S10-S19.Le Pen C. Substitution générique et prescription dans le répertoire (<strong>Generic</strong> substitution andprescrib<strong>in</strong>g practices <strong>in</strong> the off-patent market). University of Paris-Dauph<strong>in</strong>e: Paris, 2005.Lopez-Casasnovas G., Puig-Junoy J. Review of the literature on reference pric<strong>in</strong>g. Health Policy2000, vol. 54, p. 87-123.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 100Lucioni C. Quale futuro per I prodotti generici <strong>in</strong> Italia? (What future awaits generic medic<strong>in</strong>es <strong>in</strong>Italy?) Farmeconomia 1995, vol. 2, p. 12-18.Mapelli V., Lucioni C. Spend<strong>in</strong>g on pharmaceuticals <strong>in</strong> Italy: macro constra<strong>in</strong>ts with localautonomy. Value <strong>in</strong> Health 2003, vol. 6, suppl. 1, p. S31-S45.Medical Insurance. <strong>Generic</strong> medic<strong>in</strong>es: Medical Insurance will contact <strong>in</strong>sured patients directly.Press release 8 th September 2005. (http://www.ameli.fr).Mrazek M.F. Comparative approaches to pharmaceutical price regulation <strong>in</strong> the <strong>Europe</strong>an Union.Croatian Medical Journal 2002, vol. 43, no. 4, p. 453-461.Mutualité Française. Baromètre de la prescription en DCI en France (Barometer of INNprescrib<strong>in</strong>g <strong>in</strong> France). Mutualité Française, 2006.(http://www.mutualite.fr/web/frameset.nsf/Mutuelles/<strong>in</strong>fosante_medic_BarometrePrescription?).OECD. Health at a glance: OECD <strong>in</strong>dicators 2005. OECD: Paris, 2005.Or Z. Improv<strong>in</strong>g the performance of health care systems: from measures to action. A review ofexperiences <strong>in</strong> four OECD countries. Labour Market and Social Policy Occasional Papers SeriesNo. 57. OECD: Paris, 2002, 87 p.OsMed. Rapporto nazionale OsMed 2003. Italian M<strong>in</strong>istry of Health.(http://www.m<strong>in</strong>isterosalute.it/medic<strong>in</strong>ali/osmed).Peny JM. Barriers to substitution. Scrip Magaz<strong>in</strong>e 2005, April, p. 19-23.Pharmacos. Poland – health care, pharmaceutical pric<strong>in</strong>g and reimbursement. <strong>Europe</strong>anCommission, Enterprise and Industry DG, Directorate F – Consumer goods, 2005.(http://pharmacos.eudra.org/g10/docs/tse/Poland.pdf).Pharmig. Medication and health care <strong>in</strong> Austria: facts and figures 2000. Pharmig: Vienna, 2003.Puig-Junoy J. Medic<strong>in</strong>e price system <strong>in</strong> Spa<strong>in</strong>. Health Policy Monitor Survey No. 02/2003(http://www.healthpolicymonitor.org/<strong>in</strong>dex.jsp).
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 101Puig-Junoy J. Incentives and pharmaceutical reimbursement reforms <strong>in</strong> Spa<strong>in</strong>. Health Policy2004, vol. 67, p. 149-165.Purves I. PRODIGY <strong>in</strong>terim report. Department of Health: London, 1996, 13 p.Rovira J., Albarrac<strong>in</strong> G. The market for generic medic<strong>in</strong>es <strong>in</strong> Spa<strong>in</strong>. Current situation and futureprospects. Soikos: Barcelona, 2001, 77 p.Rovira J., Darba J. Pharmaceutical pric<strong>in</strong>g and reimbursement <strong>in</strong> Spa<strong>in</strong>. Health Economics <strong>in</strong>Prevention and Care 2001, vol. 2, no. 1, p. 39-43.Schoffski O. Consequences of implement<strong>in</strong>g a medic<strong>in</strong>e budget for office-based physicians <strong>in</strong>Germany. Pharmacoeconomics 1996, vol. 10, suppl. 2, p. 37-47.Schreyögg J., Henke K.D., Busse R. Manag<strong>in</strong>g pharmaceutical regulation <strong>in</strong> Germany - overviewand economic assessment. Discussion Paper 2004/6. Technical University of Berl<strong>in</strong>: Berl<strong>in</strong>, 2004.Schulz A. Evolv<strong>in</strong>g dynamics of US and <strong>Europe</strong>an generics markets. Journal of <strong>Generic</strong><strong>Medic<strong>in</strong>es</strong> 2004, vol. 2, no. 1, p. 23-32.Senior I., Bramley-Harker E., Lewis D., Baker S., Harl<strong>in</strong>g G. Manufacture, distribution andreimbursement of generic medic<strong>in</strong>es <strong>in</strong> the UK. National Economic Research Associates:London, 2000. Unpublished document.Simoens S., De Bruyn K., Bogaert M., Laekeman G. Pharmaceutical policy regard<strong>in</strong>g genericdrugs <strong>in</strong> Belgium. Pharmacoeconomics 2005, vol. 23, no. 8, p. 755-766.von der Schulenburg J.M.G. Management of cost and utilization of pharmaceuticals <strong>in</strong> Germany.Health Policy 1997, vol. 41, suppl. 1, p. S45-S53.Wilk<strong>in</strong> D., Coleman A., Dowl<strong>in</strong>g B., Smith K. The national Tracker survey of primary care groupsand trusts 2001/2002: tak<strong>in</strong>g responsibility? National Primary Care Research and DevelopmentCentre: Manchester and K<strong>in</strong>g’s Fund: London, 2002.Wilk<strong>in</strong> D., Gillam S., Coleman A. The national Tracker survey of primary care groups and trusts2000/2001: modernis<strong>in</strong>g the NHS? National Primary Care Research and Development Centre:Manchester and K<strong>in</strong>g’s Fund: London, 2001.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 102Wilk<strong>in</strong> D., Gillam S., Leese B. The national Tracker survey of primary care groups and trusts.Progress and challenges 1999 / 2000. National Primary Care Research and Development Centre:Manchester and K<strong>in</strong>g’s Fund: London, 1999.
<strong>Susta<strong>in</strong><strong>in</strong>g</strong> generic medic<strong>in</strong>es markets 103Rectorale dienstenDienst CommunicatieOude Markt 13BE-3000 Leuventel. + 32 16 32 40 10fax + 32 16 32 40 14pr@kuleuven.bewww.kuleuven.be/pr
<strong>Generic</strong> medic<strong>in</strong>es create major sav<strong>in</strong>gs for healthcare providers andstimulate <strong>in</strong>novation. However, the EU is not maximiz<strong>in</strong>g its fullpotential <strong>in</strong> generic medic<strong>in</strong>es. Added sav<strong>in</strong>gs of 27%-48% could beatta<strong>in</strong>ed if the appropriate measures were taken by EU countries.This study shows that coord<strong>in</strong>ated government policies are critically needed <strong>in</strong>many EU countries. Experience demonstrates that supply-side policies (such aspric<strong>in</strong>g reductions) need to be supplemented by demand-side policies (such as<strong>in</strong>centives for physicians, pharmacists and patients to use generic medic<strong>in</strong>es)to lead to a successful and susta<strong>in</strong>able generic medic<strong>in</strong>es market.The EU should now seek to foster and susta<strong>in</strong> its EU generic medic<strong>in</strong>es <strong>in</strong>dustry,which plays an important role <strong>in</strong> the overall competitiveness of the EUpharmaceutical <strong>in</strong>dustry.RESEARCH CENTRE FOR PHARMACEUTICAL CARE AND PHARMACO-ECONOMICSFaculty of Pharmaceutical Sciences I Katholieke Universiteit LeuvenOnderwijs en Navors<strong>in</strong>g 2, P.O. Box 521Herestraat 49 - 3000 Leuvenwww.kuleuven.be