Recommendations
ACC/AHA/SCAI PCI Guidelines - British Cardiovascular Intervention ...
ACC/AHA/SCAI PCI Guidelines - British Cardiovascular Intervention ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
46<br />
Smith et al. 2005<br />
ACC/AHA/SCAI Practice Guidelines<br />
ACC - www.acc.org<br />
AHA - www.americanheart.org<br />
SCAI - www.scai.org<br />
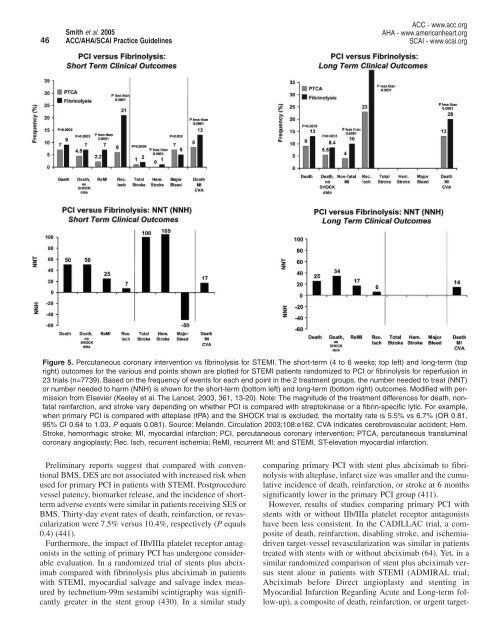
Figure 5. Percutaneous coronary intervention vs fibrinolysis for STEMI. The short-term (4 to 6 weeks; top left) and long-term (top<br />
right) outcomes for the various end points shown are plotted for STEMI patients randomized to PCI or fibrinolysis for reperfusion in<br />
23 trials (n=7739). Based on the frequency of events for each end point in the 2 treatment groups, the number needed to treat (NNT)<br />
or number needed to harm (NNH) is shown for the short-term (bottom left) and long-term (bottom right) outcomes. Modified with permission<br />
from Elsevier (Keeley et al. The Lancet, 2003, 361, 13-20). Note: The magnitude of the treatment differences for death, nonfatal<br />
reinfarction, and stroke vary depending on whether PCI is compared with streptokinase or a fibrin-specific lytic. For example,<br />
when primary PCI is compared with alteplase (tPA) and the SHOCK trial is excluded, the mortality rate is 5.5% vs 6.7% (OR 0.81,<br />
95% CI 0.64 to 1.03, P equals 0.081). Source: Melandri. Circulation 2003;108:e162. CVA indicates cerebrovascular accident; Hem.<br />
Stroke, hemorrhagic stroke; MI, myocardial infarction; PCI, percutaneous coronary intervention; PTCA, percutaneous transluminal<br />
coronary angioplasty; Rec. Isch, recurrent ischemia; ReMI, recurrent MI; and STEMI, ST-elevation myocardial infarction.<br />
Preliminary reports suggest that compared with conventional<br />
BMS, DES are not associated with increased risk when<br />
used for primary PCI in patients with STEMI. Postprocedure<br />
vessel patency, biomarker release, and the incidence of shortterm<br />
adverse events were similar in patients receiving SES or<br />
BMS. Thirty-day event rates of death, reinfarction, or revascularization<br />
were 7.5% versus 10.4%, respectively (P equals<br />
0.4) (441).<br />
Furthermore, the impact of IIb/IIIa platelet receptor antagonists<br />
in the setting of primary PCI has undergone considerable<br />
evaluation. In a randomized trial of stents plus abciximab<br />
compared with fibrinolysis plus abciximab in patients<br />
with STEMI, myocardial salvage and salvage index measured<br />
by technetium-99m sestamibi scintigraphy was significantly<br />
greater in the stent group (430). In a similar study<br />
comparing primary PCI with stent plus abciximab to fibrinolysis<br />
with alteplase, infarct size was smaller and the cumulative<br />
incidence of death, reinfarction, or stroke at 6 months<br />
significantly lower in the primary PCI group (411).<br />
However, results of studies comparing primary PCI with<br />
stents with or without IIb/IIIa platelet receptor antagonists<br />
have been less consistent. In the CADILLAC trial, a composite<br />
of death, reinfarction, disabling stroke, and ischemiadriven<br />
target-vessel revascularization was similar in patients<br />
treated with stents with or without abciximab (64). Yet, in a<br />
similar randomized comparison of stent plus abciximab versus<br />
stent alone in patients with STEMI (ADMIRAL trial;<br />
Abciximab before Direct angioplasty and stenting in<br />
Myocardial Infarction Regarding Acute and Long-term follow-up),<br />
a composite of death, reinfarction, or urgent target-